Polycaprolactone 3d printing
The Application of Polycaprolactone in Three-Dimensional Printing Scaffolds for Bone Tissue Engineering
1. Bhattacharjee P., Kundu B., Naskar D., Kim H.-W., Maiti T.K., Bhattacharya D., Kundu S.C. Silk scaffolds in bone tissue engineering: An overview. Acta Biomater. 2017;63:1–17. doi: 10.1016/j.actbio.2017.09.027. [PubMed] [CrossRef] [Google Scholar]
2. Samorezov J.E., Alsberg E. Spatial regulation of controlled bioactive factor delivery for bone tissue engineering. Adv. Drug Deliv. Rev. 2014;84:45–67. doi: 10.1016/j.addr.2014.11.018. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. Bishop E.S., Mostafa S., Pakvasa M., Luu H.H., Lee M.J., Wolf J.M., Ameer G.A., He T.-C., Reid R.R. 3-D bioprinting technologies in tissue engineering and regenerative medicine: Current and future trends. Genes Dis. 2017;4:185–195. doi: 10.1016/j.gendis.2017.10.002. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Derakhshanfar S., Mbeleck R., Xu K., Zhang X. , Zhong W., Xing M. 3D bioprinting for biomedical devices and tissue engineering: A review of recent trends and advances. Bioact. Mater. 2018;3:144–156. doi: 10.1016/j.bioactmat.2017.11.008. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Yan Q., Dong H., Su J., Han J., Song B., Wei Q., Shi Y. A Review of 3D Printing Technology for Medical Applications. Engineering. 2018;4:729–742. doi: 10.1016/j.eng.2018.07.021. [CrossRef] [Google Scholar]
6. Huang K.-H., Wang C.-Y., Chen C.-Y., Hsu T.-T., Lin C.-P. Incorporation of Calcium Sulfate Dihydrate into a Mesoporous Calcium Silicate/Poly-ε-Caprolactone Scaffold to Regulate the Release of Bone Morphogenetic Protein-2 and Accelerate Bone Regeneration. Biomedicines. 2021;9:128. doi: 10.3390/biomedicines9020128. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
7. Cao Y., Cheng P., Sang S., Xiang C., An Y., Wei X., Shen Z., Zhang Y., Li P. Mesenchymal stem cells loaded on 3D-printed gradient poly(ε-caprolactone)/methacrylated alginate composite scaffolds for cartilage tissue engineering. Regen. Biomater. 2021;8:rbab019. doi: 10.1093/rb/rbab019. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Regen. Biomater. 2021;8:rbab019. doi: 10.1093/rb/rbab019. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Dias D., Vale A.C., Cunha E.P.F., Paiva M.C., Reis R.L., Vaquette C., Alves N.M. 3D -printed cryomilled poly(ε-caprolactone)/graphene composite scaffolds for bone tissue regeneration. J. Biomed. Mater. Res. Part B Appl. Biomater. 2021;109:961–972. doi: 10.1002/jbm.b.34761. [PubMed] [CrossRef] [Google Scholar]
9. Radhakrishnan S., Nagarajan S., Belaid H., Farha C., Iatsunskyi I., Coy E., Soussan L., Huon V., Bares J., Belkacemi K., et al. Fabrication of 3D printed antimicrobial polycaprolactone scaffolds for tissue engineering applications. Mater. Sci. Eng. C. 2021;118:111525. doi: 10.1016/j.msec.2020.111525. [PubMed] [CrossRef] [Google Scholar]
10. Guo W., Chen M., Wang Z., Tian Y., Zheng J., Gao S., Li Y., Zheng Y., Li X., Huang J., et al. 3D-printed cell-free PCL–MECM scaffold with biomimetic micro-structure and micro-environment to enhance in situ meniscus regeneration. Bioact. Mater. 2021;6:3620–3633. doi: 10.1016/j.bioactmat.2021.02.019. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Bioact. Mater. 2021;6:3620–3633. doi: 10.1016/j.bioactmat.2021.02.019. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Lee H., Yeo M., Ahn S., Kang D.-O., Jang C.H., Lee H., Park G.-M., Kim G.H. Designed hybrid scaffolds consisting of polycaprolactone microstrands and electrospun collagen-nanofibers for bone tissue regeneration. J. Biomed. Mater. Res. Part B Appl. Biomater. 2011;97:263–270. doi: 10.1002/jbm.b.31809. [PubMed] [CrossRef] [Google Scholar]
12. Zimmerling A., Yazdanpanah Z., Cooper D.M.L., Johnston J.D., Chen X. 3D printing PCL/nHA bone scaffolds: Exploring the influence of material synthesis techniques. Biomater Res. 2021;25:3. doi: 10.1186/s40824-021-00204-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
13. Seyedsalehi A., Daneshmandi L., Barajaa M., Riordan J., Laurencin C.T. Fabrication and characterization of mechanically competent 3D printed polycaprolactone-reduced graphene oxide scaffolds. Sci. Rep. 2020;10:22210. doi: 10.1038/s41598-020-78977-w. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Cakmak A.M., Unal S., Sahin A., Oktar F.N., Sengor M., Ekren N., Gunduz O., Kalaskar D.M. 3D Printed Polycaprolactone/Gelatin/BacterialCellulose/Hydroxyapatite Composite Scaffold for Bone Tissue Engineering. Polymers. 2020;12:1962. doi: 10.3390/polym12091962. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Park S.A., Lee H.J., Kim S.Y., Kim K.S., Jo D.W., Park S.Y. Three-dimensionally printed polycaprolactone/beta-tricalcium phosphate scaffold was more effective as an rhBMP-2 carrier for new bone formation than polycaprolactone alone. J. Biomed. Mater. Res. Part A. 2021;109:840–848. doi: 10.1002/jbm.a.37075. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Turnbull G., Clarke J., Picard F., Riches P., Jia L., Han F., Li B., Shu W. 3D bioactive composite scaffolds for bone tissue engineering. Bioact. Mater. 2018;3:278–314. doi: 10.1016/j.bioactmat.2017.10.001. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
17. Moreno Madrid A.P., Mariel Vrech S., Alejandra Sanchez M., Paola Rodriguez A. Advances in additive manufacturing for bone tissue engineering scaffolds. Mater. Sci. Eng. C-Mater. Biol. Appl. 2019;100:631–644. doi: 10.1016/j.msec.2019.03.037. [PubMed] [CrossRef] [Google Scholar]
Moreno Madrid A.P., Mariel Vrech S., Alejandra Sanchez M., Paola Rodriguez A. Advances in additive manufacturing for bone tissue engineering scaffolds. Mater. Sci. Eng. C-Mater. Biol. Appl. 2019;100:631–644. doi: 10.1016/j.msec.2019.03.037. [PubMed] [CrossRef] [Google Scholar]
18. Arealis G., Nikolaou V.S. Bone printing: New frontiers in the treatment of bone defects. Injury. 2015;46:S20–S22. doi: 10.1016/S0020-1383(15)30050-4. [PubMed] [CrossRef] [Google Scholar]
19. Wu G.H., Hsu S.H. Review: Polymeric-Based 3D Printing for Tissue Engineering. J. Med. Biol. Eng. 2015;35:285–292. doi: 10.1007/s40846-015-0038-3. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
20. Xie C., Gao Q., Wang P., Shao L., Yuan H., Fu J., Chen W., He Y. Structure-induced cell growth by 3D printing of heterogeneous scaffolds with ultrafine fibers. Mater. Des. 2019;181:108092. doi: 10.1016/j.matdes.2019.108092. [CrossRef] [Google Scholar]
21. Eichholz K.F., Hoey D.A. Mediating human stem cell behaviour via defined fibrous architectures by melt electrospinning writing. Acta Biomater. 2018;75:140–151. doi: 10.1016/j.actbio.2018.05.048. [PubMed] [CrossRef] [Google Scholar]
Acta Biomater. 2018;75:140–151. doi: 10.1016/j.actbio.2018.05.048. [PubMed] [CrossRef] [Google Scholar]
22. He J., Xu F., Cao Y., Liu Y., Li D. Towards microscale electrohydrodynamic three-dimensional printing. J. Phys. D Appl. Phys. 2016;49:055504. doi: 10.1088/0022-3727/49/5/055504. [CrossRef] [Google Scholar]
23. Kade J.C., Dalton P.D. Polymers for Melt Electrowriting. Adv. Healthc. Mater. 2021;10:e2001232. doi: 10.1002/adhm.202001232. [PubMed] [CrossRef] [Google Scholar]
24. Hochleitner G., Jungst T., Brown T.D., Hahn K., Moseke C., Jakob F., Dalton P.D., Groll J. Additive manufacturing of scaffolds with sub-micron filaments via melt electrospinning writing. Biofabrication. 2015;7:035002. doi: 10.1088/1758-5090/7/3/035002. [PubMed] [CrossRef] [Google Scholar]
25. Kim M., Yun H-s Kim G.H. Electric-field assisted 3D-fibrous bioceramic-based scaffolds for bone tissue regeneration: Fabrication, characterization, and in vitro cellular activities. Sci. Rep. 2017;7:3166. doi: 10.1038/s41598-017-03461-x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
doi: 10.1038/s41598-017-03461-x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
26. Youssef A., Hollister S.J., Dalton P.D. Additive manufacturing of polymer melts for implantable medical devices and scaffolds. Biofabrication. 2017;9:1. doi: 10.1088/1758-5090/aa5766. [PubMed] [CrossRef] [Google Scholar]
27. Swetha S., Lavanya K., Sruthi R., Selvamurugan N. An insight into cell-laden 3D-printed constructs for bone tissue engineering. J. Mater Chem. B. 2020;8:9836–9862. doi: 10.1039/D0TB02019B. [PubMed] [CrossRef] [Google Scholar]
28. Kuss M.A., Wu S., Wang Y., Untrauer J.B., Li W., Lim J.Y., Duan B. Prevascularization of 3D printed bone scaffolds by bioactive hydrogels and cell co-culture. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018;106:1788–1798. doi: 10.1002/jbm.b.33994. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
29. Chen Y.-W., Shen Y.-F., Ho C.-C., Yu J., Wu Y.-H.A., Wang K., Shih C.-T., Shie M.-Y. Osteogenic and angiogenic potentials of the cell-laden hydrogel/mussel-inspired calcium silicate complex hierarchical porous scaffold fabricated by 3D bioprinting.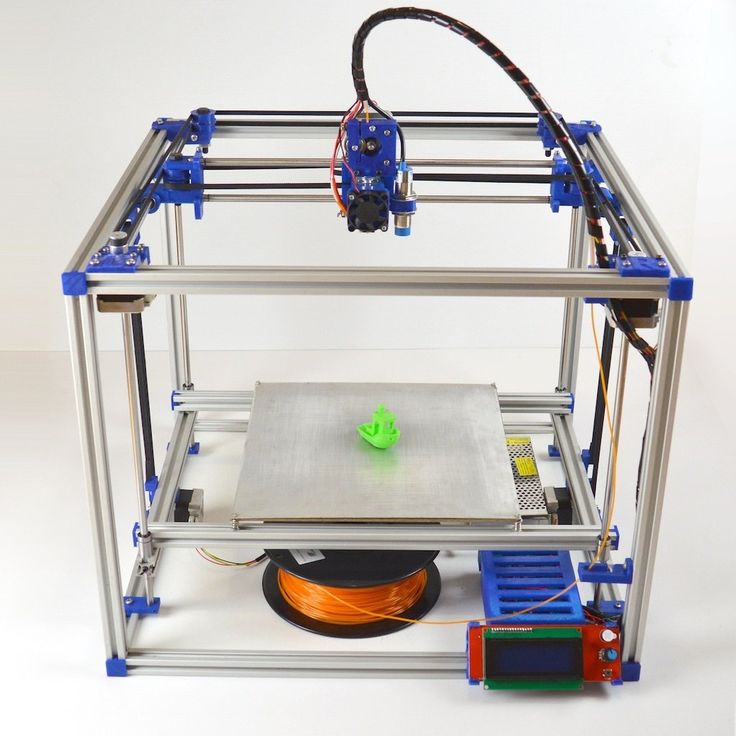 Mater. Sci. Eng. C. 2018;91:679–687. doi: 10.1016/j.msec.2018.06.005. [PubMed] [CrossRef] [Google Scholar]
Mater. Sci. Eng. C. 2018;91:679–687. doi: 10.1016/j.msec.2018.06.005. [PubMed] [CrossRef] [Google Scholar]
30. Xie H., Wang Z., Zhang L., Lei Q., Zhao A., Wang H., Li Q., Chen Z., Zhang W. Development of an angiogenesis-promoting microvesicle-alginate-polycaprolactone composite graft for bone tissue engineering applications. PeerJ. 2016;4:e2040. doi: 10.7717/peerj.2040. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Jian Z., Zhuang T., Qinyu T., Liqing P., Kun L., Xujiang L., Diaodiao W., Zhen Y., Shuangpeng J., Xiang S., et al. 3D bioprinting of a biomimetic meniscal scaffold for application in tissue engineering. Bioact. Mater. 2021;6:1711–1726. doi: 10.1016/j.bioactmat.2020.11.027. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
32. Do A.V., Khorsand B., Geary S.M., Salem A.K. 3D Printing of Scaffolds for Tissue Regeneration Applications. Adv. Healthc. Mater. 2015;4:1742–1762. doi: 10.1002/adhm.201500168. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. Fedorovich N.E., Alblas J., Hennink W.E., Oner F.C., Dhert W.J. Organ printing: The future of bone regeneration? Trends Biotechnol. 2011;29:601–606. doi: 10.1016/j.tibtech.2011.07.001. [PubMed] [CrossRef] [Google Scholar]
Fedorovich N.E., Alblas J., Hennink W.E., Oner F.C., Dhert W.J. Organ printing: The future of bone regeneration? Trends Biotechnol. 2011;29:601–606. doi: 10.1016/j.tibtech.2011.07.001. [PubMed] [CrossRef] [Google Scholar]
34. Liao G., Jiang S., Xu X., Ke Y. Electrospun aligned PLLA/PCL/HA composite fibrous membranes and their in vitro degradation behaviors. Mater. Lett. 2012;82:159–162. doi: 10.1016/j.matlet.2012.05.085. [CrossRef] [Google Scholar]
35. Guarino V., Causa F., Taddei P., Di Foggia M., Ciapetti G., Martini D., Fagnano C., Baldini N., Ambrosio L. Polylactic acid fibre-reinforced polycaprolactone scaffolds for bone tissue engineering. Biomaterials. 2008;29:3662–3670. doi: 10.1016/j.biomaterials.2008.05.024. [PubMed] [CrossRef] [Google Scholar]
36. Doyle S., Henry L., McGennisken E., Onofrillo C., Bella C., Duchi S., O’Connell C., Pirogova E. Characterization of Polycaprolactone Nanohydroxyapatite Composites with Tunable Degradability Suitable for Indirect Printing. Polymers. 2021;13:295. doi: 10.3390/polym13020295. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Polymers. 2021;13:295. doi: 10.3390/polym13020295. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
37. Liu H., Du Y., Yang G., Hu X., Wang L., Liu B., Wang J., Zhang S. Delivering Proangiogenic Factors from 3D-Printed Polycaprolactone Scaffolds for Vascularized Bone Regeneration. Adv. Health Mater. 2020;9:e2000727. doi: 10.1002/adhm.202000727. [PubMed] [CrossRef] [Google Scholar]
38. Wu Y.-H.A., Chiu Y.-C., Lin Y.-H., Ho C.-C., Shie M.-Y., Chen Y.-W. 3D-Printed Bioactive Calcium Silicate/Poly-epsilon-Caprolactone Bioscaffolds Modified with Biomimetic Extracellular Matrices for Bone Regeneration. Int. J. Mol. Sci. 2019;20:942. doi: 10.3390/ijms20040942. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
39. Wang W., Junior J.R.P., Nalesso P.R., Musson D., Cornish J., Mendonça F., Caetano G.F., Bartolo P. Engineered 3D printed poly(ε-caprolactone)/graphene scaffolds for bone tissue engineering. Mater. Sci. Eng. C. 2019;100:759–770. doi: 10.1016/j.msec.2019.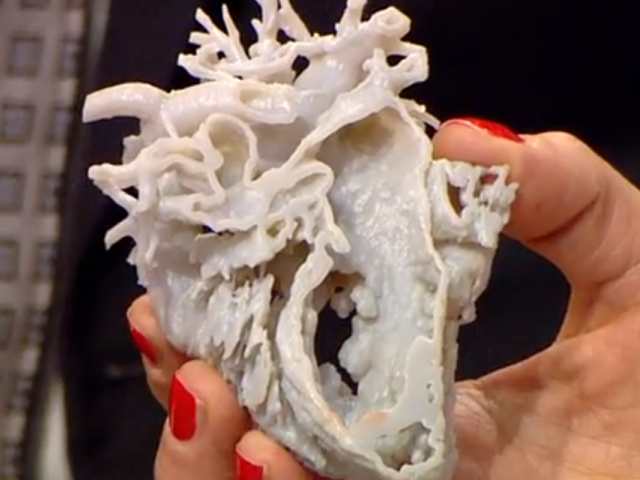 03.047. [PubMed] [CrossRef] [Google Scholar]
03.047. [PubMed] [CrossRef] [Google Scholar]
40. Unagolla J.M., Jayasuriya A.C. Enhanced cell functions on graphene oxide incorporated 3D printed polycaprolactone scaffolds. Mater. Sci. Eng. C-Mater. Biol. Appl. 2019;102:1–11. doi: 10.1016/j.msec.2019.04.026. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
41. Park J., Park S., Kim J.E., Jang K.J., Seonwoo H., Chung J.H. Enhanced Osteogenic Differentiation of Periodontal Ligament Stem Cells Using a Graphene Oxide-Coated Poly(epsilon-caprolactone) Scaffold. Polymers. 2021;13:797. doi: 10.3390/polym13050797. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Huang B., Vyas C., Roberts I., Poutrel Q.-A., Chiang W.-H., Blaker J.J., Huang Z., Bártolo P. Fabrication and characterisation of 3D printed MWCNT composite porous scaffolds for bone regeneration. Mater. Sci. Eng. C. 2019;98:266–278. doi: 10.1016/j.msec.2018.12.100. [PubMed] [CrossRef] [Google Scholar]
43. Rogowska-Tylman J., Locs J., Salma I.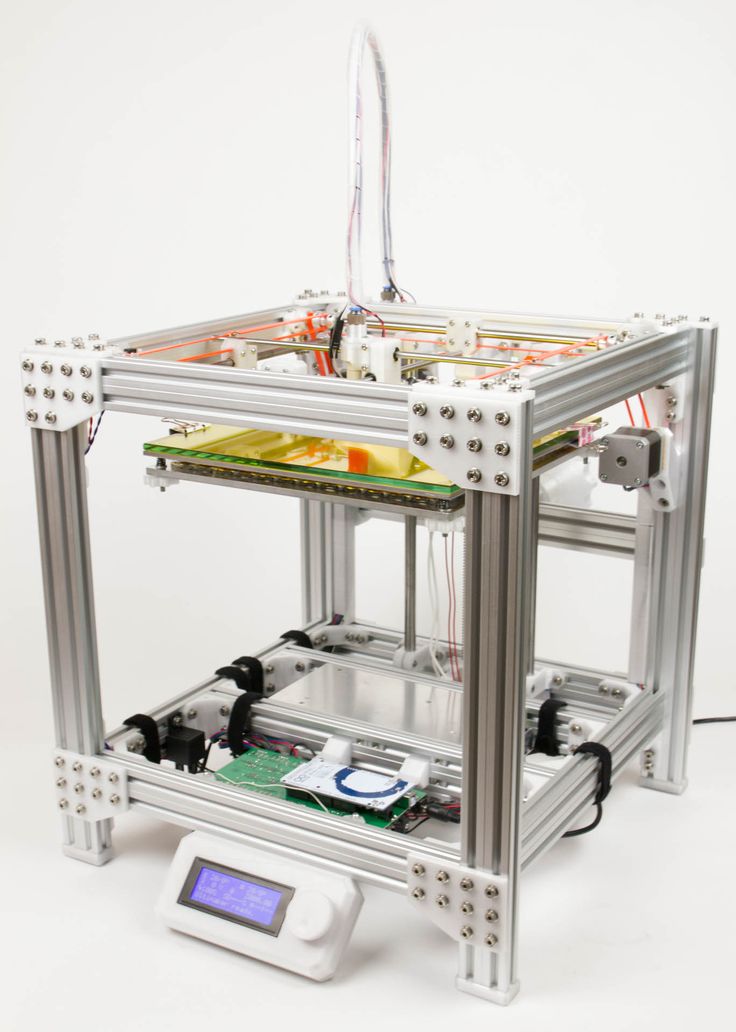 , Woźniak B., Pilmane M., Zalite V., Wojnarowicz J., Kędzierska-Sar A., Chudoba T., Szlazak K., et al. In vivo and in vitro study of a novel nanohydroxyapatite sonocoated scaffolds for enhanced bone regeneration. Mater. Sci. Eng. C. 2019;99:669–684. doi: 10.1016/j.msec.2019.01.084. [PubMed] [CrossRef] [Google Scholar]
, Woźniak B., Pilmane M., Zalite V., Wojnarowicz J., Kędzierska-Sar A., Chudoba T., Szlazak K., et al. In vivo and in vitro study of a novel nanohydroxyapatite sonocoated scaffolds for enhanced bone regeneration. Mater. Sci. Eng. C. 2019;99:669–684. doi: 10.1016/j.msec.2019.01.084. [PubMed] [CrossRef] [Google Scholar]
44. Bas O., Hanßke F., Lim J., Ravichandran A., Kemnitz E., Teoh S.-H., Hutmacher D.W., Börner H.G. Tuning mechanical reinforcement and bioactivity of 3D printed ternary nanocomposites by interfacial peptide-polymer conjugates. Biofabrication. 2019;11:035028. doi: 10.1088/1758-5090/aafec8. [PubMed] [CrossRef] [Google Scholar]
45. Petretta M., Gambardella A., Boi M., Berni M., Cavallo C., Marchiori G., Maltarello M., Bellucci D., Fini M., Baldini N., et al. Composite Scaffolds for Bone Tissue Regeneration Based on PCL and Mg-Containing Bioactive Glasses. Biology. 2021;10:398. doi: 10.3390/biology10050398. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
46. Rumiński S., Ostrowska B., Jaroszewicz J., Skirecki T., Włodarski K., Swieszkowski W., Lewandowska-Szumieł M. Three-dimensional printed polycaprolactone-based scaffolds provide an advantageous environment for osteogenic differentiation of human adipose-derived stem cells. J. Tissue Eng. Regen. Med. 2018;12:e473–e485. doi: 10.1002/term.2310. [PubMed] [CrossRef] [Google Scholar]
Rumiński S., Ostrowska B., Jaroszewicz J., Skirecki T., Włodarski K., Swieszkowski W., Lewandowska-Szumieł M. Three-dimensional printed polycaprolactone-based scaffolds provide an advantageous environment for osteogenic differentiation of human adipose-derived stem cells. J. Tissue Eng. Regen. Med. 2018;12:e473–e485. doi: 10.1002/term.2310. [PubMed] [CrossRef] [Google Scholar]
47. Luo W., Zhang S., Lan Y., Huang C., Wang C., Lai X., Chen H., Ao N. 3D printed porous polycaprolactone/oyster shell powder (PCL/OSP) scaffolds for bone tissue engineering. Mater. Res. Express. 2018;5:045403. doi: 10.1088/2053-1591/aab916. [CrossRef] [Google Scholar]
48. Moncal K.K., Heo D.N., Godzik K.P., Sosnoski D.M., Mrowczynski O.D., Rizk E., Ozbolat V., Tucker S.M., Gerhard E.M., Dey M., et al. 3D printing of poly(ε-caprolactone)/poly(d,l-lactide-co-glycolide)/hydroxyapatite composite constructs for bone tissue engineering. J. Mater. Res. 2018;33:1972–1986. doi: 10.1557/jmr.2018.111. [CrossRef] [Google Scholar]
[CrossRef] [Google Scholar]
49. Rindone A.N., Nyberg E., Grayson W.L. 3D-Printing Composite Polycaprolactone-Decellularized Bone Matrix Scaffolds for Bone Tissue Engineering Applications. Methods Mol. Biol. 2018;1577:209–226. [PubMed] [Google Scholar]
50. Hung B.P., Naved B.A., Nyberg E.L., Dias M., Holmes C., Elisseeff J.H., Dorafshar A., Grayson W.L. Three-Dimensional Printing of Bone Extracellular Matrix for Craniofacial Regeneration. ACS Biomater. Sci. Eng. 2016;2:1806–1816. doi: 10.1021/acsbiomaterials.6b00101. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
51. Park S.A., Lee S.J., Seok J.M., Lee J.H., Kim W.D., Kwon I.K. Fabrication of 3D Printed PCL/PEG Polyblend Scaffold Using Rapid Prototyping System for Bone Tissue Engineering Application. J. Bionic. Eng. 2018;15:435–442. doi: 10.1007/s42235-018-0034-8. [CrossRef] [Google Scholar]
52. Kim J.-Y., Ahn G., Kim C., Lee J.-S., Lee I.-G., An S.-H., Yun W.-S., Kim S.-Y., Shim J.-H. Synergistic Effects of Beta Tri-Calcium Phosphate and Porcine-Derived Decellularized Bone Extracellular Matrix in 3D-Printed Polycaprolactone Scaffold on Bone Regeneration.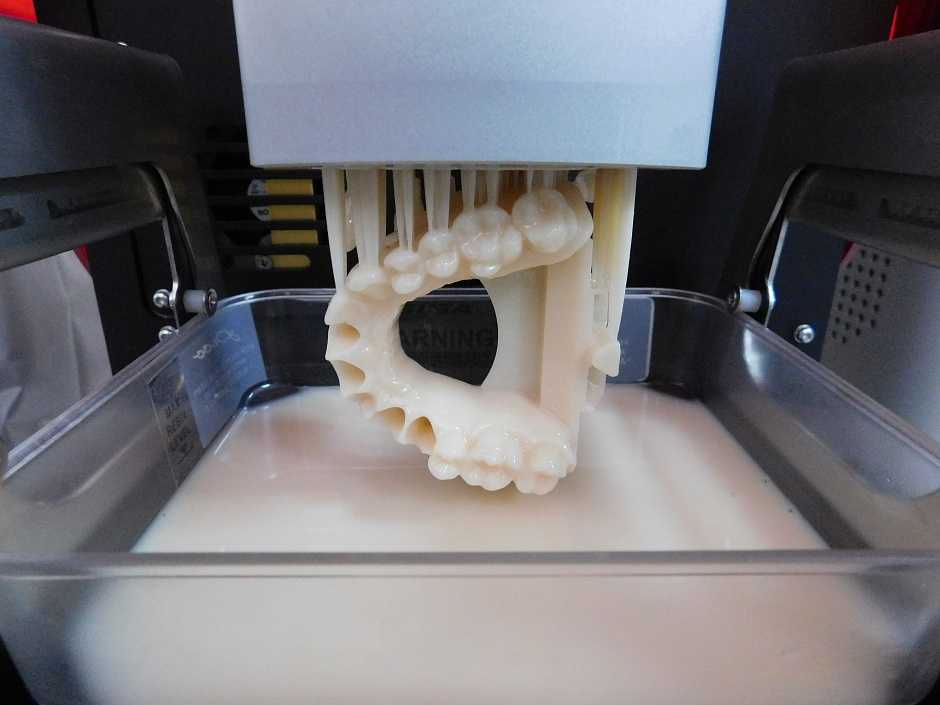 Macromol. Biosci. 2018;18:e1800025. doi: 10.1002/mabi.201800025. [PubMed] [CrossRef] [Google Scholar]
Macromol. Biosci. 2018;18:e1800025. doi: 10.1002/mabi.201800025. [PubMed] [CrossRef] [Google Scholar]
53. Vella J.B., Trombetta R.P., Hoffman M.D., Inzana J., Awad H., Benoit D.S.W. Three-dimensional printed calcium phosphate and poly(caprolactone) composites with improved mechanical properties and preserved microstructure. J. Biomed. Mater. Res. Part A. 2018;106:663–672. doi: 10.1002/jbm.a.36270. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
54. Tamjid E. Three-dimensional polycaprolactone-bioactive glass composite scaffolds: Effect of particle size and volume fraction on mechanical properties and in vitro cellular behavior. Int. J. Polym. Mater. Polym. Biomater. 2018;67:1005–1015. doi: 10.1080/00914037.2017.1417285. [CrossRef] [Google Scholar]
55. Neufurth M., Wang X., Wang S., Steffen R., Ackermann M., Haep N.D., Schröder H.C., Müller W.E. 3D printing of hybrid biomaterials for bone tissue engineering: Calcium-polyphosphate microparticles encapsulated by polycaprolactone. Acta Biomater. 2017;64:377–388. doi: 10.1016/j.actbio.2017.09.031. [PubMed] [CrossRef] [Google Scholar]
Acta Biomater. 2017;64:377–388. doi: 10.1016/j.actbio.2017.09.031. [PubMed] [CrossRef] [Google Scholar]
56. Hwang K.-S., Choi J.-W., Kim J.-H., Chung H.Y., Jin S., Shim J.-H., Yun W.-S., Jeong C.-M., Huh J.-B. Comparative Efficacies of Collagen-Based 3D Printed PCL/PLGA/β-TCP Composite Block Bone Grafts and Biphasic Calcium Phosphate Bone Substitute for Bone Regeneration. Materials. 2017;10:421. doi: 10.3390/ma10040421. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
57. Park J., Lee S.J., Jo H.H., Lee J.H., Kim W.D., Lee J.Y., Park S.A. Fabrication and characterization of 3D-printed bone-like β-tricalcium phosphate/polycaprolactone scaffolds for dental tissue engineering. J. Ind. Eng. Chem. 2017;46:175–181. doi: 10.1016/j.jiec.2016.10.028. [CrossRef] [Google Scholar]
58. Shim K.-S., Kim S.E., Yun Y.-P., Jeon D.I., Kim H.J., Park K., Song H.-R. Surface immobilization of biphasic calcium phosphate nanoparticles on 3D printed poly(caprolactone) scaffolds enhances osteogenesis and bone tissue regeneration. J. Ind. Eng. Chem. 2017;55:101–109. doi: 10.1016/j.jiec.2017.06.033. [CrossRef] [Google Scholar]
J. Ind. Eng. Chem. 2017;55:101–109. doi: 10.1016/j.jiec.2017.06.033. [CrossRef] [Google Scholar]
59. Chiu Y.-C., Fang H.-Y., Hsu T.-T., Lin C.-Y., Shie M.-Y. The Characteristics of Mineral Trioxide Aggregate/Polycaprolactone 3-dimensional Scaffold with Osteogenesis Properties for Tissue Regeneration. J. Endod. 2017;43:923–929. doi: 10.1016/j.joen.2017.01.009. [PubMed] [CrossRef] [Google Scholar]
60. Daly A.C., Cunniffe G.M., Sathy B.N., Jeon O., Alsberg E., Kelly D.J. 3D Bioprinting of Developmentally Inspired Templates for Whole Bone Organ Engineering. Adv. Healthc. Mater. 2016;5:2353–2362. doi: 10.1002/adhm.201600182. [PubMed] [CrossRef] [Google Scholar]
61. Miao S., Zhu W., Castro N.J., Leng J., Zhang L.G. Four-Dimensional Printing Hierarchy Scaffolds with Highly Biocompatible Smart Polymers for Tissue Engineering Applications. Tissue Eng. Part C-Methods. 2016;22:952–963. doi: 10.1089/ten.tec.2015.0542. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
62. Gonçalves E.M., Oliveira F., Silva R., Neto M.A., Fernandes M.H., Amaral M., Vallet-Regí M., Vila M. Three-dimensional printed PCL-hydroxyapatite scaffolds filled with CNTs for bone cell growth stimulation. J. Biomed. Mater. Res. Part B Appl. Biomater. 2016;104:1210–1219. doi: 10.1002/jbm.b.33432. [PubMed] [CrossRef] [Google Scholar]
Gonçalves E.M., Oliveira F., Silva R., Neto M.A., Fernandes M.H., Amaral M., Vallet-Regí M., Vila M. Three-dimensional printed PCL-hydroxyapatite scaffolds filled with CNTs for bone cell growth stimulation. J. Biomed. Mater. Res. Part B Appl. Biomater. 2016;104:1210–1219. doi: 10.1002/jbm.b.33432. [PubMed] [CrossRef] [Google Scholar]
63. Karimipour-Fard P., Jeffrey M.P., JonesTaggart H., Pop-Iliev R., Rizvi G. Development, processing and characterization of Polycaprolactone/Nano-Hydroxyapatite/Chitin-Nano-Whisker nanocomposite filaments for additive manufacturing of bone tissue scaffolds. J. Mech. Behav. Biomed. Mater. 2021;120:104583. doi: 10.1016/j.jmbbm.2021.104583. [PubMed] [CrossRef] [Google Scholar]
64. Wang C., Xu H., Liu C., Peng Z., Min R., Zhang Z., Li J., Jin Y., Wang Y., Li Z., et al. CaO2/gelatin oxygen slow-releasing microspheres facilitate tissue engineering efficiency for the osteonecrosis of femoral head by enhancing the angiogenesis and survival of grafted bone marrow mesenchymal stem cells. Biomater. Sci. 2021;9:3005–3018. doi: 10.1039/D0BM02071K. [PubMed] [CrossRef] [Google Scholar]
Biomater. Sci. 2021;9:3005–3018. doi: 10.1039/D0BM02071K. [PubMed] [CrossRef] [Google Scholar]
65. Nyberg E., Rindone A., Dorafshar A., Grayson W.L. Comparison of 3D-Printed Poly-epsilon-Caprolactone Scaffolds Functionalized with Tricalcium Phosphate, Hydroxyapatite, Bio-Oss, or Decellularized Bone Matrix. Tissue Eng. Part A. 2017;23:503. doi: 10.1089/ten.tea.2016.0418. [PubMed] [CrossRef] [Google Scholar]
66. Domingos M., Gloria A., Coelho J., Bartolo P., Ciurana J. Three-dimensional printed bone scaffolds: The role of nano/micro-hydroxyapatite particles on the adhesion and differentiation of human mesenchymal stem cells. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2017;231:555–564. doi: 10.1177/0954411916680236. [PubMed] [CrossRef] [Google Scholar]
67. Chen F., Hochleitner G., Woodfield T., Groll J., Dalton P.D., Amsden B.G. Additive Manufacturing of a Photo-Cross-Linkable Polymer via Direct Melt Electrospinning Writing for Producing High Strength Structures. Biomacromolecules.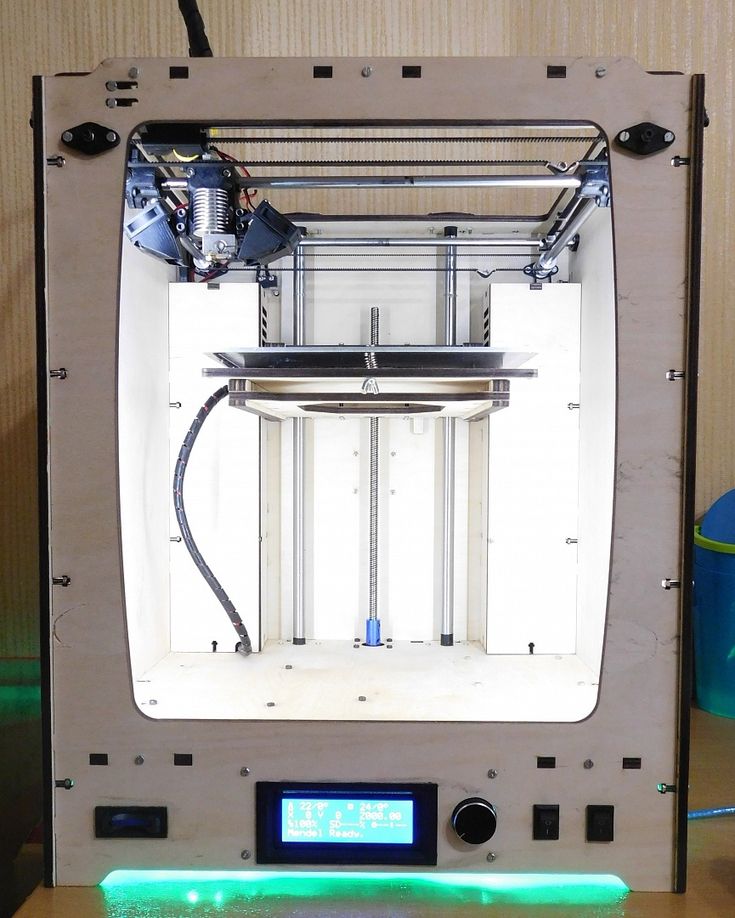 2016;17:208–214. doi: 10.1021/acs.biomac.5b01316. [PubMed] [CrossRef] [Google Scholar]
2016;17:208–214. doi: 10.1021/acs.biomac.5b01316. [PubMed] [CrossRef] [Google Scholar]
68. Butscher A., Bohner M., Hofmann S., Gauckler L., Muller R. Structural and material approaches to bone tissue engineering in powder-based three-dimensional printing. Acta Biomater. 2011;7:907–920. doi: 10.1016/j.actbio.2010.09.039. [PubMed] [CrossRef] [Google Scholar]
69. Loh Q.L., Choong C. Three-dimensional scaffolds for tissue engineering applications: Role of porosity and pore size. Tissue Eng. Part B Rev. 2013;19:485–502. doi: 10.1089/ten.teb.2012.0437. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
70. Fonseca D.R., Sobreiro-Almeida R., Sol P.C., Neves N.M. Development of non-orthogonal 3D-printed scaffolds to enhance their osteogenic performance. Biomater. Sci. 2018;6:1569–1579. doi: 10.1039/C8BM00073E. [PubMed] [CrossRef] [Google Scholar]
71. Shim J.-H., Jeong J.-H., Won J.-Y., Bae J.-H., Ahn G., Jeon H., Yun W.-S., Bae E.-B., Choi J.-W., Lee S.-H., et al. Porosity effect of 3D-printed polycaprolactone membranes on calvarial defect model for guided bone regeneration.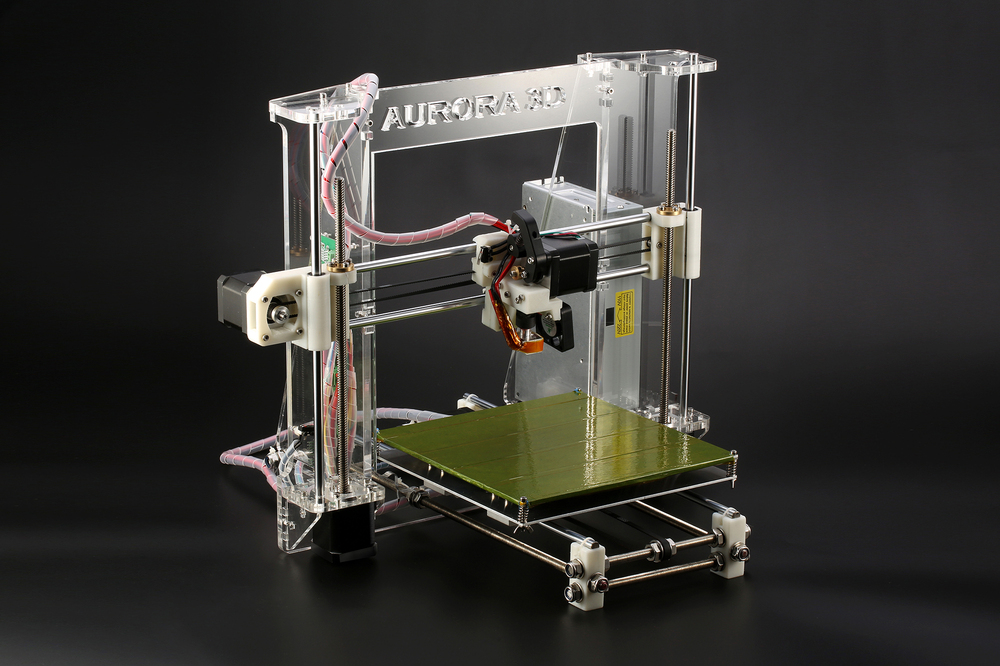 Biomed. Mater. 2017;13:015014. doi: 10.1088/1748-605X/aa9bbc. [PubMed] [CrossRef] [Google Scholar]
Biomed. Mater. 2017;13:015014. doi: 10.1088/1748-605X/aa9bbc. [PubMed] [CrossRef] [Google Scholar]
72. Yang T., Hu Y., Wang C., Binks B.P. Fabrication of Hierarchical Macroporous Biocompatible Scaffolds by Combining Pickering High Internal Phase Emulsion Templates with Three-Dimensional Printing. ACS Appl. Mater. Interfaces. 2017;9:22950–22958. doi: 10.1021/acsami.7b05012. [PubMed] [CrossRef] [Google Scholar]
73. Olubamiji A.D., Izadifar Z., Si J.L., Cooper D.M.L., Eames B.F., Chen D.X.B. Modulating mechanical behaviour of 3D-printed cartilage-mimetic PCL scaffolds: Influence of molecular weight and pore geometry. Biofabrication. 2016;8:025020. doi: 10.1088/1758-5090/8/2/025020. [PubMed] [CrossRef] [Google Scholar]
74. Lee S.-H., Cho Y.S., Hong M.W., Lee B.-K., Park Y., Park S.-H., Kim Y.Y., Cho Y.-S. Mechanical properties and cell-culture characteristics of a polycaprolactone kagome-structure scaffold fabricated by a precision extruding deposition system. Biomed. Mater.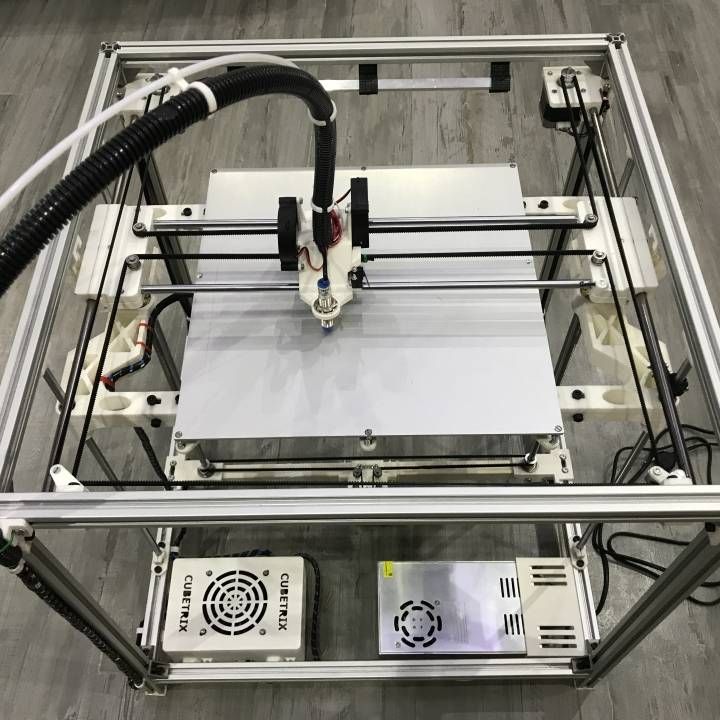 2017;12:055003. doi: 10.1088/1748-605X/aa8357. [PubMed] [CrossRef] [Google Scholar]
2017;12:055003. doi: 10.1088/1748-605X/aa8357. [PubMed] [CrossRef] [Google Scholar]
75. Feasibility of Fabricating Personalized 3D-Printed Bone Grafts Guided by High-Resolution Imaging. [(accessed on 27 June 2021)]; Available online: https://www.spiedigitallibrary.org/conference-proceedings-of-spie/10138/101380O/Feasibility-of-fabricating-personalized-3D-printed-bone-grafts-guided-by/10.1117/12.2254475.short?SSO=1
76. Barbara O., Andrea D.L., Lorenzo M., Wojciech S. Influence of internal pore architecture on biological and mechanical properties of three-dimensional fiber deposited scaffolds for bone regeneration. Biomed. Mater Res. A. 2016;104:991–1001. [PubMed] [Google Scholar]
77. Roh H.-S., Lee C.-M., Hwang Y.-H., Kook M.-S., Yang S.-W., Lee D., Kim B.-H. Addition of MgO nanoparticles and plasma surface treatment of three-dimensional printed polycaprolactone/hydroxyapatite scaffolds for improving bone regeneration. Mater. Sci. Eng. C. 2017;74:525–535. doi: 10.1016/j. msec.2016.12.054. [PubMed] [CrossRef] [Google Scholar]
msec.2016.12.054. [PubMed] [CrossRef] [Google Scholar]
78. Stichler S., Böck T., Paxton N., Bertlein S., Levato R., Schill V., Smolan W., Malda J., Tessmar J., Blunk T., et al. Double printing of hyaluronic acid/poly(glycidol) hybrid hydrogels with poly(ε-caprolactone) for MSC chondrogenesis. Biofabrication. 2017;9:044108. doi: 10.1088/1758-5090/aa8cb7. [PubMed] [CrossRef] [Google Scholar]
79. Zheng P., Yao Q., Mao F., Liu N., Xu Y., Wei B., Wang L. Adhesion, proliferation and osteogenic differentiation of mesenchymal stem cells in 3D printed poly-ε-caprolactone/hydroxyapatite scaffolds combined with bone marrow clots. Mol. Med. Rep. 2017;16:5078–5084. doi: 10.3892/mmr.2017.7266. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
80. Szlazak K., Jaroszewicz J., Ostrowska B., Nabiałek M., Szota M., Swieszkowski W. Characterization of Three-Dimensional Printed Composite Scaffolds Prepared with Different Fabrication Methods. Arch. Met. Mater. 2016;61:645–650. doi: 10. 1515/amm-2016-0110. [CrossRef] [Google Scholar]
1515/amm-2016-0110. [CrossRef] [Google Scholar]
81. Theodoridis K., Aggelidou E., Vavilis T., Manthou M.E., Tsimponis A., Demiri E.C., Boukla A., Salpistis C., Bakopoulou A., Mihailidis A., et al. Hyaline cartilage next generation implants from adipose-tissue-derived mesenchymal stem cells: Comparative study on 3D-printed polycaprolactone scaffold patterns. J. Tissue Eng. Regen. Med. 2019;13:342–355. doi: 10.1002/term.2798. [PubMed] [CrossRef] [Google Scholar]
82. Yang G.H., Kim M., Kim G. Additive-manufactured polycaprolactone scaffold consisting of innovatively designed microsized spiral struts for hard tissue regeneration. Biofabrication. 2016;9:15005. doi: 10.1088/1758-5090/9/1/015005. [PubMed] [CrossRef] [Google Scholar]
83. Yang G.-H., Lee H., Kim G. Preparation and characterization of spiral-like micro-struts with nano-roughened surface for enhancing the proliferation and differentiation of preosteoblasts. J. Ind. Eng. Chem. 2018;61:244–254. doi: 10.1016/j.jiec. 2017.12.022. [CrossRef] [Google Scholar]
2017.12.022. [CrossRef] [Google Scholar]
84. Cho Y.S., Hong M.W., Quan M., Kim S.-Y., Lee S.-H., Lee S.-J., Kim Y.Y., Cho Y.-S. Assessments for bone regeneration using the polycaprolactone SLUP (salt-leaching using powder) scaffold. J. Biomed. Mater. Res. Part A. 2017;105:3432–3444. doi: 10.1002/jbm.a.36196. [PubMed] [CrossRef] [Google Scholar]
85. Gupta D., Singh A.K., Kar N., Dravid A., Bellare J. Modelling and optimization of NaOH-etched 3-D printed PCL for enhanced cellular attachment and growth with minimal loss of mechanical strength. Mater. Sci. Eng. C-Mater. Biol. Appl. 2019;98:602–611. doi: 10.1016/j.msec.2018.12.084. [PubMed] [CrossRef] [Google Scholar]
86. Shan Y., Wang Y., Fan Y., Yang J., Ren W., Yu X., Li J., Shi H. Biomechanical properties and cellular biocompatibility of 3D printed tracheal graft. Bioprocess Biosyst. Eng. 2017;40:1813–1823. doi: 10.1007/s00449-017-1835-6. [PubMed] [CrossRef] [Google Scholar]
87. Lee S.-H., Lee K.-G., Hwang J.-H., Cho Y.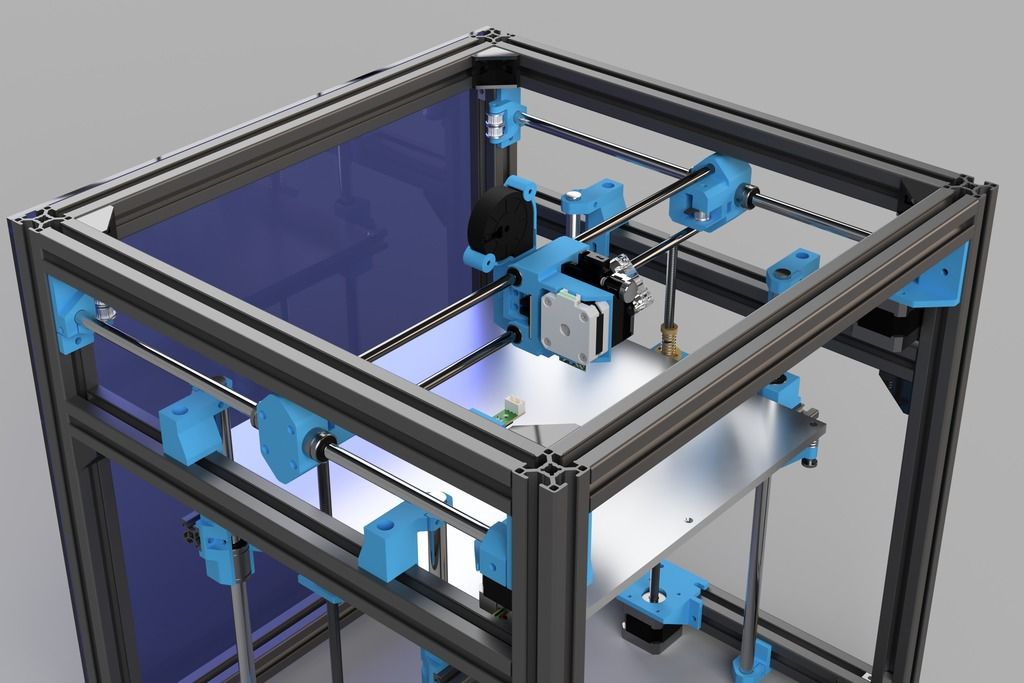 S., Jeong H.-J., Park S.-H., Park Y., Cho Y.-S., Lee B.-K. Evaluation of mechanical strength and bone regeneration ability of 3D printed kagome-structure scaffold using rabbit calvarial defect model. Mater. Sci. Eng. C. 2019;98:949–959. doi: 10.1016/j.msec.2019.01.050. [PubMed] [CrossRef] [Google Scholar]
S., Jeong H.-J., Park S.-H., Park Y., Cho Y.-S., Lee B.-K. Evaluation of mechanical strength and bone regeneration ability of 3D printed kagome-structure scaffold using rabbit calvarial defect model. Mater. Sci. Eng. C. 2019;98:949–959. doi: 10.1016/j.msec.2019.01.050. [PubMed] [CrossRef] [Google Scholar]
88. Lee J.W., Chu S.G., Kim H.T., Choi K.Y., Oh E.J., Shim J.-H., Yun W.-S., Huh J.B., Moon S.H., Kang S.S., et al. Osteogenesis of Adipose-Derived and Bone Marrow Stem Cells with Polycaprolactone/Tricalcium Phosphate and Three-Dimensional Printing Technology in a Dog Model of Maxillary Bone Defects. Polymers. 2017;9:450. doi: 10.3390/polym9090450. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
89. Bae J.C., Lee J.-J., Shim J.-H., Park K.-H., Lee J.-S., Bae E.-B., Choi J.-W., Huh J.-B. Development and Assessment of a 3D-Printed Scaffold with rhBMP-2 for an Implant Surgical Guide Stent and Bone Graft Material: A Pilot Animal Study. Materials. 2017;10:1434. doi: 10.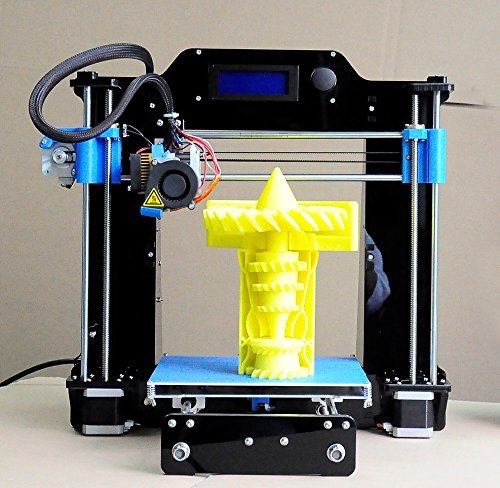 3390/ma10121434. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3390/ma10121434. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
90. Rider P., Kacarevic Z.P., Alkildani S., Retnasingh S., Schnettler R., Barbeck M. Additive Manufacturing for Guided Bone Regeneration: A Perspective for Alveolar Ridge Augmentation. Int. J. Mol. Sci. 2018;19:3308. doi: 10.3390/ijms19113308. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
91. Bartolo P., Domingos M., Gloria A., Ciurana J. BioCell Printing: Integrated automated assembly system for tissue engineering constructs. CIRP Ann. 2011;60:271–274. doi: 10.1016/j.cirp.2011.03.116. [CrossRef] [Google Scholar]
92. Daly A.C., Critchley S.E., Rencsok E.M., Kelly D.J. A comparison of different bioinks for 3D bioprinting of fibrocartilage and hyaline cartilage. Biofabrication. 2016;8:045002. doi: 10.1088/1758-5090/8/4/045002. [PubMed] [CrossRef] [Google Scholar]
93. Critchley S., Sheehy E., Cunniffe G., Diaz-Payno P., Carroll S.F., Jeon O., Alsberg E., Brama P.A., Kelly D.J. 3D printing of fibre-reinforced cartilaginous templates for the regeneration of osteochondral defects.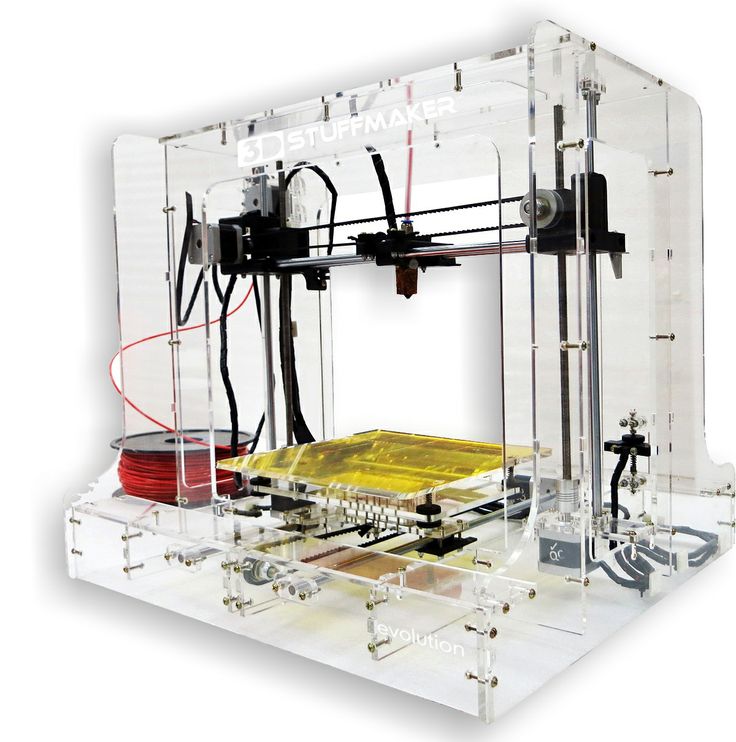 Acta Biomater. 2020;113:130–143. doi: 10.1016/j.actbio.2020.05.040. [PubMed] [CrossRef] [Google Scholar]
Acta Biomater. 2020;113:130–143. doi: 10.1016/j.actbio.2020.05.040. [PubMed] [CrossRef] [Google Scholar]
94. Sun Y., Wu Q., Zhang Y., Dai K., Wei Y. 3D-bioprinted gradient-structured scaffold generates anisotropic cartilage with vascularization by pore-size-dependent activation of HIF1α/FAK signaling axis. Nanomedicine. 2021:102426. doi: 10.1016/j.nano.2021.102426. [PubMed] [CrossRef] [Google Scholar]
95. Murphy C., Kolan K., Li W., Semon J., Day D., Leu M. 3D bioprinting of stem cells and polymer/bioactive glass composite scaffolds for bone tissue engineering. Int. J. Bioprinting. 2017;3:54–64. doi: 10.18063/IJB.2017.01.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
96. Kim Y.B., Lee H., Yang G.-H., Choi C.H., Lee D., Hwang H., Jung W.-K., Yoon H., Kim G.H. Mechanically reinforced cell-laden scaffolds formed using alginate-based bioink printed onto the surface of a PCL/alginate mesh structure for regeneration of hard tissue. J. Colloid Interface Sci. 2016;461:359–368.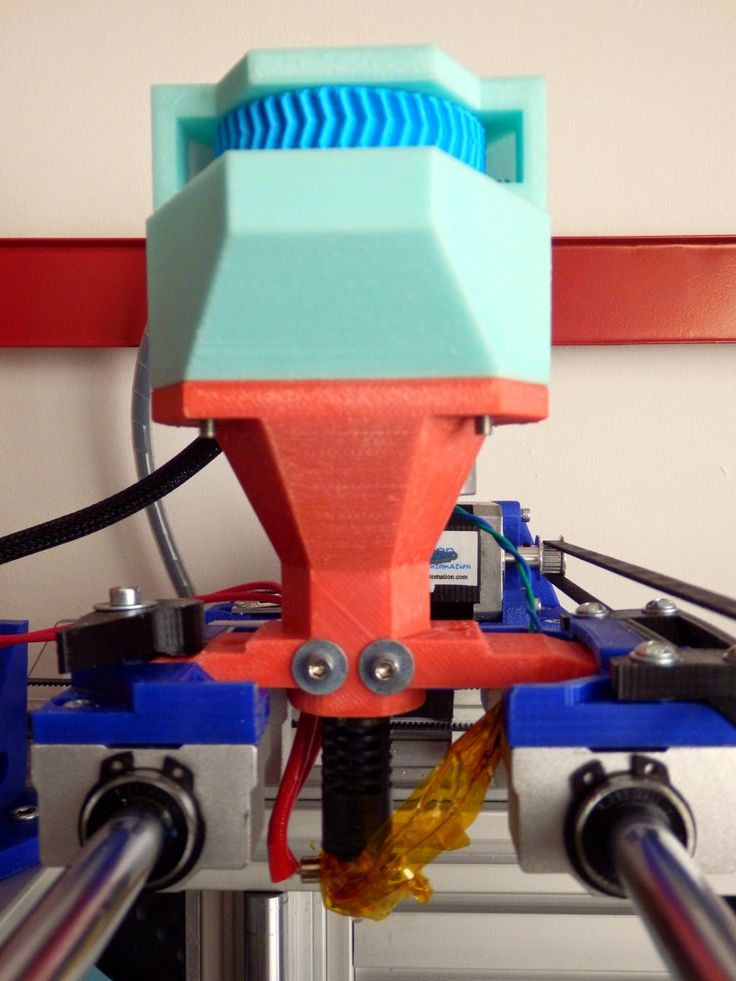 doi: 10.1016/j.jcis.2015.09.044. [PubMed] [CrossRef] [Google Scholar]
doi: 10.1016/j.jcis.2015.09.044. [PubMed] [CrossRef] [Google Scholar]
97. Garcia J.R., Garcia A.J. Biomaterial-mediated strategies targeting vascularization for bone repair. Drug Deliv. Trans. L Res. 2016;6:77–95. doi: 10.1007/s13346-015-0236-0. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
98. Amini A.R., Laurencin C.T., Nukavarapu S.P. Differential analysis of peripheral blood- and bone marrow-derived endothelial progenitor cells for enhanced vascularization in bone tissue engineering. J. Orthop. Res. 2012;30:1507–1515. doi: 10.1002/jor.22097. [PubMed] [CrossRef] [Google Scholar]
99. Zhang Q., Nettleship I., Schmelzer E., Gerlach J.C., Zhang M.X., Wang J., Liu C. Tissue Engineering and Regenerative Medicine Therapies for Cell Senescence in Bone and Cartilage. Tissue Eng. Part B Rev. 2020;26:64–78. doi: 10.1089/ten.teb.2019.0215. [PubMed] [CrossRef] [Google Scholar]
100. Dang H.P., Shabab T., Shafiee A., Peiffer Q.C., Fox K., Tran N., Dargaville T., Hutmacher D. W., A Tran P. 3D printed dual macro-, microscale porous network as a tissue engineering scaffold with drug delivering function. Biofabrication. 2019;11:035014. doi: 10.1088/1758-5090/ab14ff. [PubMed] [CrossRef] [Google Scholar]
W., A Tran P. 3D printed dual macro-, microscale porous network as a tissue engineering scaffold with drug delivering function. Biofabrication. 2019;11:035014. doi: 10.1088/1758-5090/ab14ff. [PubMed] [CrossRef] [Google Scholar]
101. Govender M., Indermun S., Kumar P., Choonara Y.E., Pillay V. 3D Printed, PVA–PAA Hydrogel Loaded-Polycaprolactone Scaffold for the Delivery of Hydrophilic In-Situ Formed Sodium Indomethacin. Materials. 2018;11:1006. doi: 10.3390/ma11061006. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
102. Shao J., Ma J., Lin L., Wang B., Jansen J.A., Walboomers X.F., Zuo Y., Yang F. Three-Dimensional Printing of Drug-Loaded Scaffolds for Antibacterial and Analgesic Applications. Tissue Eng. Part C Methods. 2019;25:222–231. doi: 10.1089/ten.tec.2018.0293. [PubMed] [CrossRef] [Google Scholar]
103. Kim S.E., Yun Y.-P., Shim K.-S., Kim H.J., Park K., Song H.-R. 3D printed alendronate-releasing poly(caprolactone) porous scaffolds enhance osteogenic differentiation and bone formation in rat tibial defects. Biomed. Mater. 2016;11:055005. doi: 10.1088/1748-6041/11/5/055005. [PubMed] [CrossRef] [Google Scholar]
Biomed. Mater. 2016;11:055005. doi: 10.1088/1748-6041/11/5/055005. [PubMed] [CrossRef] [Google Scholar]
104. Puppi D., Piras A.M., Pirosa A., Sandreschi S., Chiellini F. Levofloxacin-loaded star poly(ε-caprolactone) scaffolds by additive manufacturing. J. Mater. Sci. Mater. Med. 2016;27:44. doi: 10.1007/s10856-015-5658-1. [PubMed] [CrossRef] [Google Scholar]
105. Bessa P.C., Balmayor E.R., Azevedo H., Nürnberger S., Casal M., van Griensven M., Reis R.L., Redl H. Silk fibroin microparticles as carriers for delivery of human recombinant BMPs. Physical characterization and drug release. J. Tissue Eng. Regen. Med. 2010;4:349–355. doi: 10.1002/term.245. [PubMed] [CrossRef] [Google Scholar]
106. Jang C.H., Lee J., Kim G. Synergistic effect of alginate/BMP-2/Umbilical cord serum-coated on 3D-printed PCL biocomposite for mastoid obliteration model. J. Ind. Eng. Chem. 2019;72:432–441. doi: 10.1016/j.jiec.2018.12.046. [CrossRef] [Google Scholar]
107. Melke J., Midha S., Ghosh S. , Ito K., Hofmann S. Silk fibroin as biomaterial for bone tissue engineering. Acta Biomater. 2016;31:1–16. doi: 10.1016/j.actbio.2015.09.005. [PubMed] [CrossRef] [Google Scholar]
, Ito K., Hofmann S. Silk fibroin as biomaterial for bone tissue engineering. Acta Biomater. 2016;31:1–16. doi: 10.1016/j.actbio.2015.09.005. [PubMed] [CrossRef] [Google Scholar]
108. Wagner E., Parry J., Dadsetan M., Bravo D., Riester S.M., Van Wijnen A.J., Yaszemski M.J., Kakar S. VEGF-mediated angiogenesis and vascularization of a fumarate-crosslinked polycaprolactone (PCLF) scaffold. Connect. Tissue Res. 2018;59:542–549. doi: 10.1080/03008207.2018.1424145. [PubMed] [CrossRef] [Google Scholar]
109. He Y., Liu W., Guan L., Chen J., Duan L., Jia Z., Huang Z., Li W., Liu J., Xiong Z., et al. A 3D-Printed PLCL Scaffold Coated with Collagen Type I and Its Biocompatibility. Biomed Res. Int. 2018;2018:5147156. doi: 10.1155/2018/5147156. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
110. Kim W., Jang C.H., Kim G. Optimally designed collagen/polycaprolactone biocomposites supplemented with controlled. release of HA/TCP/rhBMP-2 and HA/TCP/PRP for hard tissue regeneration. Mater. Sci. Eng. C-Mater. Biol. Appl. 2017;78:763–772. doi: 10.1016/j.msec.2017.04.144. [PubMed] [CrossRef] [Google Scholar]
Mater. Sci. Eng. C-Mater. Biol. Appl. 2017;78:763–772. doi: 10.1016/j.msec.2017.04.144. [PubMed] [CrossRef] [Google Scholar]
111. Lee S.J., Lee H.-J., Kim S.-Y., Seok J.M., Lee J.H., Kim W.D., Kwon I.K., Park S.-Y., A Park S. In situgold nanoparticle growth on polydopamine-coated 3D-printed scaffolds improves osteogenic differentiation for bone tissue engineering applications:in vitroandin vivostudies. Nanoscale. 2018;10:15447–15453. doi: 10.1039/C8NR04037K. [PubMed] [CrossRef] [Google Scholar]
112. Bartnikowski M., Moon H.-J., Ivanovski S. Release of lithium from 3D printed polycaprolactone scaffolds regulates macrophage and osteoclast response. Biomed. Mater. 2018;13:065003. doi: 10.1088/1748-605X/aad916. [PubMed] [CrossRef] [Google Scholar]
113. Hamlet S.M., Vaquette C., Shah A., Hutmacher D.W., Ivanovski S. 3-Dimensional functionalized polycaprolactone-hyaluronic acid hydrogel constructs for bone tissue engineering. J. Clin. Periodontol. 2017;44:428–437. doi: 10.1111/jcpe. 12686. [PubMed] [CrossRef] [Google Scholar]
12686. [PubMed] [CrossRef] [Google Scholar]
114. Lee S.J., Lee D., Yoon T.R., Kim H.K., Jo H.H., Park J.S., Lee J.H., Kim W.D., Kwon I.K., A Park S. Surface modification of 3D-printed porous scaffolds via mussel-inspired polydopamine and effective immobilization of rhBMP-2 to promote osteogenic differentiation for bone tissue engineering. Acta Biomater. 2016;40:182–191. doi: 10.1016/j.actbio.2016.02.006. [PubMed] [CrossRef] [Google Scholar]
115. Bari E., Scocozza F., Perteghella S., Sorlini M., Auricchio F., Torre M., Conti M. 3D Bioprinted Scaffolds Containing Mesenchymal Stem/Stromal Lyosecretome: Next Generation Controlled Release Device for Bone Regenerative Medicine. Pharmacrutics. 2021;13:515. doi: 10.3390/pharmaceutics13040515. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
116. Gong L., Li J., Zhang J., Pan Z., Liu Y., Zhou F., Hong Y., Hu Y., Gu Y., Ouyang H., et al. An interleukin-4-loaded bi-layer 3D printed scaffold promotes osteochondral regeneration. Acta Biomater. 2020;117:246–260. doi: 10.1016/j.actbio.2020.09.039. [PubMed] [CrossRef] [Google Scholar]
Acta Biomater. 2020;117:246–260. doi: 10.1016/j.actbio.2020.09.039. [PubMed] [CrossRef] [Google Scholar]
117. Li J., Chen M., Wei X., Hao Y., Wang J. Evaluation of 3D-Printed Polycaprolactone Scaffolds Coated with Freeze-Dried Platelet-Rich Plasma for Bone Regeneration. Materials. 2017;10:831. doi: 10.3390/ma10070831. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
118. Cunniffe G.M., Gonzalez-Fernandez T., Daly A., Sathy B.N., Jeon O., Alsberg E., Kelly D. Three-Dimensional Bioprinting of Polycaprolactone Reinforced Gene Activated Bioinks for Bone Tissue Engineering. Tissue Eng. Part A. 2017;23:891–900. doi: 10.1089/ten.tea.2016.0498. [PubMed] [CrossRef] [Google Scholar]
119. Wei P., Xu Y., Gu Y., Yao Q., Li J., Wang L. IGF-1-releasing PLGA nanoparticles modified 3D printed PCL scaffolds for cartilage tissue engineering. Drug Deliv. 2020;27:1106–1114. doi: 10.1080/10717544.2020.1797239. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
120. Mostafavi A. , Abudula T., Russell C.S., Mostafavi E., Williams T.J., Salah N., Alshahrie A., Harris S., Basri S.M.M., Mishra Y.K., et al. In situ printing of scaffolds for reconstruction of bone defects. Acta Biomater. 2021;127:313–326. doi: 10.1016/j.actbio.2021.03.009. [PubMed] [CrossRef] [Google Scholar]
, Abudula T., Russell C.S., Mostafavi E., Williams T.J., Salah N., Alshahrie A., Harris S., Basri S.M.M., Mishra Y.K., et al. In situ printing of scaffolds for reconstruction of bone defects. Acta Biomater. 2021;127:313–326. doi: 10.1016/j.actbio.2021.03.009. [PubMed] [CrossRef] [Google Scholar]
121. Zhao S., Xie K., Guo Y., Tan J., Wu J., Yang Y., Fu P., Wang L., Jiang W., Hao Y. Fabrication and Biological Activity of 3D-Printed Polycaprolactone/Magnesium Porous Scaffolds for Critical Size Bone Defect Repair. ACS Biomater. Sci. Eng. 2020;6:5120–5131. doi: 10.1021/acsbiomaterials.9b01911. [PubMed] [CrossRef] [Google Scholar]
122. Hansske F., Bas O., Vaquette C., Hochleitner G., Groll J., Kemnitz E., Hutmacher D.W., Börner H.G. Via precise interface engineering towards bioinspired composites with improved 3D printing processability and mechanical properties. J. Mater. Chem. B. 2017;5:5037–5047. doi: 10.1039/C7TB00165G. [PubMed] [CrossRef] [Google Scholar]
123. Yang L., Ullah I. , Yu K., Zhang W., Zhou J., Sun T., Shi L., Yao S., Chen K., Zhang X., et al. Bioactive Sr(2+)/Fe(3+)co-substituted hydroxyapatite in cryogenically 3D printed porous scaffolds for bone tissue engineering. Biofabrication. 2021;13:035007. doi: 10.1088/1758-5090/abcf8d. [PubMed] [CrossRef] [Google Scholar]
, Yu K., Zhang W., Zhou J., Sun T., Shi L., Yao S., Chen K., Zhang X., et al. Bioactive Sr(2+)/Fe(3+)co-substituted hydroxyapatite in cryogenically 3D printed porous scaffolds for bone tissue engineering. Biofabrication. 2021;13:035007. doi: 10.1088/1758-5090/abcf8d. [PubMed] [CrossRef] [Google Scholar]
124. Poh P.S.P., Hutmacher D.W., Holzapfel B.M., Solanki A.K., Stevens M.M., Woodruff M.A. In vitro and in vivo bone formation potential of surface calcium phosphate-coated polycaprolactone and polycaprolactone/bioactive glass composite scaffolds. Acta Biomater. 2016;30:319–333. doi: 10.1016/j.actbio.2015.11.012. [PubMed] [CrossRef] [Google Scholar]
125. Nyberg E.L., Farris A.L., Hung B.P., Dias M., Garcia J.R., Dorafshar A., Grayson W.L. 3D-Printing Technologies for Craniofacial Rehabilitation, Reconstruction, and Regeneration. Ann. Biomed. Eng. 2017;45:45–57. doi: 10.1007/s10439-016-1668-5. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
126. VijayaVenkataRaman S.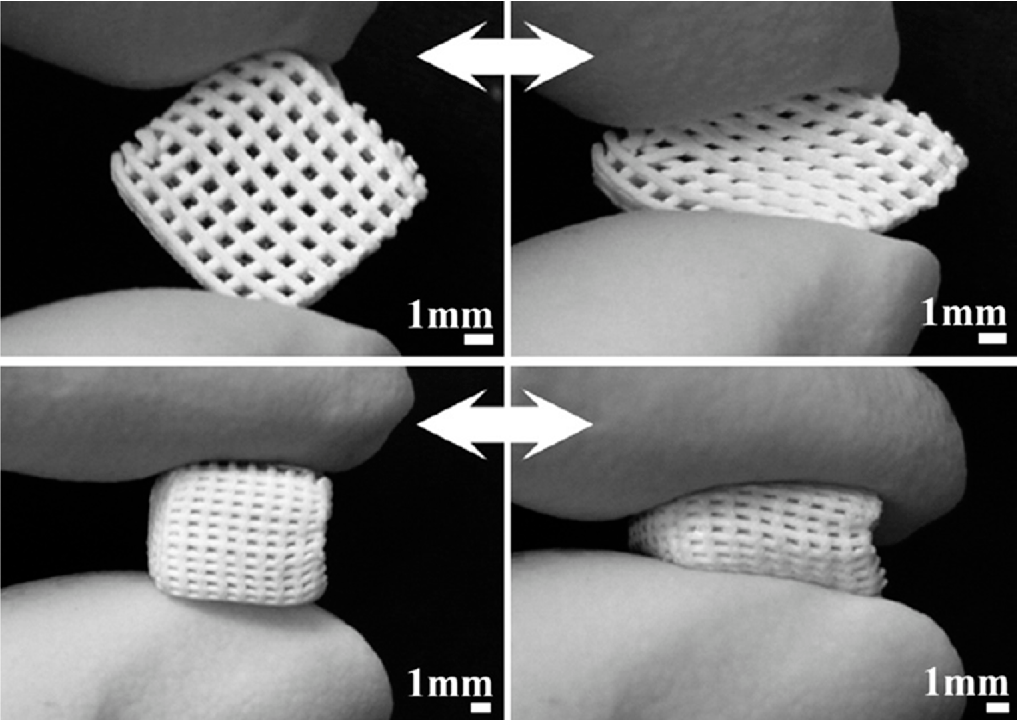 , Lu W.F., Fuh J.Y.H. 3D bioprinting of skin: A state-of-the-art review on modelling, materials, and processes. Biofabrication. 2016;8:032001. doi: 10.1088/1758-5090/8/3/032001. [PubMed] [CrossRef] [Google Scholar]
, Lu W.F., Fuh J.Y.H. 3D bioprinting of skin: A state-of-the-art review on modelling, materials, and processes. Biofabrication. 2016;8:032001. doi: 10.1088/1758-5090/8/3/032001. [PubMed] [CrossRef] [Google Scholar]
127. Yeo M., Lee H., Kim G.H. Combining a micro/nano-hierarchical scaffold with cell-printing of myoblasts induces cell alignment and differentiation favorable to skeletal muscle tissue regeneration. Biofabrication. 2016;8:035021. doi: 10.1088/1758-5090/8/3/035021. [PubMed] [CrossRef] [Google Scholar]
128. Bahcecioglu G., Hasirci N., Bilgen B., Hasirci V. A 3D printed PCL/hydrogel construct with zone-specific biochemical composition mimicking that of the meniscus. Biofabrication. 2018;11:025002. doi: 10.1088/1758-5090/aaf707. [PubMed] [CrossRef] [Google Scholar]
129. Zhang Z.-Z., Wang S.-J., Zhang J.-Y., Jiang W.-B., Huang A.-B., Qi Y.-S., Ding J.-X., Chen X.-S., Jiang D., Yu J.-K. 3D-Printed Poly(ε-caprolactone) Scaffold Augmented With Mesenchymal Stem Cells for Total Meniscal Substitution: A 12- and 24-Week Animal Study in a Rabbit Model. Am. J. Sports Med. 2017;45:1497–1511. doi: 10.1177/0363546517691513. [PubMed] [CrossRef] [Google Scholar]
Am. J. Sports Med. 2017;45:1497–1511. doi: 10.1177/0363546517691513. [PubMed] [CrossRef] [Google Scholar]
130. Jung B.K., Kim J.Y., Kim Y.S., Roh T.S., Seo A., Park K.-H., Shim J.-H., Yun I.S. Ideal scaffold design for total ear reconstruction using a three-dimensional printing technique. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019;107:1295–1303. doi: 10.1002/jbm.b.34222. [PubMed] [CrossRef] [Google Scholar]
131. Park H.S., Lee J.S., Jung H., Kim D.Y., Kim S.W., Sultan T., Park C.H. An omentum-cultured 3D-printed artificial trachea: In Vivo bioreactor. Artif. Cells Nanomed. Biotechnol. 2018;46:S1131–S1140. doi: 10.1080/21691401.2018.1533844. [PubMed] [CrossRef] [Google Scholar]
132. Gao M., Zhang H., Dong W., Bai J., Gao B., Xia D., Feng B., Chen M., He X., Yin M., et al. Tissue-engineered trachea from a 3D-printed scaffold enhances whole-segment tracheal repair. Sci. Rep. 2017;7:5246. doi: 10.1038/s41598-017-05518-3. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
133. Soares C.S., Barros L.C., Saraiva V., Gomez-Florit M., Babo P.S., Dias I., Reis R.L., Carvalho P.P., E Gomes M. Bioengineered surgical repair of a chronic oronasal fistula in a cat using autologous platelet-rich fibrin and bone marrow with a tailored 3D printed implant. J. Feline Med. Surg. 2018;20:835–843. doi: 10.1177/1098612X18789549. [PubMed] [CrossRef] [Google Scholar]
Soares C.S., Barros L.C., Saraiva V., Gomez-Florit M., Babo P.S., Dias I., Reis R.L., Carvalho P.P., E Gomes M. Bioengineered surgical repair of a chronic oronasal fistula in a cat using autologous platelet-rich fibrin and bone marrow with a tailored 3D printed implant. J. Feline Med. Surg. 2018;20:835–843. doi: 10.1177/1098612X18789549. [PubMed] [CrossRef] [Google Scholar]
134. Chung R., Kalyon D.M., Yu X., Valdevit A. Segmental bone replacement via patient-specific, three-dimensional printed bioresorbable graft substitutes and their use as templates for the culture of mesenchymal stem cells under mechanical stimulation at various frequencies. Biotechnol. Bioeng. 2018;115:2365–2376. doi: 10.1002/bit.26780. [PubMed] [CrossRef] [Google Scholar]
135. Temple J.P., Hutton D.L., Hung B.P., Huri P.Y., Cook C.A., Kondragunta R., Jia X., Grayson W.L. Engineering anatomically shaped vascularized bone grafts with hASCs and 3D-printed PCL scaffolds. J. Biomed. Mater. Res. Part A. 2014;102:4317–4325.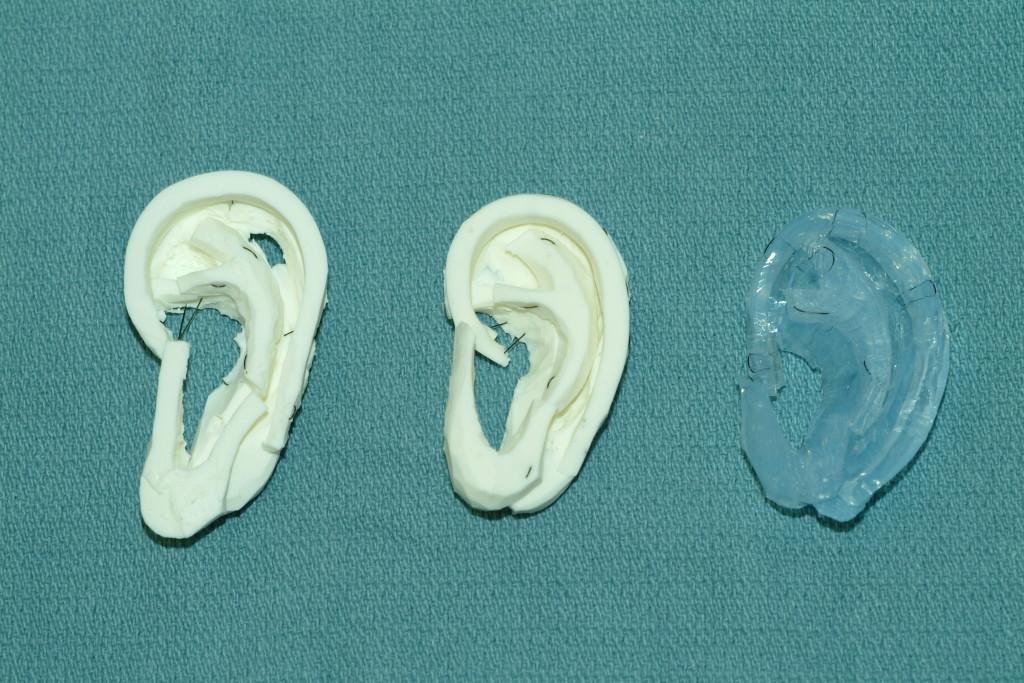 doi: 10.1002/jbm.a.35107. [PubMed] [CrossRef] [Google Scholar]
doi: 10.1002/jbm.a.35107. [PubMed] [CrossRef] [Google Scholar]
136. Vaquette C., Mitchell J., Fernandez-Medina T., Kumar S., Ivanovski S. Resorbable additively manufactured scaffold imparts dimensional stability to extraskeletally regenerated bone. Biomaterials. 2021;269:120671. doi: 10.1016/j.biomaterials.2021.120671. [PubMed] [CrossRef] [Google Scholar]
3D-Printed Poly-Caprolactone Scaffolds Modified With Biomimetic Extracellular Matrices for Tarsal Plate Tissue Engineering
Introduction
The tarsal plate is one of the most important components of the eyelid. It is composed of dense connective tissue, rich elastic fibers, and a large number of meibomian glands. The tarsal plate provides both structural support and physical form, making it an essential component of the eyelid's function and appearance (Sun et al., 2015). The meibomian gland is a type of sebaceous gland with a tubuloacinar structure and holocrine function. It is located in the superior and inferior tarsal plates (Nichols et al. , 2011). Meibomian glands secrete meibum, a compound made up of polar (phospholipids) and non-polar (cholesterol, wax esters, and cholesterol esters) lipids (Foulks and Bron, 2003). These lipids then diffuse onto the tear film, forming the lipid layer of the tear film, which acts to stabilize the tear film and prevent tear evaporation (Hwang et al., 2017).
, 2011). Meibomian glands secrete meibum, a compound made up of polar (phospholipids) and non-polar (cholesterol, wax esters, and cholesterol esters) lipids (Foulks and Bron, 2003). These lipids then diffuse onto the tear film, forming the lipid layer of the tear film, which acts to stabilize the tear film and prevent tear evaporation (Hwang et al., 2017).
The common causes of eyelid defects are mainly the tumor invasion of the tarsal plate or orbital trauma, leading to partial- or full-thickness defects of the eyelids (Zhou et al., 2010). Tarsal plate tissue engineering is vital for eyelid reconstruction, but presently it remains limited by the complexity of the tarsal plate tissue and the lack of suitable substitutes. An ideal tarsal plate substitute should have characteristics similar to the thickness, surface characteristics, strength, and flexibility of natural tarsal tissue. Moreover, it should be tissue compatible and easy to obtain and handle (Chen et al., 2005). The commonly used substitutes to repair defects of the tarsal plate mainly include hard plate mucosa (Mannor et al. , 1994; Goldberg et al., 1999), nasal cartilage, and heterogenic sclera (Tenzel et al., 1975). However, these tissues have their limitations, such as large shrinkage of postoperative grafts, a limited range of tissues, and immune rejection. The biggest defect is the inability to replace the secretory function of the meibomian glands in the tarsal plate. Therefore, fabricating a tarsal plate substitute that has a certain secretion function of lipids is important.
, 1994; Goldberg et al., 1999), nasal cartilage, and heterogenic sclera (Tenzel et al., 1975). However, these tissues have their limitations, such as large shrinkage of postoperative grafts, a limited range of tissues, and immune rejection. The biggest defect is the inability to replace the secretory function of the meibomian glands in the tarsal plate. Therefore, fabricating a tarsal plate substitute that has a certain secretion function of lipids is important.
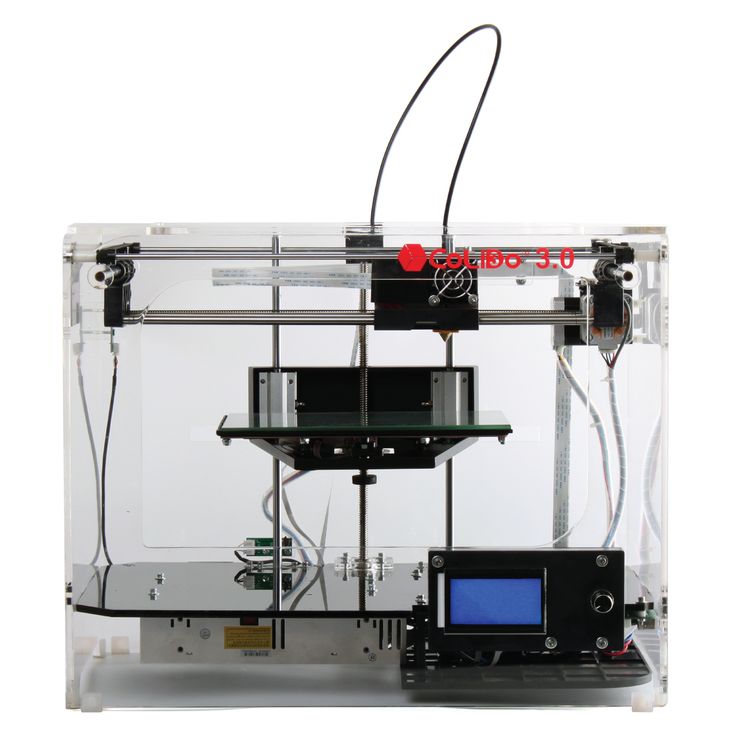
Three-dimensional (3D) printing is a technique for creating 3D objects of an individual nature using computer-aided design (Song et al., 2018). It has played a revolutionary role in the production of tissue engineering scaffolds because it overcomes the existing limitations and creates the most suitable scaffolds through simple and effective porosity dimensions that cannot be achieved using traditional scaffolding techniques (Kao et al., 2015; Yu et al., 2016). The useful features of the additive manufacturing technology can also be further implemented in the bioprinting and bio-scaffolding of biological objects with intricate architecture (Bae et al. , 2018; Hiller et al., 2018). Because of these advantages, the 3D printing technology can be very well used to print delicate and complex tissues such as printing cornea (Isaacson et al., 2018; Sorkio et al., 2018).
, 2018; Hiller et al., 2018). Because of these advantages, the 3D printing technology can be very well used to print delicate and complex tissues such as printing cornea (Isaacson et al., 2018; Sorkio et al., 2018).
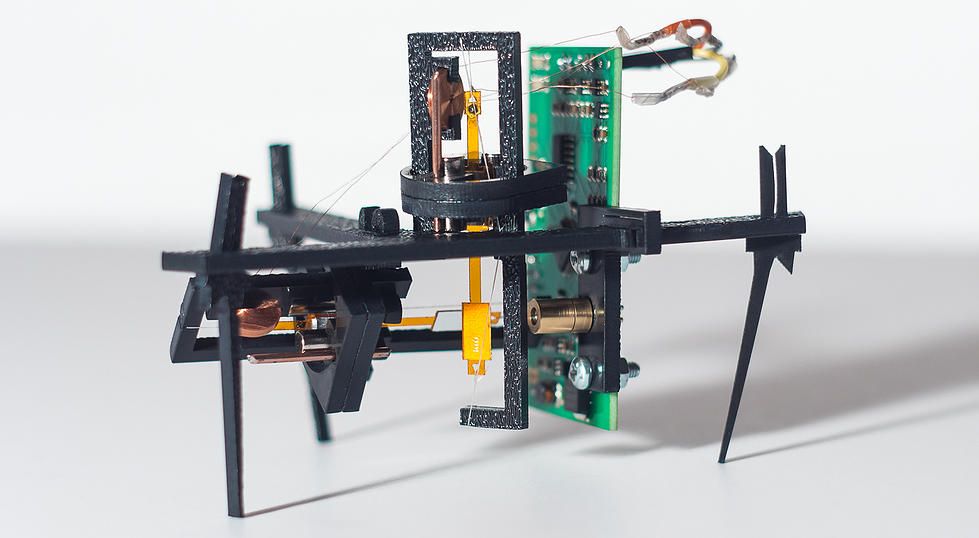
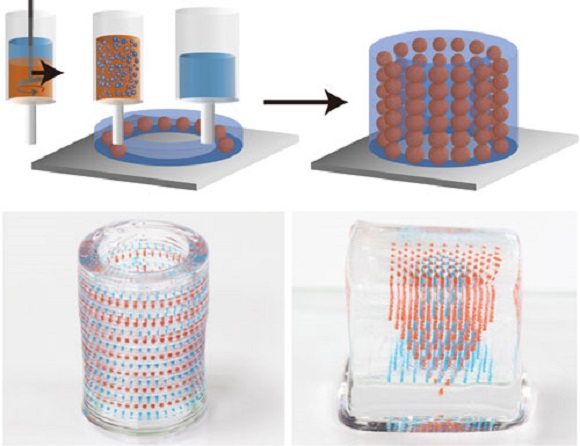
In this study, the 3D printing technology was applied, for the first time, to the fabrication of tarsal plate scaffolds through PCL. Human adipose tissue–derived stem cells (hADSCs) were seeded on PCL scaffolds and then decellularized to get a DMA–PCL scaffolds so as to enhance the biological behavior. SZ95 sebocytes were seeded on the scaffold to secrete lipids. This study aimed to assess the potential value of SZ95 sebocytes seeded on DMA–PCL scaffolds in future tarsal plate tissue engineering. The extent of cytocompatibility, cell adhesion, proliferation, and adipogenesis of the scaffolds was verified in vitro using human SZ95 sebocytes and in vivo using nude mice. A schematic showing the processes used in this study is presented in Figure 1.
Figure 1. Schematic diagram of this study. The schematic diagram of fabrication of 3D-printed DMA–PCL scaffolds and seeding of SZ95 sebocytes on the scaffolds for tarsal plate tissue engineering.
Schematic diagram of this study. The schematic diagram of fabrication of 3D-printed DMA–PCL scaffolds and seeding of SZ95 sebocytes on the scaffolds for tarsal plate tissue engineering.
Materials and Methods
Fabrication of PCL Scaffolds
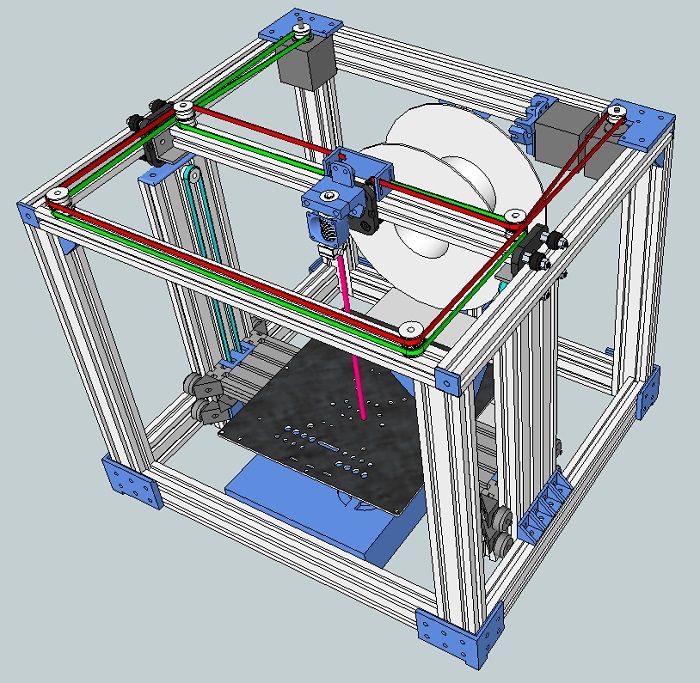
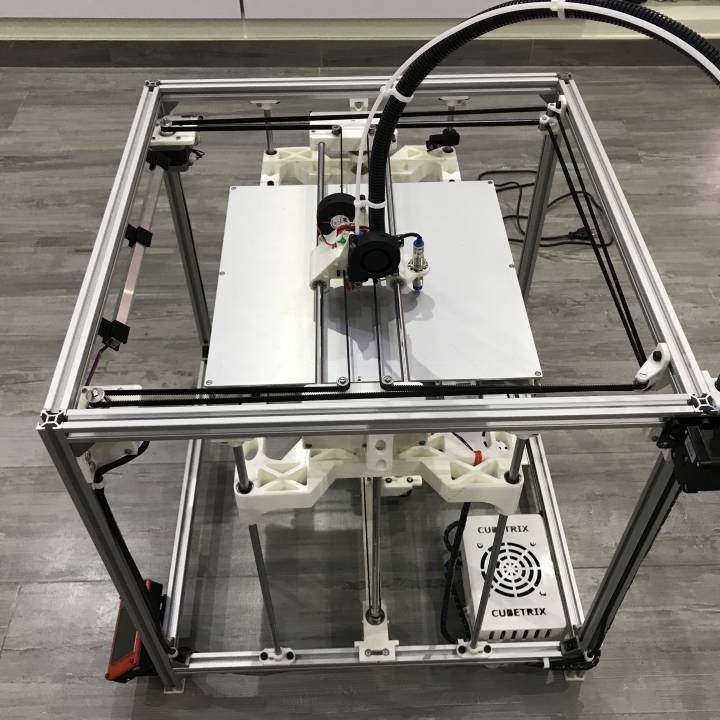
The 3D scaffolds were fabricated using a 3D printer (HTS−1200, Fochif Tech, China). The PCL beads (Mw: 40–45 kDa, supplied by Wuxi Shaxinnaxin Material, China) were put into the printing cartridge and pre-heated. Subsequently, the paste was heated to 70°C and layered with a nozzle (diameter, 0.31 μm) at a printing speed of 2 mm/s. Different pore sizes (200, 300, and 400 μm) of PCL were evaluated and an optimal pore size was chosen.
Characterization of PCL Scaffolds
The morphology of PCL scaffolds was observed using scanning electron microscopy (SEM; JSM-6701; JEOL, Tokyo, Japan). Samples were sputtered with gold for 50 s to increase conductivity before imaging using SEM.
Mechanical properties of PCL scaffolds were determined using a uniaxial material testing machine (CMT4202, China). Rectangular-shaped specimens (20 × 10 mm) were compressed at a constant speed of 0.5 mm/min. For each sample, the maximum slope in the linear region of the compressive stress-strain curve corresponding to a strain of 0–20% was used to calculate the compressive modulus. At least three samples were tested.
Rectangular-shaped specimens (20 × 10 mm) were compressed at a constant speed of 0.5 mm/min. For each sample, the maximum slope in the linear region of the compressive stress-strain curve corresponding to a strain of 0–20% was used to calculate the compressive modulus. At least three samples were tested.
Isolation and Culture of hADSCs
hADSCs were isolated from the eyelid subcutaneous adipose tissue of young outpatients (mainly female, aged 20–25 years) admitted for blepharoplasty. This study was approved by the Institutional Review Board of Shanghai Ninth People's Hospital affiliated to the Shanghai Jiao Tong University School of Medicine. In brief, the collected adipose tissues were minced into small pieces and digested with 0.2% collagenase A for 10 h with shaking at 37°C. The cells were then centrifuged at 1200 rpm for 10 min, and the precipitated cells were cultured in Dulbecco's modified Eagle's medium (DMEM)/F12 (Invitrogen, USA) containing 10% fetal bovine serum (FBS) and 100 U/mL penicillin/streptomycin (Gibco, USA) at 37°C in the presence of 5% CO2. The medium was replaced every 2 days.
The medium was replaced every 2 days.
DMA–PCL Scaffolds
hADSCs were cultured in DMEM/F12, containing 10% FBS and 50 μmol/L vitamin C (Sigma–Aldrich, USA) as discussed in a previous study (Ji et al., 2018). Before cell seeding, PCL scaffolds were placed in a 24-well plate. 5 × 104 of hADSCs (passage 3-5) were suspended in a 50 μL culture medium, and the cell suspension was applied dropwise on top of the scaffolds. The cell-seeded scaffolds were subsequently incubated at 37°C for half an hour to allow the adhesion of the cells into the porous structure before the expansion medium was added (500 μL/scaffold). The medium was changed every 2 days for 2 weeks. After 2 weeks, the cell separation buffer was applied. The cell separation buffer was composed of 0.5% ammonium hydroxide Triton + 20 mmol/L NH4OH and dissolved in phosphate-buffered saline (PBS). The cell separation buffer was gradually dropped into the plate, allowed to stand for 5 min, and then washed three times with PBS. Subsequently, 100 U/mL DNase (Sigma–Aldrich, USA) was added. The scaffolds were retained at 37°C for 1 h, washed three times with PBS, dried, and stored (in the dark) at 4°C.
Subsequently, 100 U/mL DNase (Sigma–Aldrich, USA) was added. The scaffolds were retained at 37°C for 1 h, washed three times with PBS, dried, and stored (in the dark) at 4°C.
Contact Angle of PCL and DMA-PCL Scaffolds
The water contact angles of PCL and DMA-PCL scaffolds were determined by the solid drop method. Measurements were handled using a goniometer, Data Physics (model OCA 15 Plus) System, equipped with an electronic syringe, a video camera and SCA 20 software. First, the scaffolds were placed on the plate of the goniometer and centered with the tip of the needle. Afterwards, using the software, a drop of 4 μL ultrapure water was released through the needle over the scaffold. The process was observed using a camera, which captured the exact moment the raindrops reached the surface of the scaffold. This procedure was repeated three times to obtain the average contact angle of the left and right parts of the droplet.
Immunofluorescence of Collagen I and Fibronectin on PCL and DMA-PCL Scaffolds
ADSCs both with and without decellularization on scaffolds were fixed with 4% paraformaldehyde, and the samples were incubated with the following antibodies overnight at 4°C: anti-fibronectin (1:500, BD Biosciences) and anti-collagen I (1:200, Santa Cruz). Following immunofluorescence, the scaffolds were incubated with a 1:400 dilution of fluorescence-labeled secondary antibodies diluted in PBS (Alexa Fluor 488-goat anti-rabbit/mouse and Alexa Fluor 546-goat anti-rabbit/mouse, BD Biosciences) and protected from light for 1 h at room temperature. A confocal laser scanning microscope (CLSM) (A1, Nikon, Japan) was used to capture images.
Following immunofluorescence, the scaffolds were incubated with a 1:400 dilution of fluorescence-labeled secondary antibodies diluted in PBS (Alexa Fluor 488-goat anti-rabbit/mouse and Alexa Fluor 546-goat anti-rabbit/mouse, BD Biosciences) and protected from light for 1 h at room temperature. A confocal laser scanning microscope (CLSM) (A1, Nikon, Japan) was used to capture images.
Culture of SZ95 Sebocytes and Cell Morphology on 3D Scaffolds
A total of 1 × 105 SZ95 sebocytes (Zouboulis et al., 1999) were seeded on PCL scaffolds or DMA-PCL scaffolds, in DMEM (Gibco, CA, USA), supplemented with 10% FBS (Gibco), 5 ng/mL recombinant human epidermal growth factor (Peprotech, USA), and 100 U/mL penicillin/streptomycin (Gibco, USA) in a humidified atmosphere containing 5% CO2 at 37°C. The detailed cell culture method was the same as mentioned earlier for hADSCs. The medium was replaced every other day. Seven days after cell seeding, the scaffolds were fixed with 0. 25% glutaraldehyde (Merck, Germany) at 4°C overnight. The samples were rinsed with PBS three times and then dehydrated with graded concentrations of ethanol (30, 50, 70, 80, 90, and 100% v/v) for 10 min each. Subsequently, the samples were critical-point dried, following which they were sputter-coated with gold and examined using an SEM.
25% glutaraldehyde (Merck, Germany) at 4°C overnight. The samples were rinsed with PBS three times and then dehydrated with graded concentrations of ethanol (30, 50, 70, 80, 90, and 100% v/v) for 10 min each. Subsequently, the samples were critical-point dried, following which they were sputter-coated with gold and examined using an SEM.
Live/Dead Viability Assay
Viability staining was performed using Live/Dead assay (Thermo Fisher Scientific, CA, USA) as described in a previous study (Chen et al., 2015). In brief, 5 × 104 SZ95 sebocytes were cultured for 7 days in the culture medium on scaffolds or in 24-well plates (control group). After the culture solution was sucked and rinsed with PBS, the cells were incubated in PBS containing ethidium homodimer 2 (EthD-2) and calcein-acetoxymethyl ester (CAM) at 37°C for 15 min and washed with PBS for three times. Live cells were stained with green-fluorescent CAM, and dead cells were stained with red-fluorescent EthD-2. A fluorescent microscope (Olympus BX51; Olympus, Tokyo, Japan) was used to capture images of cell staining.
A fluorescent microscope (Olympus BX51; Olympus, Tokyo, Japan) was used to capture images of cell staining.
Quantification of Cell Viability
To detect the effect of 3D-printed scaffolds with or without DMA on cell proliferation, a cell CCK-8 assay kit (Dojindo, Japan) was used. In brief, SZ95 sebocytes were seeded onto the scaffolds at a density of 2 × 104 cells/well in 24-well plates. After 0, 1, 3, 5, and 7 days of cell seeding, the cells were incubated with 10% CCK-8 in the medium. After incubation for 4 h, the absorbance of each well was measured at 450 nm using a microplate reader (ELx800, Bio-Tek, USA).
Immunofluorescence of F-actin and Assessment of Lipid Production on Scaffolds
SZ95 sebocytes were seeded onto the scaffolds at a density of 5 × 104 cells/well in 24-well plates. After 7 days of culture, the SZ95 sebocytes were fixed with 4% paraformaldehyde (Sigma–Aldrich), dissolved in PBS for 15 min, and washed with PBS at room temperature. The specimens were immersed in phalloidin conjugated to Alexa Fluor 505 (1:1,000 dilution in PBS, Invitrogen) to obtain an F-actin cytoskeleton for 1 h at room temperature. Then, the scaffolds were washed with PBS for three times. For neutral lipid droplet staining, the cells were incubated in HCS LipidTox solution (1:1,000 dilution in PBS, Invitrogen) for 30 min at room temperature. CLSM was used to capture images of cell staining.
The specimens were immersed in phalloidin conjugated to Alexa Fluor 505 (1:1,000 dilution in PBS, Invitrogen) to obtain an F-actin cytoskeleton for 1 h at room temperature. Then, the scaffolds were washed with PBS for three times. For neutral lipid droplet staining, the cells were incubated in HCS LipidTox solution (1:1,000 dilution in PBS, Invitrogen) for 30 min at room temperature. CLSM was used to capture images of cell staining.
RNA Isolation, Reverse Transcription, and Quantitative Polymerase Chain Reaction
The SZ95 sebocytes were seeded onto the scaffolds at a density of 5 × 104 cells/well in 24-well plates. After 7 days of culture, the cell-loaded scaffolds were taken out from the culture dish using microscope forceps and immersed in TRIzol reagent (Thermo Fisher Scientific, USA). Total RNA was extracted using TRIzol reagent following the manufacturer's protocols. The RNA concentration was measured using a spectrophotometer and NanoDrop 2000 software, and the OD260/280 ratio of RNA was considered to be of purity between 1. 9 and 2.1. Subsequently, 1,000 ng RNA was reverse-transcribed using a PrimeScript RT reagent kit (TaKaRa, Japan). A real-time polymerase chain reaction (PCR) was performed using a 7500 Real-Time PCR Detection System (Applied Biosystems). After 40 cycles of amplification, the relative mRNA was analyzed using the Pfaffl method (Pfaffl, 2001). The PCR efficiency of the reaction was measured with primers using serial dilutions of cDNA (1:1, 1:5, 1:25, 1:125, 1:625, and 1:3125). The primer sequences used for real-time PCR are listed in Table 1.
9 and 2.1. Subsequently, 1,000 ng RNA was reverse-transcribed using a PrimeScript RT reagent kit (TaKaRa, Japan). A real-time polymerase chain reaction (PCR) was performed using a 7500 Real-Time PCR Detection System (Applied Biosystems). After 40 cycles of amplification, the relative mRNA was analyzed using the Pfaffl method (Pfaffl, 2001). The PCR efficiency of the reaction was measured with primers using serial dilutions of cDNA (1:1, 1:5, 1:25, 1:125, 1:625, and 1:3125). The primer sequences used for real-time PCR are listed in Table 1.
Table 1. Primers used for quantitative polymerase chain reaction.
In vivo ImplantationSix nude mice were supplied by the Shanghai Animal Experimental Center. All procedures on animals were performed according to the Guidelines for Care and Use of Laboratory Animals of Shanghai Jiao Tong University School of Medicine and approved by the Animal Ethics Committee of Shanghai Ninth People's Hospital affiliated to Shanghai Jiao Tong University School of Medicine. 1 × 106 sebocytes were seeded on 3D scaffolds and cultured for 7 days in vitro. Then, the cell-seeded scaffolds were implanted into the nude mice subcutaneously. After implantation for 1 month, the nude mice were sacrificed and the samples were collected for further experiments. Each experiment was tested in triplicate. The implants were embedded in optimal cutting temperature compound (Sakura Seiki, Tokyo, Japan) and then cut into 8-mm-thick sections. Human SZ95 sebocytes were stained with human nuclear antigen antibody (Novus Biological, USA, 235-1) to evaluate the in vivo proliferation status. For Oil Red O staining, frozen DMA-PCL scaffold sections were fixed in 4% paraformaldehyde for 15 min, washed in PBS for 5 min, and stained for 10 min in freshly prepared Oil Red O solution. After washing with PBS for 15 min, the sections were counterstained with hematoxylin and mounted in 90% glycerol.
1 × 106 sebocytes were seeded on 3D scaffolds and cultured for 7 days in vitro. Then, the cell-seeded scaffolds were implanted into the nude mice subcutaneously. After implantation for 1 month, the nude mice were sacrificed and the samples were collected for further experiments. Each experiment was tested in triplicate. The implants were embedded in optimal cutting temperature compound (Sakura Seiki, Tokyo, Japan) and then cut into 8-mm-thick sections. Human SZ95 sebocytes were stained with human nuclear antigen antibody (Novus Biological, USA, 235-1) to evaluate the in vivo proliferation status. For Oil Red O staining, frozen DMA-PCL scaffold sections were fixed in 4% paraformaldehyde for 15 min, washed in PBS for 5 min, and stained for 10 min in freshly prepared Oil Red O solution. After washing with PBS for 15 min, the sections were counterstained with hematoxylin and mounted in 90% glycerol.
Statistical Analysis
A computer-based Sigma Gel System (SPSS Inc. , IL, USA) and the Image J program were used to analyze the integral optical density (IOD) of immunofluorescence images. A one-way analysis of variance followed by the Student t-test was used to determine the statistical significance (P-value) of the obtained data. All data presented in this study were reported as the mean ± SEM of three parallel studies. A P < 0.05 was considered statistically significant (*P < 0.05 and ***P < 0.001).
, IL, USA) and the Image J program were used to analyze the integral optical density (IOD) of immunofluorescence images. A one-way analysis of variance followed by the Student t-test was used to determine the statistical significance (P-value) of the obtained data. All data presented in this study were reported as the mean ± SEM of three parallel studies. A P < 0.05 was considered statistically significant (*P < 0.05 and ***P < 0.001).
Results
Characterizations of 3D-printed Scaffolds
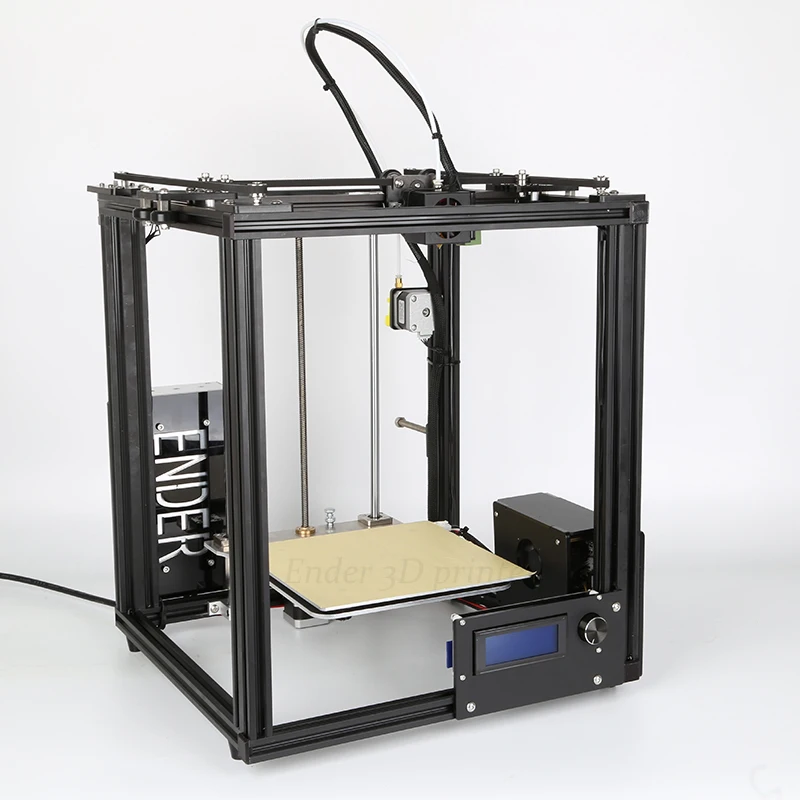
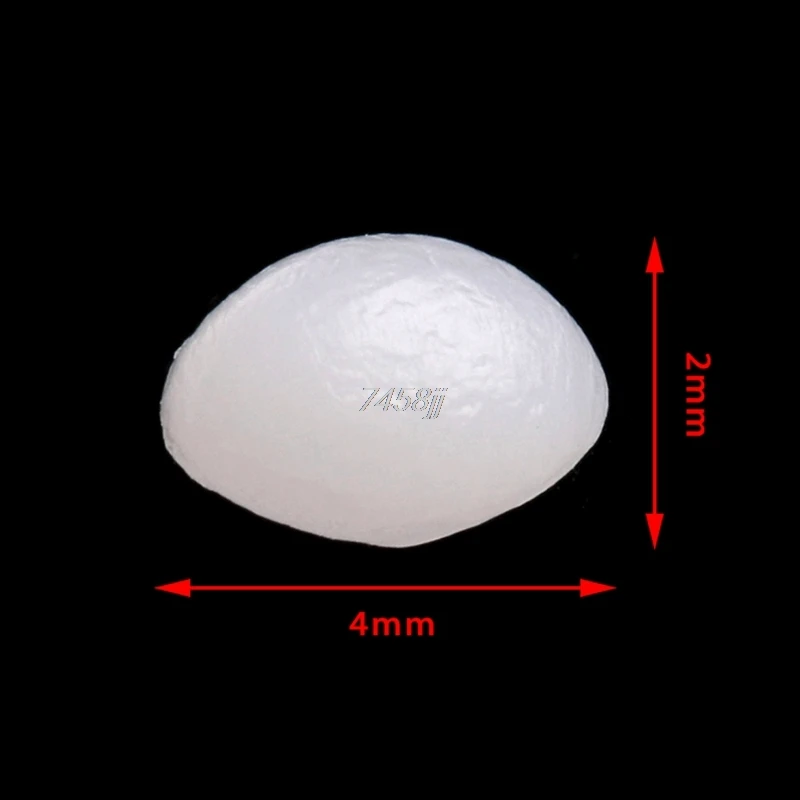
The parameters of this scaffold were based on the study by Dr. Michelle (Sun et al., 2015), who examined 10 healthy tarsal plate tissues. The 3D scaffolds measured 20 × 10 × 2 mm, with five central ducts (diameter, 1 mm) inside the scaffold (Figure 2A).
Figure 2. 3D-printed PCL scaffold and its detailed parameters. (A) Length, width and thickness (20 × 10 × 2 mm) of 3D-printed scaffolds were presented, with five central ducts (diameter, 1 mm) inside the scaffold. (B) Different printing pore sizes (200, 300, and 400 μm) were printed and shown. Central ducts were well-formed when the printing pore size was set to 200 or 300 μm. In contrast, when the pore size increased to 400 μm, the central ducts were not well formed due to the collapse of some areas. (C) Typical compressive stress-strain curves of different pore sizes of 3D-printed PCL scaffolds were demonstrated. Compressive modulus decreased when the pore size increased from 200 to 400 μm. (D) SEM images showed the top view and side view of 3D-printed scaffolds with a pore size of 200 μm. (E) Contact angle of water on PCL and DMA-PCL scaffolds. Photograph of the drop at the exact moment it reached the sample surface. The mean contact angle of water on PCL scaffolds was 93.3 ± 7.5°, while the water drop was immediately absorbed into the DMA-PCL scaffolds.
(B) Different printing pore sizes (200, 300, and 400 μm) were printed and shown. Central ducts were well-formed when the printing pore size was set to 200 or 300 μm. In contrast, when the pore size increased to 400 μm, the central ducts were not well formed due to the collapse of some areas. (C) Typical compressive stress-strain curves of different pore sizes of 3D-printed PCL scaffolds were demonstrated. Compressive modulus decreased when the pore size increased from 200 to 400 μm. (D) SEM images showed the top view and side view of 3D-printed scaffolds with a pore size of 200 μm. (E) Contact angle of water on PCL and DMA-PCL scaffolds. Photograph of the drop at the exact moment it reached the sample surface. The mean contact angle of water on PCL scaffolds was 93.3 ± 7.5°, while the water drop was immediately absorbed into the DMA-PCL scaffolds.
Printing pore size of 200, 300, and 400 μm were used (Figure 2B). When the pore size of the printing scaffold was set to 400 μm, the central ducts were not well-formed because the spacing of the central duct was too large. When the printing pore size was set to 200 or 300 μm, the shape of the central duct was well-formed. However, considering that the smaller the pore size, the larger the area of the cell for cell attachment, the more the cells proliferated in the duct. The compressive strength was measured to confirm the operability of the scaffolds in tissue engineering. Typical compressive stress-strain curves of different pore sizes of 3D-printed PCL scaffolds were shown (Figure 2C). The compressive modulus decreased slightly when the pore size increased from 200 to 400 μm. According to a previous study, the mean initial Young's modulus of the human tarsal plate was 0.14 MPa (Sun et al., 2015). The printing scaffolds (200 μm) presented a mean compressive modulus of 0.23 MPa, which was not particularly different from that of the human tarsal plate. Therefore, considering the structure and the strength of the scaffolds, 200 μm was chosen as the optimal printing parameter in this study.
When the printing pore size was set to 200 or 300 μm, the shape of the central duct was well-formed. However, considering that the smaller the pore size, the larger the area of the cell for cell attachment, the more the cells proliferated in the duct. The compressive strength was measured to confirm the operability of the scaffolds in tissue engineering. Typical compressive stress-strain curves of different pore sizes of 3D-printed PCL scaffolds were shown (Figure 2C). The compressive modulus decreased slightly when the pore size increased from 200 to 400 μm. According to a previous study, the mean initial Young's modulus of the human tarsal plate was 0.14 MPa (Sun et al., 2015). The printing scaffolds (200 μm) presented a mean compressive modulus of 0.23 MPa, which was not particularly different from that of the human tarsal plate. Therefore, considering the structure and the strength of the scaffolds, 200 μm was chosen as the optimal printing parameter in this study.
Figure 2D shows the SEM image of the scaffolds with a pore size of 200 μm. The diameter of the wire and the pore size were found to be the same, and the central duct was also well formed.
The diameter of the wire and the pore size were found to be the same, and the central duct was also well formed.
Material's wettability is an important parameter affecting the attachment, proliferation, migration, and viability of cells (Yao et al., 2017). The water contact angle was measured to determine the wettability of the scaffolds. The results revealed that the average water contact angle of the PCL scaffold was 93.3 ± 7.5°, resulting in hydrophobic surfaces (Figure 2E). The water drop in the DMA-PCL scaffolds was immediately absorbed into the scaffolds, indicating they were hydrophilic. However, because water droplets penetrated the surface too quickly for the camera to take a picture, the result was presented as a Supplementary Video 1.
Evaluation of DMA and Morphology of SZ95 Sebocytes on DMA–PCL Scaffolds
The partial composition of DMA was revealed using immunofluorescence staining of collagen I and fibronectin. As shown in Figure 3A, both matrix proteins of collagen I and fibronectin were immunostained with strong fluorescence intensity, indicating that the surface of the scaffold was covered with sufficient DMA. The ideal material scaffolds for tissue engineering ought to maintain a normal morphology and proliferation of the cells. The cells with a cobblestone-like morphology adhered to, and were spread on, the scaffolds 7 days after SZ95 sebocytes were seeded on DMA–PCL scaffolds (Figure 3B). Compared with the PCL scaffold, the cells on the DMA-PCL scaffold showed tighter cell connections and the cell morphology was more complete.
The ideal material scaffolds for tissue engineering ought to maintain a normal morphology and proliferation of the cells. The cells with a cobblestone-like morphology adhered to, and were spread on, the scaffolds 7 days after SZ95 sebocytes were seeded on DMA–PCL scaffolds (Figure 3B). Compared with the PCL scaffold, the cells on the DMA-PCL scaffold showed tighter cell connections and the cell morphology was more complete.
Figure 3. Evaluation of DMA and morphology of SZ95 sebocytes on PCL and DMA–PCL scaffolds. (A) Representative immunofluorescence staining images of collagen I and fibronectin. Both matrix proteins were immunostained with strong fluorescence intensity on DMA-PCL scaffolds (scale bar: 200 μm). Immunofluorescence was used to detect the expression of collagen I (green) and fibronectin (red) after hADSCs were seeded on the scaffold, before and after the decellularized matrix. After the decellularized matrix, the nucleus (4′,6-diamidino-2-phenylindole, DAPI, Blue) disappeared, and collagen I and fibronectin formed a uniform fiber network structure on the surface of the scaffold. (B) SEM images showed the morphology of SZ95 sebocytes 7 days after seeding on PCL and DMA-PCL scaffolds. Compared with the PCL scaffold, the cells on the DMA-PCL scaffold showed tighter cell connections, and the cell morphology was more complete.
(B) SEM images showed the morphology of SZ95 sebocytes 7 days after seeding on PCL and DMA-PCL scaffolds. Compared with the PCL scaffold, the cells on the DMA-PCL scaffold showed tighter cell connections, and the cell morphology was more complete.
Cell Viability and Proliferation
A Live/Dead assay kit was used to evaluate the biocompatibility of the scaffold. The biocompatibility of the scaffold was significantly increased by coating it with DMA, as shown in Figure 4A. Figure 4B shows statistics pertaining to Live/Dead results: the proportion of dead cells on PCL scaffolds was significantly higher than that on culture dish or DMA-coated culture dish, while the proportion of dead cells of DMA-PCL dropped significantly. The results of CCK-8 assay were shown in Figure 4C. It was observed that from day 3, the OD 450 value in the DMA group was significantly higher than that in the CTR group, which proved that DMA could promote the proliferation of sebocytes. Meanwhile, the OD 450 value in the PCL group was significantly lower than that in the other three groups on days 5 and 7, demonstrating that the simple PCL scaffolds were not conducive to cell proliferation. Compared with the PCL group, the OD 450 value in the DMA-PCL group significantly increased, confirming that DMA layer on the PCL scaffold promoted sebocyte proliferation as well.
Compared with the PCL group, the OD 450 value in the DMA-PCL group significantly increased, confirming that DMA layer on the PCL scaffold promoted sebocyte proliferation as well.
Figure 4. Cell viability and proliferation on DMA-PCL scaffolds. (A) Viable cells on the DMA–PCL scaffolds were evaluated using a Live/Dead staining assay. The live cells were stained green, and the dead cells were stained red (scale bar: 100 μm). (B) Statistical results of the Live/Dead staining assay showed that the proportion of dead cells on PCL scaffolds was significantly higher than that on the culture dish, while the proportion of dead cells of DMA-PCL dropped significantly. (C) Proliferation of SZ95 sebocytes on DMA-PCL scaffolds 0, 1, 3, 5, and 7 days after cell seeding were determined using a CCK-8 assay. DMA coated on the PCL scaffolds could significantly enhance the proliferation of sebocytes compared with the PCL group. Values are expressed as mean ± standard deviation. *P < 0.05 and ***P < 0.001. CTR, Culture dish; DMA, culture dish coated with DMA; PCL, poly-caprolactone scaffold; DMA-PCL, poly-caprolactone scaffold coated with DMA.
*P < 0.05 and ***P < 0.001. CTR, Culture dish; DMA, culture dish coated with DMA; PCL, poly-caprolactone scaffold; DMA-PCL, poly-caprolactone scaffold coated with DMA.
Lipid Synthesis on PCL and DMA–PCL Scaffolds
SZ95 sebocytes were cultured on PCL and DMA–PCL scaffolds for 7 days and then stained with F-actin and LipidTox. F-actin reflected the number of cells on scaffolds. Therefore, the relative IOD of Lipid/F-actin might partially reflect the cells' capacity to secrete lipids. Figure 5A showed the immunofluorescence of F-actin and lipid on PCL and DMA-PCL scaffold, and Figure 5B showed the statistical results of lipid synthesis. Figure 5C showed a 3D reconstruction of lipid on PCL scaffolds. SZ95 sebocytes seeded on DMA–PCL scaffolds secreted more lipids than those seeded on PCL scaffolds (P < 0.001), indicating that DMA could promote the differentiation of SZ95 sebocytes and contribute to the adipogenesis function.
Figure 5. Comparison of lipid droplet formation on PCL and DMA-PCL scaffolds. (A) Representative immunofluorescent staining images of F-actin and neutral lipid after cells were seeded 7 days in vitro on PCL and DMA-PCL scaffolds (scale bar: 500 μm). Significantly higher amounts of lipids were secreted by sebocytes on the DMA-PCL scaffolds compared with that on the PCL scaffolds. (B) Quantitative analysis of the relative IOD value of Lipid/F-actin. (C) 3D volume image of F-actin and lipid 7 days after cell seeding. The amount of lipids secreted by sebocytes on DMA-PCL scaffolds was obviously higher than that on PCL scaffolds (scale bar: 100 μm). ***P < 0.001.
Comparison of lipid droplet formation on PCL and DMA-PCL scaffolds. (A) Representative immunofluorescent staining images of F-actin and neutral lipid after cells were seeded 7 days in vitro on PCL and DMA-PCL scaffolds (scale bar: 500 μm). Significantly higher amounts of lipids were secreted by sebocytes on the DMA-PCL scaffolds compared with that on the PCL scaffolds. (B) Quantitative analysis of the relative IOD value of Lipid/F-actin. (C) 3D volume image of F-actin and lipid 7 days after cell seeding. The amount of lipids secreted by sebocytes on DMA-PCL scaffolds was obviously higher than that on PCL scaffolds (scale bar: 100 μm). ***P < 0.001.
Gene Expression
The in vitro lipid metabolism related gene expression assay (Figure 6A) clearly indicated that SZ95 sebocytes cultured on DMA-PCL scaffolds exhibited significantly higher expression of SREBP-1, FADS-2 and FAS genes after 7 days compared with cells cultured on PCL scaffolds and on culture wells. SREBP-1, FADS-2, PPARγ, and FAS expressed on 3D scaffolds were at least two-fold of those expressed on culture wells. Also, DMA-PCL had higher gene expression levels for SREBP-1, FADS-2, and FAS compared with PCL, indicating that, perhaps, DMA was crucial during the process of sebocyte lipid metabolism. Meanwhile, the expression levels of genes related to cell proliferation, adhesion, apoptosis, and inflammation were examined (Figure 6B). The expression level of Ki67 on 3D scaffolds were at least three-fold of that on culture wells. Although the expression levels of IL-6 and caspase-3 in cells on PCL scaffolds were higher compared with cells that were cultured on culture wells, the expression levels of these two genes significantly decreased after DMA was coated on the scaffolds. These results further demonstrated that DMA played an important role in promoting cell proliferation and exhibiting an anti-inflammatory effect at the RNA level.
SREBP-1, FADS-2, PPARγ, and FAS expressed on 3D scaffolds were at least two-fold of those expressed on culture wells. Also, DMA-PCL had higher gene expression levels for SREBP-1, FADS-2, and FAS compared with PCL, indicating that, perhaps, DMA was crucial during the process of sebocyte lipid metabolism. Meanwhile, the expression levels of genes related to cell proliferation, adhesion, apoptosis, and inflammation were examined (Figure 6B). The expression level of Ki67 on 3D scaffolds were at least three-fold of that on culture wells. Although the expression levels of IL-6 and caspase-3 in cells on PCL scaffolds were higher compared with cells that were cultured on culture wells, the expression levels of these two genes significantly decreased after DMA was coated on the scaffolds. These results further demonstrated that DMA played an important role in promoting cell proliferation and exhibiting an anti-inflammatory effect at the RNA level.
Figure 6. Gene expression of cells after seeding on PCL and DMA–PCL scaffolds for 7 days. (A) Expression levels of four lipid metabolism genes (SREBP-1, PPARγ, FADS-2, and FAS) were tested. Expressions levels of SREBP-1, FADS-2 and FAS were significantly higher in cells on DMA-PCL scaffolds indicating 3D-printed scaffolds better promoted lipid synthesis. (B) Expression levels of ZO-1 (a junction gene), Ki67 (a proliferation gene), Caspase-3 (an apoptosis-related gene), and IL-6 (an inflammation cytokine). The expression levels of ZO-1 and Ki67 were significantly higher in cells on DMA-PCL scaffolds compared with those in cells on CTR, indicating that DMA-PCL enhanced the adhesion and proliferation of sebocytes. Meanwhile, the expression levels of Caspase-3 and IL-6 were significantly lower on the DMA-PCL scaffold compared with the PCL scaffold, indicating that DMA coated on the PCL suppressed apoptosis and inflammation. SREBP-1, Sterol-Regulatory Element Binding Protein-1; PPARγ, Peroxisome Proliferator-Activated Receptor-γ; FADS-2, Fatty Acid Desaturase-2; FAS, Fatty Acid Synthase; ZO-1, Zona Occludens-1; IL-6, Interleukin-6.
(A) Expression levels of four lipid metabolism genes (SREBP-1, PPARγ, FADS-2, and FAS) were tested. Expressions levels of SREBP-1, FADS-2 and FAS were significantly higher in cells on DMA-PCL scaffolds indicating 3D-printed scaffolds better promoted lipid synthesis. (B) Expression levels of ZO-1 (a junction gene), Ki67 (a proliferation gene), Caspase-3 (an apoptosis-related gene), and IL-6 (an inflammation cytokine). The expression levels of ZO-1 and Ki67 were significantly higher in cells on DMA-PCL scaffolds compared with those in cells on CTR, indicating that DMA-PCL enhanced the adhesion and proliferation of sebocytes. Meanwhile, the expression levels of Caspase-3 and IL-6 were significantly lower on the DMA-PCL scaffold compared with the PCL scaffold, indicating that DMA coated on the PCL suppressed apoptosis and inflammation. SREBP-1, Sterol-Regulatory Element Binding Protein-1; PPARγ, Peroxisome Proliferator-Activated Receptor-γ; FADS-2, Fatty Acid Desaturase-2; FAS, Fatty Acid Synthase; ZO-1, Zona Occludens-1; IL-6, Interleukin-6. *P < 0.05, **P < 0.01, and ***P < 0.001.
*P < 0.05, **P < 0.01, and ***P < 0.001.
The in vivo status of SZ95 sebocytes was observed using immunohistochemistry 1 month after the scaffolds were embedded under the skin of nude mice. The sebocytes proliferated well in vivo after 1 month and formed a meibomian gland acinar-like structure with an intact epithelial layer (Figure 7A). At the same time, the scaffold with sebocytes was stained with Oil Red O. The scaffold was found to have wild lipid distribution, which proved that the sebocytes still secreted abundant lipids in vivo (Figure 7B).
Figure 7. In vivo status of SZ95 sebocytes. SZ95 sebocytes were seeded on DMA-PCL scaffolds, and the cell-scaffold complex was implanted into the nude mice subcutaneously. (A) Immunohistochemistry staining images for human nuclear antigen antibody. Sebocytes on the scaffolds still proliferated well in vivo after 1 month. A meibomian gland acinar like structure following the shape of the scaffold could be observed, together with an intact epithelial layer. (B) Oil Red O staining image. Amount of lipids were secreted by sebocytes inside the scaffolds in vivo (scale bar: 200 μm).
A meibomian gland acinar like structure following the shape of the scaffold could be observed, together with an intact epithelial layer. (B) Oil Red O staining image. Amount of lipids were secreted by sebocytes inside the scaffolds in vivo (scale bar: 200 μm).
Discussion
Tarsal plate tissue engineering has been difficult to achieve due to the complex structure and lipid secretion function of tarsal plate. In this study, 3D printing technology was used, for the first time, to fabricate tarsal plate scaffolds. Meanwhile, the surface of the scaffold was coated with DMA, which could be simply achieved by seeding autologous ADSCs. The as-prepared DMA–PCL scaffolds showed good biocompatibility and enhanced cell proliferation, differentiation, and anti-inflammation characteristics. Sebocytes seeded on DMA–PCL scaffolds secreted abundant lipids in vitro and proliferated well in vivo.
Few studies have been conducted to date in the field of tarsal plate engineering. In 2010, Dr. Jing Zhou used poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) to fabricate scaffolds and applied them to the rat eyelid tarsal plate defects. The morphology of the eyelids was repaired 2 months after implantation (Zhou et al., 2010). In 2018 Dai et al. established a poly(lactide-co-glycolide)/fibrin gel/bone marrow stem cells/ (lipofectamine/pDNA-transforming growth factor-β1) construct and applied it to a rabbit eyelid tarsal plate defect model. After 8 weeks, a new eyelid tarsal plate was generated (Dai et al., 2019). The shape of the eyelids was successfully regenerated in these studies, but the function of secretion of lipid by meibomian glands could not be restored.
In 2010, Dr. Jing Zhou used poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) to fabricate scaffolds and applied them to the rat eyelid tarsal plate defects. The morphology of the eyelids was repaired 2 months after implantation (Zhou et al., 2010). In 2018 Dai et al. established a poly(lactide-co-glycolide)/fibrin gel/bone marrow stem cells/ (lipofectamine/pDNA-transforming growth factor-β1) construct and applied it to a rabbit eyelid tarsal plate defect model. After 8 weeks, a new eyelid tarsal plate was generated (Dai et al., 2019). The shape of the eyelids was successfully regenerated in these studies, but the function of secretion of lipid by meibomian glands could not be restored.
Therefore, this study was conducted to mimic the structure of the tarsal plate, simultaneously focusing on the function of lipid secretion.
Among the synthetic polymers, PCL has attracted extensive attention because of its biocompatibility, low melting point (59–64°C), good solubility, and ease of use (Bahcecioglu et al.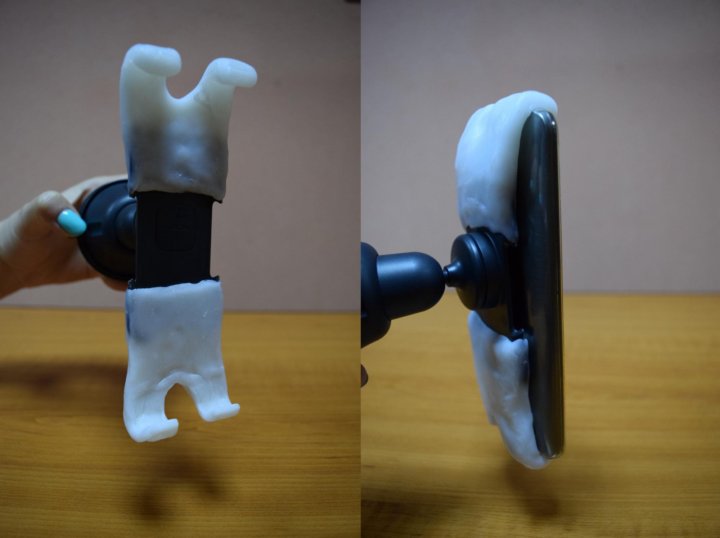 , 2019). It was widely applied in 3D printing systems involving selective laser sintering and FDM. Its widespread adoption could be partially attributed to its regulatory approval as a synthetic polymer for tissue repair and as a drug delivery vehicle by the US Food and Drug Administration (Jing et al., 2018). As a result, the scaffold printed with PCL was easier to apply in the clinic. In this study, PCL was used to fabricate a tarsal plate scaffold using the FDM technique. Compared with the traditional processes, such as particle/salt leaching (Esposito et al., 2013) and electrospinning (Baker and, 2007), FDM was a rapid prototyping technique that could produce a 3D scaffold with a complete control of geometric parameters, such as pore size, porosity, and pore interconnection size (Lantada and Morgado, 2012). As mentioned earlier, the shape of the eyelid defect caused by the tumor resection or trauma was irregular in many cases. 3D printing technology could accurately print the bionic tarsal plate according to the shape of the eyelid defect.
, 2019). It was widely applied in 3D printing systems involving selective laser sintering and FDM. Its widespread adoption could be partially attributed to its regulatory approval as a synthetic polymer for tissue repair and as a drug delivery vehicle by the US Food and Drug Administration (Jing et al., 2018). As a result, the scaffold printed with PCL was easier to apply in the clinic. In this study, PCL was used to fabricate a tarsal plate scaffold using the FDM technique. Compared with the traditional processes, such as particle/salt leaching (Esposito et al., 2013) and electrospinning (Baker and, 2007), FDM was a rapid prototyping technique that could produce a 3D scaffold with a complete control of geometric parameters, such as pore size, porosity, and pore interconnection size (Lantada and Morgado, 2012). As mentioned earlier, the shape of the eyelid defect caused by the tumor resection or trauma was irregular in many cases. 3D printing technology could accurately print the bionic tarsal plate according to the shape of the eyelid defect.:quality(80)/images.vogel.de/vogelonline/bdb/1605100/1605167/original.jpg) Meanwhile, according to clinical experience, tarsal plate regeneration is hard and more time-consuming. PCL degrades considerably more slowly compared with other aliphatic polyesters in vivo (Kweon et al., 2003), and the scaffold can maintain the initial mechanical support until adequate tissue ingrowth occurs (Zhang et al., 2017). Therefore, the relatively slow degradation of PCL could provide mechanical support for enough time.
Meanwhile, according to clinical experience, tarsal plate regeneration is hard and more time-consuming. PCL degrades considerably more slowly compared with other aliphatic polyesters in vivo (Kweon et al., 2003), and the scaffold can maintain the initial mechanical support until adequate tissue ingrowth occurs (Zhang et al., 2017). Therefore, the relatively slow degradation of PCL could provide mechanical support for enough time.
Of course, PCL also has some disadvantages, such as poor hydrophilicity and poor cell adhesion (Sun et al., 2006). Hence, most of the PCL-based tissue constructs fail to mimic the biochemical characteristics of native tissues. Extracellular matrix (ECM) can provide cells with a complex cellular environment and maintain an ideal structure for cells at both the tissue and organ levels (Wu et al., 2019). As reported, decellularized ECM has discrete influences on matrix assembly, cell proliferation, migration, signaling, and cellular feedbacks compared with planar protein-coated surfaces (Satyam et al.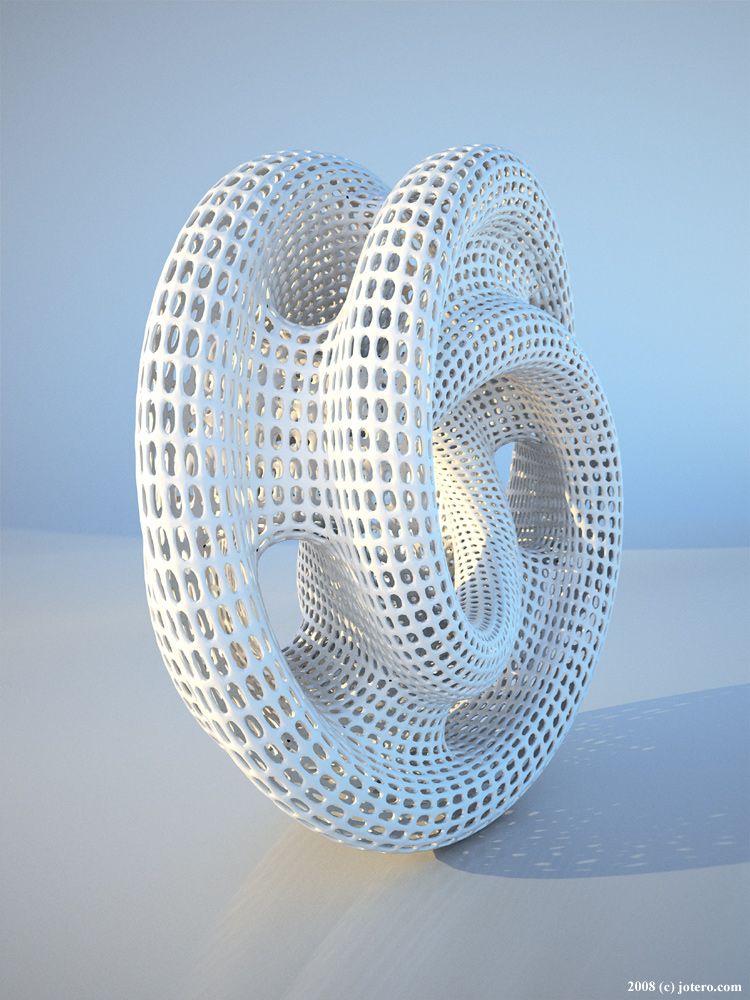 , 2020). Therefore, decellularized matrix technology has been used to improve the biocompatibility of PCL. For example Guilak et al., showed that decellularized ECM from biological tissues could significantly enhance wound healing, even in chronic-inflammation-prone diabetic rat models (Guilak et al., 2009). Ji et al. discovered that the DMA enhanced retinal progenitor cell proliferation and neuronal differentiation (Ji et al., 2018). In this study, autologous ADSCs were used for decellularization. On the one hand, the adipose tissue was abundant and superficial, which could be harvested without causing much damage to the body compared with other tissues. On the other hand, some relative researches on the function of DMA were already done in the lab. Thus, the DMA-PCL scaffolds could be easily achieved and the effect of DMA on the adhesion and proliferation of SZ95 sebocytes was investigated. The data visibly demonstrated that DMA enhanced cell adhesion and proliferation, probably due to the enhanced hydrophilicity of PCL scaffolds (Pattison et al.
, 2020). Therefore, decellularized matrix technology has been used to improve the biocompatibility of PCL. For example Guilak et al., showed that decellularized ECM from biological tissues could significantly enhance wound healing, even in chronic-inflammation-prone diabetic rat models (Guilak et al., 2009). Ji et al. discovered that the DMA enhanced retinal progenitor cell proliferation and neuronal differentiation (Ji et al., 2018). In this study, autologous ADSCs were used for decellularization. On the one hand, the adipose tissue was abundant and superficial, which could be harvested without causing much damage to the body compared with other tissues. On the other hand, some relative researches on the function of DMA were already done in the lab. Thus, the DMA-PCL scaffolds could be easily achieved and the effect of DMA on the adhesion and proliferation of SZ95 sebocytes was investigated. The data visibly demonstrated that DMA enhanced cell adhesion and proliferation, probably due to the enhanced hydrophilicity of PCL scaffolds (Pattison et al. , 2005; Stevens and George, 2005). The components of DMA, such as collagen and fibronectin, also played important roles in promoting cell proliferation and reduced inflammatory response (Kang et al., 2012). Sebocytes also secreted more lipids on DMA-PCL scaffolds, contributing to continuous lipid secretion to the ocular surface and help form the lipid layer of the tear film after transplantation. In the in vivo study, SZ95 sebocytes seeded on DMA-PCL scaffolds still proliferated well after 1 month under the skin of nude mice. This suggested that the scaffolds seeded with SZ95 sebocytes might be a promising biomaterial for the regeneration of tarsal plate defects.
, 2005; Stevens and George, 2005). The components of DMA, such as collagen and fibronectin, also played important roles in promoting cell proliferation and reduced inflammatory response (Kang et al., 2012). Sebocytes also secreted more lipids on DMA-PCL scaffolds, contributing to continuous lipid secretion to the ocular surface and help form the lipid layer of the tear film after transplantation. In the in vivo study, SZ95 sebocytes seeded on DMA-PCL scaffolds still proliferated well after 1 month under the skin of nude mice. This suggested that the scaffolds seeded with SZ95 sebocytes might be a promising biomaterial for the regeneration of tarsal plate defects.
SZ95 sebocytes were selected as promising seed cells in this study to restore the function of secreting lipids. The meibomian gland is a type of sebaceous gland located on the upper and lower tarsal plates with a tubular structure and a full secretory function. Meibocytes or sebocytes secrete lipids to the ocular or skin surface, and the lipid layer functions as a barrier (Chhadva et al.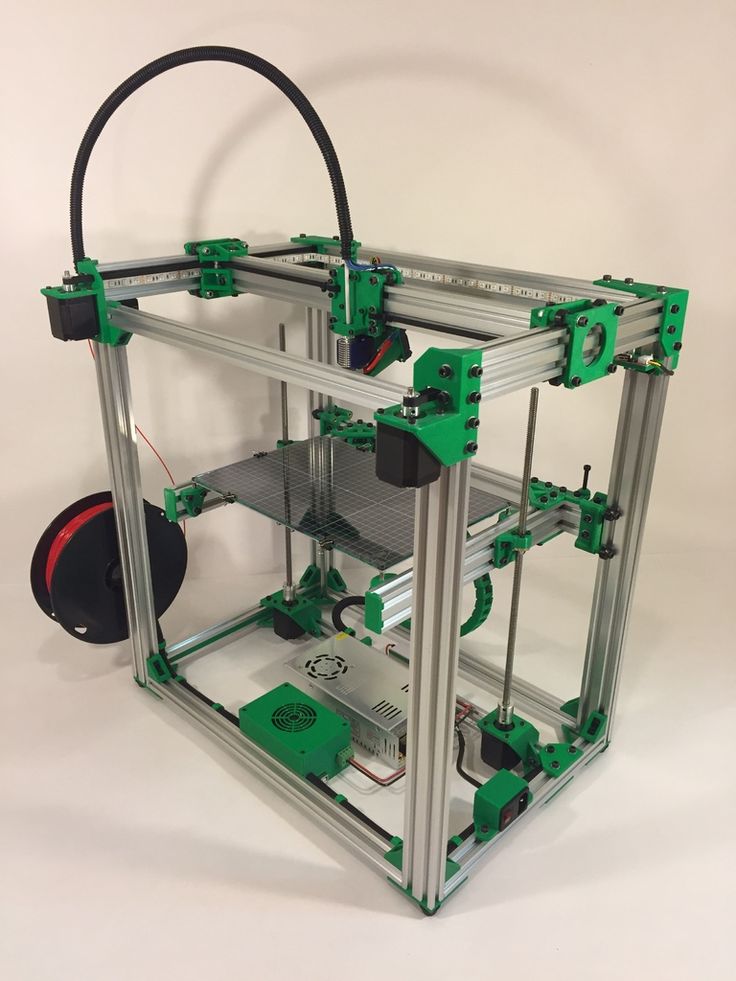 , 2017). The tarsal plate has poor regenerative capacity due to the lack of vascular tissues around it. Therefore, the source of meibocytes is limited. With the absence of meibomian glands, many patients with eyelid defects develop dry eye disease. In contrast, sebocytes are widely distributed throughout the body, secreting lipids, triglycerides and free fatty acids to protect the skin. As sebocytes have lipid secretion function and they are rich in autologous sources, they may serve as important seed cells for the replacement of meibocytes in the future.
, 2017). The tarsal plate has poor regenerative capacity due to the lack of vascular tissues around it. Therefore, the source of meibocytes is limited. With the absence of meibomian glands, many patients with eyelid defects develop dry eye disease. In contrast, sebocytes are widely distributed throughout the body, secreting lipids, triglycerides and free fatty acids to protect the skin. As sebocytes have lipid secretion function and they are rich in autologous sources, they may serve as important seed cells for the replacement of meibocytes in the future.
This study also had some limitations. First, the scaffolds were designed and printed according to the scale of the human tarsal plate. The thickness of the scaffold was relatively thick, making it difficult to repair the defect in situ in animals, such as rabbits or rats. Second, the sebocytes were seeded on the scaffolds after printing was completed; however, the accurate distribution of cells could not be guaranteed. The 3D bioprinting technology can be applied to print sebocytes and materials simultaneously in the future, for the accurate distribution of sebocytes in the acinar position and formation of a functioning acinus.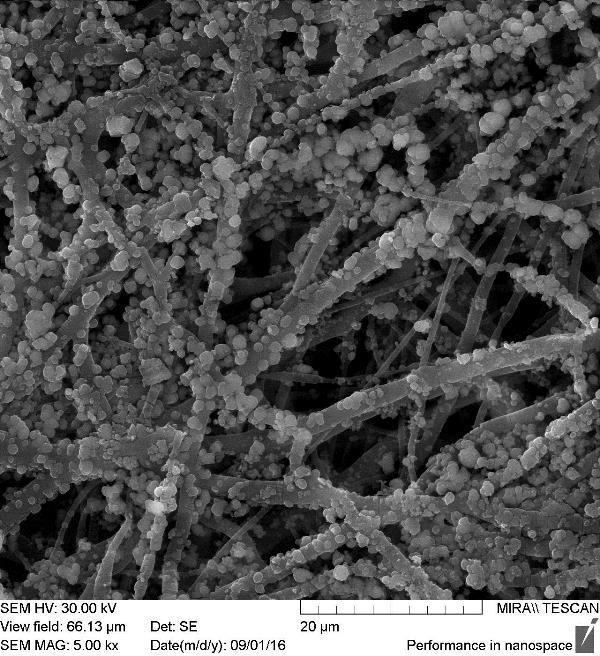
Conclusions
This study was novel in using the 3D printing technology to print PCL scaffolds that simulated the human tarsal plate. Subsequently, DMA was coated over the scaffolds through cell culturing and decellularization of hADSCs. DMA coated on the scaffolds made the surface more hydrophilic. The DMA-PCL scaffolds significantly enhanced sebocyte adhesion and proliferation. Moreover, sebocytes could differentiate well on the scaffold and exert the function of secreting lipids. Compared with scaffolds without DMA, the DMA-PCL scaffolds significantly suppressed inflammatory gene and apoptosis gene expression. At the same time, sebocytes climbed out of the scaffolds and formed a meibomian gland acinar-like structure and an epithelial layer after 1 month in vivo. Based on these results, it was believed that the 3D-printed scaffolds, combined with the decellularization technology, could be largely applied to tissue engineering. The 3D-printed DMA-PCL scaffolds along with sebocytes are promising substitutes in tarsal plate tissue engineering.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The animal study was reviewed and approved by Animal Ethics Committee of Shanghai Ninth People's Hospital affiliated to Shanghai Jiao Tong University School of Medicine.
Author Contributions
LC, HS, and YF designed the study and the experiments. LC and DY performed the experiments. NW and WZ contributed to the data analysis. QY participated in the design of the experiments and the revision of the final article. CY, HS, and YF revised the manuscript. CZ established the human sebaceous gland cell line SZ95. All authors discussed the results, reviewed the manuscript, and approved the final version of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (Grant nos. 81570812, 81770888), the Shanghai Municipal Education Commission: Gaofeng Clinical Medicine Grant Support (Grant no. 20161421), the Shanghai Municipal Science and Technology Commission: the Commercialization and Industrialization of Research Findings Project (Grant no. 17411963800), and the Science and Technology Commission of Shanghai (Grant no. 17DZ2260100).
20161421), the Shanghai Municipal Science and Technology Commission: the Commercialization and Industrialization of Research Findings Project (Grant no. 17411963800), and the Science and Technology Commission of Shanghai (Grant no. 17DZ2260100).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbioe.2020.00219/full#supplementary-material
Supplementary Video 1. Contact angle of DMA-PCL scaffolds.
References
Bae, S. W., Lee, K.-W., Park, J. H., Lee, J., Jung, C. R., Yu, J., et al. (2018). 3D bioprinted artificial trachea with epithelial cells and chondrogenic-differentiated bone marrow-derived mesenchymal stem cells. Int. J. Mol. Sci. 19:1624.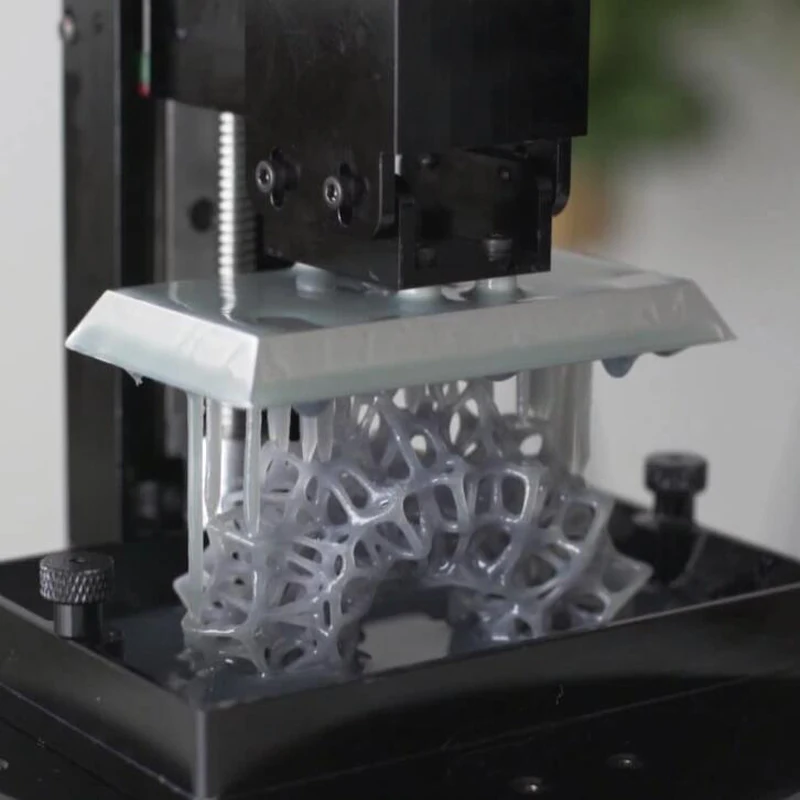 doi: 10.3390/ijms19061624
doi: 10.3390/ijms19061624
PubMed Abstract | CrossRef Full Text | Google Scholar
Bahcecioglu, G., Hasirci, N., Bilgen, B., and Hasirci, V. (2019). A 3D printed PCL/hydrogel construct with zone-specific biochemical composition mimicking that of the meniscus. Biofabrication 11:025002. doi: 10.1088/1758-5090/aaf707
PubMed Abstract | CrossRef Full Text | Google Scholar
Baker, B. M., and Mauck R. L. (2007). The effect of nanofiber alignment on the maturation of engineered meniscus constructs. Biomaterials 28, 1967–1977. doi: 10.1016/j.biomaterials.2007.01.004
PubMed Abstract | CrossRef Full Text | Google Scholar
Chen, J., Yan, C., Zhu, M., Yao, Q., Shao, C., Lu, W., et al. (2015). Electrospun nanofibrous SF/P(LLA-CL) membrane: a potential substratum for endothelial keratoplasty. Int. J. Nanomedicine 10, 3337–3350. doi: 10.2147/IJN.S77706
PubMed Abstract | CrossRef Full Text | Google Scholar
Chen, J. Q., Gu, J.-J., Peng, H. J., Huang, T., Chen, L. S., and Zhou, S.-Y. (2005). [The eyelid reconstruction in situ with allograft acellular dermal matrix]. Zhonghua Yan Ke Za Zhi 41, 409–413. doi: 10.3760/j:issn:0412-4081.2005.05.007
J., Huang, T., Chen, L. S., and Zhou, S.-Y. (2005). [The eyelid reconstruction in situ with allograft acellular dermal matrix]. Zhonghua Yan Ke Za Zhi 41, 409–413. doi: 10.3760/j:issn:0412-4081.2005.05.007
PubMed Abstract | CrossRef Full Text | Google Scholar
Chhadva, P., Goldhardt, R., and Galor, A. (2017). Meibomian gland disease: the role of gland dysfunction in dry eye disease. Ophthalmology 124, S20–S26. doi: 10.1016/j.ophtha.2017.05.031
PubMed Abstract | CrossRef Full Text | Google Scholar
Dai, Y., Jin, K., Feng, X., Ye, J., and Gao, C. (2019). Regeneration of different types of tissues depends on the interplay of stem cells-laden constructs and microenvironments in vivo. Mater. Sci. Eng. C Mater. Biol. Appl. 94, 938–948. doi: 10.1016/j.msec.2018.10.035
PubMed Abstract | CrossRef Full Text | Google Scholar
Esposito, A. R., Moda, M., de Melo Cattani, S. M., de Santana, G. M., Barbieri J. A., Munhoz M. M., et al. (2013). PLDLA/PCL-T scaffold for meniscus tissue engineering. Biores. Open Access 2, 138–147. doi: 10.1089/biores.2012.0293
PLDLA/PCL-T scaffold for meniscus tissue engineering. Biores. Open Access 2, 138–147. doi: 10.1089/biores.2012.0293
PubMed Abstract | CrossRef Full Text | Google Scholar
Foulks, G. N., and Bron, A. J. (2003). Meibomian gland dysfunction: a clinical scheme for description, diagnosis, classification, and grading. Ocul. Surf. 1, 107–126. doi: 10.1016/S1542-0124(12)70139-8
PubMed Abstract | CrossRef Full Text | Google Scholar
Goldberg, R. A., Joshi, A. R., McCann, J. D., and Shorr, N. (1999). Management of severe cicatricial entropion using shared mucosal grafts. Arch. Ophthalmol. 117, 1255–1259. doi: 10.1001/archopht.117.9.1255
PubMed Abstract | CrossRef Full Text | Google Scholar
Guilak, F., Cohen, D. M., Estes, B. T., Gimble, J. M., Liedtke W., Chen C. S., et al. (2009). Control of stem cell fate by physical interactions with the extracellular matrix. Cell Stem Cell 5, 17–26. doi: 10.1016/j.stem.2009.06.016
PubMed Abstract | CrossRef Full Text | Google Scholar
Hiller, T. , Berg, J., Elomaa, L., Rohrs, V., Ullah, I., Schaar, K., et al. (2018). Generation of a 3D liver model comprising human extracellular matrix in an alginate/gelatin-based bioink by extrusion bioprinting for infection and transduction studies. Int. J. Mol. Sci. 19:3129. doi: 10.3390/ijms19103129
, Berg, J., Elomaa, L., Rohrs, V., Ullah, I., Schaar, K., et al. (2018). Generation of a 3D liver model comprising human extracellular matrix in an alginate/gelatin-based bioink by extrusion bioprinting for infection and transduction studies. Int. J. Mol. Sci. 19:3129. doi: 10.3390/ijms19103129
PubMed Abstract | CrossRef Full Text | Google Scholar
Hwang, H. S., Parfitt, G. J., Brown, D. J., and Jester, J. V. (2017). Meibocyte differentiation and renewal: insights into novel mechanisms of meibomian gland dysfunction (MGD). Exp. Eye Res. 163, 37–45. doi: 10.1016/j.exer.2017.02.008
PubMed Abstract | CrossRef Full Text | Google Scholar
Isaacson, A., Swioklo, S., and Connon, C. J. (2018). 3D bioprinting of a corneal stroma equivalent. Exp. Eye Res. 173, 188–193. doi: 10.1016/j.exer.2018.05.010
PubMed Abstract | CrossRef Full Text | Google Scholar
Ji, J., Zhang, D., Wei, W., Shen, B., Zhang, Y., Wang, Y., et al. (2018). Decellularized matrix of adipose-derived mesenchymal stromal cells enhanced retinal progenitor cell proliferation via the Akt/Erk pathway and neuronal differentiation. Cytotherapy 20, 74–86. doi: 10.1016/j.jcyt.2017.08.019
Cytotherapy 20, 74–86. doi: 10.1016/j.jcyt.2017.08.019
PubMed Abstract | CrossRef Full Text | Google Scholar
Jing, L., Wang, X., Liu, H., Lu, Y., Bian, J., Sun, J., et al. (2018). Zein increases the cytoaffinity and biodegradability of scaffolds 3D-printed with zein and poly(epsilon-caprolactone) composite ink. ACS Appl. Mater. Interfaces 10, 18551–18559. doi: 10.1021/acsami.8b04344
PubMed Abstract | CrossRef Full Text | Google Scholar
Kang, Y., Kim, S., Bishop, J., Khademhosseini, A., and Yang, Y. (2012). The osteogenic differentiation of human bone marrow MSCs on HUVEC-derived ECM and beta-TCP scaffold. Biomaterials 33, 6998–7007. doi: 10.1016/j.biomaterials.2012.06.061
PubMed Abstract | CrossRef Full Text | Google Scholar
Kao, C. T., Lin, C. C., Chen, Y-W., Yeh, C-H., Fang, H. Y., Shie, M. Y., et al. (2015). Poly(dopamine) coating of 3D printed poly(lactic acid) scaffolds for bone tissue engineering. Mater. Sci. Eng. C Mater. Biol. Appl. 56, 165–173. doi: 10.1016/j.msec.2015.06.028
Biol. Appl. 56, 165–173. doi: 10.1016/j.msec.2015.06.028
PubMed Abstract | CrossRef Full Text | Google Scholar
Kweon, H., Yoo, M. K., Park, I. K., Kim, T. H., Lee, H. C., Lee, H.-S., et al. (2003). A novel degradable polycaprolactone networks for tissue engineering. Biomaterials 24, 801–808. doi: 10.1016/S0142-9612(02)00370-8
PubMed Abstract | CrossRef Full Text | Google Scholar
Lantada, A. D., and Morgado, P. L. (2012). Rapid prototyping for biomedical engineering: current capabilities and challenges. Annu. Rev. Biomed. Eng. 14, 73–96. doi: 10.1146/annurev-bioeng-071811-150112
PubMed Abstract | CrossRef Full Text | Google Scholar
Mannor, G. E., Mathers, W. D., Wolfley, D. E., and Martinez, J. A. (1994). Hard-palate mucosa graft in Stevens-Johnson syndrome. Am. J. Ophthalmol. 118, 786–791. doi: 10.1016/S0002-9394(14)72559-0
PubMed Abstract | CrossRef Full Text | Google Scholar
Nichols, K. K., Foulks, G. N., Bron, A.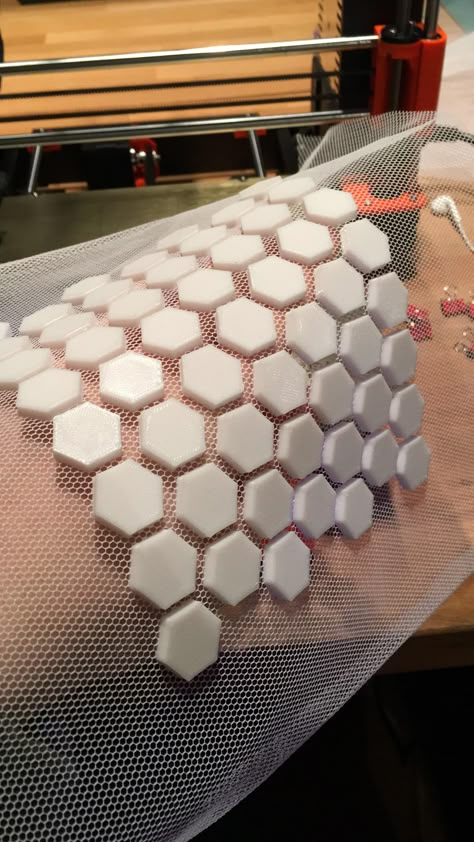 J., Glasgow, B. J., Dogru, M., Tsubota, K., et al. (2011). The international workshop on meibomian gland dysfunction: executive summary. Invest. Ophthalmol. Vis. Sci. 52, 1922–1929. doi: 10.1167/iovs.10-6997a
J., Glasgow, B. J., Dogru, M., Tsubota, K., et al. (2011). The international workshop on meibomian gland dysfunction: executive summary. Invest. Ophthalmol. Vis. Sci. 52, 1922–1929. doi: 10.1167/iovs.10-6997a
PubMed Abstract | CrossRef Full Text | Google Scholar
Pattison, M. A., Wurster, S., Webster, T. J., and Haberstroh, K. M. (2005). Three-dimensional, nano-structured PLGA scaffolds for bladder tissue replacement applications. Biomaterials 26, 2491–2500. doi: 10.1016/j.biomaterials.2004.07.011
PubMed Abstract | CrossRef Full Text | Google Scholar
Pfaffl, M. W. (2001). A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 29:e45. doi: 10.1093/nar/29.9.e45
PubMed Abstract | CrossRef Full Text | Google Scholar
Satyam, A., Tsokos, M. G., Tresback, J. S., Zeugolis, D. I., and Tsokos G. C. (2020). Cell-derived extracellular matrix-rich biomimetic substrate supports podocyte proliferation, differentiation, and maintenance of native phenotype. Adv. Funct. Mater. doi: 10.1002/adfm.201908752. [Epub ahead of print].
Adv. Funct. Mater. doi: 10.1002/adfm.201908752. [Epub ahead of print].
CrossRef Full Text | Google Scholar
Song, K., Wang, Z., Liu, R., Chen, G., and Liu, L. (2018). Microfabrication-based three-dimensional (3-D) extracellular matrix microenvironments for cancer and other diseases. Int. J. Mol. Sci. 19:935. doi: 10.3390/ijms19040935
PubMed Abstract | CrossRef Full Text | Google Scholar
Sorkio, A., Koch, L., Koivusalo, L., Deiwick, A., Miettinen, S., Chichkov, B., et al. (2018). Human stem cell based corneal tissue mimicking structures using laser-assisted 3D bioprinting and functional bioinks. Biomaterials 171, 57–71. doi: 10.1016/j.biomaterials.2018.04.034
PubMed Abstract | CrossRef Full Text | Google Scholar
Stevens, M. M., and George, J. H. (2005). Exploring and engineering the cell surface interface. Science 310, 1135–1138. doi: 10.1126/science.1106587
PubMed Abstract | CrossRef Full Text | Google Scholar
Sun, H. , Mei, L., Song, C., Cui, X., and Wang, P. (2006). The in vivo degradation, absorption and excretion of PCL-based implant. Biomaterials 27, 1735–1740. doi: 10.1016/j.biomaterials.2005.09.019
, Mei, L., Song, C., Cui, X., and Wang, P. (2006). The in vivo degradation, absorption and excretion of PCL-based implant. Biomaterials 27, 1735–1740. doi: 10.1016/j.biomaterials.2005.09.019
PubMed Abstract | CrossRef Full Text | Google Scholar
Sun, M. T., Pham, D. T., O'Connor, A. J., Wood, J., Casson, R., Selva, D., et al. (2015). The Biomechanics of eyelid tarsus tissue. J. Biomech. 48, 3455–3459. doi: 10.1016/j.jbiomech.2015.05.037
PubMed Abstract | CrossRef Full Text | Google Scholar
Tenzel, R. R., Miller, G. R., and Rubenzik, R. (1975). Cicatricial upper lid entropion treated with banked scleral graft. Arch. Ophthalmol. 93, 999–1000. doi: 10.1001/archopht.1975.01010020783008
PubMed Abstract | CrossRef Full Text | Google Scholar
Wu, Y. A., Chiu, Y. C., Lin, Y. H., Ho, C. C., Shie, M. Y., Chen, Y. W., et al. (2019). 3D-printed bioactive calcium silicate/poly-epsilon-caprolactone bioscaffolds modified with biomimetic extracellular matrices for bone regeneration. Int. J. Mol. Sci. 20:942. doi: 10.3390/ijms20040942
Int. J. Mol. Sci. 20:942. doi: 10.3390/ijms20040942
PubMed Abstract | CrossRef Full Text | Google Scholar
Yao, Q., Zhang, W., Hu, Y., Chen, J., Shao, C., Fan, X., et al. (2017). Electrospun collagen/poly(L-lactic acid-co-epsilon-caprolactone) scaffolds for conjunctival tissue engineering. Exp. Ther. Med. 14, 4141–4147. doi: 10.3892/etm.2017.5073
PubMed Abstract | CrossRef Full Text | Google Scholar
Yu, Y., Moncal, K. K., Li, J., Peng, W., Rivero, I., Martin J. A., et al. (2016). Three-dimensional bioprinting using self-assembling scalable scaffold-free “tissue strands” as a new bioink. Sci. Rep. 6:28714. doi: 10.1038/srep28714
PubMed Abstract | CrossRef Full Text | Google Scholar
Zhang, Z. Z., Wang, S.-J., Zhang, J.-Y., Jiang, W.-B., Huang, A.-B., Qi, Y.-S., et al. (2017). 3D-printed poly(epsilon-caprolactone) scaffold augmented with mesenchymal stem cells for total meniscal substitution: a 12- and 24-week animal study in a rabbit model. Am. J. Sports Med. 45, 1497–1511. doi: 10.1177/0363546517691513
Am. J. Sports Med. 45, 1497–1511. doi: 10.1177/0363546517691513
PubMed Abstract | CrossRef Full Text | Google Scholar
Zhou, J., Peng, S.-W., Wang, Y.-Y., Zheng, S.-B., Wang, Y., Chen, G.-Q., et al. (2010). The use of poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) scaffolds for tarsal repair in eyelid reconstruction in the rat. Biomaterials 31, 7512–7518. doi: 10.1016/j.biomaterials.2010.06.044
PubMed Abstract | CrossRef Full Text | Google Scholar
Zouboulis, C. C., Seltmann, H., Neitzel, H., and Orfanos, C. E. (1999). Establishment and characterization of an immortalized human sebaceous gland cell line (SZ95). J Invest Dermatol. 113, 1011–1020. doi: 10.1046/j.1523-1747.1999.00771.x
PubMed Abstract | CrossRef Full Text | Google Scholar
FDM/FFF Consumables
FFF technology has many advantages, including the relative simplicity of the design of printers and the affordability of both devices and consumables. Moreover, the range of materials is perhaps the widest among all available technologies. As a rule, thermoplastics are used for printing, but there are exceptions - composite materials containing various additives, but based, again, on thermoplastics. In this section, we will try to talk about the most widely used materials in more detail, starting with the most popular types.
Moreover, the range of materials is perhaps the widest among all available technologies. As a rule, thermoplastics are used for printing, but there are exceptions - composite materials containing various additives, but based, again, on thermoplastics. In this section, we will try to talk about the most widely used materials in more detail, starting with the most popular types.
- 1 Polylactide (PLA, PLA)
- 2 Acrylonitrile butadiene styrene (ABS)
- 3 Polyvinyl alcohol (PVA)
- 4 Nylon
- 5 Polycarbonate (PC)
- 6 High density polyethylene (HDPE)
- 7 Polypropylene (PP, PP)
- 8 Polycaprolactone (PCL)
- 9 Polyphenylsulfone (PPSU)
- 10 Polymethyl methacrylate (Acrylic, plexiglass, acrylic, PMMA)
- 11 Polyethylene terephthalate (PET, PET)
- 12 High impact polystyrene (HIPS)
- 13 Wood Simulators (LAYWOO-D3, BambooFill)
- 14 Sandstone Simulators (Laybrick)
- 15 Metal Simulators (BronzeFill)
Polylactide (PLA, PLA)
Polylactide is one of the most widely used thermoplastics due to several factors. Let's start with the fact that PLA is known for its environmental friendliness. This material is a lactic acid polymer, which makes PLA a completely biodegradable material. The raw materials for the production of polylactide are corn and sugar cane. At the same time, the environmental friendliness of polylactide causes its fragility. Plastic easily absorbs water and is relatively soft. As a rule, PLA models are not intended for functional use, but serve as designer models, souvenirs and toys. Few practical industrial applications include the production of food packaging, drug containers and surgical sutures, as well as use in bearings that do not carry high mechanical loads (for example, in modeling), which is possible due to the material's excellent slip coefficient.
Let's start with the fact that PLA is known for its environmental friendliness. This material is a lactic acid polymer, which makes PLA a completely biodegradable material. The raw materials for the production of polylactide are corn and sugar cane. At the same time, the environmental friendliness of polylactide causes its fragility. Plastic easily absorbs water and is relatively soft. As a rule, PLA models are not intended for functional use, but serve as designer models, souvenirs and toys. Few practical industrial applications include the production of food packaging, drug containers and surgical sutures, as well as use in bearings that do not carry high mechanical loads (for example, in modeling), which is possible due to the material's excellent slip coefficient.
One of the most important factors for 3D printing applications is the low melting temperature of only 170-180°C, which contributes to relatively low power consumption and the use of inexpensive brass and aluminum nozzles. As a rule, extrusion is carried out at 160-170°C. At the same time, PLA solidifies quite slowly (glass transition temperature is about 50°C), which should be taken into account when choosing a 3D printer. The best option is a device with an open case, a heated work platform (to avoid deformation of large models) and, preferably, additional fans to cool the fresh layers of the model.
As a rule, extrusion is carried out at 160-170°C. At the same time, PLA solidifies quite slowly (glass transition temperature is about 50°C), which should be taken into account when choosing a 3D printer. The best option is a device with an open case, a heated work platform (to avoid deformation of large models) and, preferably, additional fans to cool the fresh layers of the model.
PLA has low shrinkage, i.e. loss of volume on cooling, which helps prevent warping. However, shrinkage has a cumulative effect as the dimensions of printed models increase. In the latter case, the build platform may need to be heated to evenly cool the printed objects.
The cost of PLA is relatively low, which adds to the popularity of this material.
Acrylonitrile Butadiene Styrene (ABS)
ABS is perhaps the most popular thermoplastic used in 3D printing, but not the most common. This contradiction is explained by certain technical difficulties that arise when printing ABS. The desire of craftsmen to use ABS is determined by the excellent mechanical properties, durability and low cost of this material. In the industry, ABS plastic is already widely used: the production of car parts, cases of various devices, containers, souvenirs, various household accessories, etc.
The desire of craftsmen to use ABS is determined by the excellent mechanical properties, durability and low cost of this material. In the industry, ABS plastic is already widely used: the production of car parts, cases of various devices, containers, souvenirs, various household accessories, etc.
ABS plastic is resistant to moisture, acids and oil, has a fairly high temperature resistance - from 90°C to 110°C. Unfortunately, some types of material are destroyed by direct sunlight, which somewhat limits the application. At the same time, ABS plastic is easy to paint, which allows you to apply protective coatings on non-mechanical elements.
Despite a relatively high glass transition temperature of around 100°C, ABS has a relatively low melting point. Actually, due to the amorphous nature of the material, ABS does not have a melting point, as such, but 180 ° C is considered an acceptable temperature for extrusion, which is on the same level as the above-described PLA. The lower temperature spread between extrusion and glass transition allows ABS to cure faster than PLA.
The lower temperature spread between extrusion and glass transition allows ABS to cure faster than PLA.
The main disadvantage of ABS plastic can be considered a high degree of shrinkage during cooling - the material can lose up to 0.8% of its volume. This effect can lead to significant deformations of the model, twisting of the first layers and cracking. To combat these unpleasant phenomena, two main solutions are used. First, heated work platforms are used to help reduce the temperature gradient between the lower and upper layers of the model. Secondly, ABS 3D printers often use closed housings and control of the background temperature of the working chamber. This makes it possible to maintain the temperature of the applied layers at a level just below the glass transition threshold, reducing the degree of shrinkage. Full cooling is carried out after receiving the finished model.
The relatively low stickiness of ABS may require additional bonding aids such as adhesive tape, polyimide film, or applying an acetone solution of the ABS to the platform just prior to printing. For more information on how to avoid warping, see How to Avoid Warping 3D Printed Models.
For more information on how to avoid warping, see How to Avoid Warping 3D Printed Models.
While ABS is not a health hazard at room temperature, heated plastic releases acrylonitrile fumes, a poisonous compound that can irritate mucous membranes and cause poisoning. Although the amount of Acrylonitrate produced in small scale printing is negligible, it is recommended that you print in a well ventilated area or use an exhaust hood. It is not recommended to use ABS plastic for the production of food containers and utensils (especially for storing hot food or alcoholic beverages) or toys for small children.
The good solubility of ABS in acetone is very useful as it allows large models to be produced piece by piece and glued together, greatly expanding the capabilities of inexpensive desktop printers.
Polyvinyl alcohol (PVA)
Polyvinyl alcohol is a material with unique properties and special applications. The main feature of PVA is its water solubility. 3D printers equipped with dual extruders have the ability to print models with PVA support structures. Upon completion of printing, the supports can be dissolved in water, leaving a finished model that does not require mechanical or chemical roughening. Similarly, PVA can be used to create water-soluble master patterns for molds and molds themselves.
The main feature of PVA is its water solubility. 3D printers equipped with dual extruders have the ability to print models with PVA support structures. Upon completion of printing, the supports can be dissolved in water, leaving a finished model that does not require mechanical or chemical roughening. Similarly, PVA can be used to create water-soluble master patterns for molds and molds themselves.
The mechanical properties of PVA are quite interesting. At low humidity, plastic has high tensile strength. With increasing humidity, strength decreases, but elasticity increases. The extrusion temperature is 160-175°C, which allows the use of PVA in printers designed for printing with ABS and PLA plastics.
Since the material easily absorbs moisture, it is recommended to store PVA plastic in dry packaging and, if necessary, dry before use. Drying can be done in a pottery kiln or an ordinary oven. As a rule, drying of standard coils takes 6-8 hours at a temperature of 60-80°C. Exceeding 220°C will cause the plastic to decompose, which should be taken into account when printing.
Exceeding 220°C will cause the plastic to decompose, which should be taken into account when printing.
Nylon
Nylon is attractive due to its high wear resistance and low coefficient of friction. Thus, nylon is often used to coat friction parts, which improves their performance and often allows them to function without lubrication. Following the widespread use of nylon in industry, additive manufacturing has also become interested in the material. Attempts to print with nylon have been made almost since the early days of FDM/FFF technology.
In reality, there are several types of nylon produced by different methods and with slightly different characteristics. The most famous is nylon-66, created by the American company DuPont in 1935. The second most popular option is nylon-6, developed by BASF to circumvent the DuPont patent. These two options are very similar. In terms of 3D printing, the main difference is the melting point: Nylon-6 melts at 220°C, while Nylon-66 melts at 265°C.
Many hobbyists prefer to use commercially available nylon threads such as trimmer wire. The diameter of such materials often corresponds to the diameter of standard FFF materials, which makes their use tempting. At the same time, these products are usually not pure nylon. In the case of trimmer rods, the material consists of nylon and fiberglass for an optimal combination of flexibility and rigidity.
Fiberglass has a high melting point and therefore printing with these materials is prone to high nozzle wear and plugging.
Recently there have been attempts to commercially develop nylon-based printing materials specifically for FDM/FFF applications, including Nylon-PA6 and Taulman 680. These grades are extrudable at 230-260°C.
Since nylon easily absorbs moisture, store consumables in vacuum packaging or at least in a container with water-absorbing materials. A sign of excessively damp media will be steam escaping from the nozzle during printing, which is not dangerous, but may degrade the quality of the model.
When printing with nylon, it is not recommended to use a polyimide desktop coating as the two materials fuse together. As a coating, you can use adhesive tape with wax impregnation (masking tape). The use of a heated bed will help reduce the possibility of deformation of the model, similar to printing with ABS plastic. Due to the low coefficient of friction of nylon, extruders with studded feeders should be used.
The nylon layers have excellent adhesion, minimizing the chance of delamination.
Nylon is difficult to bond, making it difficult to print large multi-piece models. Alternatively, fusion of parts is possible.
Because nylon can release toxic fumes when heated, we recommend that you print in a well-ventilated area or use an exhaust fan.
Polycarbonate (PC)
Polycarbonates are attractive due to their high strength and toughness, as well as resistance to high and low temperatures.
The potential health risk of printing is worth noting: the toxic and potentially carcinogenic compound bisphenol A is often used as a raw material. .
The extrusion temperature depends on the printing speed to avoid cracking, but the minimum temperature at 30mm/s can be considered as 265°C. When printing, the use of polyimide film is recommended for better adhesion to the desktop surface. The high susceptibility of polycarbonate to deformation requires the use of a heated platform and, if possible, a closed housing with heating of the working chamber.
Polycarbonate is highly hygroscopic (easily absorbs moisture), which requires storage in dry conditions to avoid the formation of bubbles in the applied layers. For extended printing in humid climates, even the print spool may need to be stored in a moisture-proof container.
High Density Polyethylene (HDPE)
Arguably the most common plastic in the world, polyethylene is relatively rare among 3D printed materials.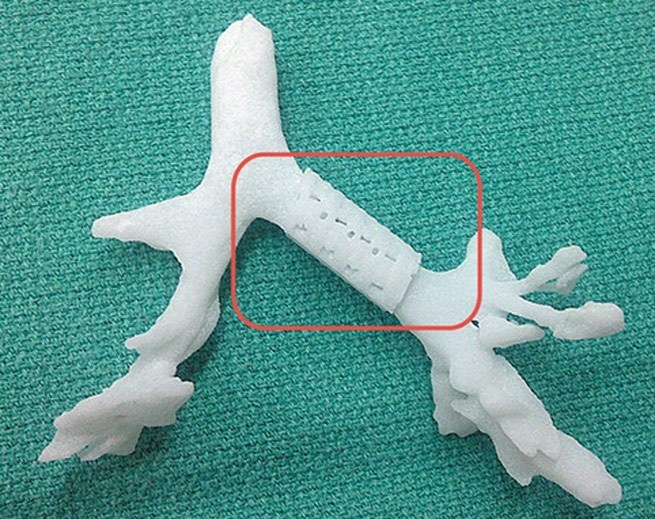 The reason for this is the difficulty in layer-by-layer manufacturing of models.
The reason for this is the difficulty in layer-by-layer manufacturing of models.
Polyethylene melts easily (130-145°C) and hardens quickly (100-120°C), as a result of which the applied layers often do not have time to set. In addition, polyethylene is characterized by high shrinkage, which provokes the twisting of the first layers and the deformation of the models as a whole during uneven solidification. Printing with polyethylene requires the use of a heated platform and a working chamber with accurate temperature control to slow down the cooling of the applied layers. In addition, you will need to print at high speed.
Difficulties in use are more than offset by the cheapness and availability of this material. Recently, several devices have been developed for processing plastic waste from HDPE (bottles, food packaging, etc.) into standard filaments for printing on FDM/FFF printers. Examples are FilaBot and RecycleBot. Due to the simplicity of design, RecycleBot devices are often assembled by 3D craftsmen.
Melting polyethylene releases harmful vapors, so it is recommended to print in well-ventilated areas.
Polypropylene (PP, PP)
Polypropylene is a widely used plastic used in the manufacture of packaging materials, utensils, syringes, pipes, etc. The material has a low specific gravity, is non-toxic, has good chemical resistance, is resistant to moisture and wear, and cheap enough. Among the disadvantages of polypropylene, one can note the vulnerability to temperatures below -5 ° C and to direct sunlight.
The main difficulty in printing with polypropylene is the high shrinkage of the material during cooling - up to 2.4%. For comparison, the shrinkage of the popular but already problematic ABS plastic reaches 0.8%. Although polypropylene adheres well to cold surfaces, it is recommended to print on a heated platform to avoid deformation of models. The minimum recommended extrusion temperature is 220°C.
Polypropylene printing filaments are sold by Orbi-Tech, German RepRap, Qingdao TSD Plastic. Stratasys has developed a polypropylene simulant optimized for 3D printing called Endur.
Polycaprolactone (PCL)
Polycaprolactone (aka Hand Moldable Plastic, Mold-Your-Own Grips, InstaMorph, Shapelock, Friendly Plastic, Polymorph, Polymorphus, Ecoformax) - biodegradable polyester, characterized by an extremely low melting point of about 60 ° C . In practice, this property creates certain problems in 3D printing, since not all 3D printers can be configured to work at such low temperatures. Heating polycaprolactone to the usual extrusion temperatures (about 200°C) causes a loss of mechanical properties and may lead to breakage of the extruder.
Polycaprolactone is non-toxic, making it suitable for use in the medical industry, and biodegradable. When ingested, polycaprolactone breaks down, which makes printing with this material safe.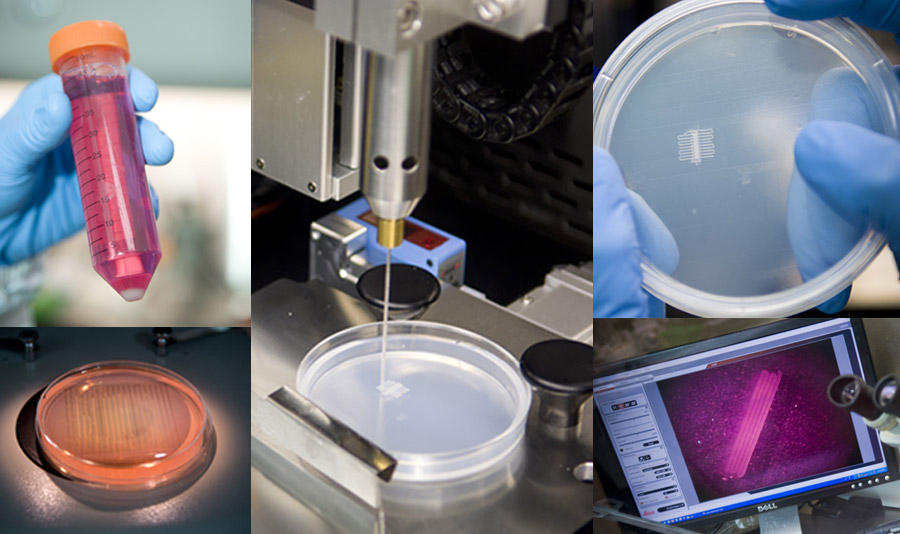 Due to the low melting point, there is no danger of burns when touching fresh models. The high plasticity of the material makes it possible to reuse.
Due to the low melting point, there is no danger of burns when touching fresh models. The high plasticity of the material makes it possible to reuse.
Polycaprolactone is of little use for creating functional mechanical models due to its viscosity (glass transition temperature is -60°C) and low heat resistance (melting point is 60°C). On the other hand, this material is perfect for the production of mock-ups and food containers.
The material sticks easily to the surface of even a cold working table and is easy to paint.
Polyphenylsulfone (PPSU)
Polyphenylsulfone is a high strength thermoplastic used extensively in the aviation industry. The material has excellent chemical and thermal stability and practically does not burn. Polyphenylsulfone is biologically inert, which makes it possible to use this material for the production of tableware and food containers. Operating temperature range is -50°С - 180°С.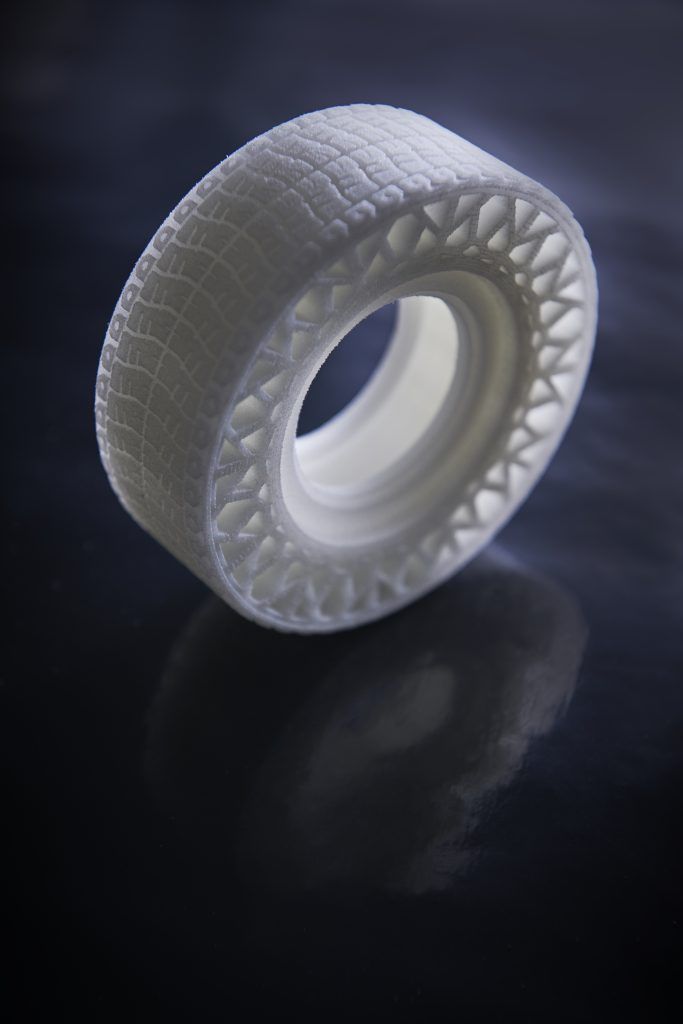 Plastic is resistant to solvents and fuels and lubricants.
Plastic is resistant to solvents and fuels and lubricants.
For all its merits, polyphenylsulfone is rarely used in 3D printing due to its high melting point, reaching 370°C. Such extrusion temperatures are beyond the power of most desktop printers, although printing is theoretically possible using ceramic nozzles. Currently, the only active user of the material is Stratasys, which offers industrial Fortus installations.
Polymethyl methacrylate (Acrylic, plexiglass, acrylic, PMMA)
Polymethyl methacrylate is a well-known organic glass. The material is durable, moisture resistant, environmentally friendly, easy to glue, plastic enough and resistant to direct sunlight.
Unfortunately, acrylic is not suitable for FDM/FFF printing for a number of reasons. Acrylic is poorly stored in the form of spools of thread, as constant mechanical stress leads to the gradual destruction of the material. To avoid bubbles, the print resolution must be high, with a precision almost impossible for home printers. Acrylic's rapid curing requires strict environmental control of the working chamber and high print speeds. Again, the print speeds of FDM/FFF printers are inversely related to print resolution, which exacerbates the problem.
Acrylic's rapid curing requires strict environmental control of the working chamber and high print speeds. Again, the print speeds of FDM/FFF printers are inversely related to print resolution, which exacerbates the problem.
However, attempts are being made to print with acrylic, and some of them are producing relatively positive results. However, when creating sufficiently strong models, it is not yet possible to avoid the formation of bubbles and achieve the usual transparency of the material. At the moment, the best results with acrylic are shown by another printing technology - multi-jet modeling (MJM) from 3D Systems. In this case, a photopolymer version of acrylic is used. Stratasys has also made significant progress using its own photopolymer acrylic simulant VeroClear on Objet Eden printers. It is hoped that the high demand for acrylic will lead to the emergence of composite materials based on polymethyl methacrylate, designed specifically for FDM/FFF printing.
Polyethylene terephthalate (PET, PET)
Polyethylene terephthalate - this complex name hides a material used for the production of plastic bottles and other food and medical containers.
The material has a high chemical resistance to acids, alkalis and organic solvents. The physical properties of PET are also impressive with high wear resistance and tolerance to a wide temperature range from -40°C to 75°C. Among other things, the material is easily machined.
Printing with PET is somewhat problematic due to the relatively high melting point of up to 260°C and significant cooling shrinkage of up to 2%. Using PET as a consumable requires approximately the same conditions as printing with ABS.
Achieving transparency of models requires rapid cooling to pass the glass transition threshold of 70°C - 80°C.
The material has become the focus of interest for 3D craftsmen using used containers as raw materials for the home production of 3D printing consumables. Recycling devices such as FilaBot or RecycleBot are used to make threads.
High impact polystyrene (HIPS)
High impact polystyrene is widely used in industry for the production of various household products, building materials, disposable tableware, toys, medical instruments, etc.
When 3D printed, polystyrene exhibits physical properties very similar to the popular ABS plastic, making it an increasingly popular material among 3D crafters. The most attractive feature of polystyrene is the difference from ABS in terms of chemical properties: polystyrene is quite easily amenable to the organic solvent Limonen. Since Limonene has no effect on ABS plastic, it is possible to use polystyrene as a material for building soluble support structures, which is extremely useful when building complex, interlaced models with internal supports. Compared to the convenient, water-soluble polyvinyl alcohol (PVA) plastic, polystyrene compares favorably with relatively low cost and resistance to humid climates that make PVA difficult to work with.
It's worth bearing in mind that some ABS manufacturers mix slightly cheaper polystyrene into their consumables. Accordingly, models made from such materials can be dissolved in Limonene along with supporting structures.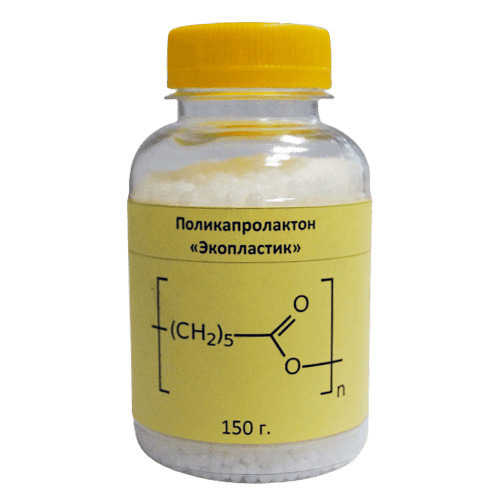
When polystyrene is heated to extrusion temperature, toxic fumes can be released, so printing in a well-ventilated area is recommended.
Wood simulants (LAYWOO-D3, BambooFill)
LAYWOO-D3 is a recent development for printing wood-like models. The material consists of 40% natural wood chips of microscopic size and 60% binder polymer. The LAYWOO-D3 is very easy to handle, being virtually warp-free and does not require the use of a heated platform. According to the manufacturers, the polymer is non-toxic and completely safe.
The unique material properties allow for different visual results when printing with different nozzle temperatures. The operating temperature range is 180°C-250°C. As the extrusion temperature increases, the shade of the material becomes progressively darker, allowing it to simulate different types of wood or annual rings.
Finished models are excellent for mechanical processing - grinding, drilling, etc.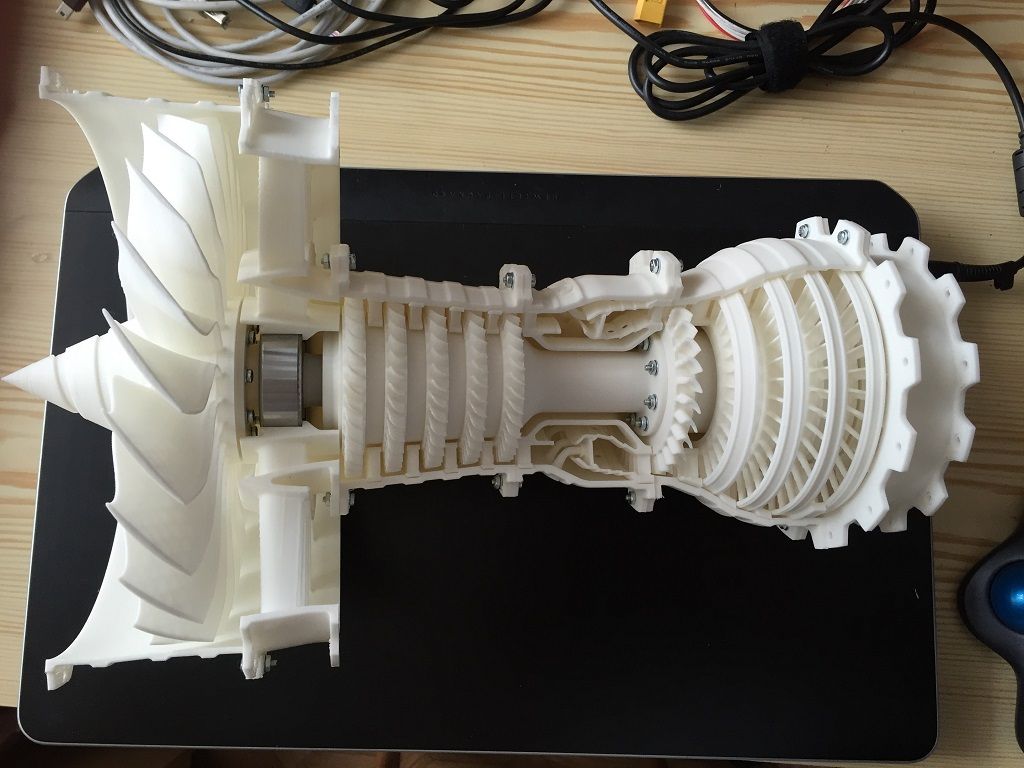 In addition, the products are easily painted, and unpainted models even have a characteristic woody smell.
In addition, the products are easily painted, and unpainted models even have a characteristic woody smell.
Unfortunately, the cost of the material is almost four times higher than the price of popular materials such as PLA and ABS plastics. As popularity is projected to grow, the material should become more accessible.
Alternative materials are currently being developed and tested, such as BambooFill from the Dutch company ColorFabb.
Sandstone simulants (Laybrick)
Composite material from the inventor Kai Parti, responsible for the revolutionary wood simulant LAYWOO-D3. This time, Kai set his sights on sandstone imitation, using a tried and tested method of mixing a binder with a filler, in this case mineral.
Laybrick allows you to produce objects with different surface textures. At low extrusion temperatures of the order of 165°C-190°C, the finished products have a smooth surface. Increasing the printing temperature makes the material rougher, up to a high degree of resemblance to natural sandstone at extrusion temperatures above 210°C.
The material is easy to work with no need to heat the work platform, does not show significant deformation when shrinking and does not produce toxic fumes when heated. The only drawback can be considered a rather high cost of the material, which is largely due to limited production.
Metal Simulators (BronzeFill)
Metals have attracted additive manufacturing enthusiasts since the early days of 3D printing technology. Unfortunately, printing with pure metals and alloys causes a lot of difficulties that are insurmountable for most 3D printing methods. Fully functional metal products can only be produced using technologies such as SLS, DLMS or EBM, which require the use of industrial plants that cost hundreds of thousands of dollars. At the same time, metal imitators are successfully used in 3D inkjet printing (3DP), where products are formed from metal powders, the particles of which are held together by an applied binder material.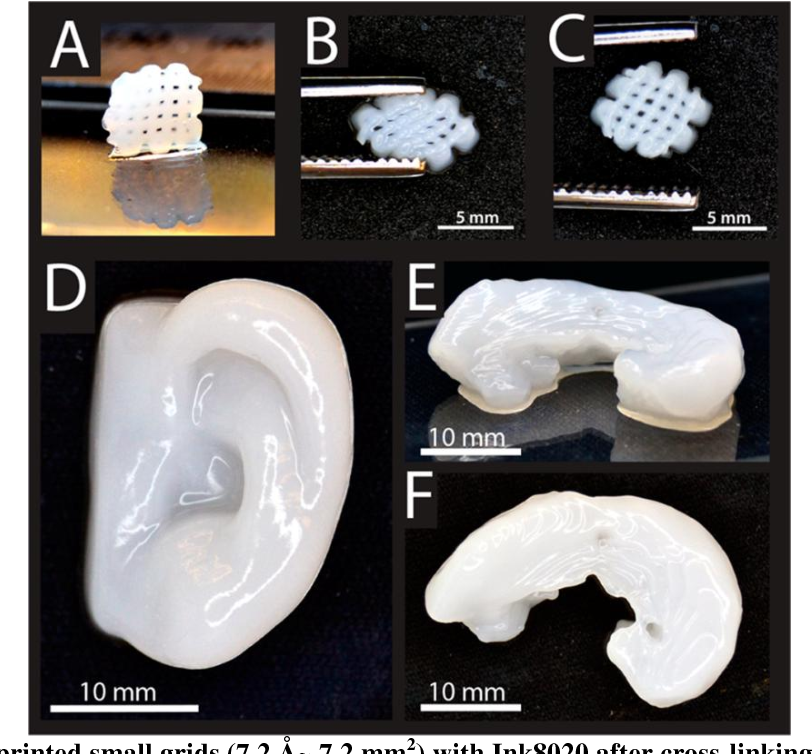 In FDM/FFF printing, metal simulants are just emerging.
In FDM/FFF printing, metal simulants are just emerging.
An interesting example is BronzeFill, which is actually a transparent PLA plastic filled with bronze microparticles. The material, currently in beta testing, must prove suitability for use in any printer designed to work with polylactide.
Finished products are easy to polish, achieving a high external resemblance to all-metal products. At the same time, it should be taken into account that the binding element of the material is thermoplastic, with appropriate mechanical and temperature limitations.
Go to the main page of the 3D Printing Encyclopedia
3D printing with low-temperature plastic
Material extrusion (FDM, FFF, etc.) is a popular technology in additive manufacturing for the manufacture of products from general-purpose thermoplastic materials, as well as engineering and special-purpose plastics, including composite . A formalized model of the technological process of extrusion printing is presented in fig.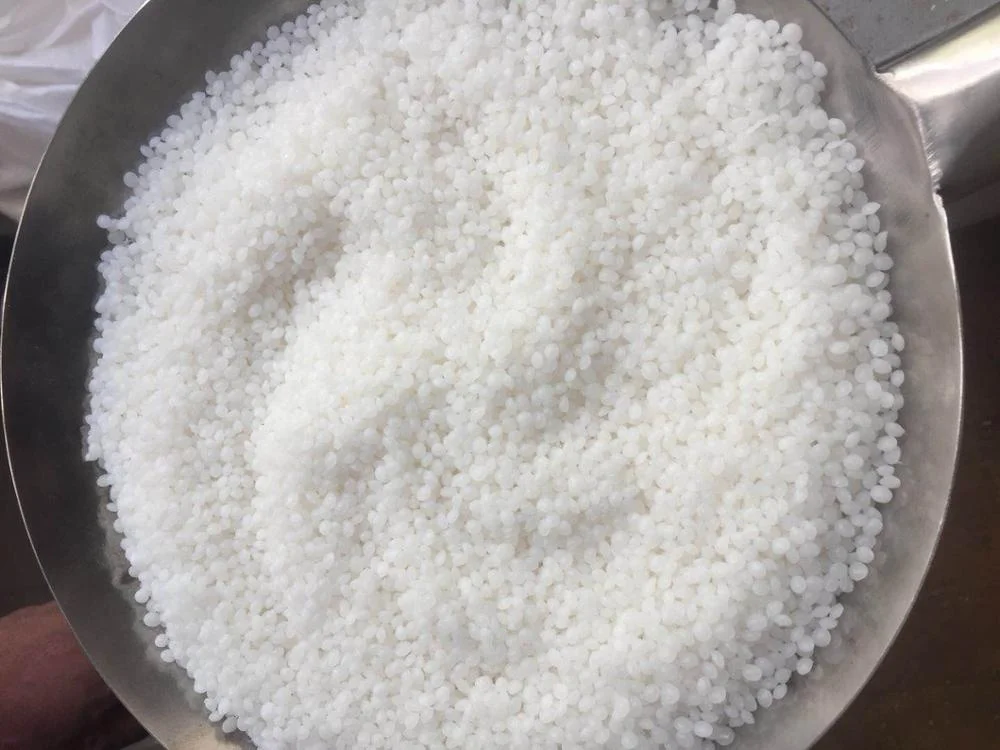 1.
1.
At the design stage, a list of requirements is formed that the product must meet during operation. When developing the technological process of extrusion 3D printing, the temperature interval for processing the selected material used for the manufacture of the product is taken into account.
When performing a 3D printing operation ( fig. 1 ), physical processes occur in the processed material, the control of which allows obtaining a defect-free product that meets the requirements formulated by the designer.
Fig. 1. Extrusion 3D printing technology model
The purpose of this article is to determine the temperature range of extrusion 3D printing of low-temperature thermoplastic materials based on the analysis of their thermal properties. Thermograms obtained by differential scanning calorimetry (DSC) on Mettler Toledo equipment, which can be used to select the temperature range of 3D printing, are considered using the example of thermoplastic materials, Wax3D wax and TPU plastics. An example of a product made from thermoplastic wax is shown in fig. 2. This is a master model for the subsequent production of a one-time shell mold using investment casting technology.
An example of a product made from thermoplastic wax is shown in fig. 2. This is a master model for the subsequent production of a one-time shell mold using investment casting technology.
Fig. 2. An example of a master model made of thermoplastic wax
Under "low temperature" is considered a thermoplastic material processed using extrusion 3D printing technology in the temperature range from 50 to 190 (200) ° C in equipment with an active or passive thermal chamber. Under these conditions, materials such as thermoplastic waxes (for example, Wax3D) [1], polycaprolactone (PCL), low-pressure polyethylene (PND, with a lower processing temperature limit of 190°C), polyurethane (TPU, with a lower temperature limit of 190°C), polyacetal (POM, with a lower temperature limit of 170°C).
Thermoplastic material PCL is described in sufficient detail in [2–4]. It is noted that biodegradable low-temperature plastic developed in the 1930s, characterized by a relatively low melting point (59–64°C), gained popularity again by the early 2000s, including due to the emergence of additive technologies.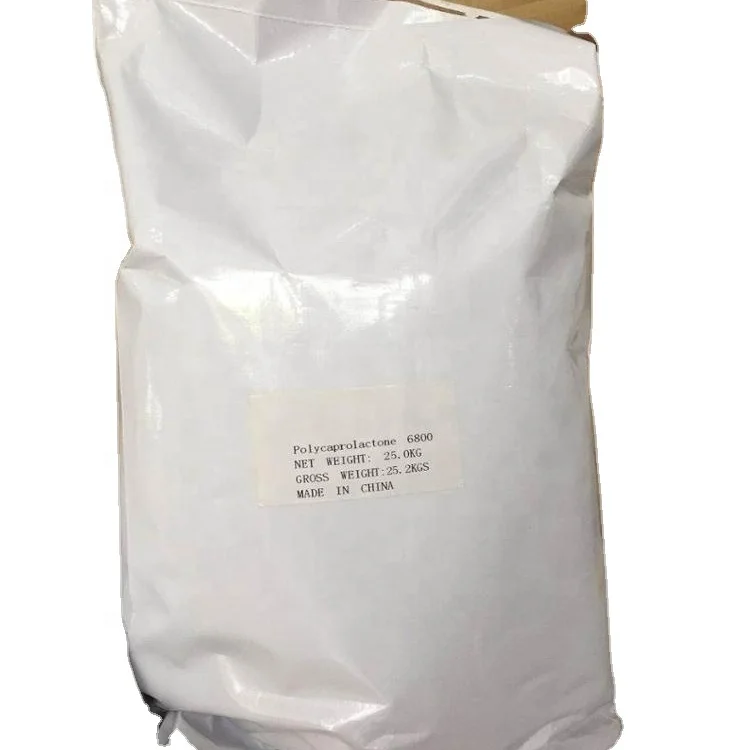
A few words about the physical processes occurring in a thermoplastic polymer material during extrusion 3D printing and the parameters that determine them. In [5, 6], a rather in-depth analysis of the physical processes and parameters ( fig. 3 and 4 ) that determine them and are associated with extrusion in 3D printing was carried out.
Fig. 3. Physical processes occurring during extrusion 3D printing [5]
Fig. Fig. 4. Key parameters affecting the result of extrusion 3D printing [6]
4 shows the external parameters that affect the course of the extrusion process. At the same time, thermophysical transformations take place in the material itself, leading to a change in the physical state of the polymer material. Extrusion 3D printing, as well as traditional methods of processing polymer materials, is based on the transfer of a polymer material into a viscous state (melt).
One of the key parameters of extrusion 3D printing is temperature: printing (heating block) temperature, working platform temperature, ambient temperature. The conditions of extrusion 3D printing are not isothermal even if the 3D printer has a passive or active thermal chamber. In [7], the temperature distribution in the 3D printing area was experimentally measured, showing its non-uniformity ( Fig. 5 ).
a) b)
Fig. 5. Temperature distribution during extrusion 3D printing [7]:
b) temperature distribution during extrusion, measured using
IR thermal cameras
, glassy, viscoelastic. One of the methods for analyzing thermophysical properties is differential scanning calorimetry (DSC; GOST R 55134–2012 (ISO 11357–1:2009), which consists in determining the difference in heat fluxes as a function of temperature and/or time in the process of exposure to the test and reference samples by a controlled temperature program. Heat fluxes are supplied to the crucible, inside which the test and reference samples are located. DSC analysis makes it possible to investigate physical transformations (glass transition, melting, crystallization, polymorphic transformations), in particular, in thermoplastic materials.
Heat fluxes are supplied to the crucible, inside which the test and reference samples are located. DSC analysis makes it possible to investigate physical transformations (glass transition, melting, crystallization, polymorphic transformations), in particular, in thermoplastic materials.
For thermoplastic wax, an example of a thermogram obtained as a result of DSC analysis is shown in fig. 6; for plastic type TPU with a hardness of 55D - on fig. 7.
Fig. Fig. 6. Thermogram of thermoplastic wax
Fig. 7. Thermogram of TPU-type thermoplastic plastic with Shore hardness 55D
The glass transition temperature (by the second heating) is determined from the thermogram - 11.85 ° C; at a temperature above the glass transition temperature and up to a temperature of ~120.0°C, the thermoplastic material gradually passes into the melt state.
The temperature maxima on the thermogram are associated with the melting of crystallites of different sizes. The temperature range of 3D printing is selected from the range of values from 90 to 115°C, which is due to the completion of the transition of the polymer material to the melt state. The boundary (minimum and maximum temperatures) is selected depending on the material properties of the product, for example, the mechanical properties that must be formed as a result of processing. Verification of mechanical properties can be performed on the basis of a tensile test of standard samples (GOST 11262–2017 and GOST 33693–2015 (ISO 20753:2008)).
The temperature range of 3D printing is selected from the range of values from 90 to 115°C, which is due to the completion of the transition of the polymer material to the melt state. The boundary (minimum and maximum temperatures) is selected depending on the material properties of the product, for example, the mechanical properties that must be formed as a result of processing. Verification of mechanical properties can be performed on the basis of a tensile test of standard samples (GOST 11262–2017 and GOST 33693–2015 (ISO 20753:2008)).
From the thermogram of plastic type TPU ( fig. 7 ) the glass transition temperature (according to the second heating; Tst) is determined - 18.97°C. The temperature range of 3D printing is selected from the range of values from 190 to 205°C, which is due to the completion of the transition of the polymer material to the melt state. The boundary (minimum and maximum temperatures) is chosen in the same way as in the case of thermoplastic wax, depending on the material properties of the product, for example, mechanical properties that need to be formed as a result of 3D printing.
Conclusions and forecast
The performed analysis of the literature, conducted full-scale experiments allow us to formulate recommendations on the choice of temperature range for extrusion 3D printing of some low-temperature thermoplastic plastics: mechanical), which must be formed in the material as a result of processing;
- a preliminary selection of the temperature range can be predicted from the results of DSC analysis - a thermogram; clarification of the temperature range - based on the results of a study of the achieved level of physical and mechanical properties required in accordance with the operational requirements for the product;
— Extrusion 3D printing temperature calculated from thermogram requires additional verification (confirmation) from test results, such as tensile testing. ■
References
Affordable printing of wax molds for casting // Additive Technologies. 2019. No. 4. P. 30–33. [electronic edition] URL: https://additiv-tech.ru/publications/dostupnaya-pechat-voskovyh-form-dlya-litya.html (date of access: 01/10/2022).
[electronic edition] URL: https://additiv-tech.ru/publications/dostupnaya-pechat-voskovyh-form-dlya-litya.html (date of access: 01/10/2022).
Van Natta FJ, Hill JW, Carruthers WH. Polymerization and ring formation, caprolactone and its polymers. J Am Chem Soc 1934;56:455–9.
Maria Ann Woodruff, Dietmar Werner Hutmacher. The return of a forgotten polymer - Polycaprolactone in the 21st century. Progress in Polymer Science. Volume 35. Issue 10. 2010. P. 1217–1256.
US8859691B2 Zhang, Zhongqun. (2014). Low temperature thermoplastic material and preparing method thereof.
Bastian Brenken, Eduardo Barocio, Anthony Favaloro, Vlastimil Kunc, R. Byron Pipes. Fused filament fabrication of fiber-reinforced polymers: a review. Additive manufacturing. Volume 21. 2018. P. 1–16.
L. G. Blok, M. L. Longana, H. Yu, B.K.S. woods. An investigation into 3D printing of fiber reinforced thermoplastic composites. additive manufacturing. Volume 22. 2018. P. 176–186.
D.