3D printing living tissue
3D Bioprinting of Living Tissues
Progress in drug testing and regenerative medicine could greatly benefit from laboratory-engineered human tissues built of a variety of cell types with precise 3D architecture. But production of greater than millimeter sized human tissues has been limited by a lack of methods for building tissues with embedded life-sustaining vascular networks.
Play
In this video, the Wyss Institute and Harvard SEAS team uses a customizable 3D bioprinting method to build a thick vascularized tissue structure comprising human stem cells, collective matrix, and blood vessel endothelial cells. Their work sets the stage for advancement of tissue replacement and tissue engineering techniques.Multidisciplinary research at the Wyss Institute has led to the development of a multi-material 3D bioprinting method that generates vascularized tissues composed of living human cells that are nearly ten-fold thicker than previously engineered tissues and that can sustain their architecture and function for upwards of six weeks. The method uses a customizable, printed silicone mold to house and plumb the printed tissue on a chip. Inside this mold, a grid of larger vascular channels containing living endothelial cells in silicone ink is printed, into which a self-supporting ink containing living mesenchymal stem cells (MSCs) is layered in a separate print job. After printing, a liquid composed of fibroblasts and extracellular matrix is used to fill open regions within the construct, adding a connective tissue component that cross-links and further stabilizes the entire structure.
Confocal microscopy image showing a cross-section of a 3D-printed, 1-centimeter-thick vascularized tissue construct showing stem cell differentiation towards development of bone cells, following one month of active perfusion of fluids, nutrients, and cell growth factors. The structure was fabricated using a novel 3D bioprinting strategy invented by Jennifer Lewis and her team at the Wyss Institute and Harvard SEAS. Credit: Lewis Lab, Wyss Institute at Harvard University
The structure was fabricated using a novel 3D bioprinting strategy invented by Jennifer Lewis and her team at the Wyss Institute and Harvard SEAS. Credit: Lewis Lab, Wyss Institute at Harvard UniversityThe resulting soft tissue structure can be immediately perfused with nutrients as well as growth and differentiation factors via a single inlet and outlet on opposite ends of the chip that connect to the vascular channel to ensure survival and maturation of the cells. In a proof-of-principle study, one centimeter thick bioprinted tissue constructs containing human bone marrow MSCs surrounded by connective tissue and supported by an artificial endothelium-lined vasculature, allowed the circulation of bone growth factors and, subsequently, the induction of bone development.
This innovative bioprinting approach can be modified to create various vascularized 3D tissues for regenerative medicine and drug testing endeavors. The Wyss team is also investigating the use of 3D bioprinting to fabricate new versions of the Institute’s organs on chips devices, which makes their manufacturing process more automated and enables development of increasingly complex microphysiological devices.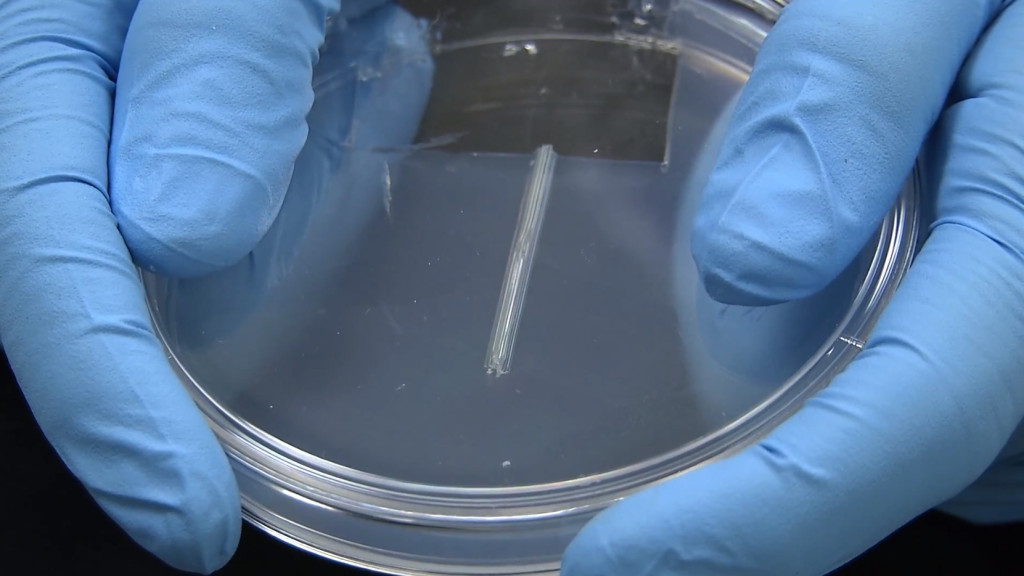 This effort has resulted in the first entirely 3D-printed organ on a chip – a heart on a chip – with integrated soft strain sensors.
This effort has resulted in the first entirely 3D-printed organ on a chip – a heart on a chip – with integrated soft strain sensors.
- 1/7 Cross section of long-term perfusion of HUVEC-lined (red) vascular network supporting HNDFladen (green) matrix.
- 2/7 Top-down view of long-term perfusion of HUVEC-lined (red) vascular network supporting HNDFladen (green) matrix.
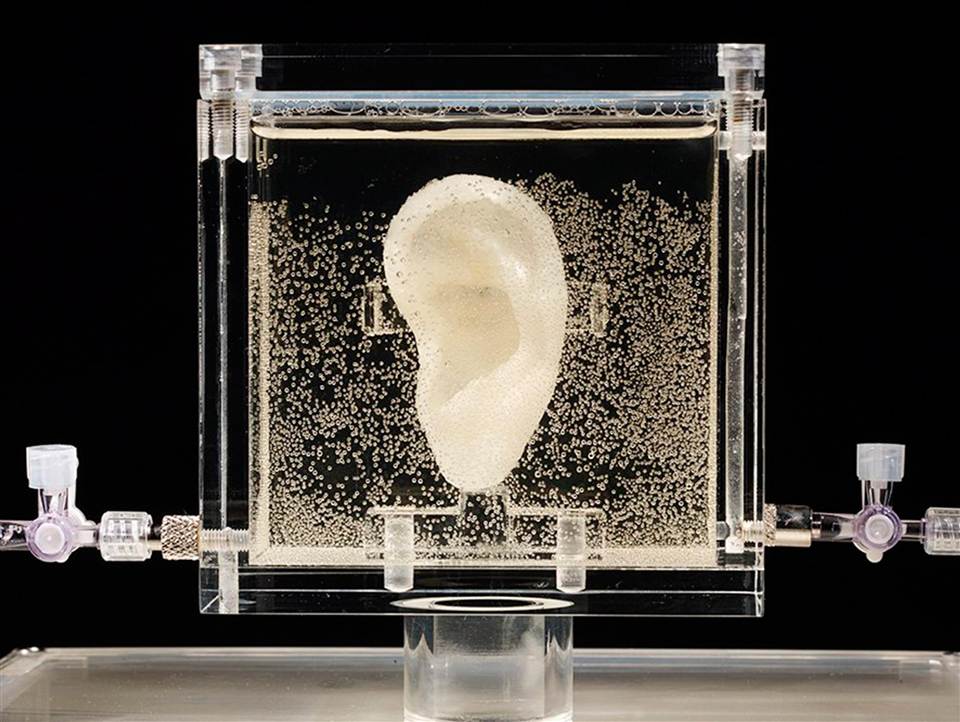
- 3/7 Photograph cross section of printed tissue construct housed within a perfusion chamber.
- 4/7 Photograph cross section of printed tissue construct housed within a perfusion chamber.
- 5/7 Photograph of a printed tissue construct housed within a perfusion chamber.
- 6/7 Photograph of vasculature network and cell inks.
- 7/7 Photograph of 3D printed vasculature network (red) within Red is the
- Next
- Prev
6 Advances in 3D Bioprinting of Living Tissue
In recent years, 3D bioprinting has made huge strides toward the goal of printing of organs that can be successfully transplanted into humans.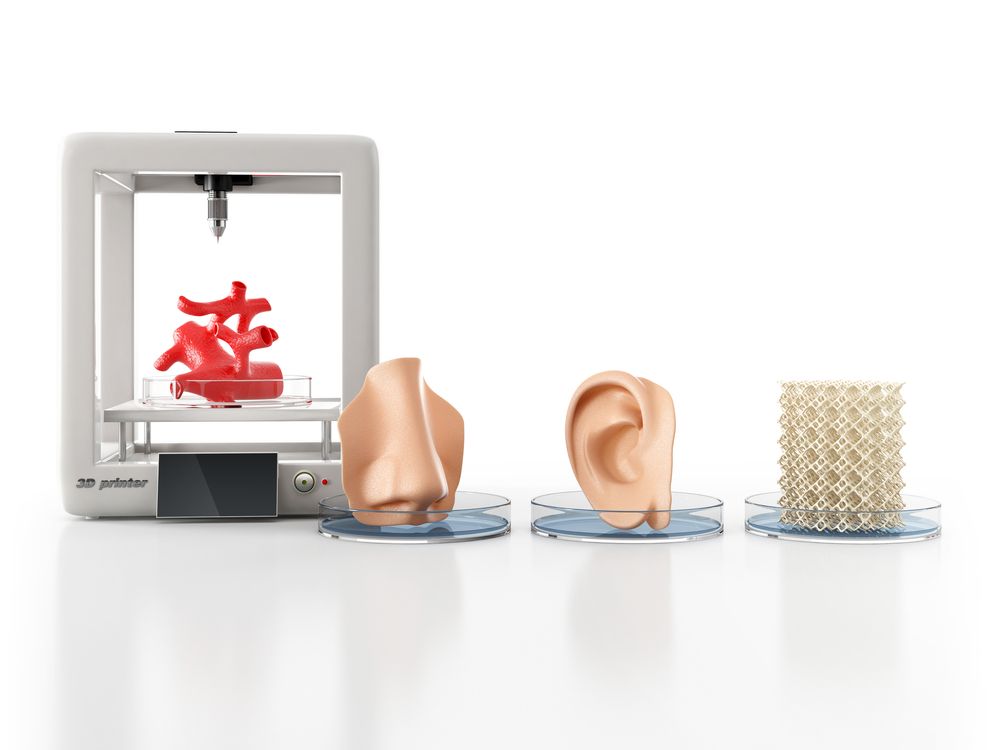 While that’s still far in the future, the method continues to be studied and perfected and advances can lead to new and improved treatments for conditions such as spinal cord injury, Alzheimer’s disease, Parkinson’s disease, brain cancer, and much more.
While that’s still far in the future, the method continues to be studied and perfected and advances can lead to new and improved treatments for conditions such as spinal cord injury, Alzheimer’s disease, Parkinson’s disease, brain cancer, and much more.
The 3D printing of living cells follows standard 3D printing methods, with a few twists. The printer, following a CAD file, lays down layer upon layer of material to build a shape. Instead of metals or plastics, bioprinters use bioinks as their materials. These contain living cells amid viscous materials like alginate or gelatin. The cells are often built upon scaffolding to support and protect the cells.
There have been many recent developments that are pushing the 3D bioprinting field forward. Here are six major advances.
Researchers at Rensselaer Polytechnic Institute and Yale University use a liquid bioink derived from human skin cells to print artificial skin. A blood vessel system then grows naturally within the skin.
A blood vessel system then grows naturally within the skin.
Researchers at Rensselaer Polytechnic Institute and Yale University use a liquid bioink derived from human skin cells to print artificial skin. Image: Rensselaer Polytechnic Institute
With a working vascular system to circulate blood, a patient could assimilate the grafted tissue much more quickly, said Pankaj Karande, a professor of chemical and biological engineering at Rensselaer, who led the research. While bioengineers have had success printing living tissue, few of those few projects have included blood vessels, he said.
“The vasculature is very important because that’s how the host and the graft talk to each other,” Karande said. “Communication between host and graft is critical if the skin substitute is not to be rejected by the body.”
Recommended for You: 3D Printing Overcoming Biocompatibility Challenge
Currently, patients in need of skin grafts have two options: an autologous skin grafts, where the doctors shave off a piece of healthy skin to cover the damaged area; or artificial skin products made from materials that range from bovine collagen to polymer foam.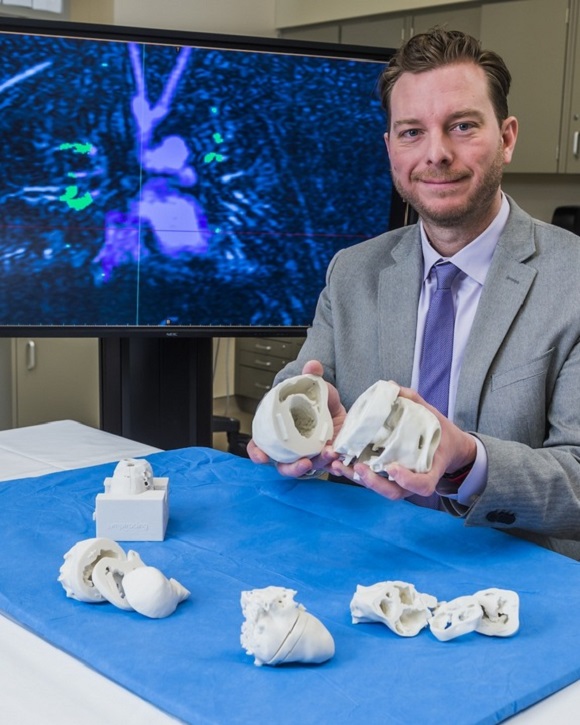 Both have disadvantages. Autologous skin grafts are painful and create a new wound. Artificial skin products have a range of limitations—they are often temporary, don’t cover deep wounds, or don’t resemble human skin, Karande added.
Both have disadvantages. Autologous skin grafts are painful and create a new wound. Artificial skin products have a range of limitations—they are often temporary, don’t cover deep wounds, or don’t resemble human skin, Karande added.
His team’s method is still in the basic research stage, Karande said.
Researchers at Rice University in Houston carve grooves into the plastic threads they use to build scaffolds. They then seed the grooves with cells or other bioactive agents that encourage the growth of new tissue.
The biocompatible implants created by Rice University researchers can degrade over time and leave only natural tissue. Image: Rice University
Unlike the cell-supporting hydrogel scaffolds under development in many labs, this process creates hard implants to be surgically inserted to heal bone, cartilage, or muscle, said Antonios Mikos, a biomedical engineer at Rice, who led the research. The biocompatible implants would degrade over time and leave only natural tissue.
The biocompatible implants would degrade over time and leave only natural tissue.
Usually, 3D-printed scaffolds are seeded with uniform distributions of cells, he said.
“If we wanted different cell populations at different points in the scaffold, we could not do that. Now we can,” he said.
“The major innovation is the capability to spatially load a 3-D printed scaffold with different types of cells populations and with different bioactive molecules,” Mikos said.
This first-of-its-kind method brings the field of tissue engineering one step closer to being able to 3-D print a full-sized, adult human heart, according to the Carnegie Mellon University researchers who created technique.
Scientists from Carnegie Mellon University use 3D bioprinting to build functional parts of the human heart, such as this heart valve.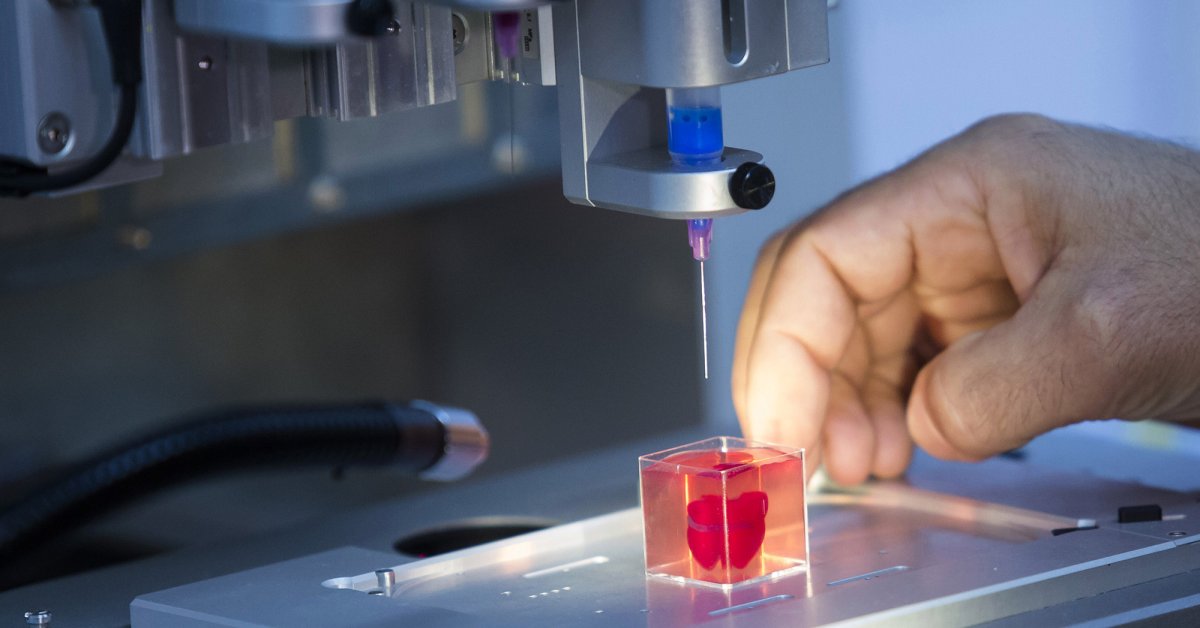 Image: Carnegie Mellon University
Image: Carnegie Mellon University
The technique, known as Freeform Reversible Embedding of Suspended Hydrogels (FRESH), overcomes challenges associated with existing 3-D bioprinting methods. It achieves unprecedented resolution and fidelity using soft and living materials, said Adam Feinberg, a professor of biomedical engineering whose Regenerative Biomaterials and Therapeutics Group performed the work.
Each of the organs in the human body, such as the heart, is built from specialized cells held together by a biological scaffold called the extracellular matrix (ECM). Networked ECM proteins provide the structure and biochemical signals that cells need to carry out their normal function.
Editor’s Pick: VA System Rolls Out 3D Printing
Until now, traditional biofabrication methods couldn’t recreate complex ECM architecture, Feinberg said.
“What we’ve shown is that out of cells and collagen, we can print parts that truly function, like a heart valve or a small beating ventricle,” he said. “By using MRI data of a human heart, we were able to accurately reproduce patient-specific anatomical structures and to 3-D bioprint collagen and human heart cells.”
“By using MRI data of a human heart, we were able to accurately reproduce patient-specific anatomical structures and to 3-D bioprint collagen and human heart cells.”
Collagen is hard to 3-D print because it starts out as a fluid, said Andrew Hudson, a doctoral student in Feinberg’s lab.
“If you try to print this in the air it just forms a puddle on your build platform,” said Hudson. “We’ve developed a technique that prevents it from deforming.”
The FRESH method deposits collagen layer-by-layer within a support bath of gel, giving the collagen a chance to solidify in place before it is removed from the support bath. The supportive gel is melted away by heating the gel from room temperature to body temperature after the print is complete. The researchers can then remove the support gel without damaging the printed structure made of collagen or cells.
A handheld 3D printer that deposits sheets of biomaterial skin to cover large burn wounds is another recent advance.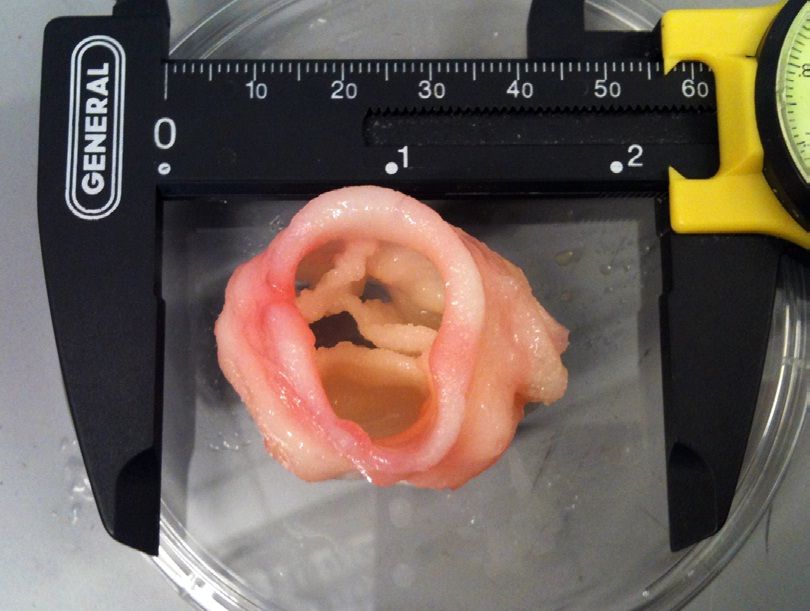 The biomaterial also accelerates the healing process.
The biomaterial also accelerates the healing process.
A handheld 3D printer lays down wound-healing strips of biomaterial to cover burn wounds. Image: University of Toronto
The device, from researchers at the University of Toronto and Sunnybrook Hospital in Toronto, dispenses bio ink over burn wound, strip by strip. The biomaterial is made from bio ink, itself composed of mesenchymal stroma cells (MSCs)—stem cells that differentiate into specialized cell types depending on their environment.
In this case, the MSC material promotes skin regeneration and reduces scarring, says biomedical doctoral candidate Richard Cheng. He heads the project under Axel Guenther, an associate professor of mechanical engineering at the school.
“Previously, we proved that we could deposit cells onto a burn, but there wasn't any proof that there were any wound-healing benefits; now we've demonstrated that,” Guenther said.
When the team unveiled its first prototype of the skin printer in 2018 it was believed to be the first device of its kind to form tissue in situ, depositing and setting tissue in place in two minutes or less.
Patient-specific, 3D-printed bone grafts could create new treatments for patients suffering from arthritis, bone fractures, dental infections, and craniofacial defects, said Akhilesh Gaharwar, associate professor of mechanical engineering at Texas A&M University. His team is leading this research.
Their bioink is an answer to the lack of bioinks that meet the demands of both 3D printing and tissue engineering, he said.
The Texas A&M group’s NICE bioink formulation is used specifically to print 3D bone. Image: Texas A&M
“The ideal bioink must be capable of being extruded into stable 3D structures while protecting cells during and after printing and providing an appropriate environment that can be remodeled into the target tissue,” Gaharwar said. “Unfortunately, conventional hydrogels are weak and poorly printable.”
“Unfortunately, conventional hydrogels are weak and poorly printable.”
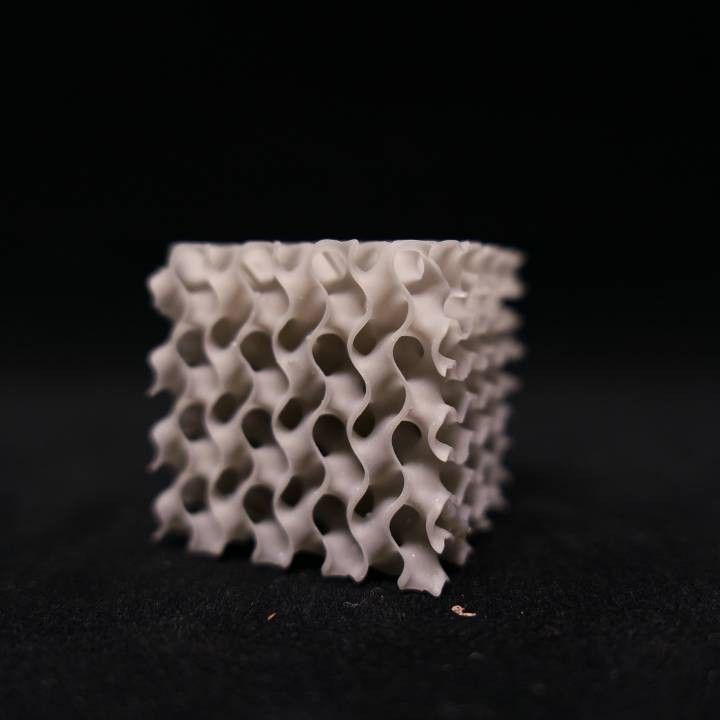
The group’s NICE bioink formulation is used specifically to print 3D bone. NICE bioinks are a combination of two reinforcement techniques. Used together, they provide an effective reinforcement that results in much stronger bone structures. The NICE bioinks allow precise control over mechanical properties and degradation characteristics, enabling custom 3D fabrication of mechanically resilient, cellularized structures, Gaharwar said.
Further Reading: 3D Printing Organs Nearing Clinical Trials
Once the bioprinting process is complete, the cell-laden NICE networks are crosslinked to form stronger scaffolds. With the technique, the researchers have been able to produce full-scale, cell-friendly reconstructions of human body parts, including ears, blood vessels, cartilage, and bone segments.
This step toward 3D-printed replacements of human parts comes from a team at University of California, San Diego.
Most 3D bioprinting is done in culture dishes, but the UCSD team was able to do this in laboratory rats.
The scientists at UCSD printed out small implants made of softgel and then filled them with neural stem cells. Image: University of California, San Diego
The scientists first printed out small implants made of softgel, then filled them with neural stem cells, again using a printer. The implants were then surgically placed inside a tiny gap in a rat’s spinal cord. The precision 3D printing allowed the softgel and cellular matrix to fit accurately into the gap, or wound, said Shaochen Chen, a professor of nanoengineering at the university and a team leader.
Over time the new nerve cells and axons grew and formed new connections across the cut spinal cord of the animal. These nerve cells connected not only with one another but with the host spinal cord tissue and the circulatory systems of the rat. The lab-grown cells then successfully bridged the gap in the spinal cord and partially restored movement to the animal's hind quarters, said Mark Tuszinski, a professor of neuroscience at the university.
The lab-grown cells then successfully bridged the gap in the spinal cord and partially restored movement to the animal's hind quarters, said Mark Tuszinski, a professor of neuroscience at the university.
The researchers said that bioprinted tissue can be used to test the effects of drug treatments and, eventually achieve the 3D bioprinting goal: printing entire organs that can be grown and then transplanted into a patient.
Jean Thilmany is an independent writer in St. Paul, Minn.
Organ printing: how 3D bioprinting technology has advanced and what is hindering its development In research centers and hospitals around the world, advances in 3D printing and bioprinting are providing new opportunities for human treatment and scientific research. In the coming decades, bioprinting could be the next major milestone in healthcare and personalized medicine.
Let's talk about bioprinting technology, the latest advances in the industry and the limitations that professionals face.
How a 3D printer works
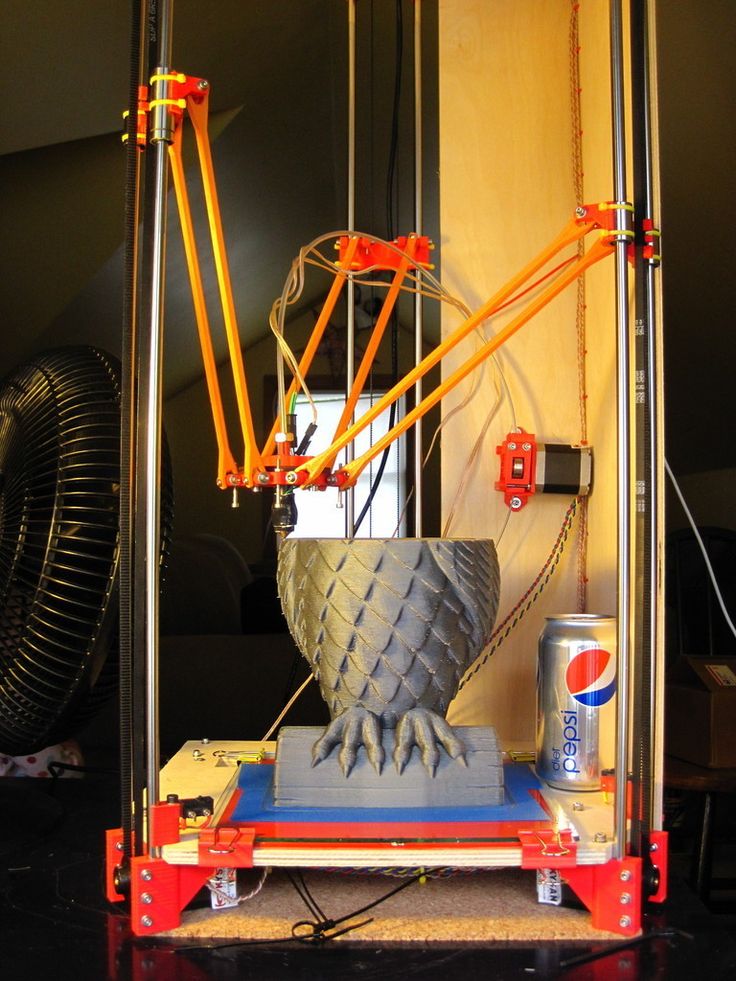
Traditional printers, like the one you have at home or office, work in two dimensions. They can print text or images on a flat surface (usually paper) using the x (horizontal) and y (vertical) dimensions. 3D printers add another dimension - depth (z). During the printing process, the printer heads can move up and down, left and right, back and forth, but instead of delivering ink to paper, they distribute various materials - polymers, metal, ceramics and even chocolate - until the "print" of a holistic, voluminous object , layer by layer in a process known as "additive manufacturing".
To create a 3D object, you need a blueprint for it, a digital file created with modeling software. After its creation, the computer-generated model is sent to the printer. Your chosen material is loaded into the machine and ready to be heated to easily flow out of the printer nozzle. As the printer reads the plan, its head moves, depositing successive layers of the selected material to create the final product.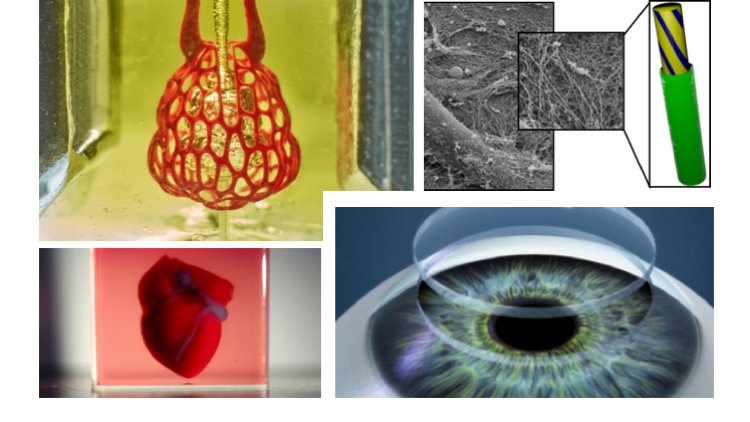
As each layer is printed, it is solidified either by cooling or by mixing two different solutions delivered by the printer head. The new layers precisely lay down on the previous ones to make a stable, cohesive element. In this way, you can create almost any shape, including a moving one.
3D printing allows you to create objects with geometric structures that would be difficult or impossible to make in other ways. A wide range of products are already being created using 3D printers, including jewelry, clothing, toys, and high-end industrial products. Even a 10-year-old Moscow schoolboy has learned how to work with a 3D printer: he prints 3D figures to order and sells them through Instagram.
How a bioprinter works
Bioprinters work in much the same way as 3D printers, with one key difference - they deposit layers of biomaterial, which can include living cells, to create complex structures such as blood vessels or skin tissue.
Living cells? Where do they get them? Every tissue in the body is made up of different types of cells. The required cells (kidney, skin, and so on) are taken from the patient and then cultured until there are enough of them to create "bio-ink" that is loaded into the printer. This is not always possible, therefore, for some tissues, stem cells are taken that are capable of becoming any cell in the body (organism), or, for example, porcine collagen protein, seaweed and others.
Often used in bioprinting is chitosan, a polysaccharide obtained from the external skeleton of mollusks (eg shrimp) or by fermenting fungi. This material has high biocompatibility and antibacterial properties. Its disadvantage is the low rate of gelation. Another popular material is a polysaccharide isolated from seaweed called agarose. Its advantages are high stability and the possibility of non-toxic cross-linking during research. However, this biomaterial does not decompose and has poor cell adhesion (the ability of cells to stick together with each other and with other substrates).
Collagen, a primary structural protein found in the skin and other connective tissues, has a high biological significance. It is the most abundant protein in mammals and a major component of connective tissue. Its disadvantages for bioprinting include the property of acid solubility. More information about biomaterials can be found here.
Based on computer designs and models, often scans and MRIs taken directly from the patient, the printer heads place the cells exactly where they are needed and within a few hours an organic object is built from a large number of very thin layers.
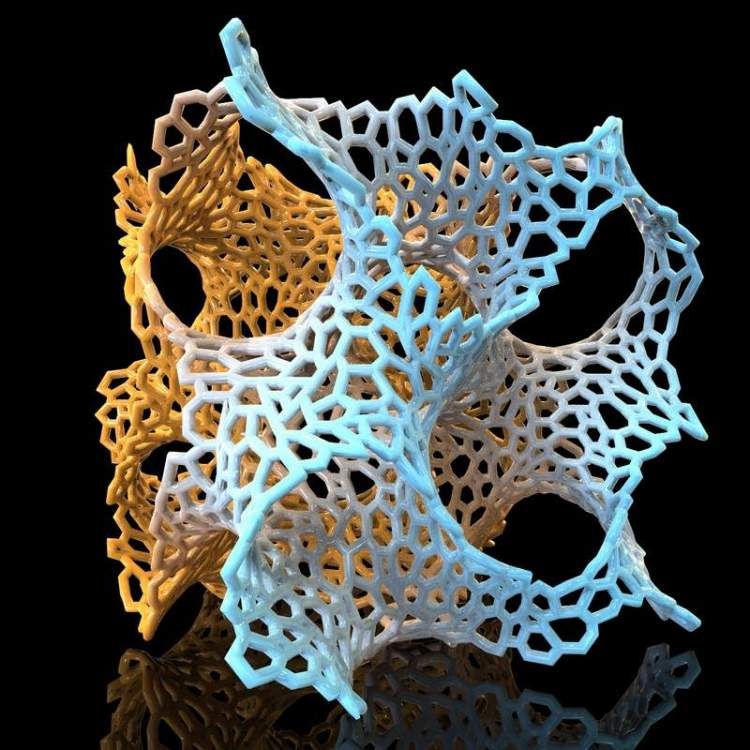
Organovo bioprinter creates tissues that mimic the structure and composition of various human organs
Source: Pbs.org
Scaffolding for ear or nose replacement at Wake Forest University in Winston-Salem, North Carolina
Source: CBS News
Computer displays an image of a "scaffold" for the human ear, created in the laboratory of Wake Forest University in Winston-Salem, North Carolina
Source: CBS News
Usually more than just cells are needed, so most bioprinters also supply some kind of organic or synthetic "glue" - a soluble gel or collagen scaffold to which cells can attach and grow. This helps them form and stabilize in the correct shape. Surprisingly, some cells can take the correct position on their own without any "scaffolding". How do they know where to go? How do embryonic cells develop in the uterus, or does adult tissue move to repair damage? Same here.
This helps them form and stabilize in the correct shape. Surprisingly, some cells can take the correct position on their own without any "scaffolding". How do they know where to go? How do embryonic cells develop in the uterus, or does adult tissue move to repair damage? Same here.
Universities, researchers and private companies around the world are involved in the development of bioprinting technologies. Let's take a look at some of the amazing things they are working on.
Bioprinting in Russia
3D Bioprinting Solutions is a biotechnology research laboratory founded by medical company INVITRO. The activity of the laboratory is the development and production of bioprinters and materials in the field of three-dimensional bioprinting and scientific research. August 23, 20193D Bioprinting Solutions laboratory sent a new batch of cuvettes to the ISS to continue experiments on bioprinting in space, which began in 2018. This was reported in the press center of the laboratory. This time it is planned to use organic and inorganic components to assemble bone tissue on the world's first space bioprinter Organ.Aut.
This time it is planned to use organic and inorganic components to assemble bone tissue on the world's first space bioprinter Organ.Aut.
Symposium "Biofabrication in Space"
Source: Zdrav.Expert
Organ.Aut magnetic bioprinter
Source: Zdrav.Expert
The astronauts will also grow protein crystals and experiment with printing biofilms of bacteria to study their behavior in zero gravity. Russian scientists expect to receive unique scientific data that can be applied in the development of new drugs.
Scientific director of 3D Bioprinting Solutions and leading researcher of the Institute of Regenerative Medicine, Candidate of Medical Sciences Vladimir Mironov, in his speech at the Department of Anatomy of Sechenov University on September 2, noted: “Living cells, tissues and human organs will be synthesized already in the current century. To do this, morphological sciences, such as microscopic anatomy and histology, must be digitized or digitalized, that is, digitized and made available for computer programs of robotic bioprinters, since without digital models it is impossible to print human tissues and organs. ”
”
Bioprinting around the world
Every year, millions of people around the world need bone grafting. Modern bone grafts often use cement-based synthetic material in combination with the patient's own bone. However, the use of these materials has a number of limitations - some transplants caused rejection and inflammatory processes in patients. Reproduction of the natural bone-cartilage "interface" has also been problematic.
However, a team at Swansea University in 2014 developed a bioprinting technology that allows the creation of an artificial bone prosthesis in the exact shape of the desired bone, using a biocompatible material that is both durable and regenerative. At the same time, scientists from the University of Nottingham in England were working on similar studies.
It takes about two hours to print a small bone. Therefore, surgeons can do it right in the operating room. This part of the bone is then covered with adult stem cells that can develop into almost any other type of cell. This is combined with bio-ink from the printer, a combination of polylactic acid (which provides mechanical strength to bone) and alginate, a gel-like substance that serves as a shock-absorbing material for cells. The end product is then implanted into the body, where it will completely disappear within about three months and be replaced by new bone.
This is combined with bio-ink from the printer, a combination of polylactic acid (which provides mechanical strength to bone) and alginate, a gel-like substance that serves as a shock-absorbing material for cells. The end product is then implanted into the body, where it will completely disappear within about three months and be replaced by new bone.
Researchers hope that in the future, bioprinted bones can be created with sufficient reliability to support complex spinal reconstruction, and that the bone material will be further improved to increase its compatibility with cartilage cells.
Source: ETH Zurich
Successful 3D printing of human cartilage may soon completely replace artificial implants for people in need of reconstructive surgery. Back in 2015, scientists in Zurich developed technology that would allow hospitals to print a full-size human nose implant in less than 20 minutes. They believe that any cartilage implant can be made using their technique.
Researcher Matti Kesti described the technology as follows:
“
“A serious car accident can cause the driver or passenger to suffer complex nose injuries. The nose can be restored by creating a 3D model on a computer. At the same time, a biopsy of the patient is performed and cartilage cells are removed from the victim's body, such as from a knee, a finger, an ear, or fragments of a broken nose. The cells are spawned in the laboratory and mixed with the biopolymer. From this suspension, a model of nasal cartilage is created using a bioprinter, which is implanted into the patient during surgery. In the process, the biopolymer is used simply as a mold. It is subsequently broken down by the body's own cartilage cells. And in a couple of months it will be impossible to distinguish between the graft and the person’s own nasal cartilage.”
Matti Kesti
Since the implant was grown from the body's own cells, the risk of rejection will be much lower than for an implant made of, say, silicone. An additional advantage is that the bioimplant grows with the patient, which is especially important for children and young adults.
An additional advantage is that the bioimplant grows with the patient, which is especially important for children and young adults.
If a person is severely burned, healthy skin can be taken from another part of the body and used to cover the affected area. Sometimes intact skin is missing.
Researchers at Wake Forest School of Medicine have successfully designed, built and tested a printer that can print skin cells directly onto a burn wound. The scanner very accurately determines the size and depth of damage. This information is sent to a printer and skin is printed to cover the wound. Unlike traditional skin grafts, it only takes a patch of skin one-tenth the size of a burn to grow enough cells to print. While this technology is still in the experimental stage, the researchers hope that it will be widely available within the next five years.
As already mentioned, 3D printers print products in layers, and since the skin is a multi-layered organ with different types of cells, it is well suited for this type of technology. However, researchers still have a lot of problems to solve, in particular, how to prevent damage to cells from the heat generated by the printer. And of course, like most parts of the human body, the skin is more complex than it first appears—there are nerve endings, blood vessels, and a host of other aspects to consider.
However, researchers still have a lot of problems to solve, in particular, how to prevent damage to cells from the heat generated by the printer. And of course, like most parts of the human body, the skin is more complex than it first appears—there are nerve endings, blood vessels, and a host of other aspects to consider.
Blood vessels
Biomechanical engineer Monica Moya holding a petri dish with printed alginate-based biotubes. Biotubes can act as temporary blood vessels similar to blood vessels that help create a patch of living tissue.
Source: embodi3D
With tens of thousands of miles of veins, arteries and capillaries in the human body, researchers are working to replace them if they ever wear out. The creation of viable blood vessels is also essential for the proper functioning of all other potential bioprinted body parts.
Biomechanical Engineer Monica Moya of Livermore National Laboratory.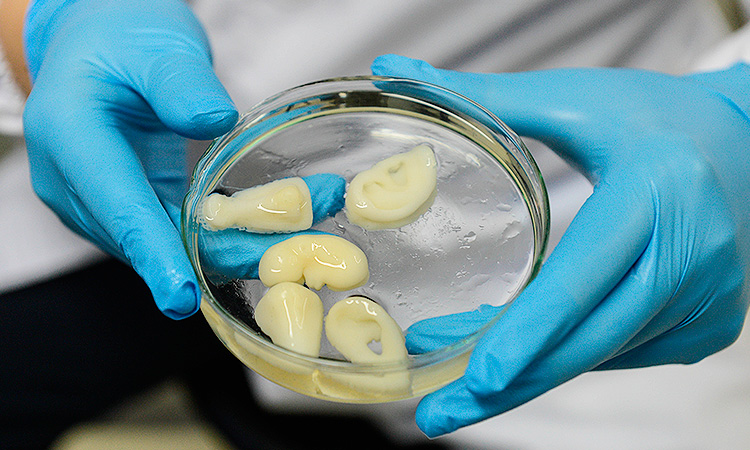 Lawrence uses bioprinting to create blood vessels. The materials created by her bioprinters are engineered to allow small blood vessels to develop on their own.
Lawrence uses bioprinting to create blood vessels. The materials created by her bioprinters are engineered to allow small blood vessels to develop on their own.
This development takes time, so vials of cells and other biomaterials are printed to help deliver vital nutrients to the printed environment. After a while, self-assembled capillaries connect with bioprinted tubes and begin to deliver nutrients to cells on their own, mimicking the work of these structures in the human body.
Internal organs
Many researchers hope that in 20 years the lists of patients waiting for organ transplants will become a thing of the past. They envision a world where any organ can be printed and transplanted in just a few hours, without rejection or complications, because these organs will be created from body cells according to the individual characteristics of each patient. Currently, bioprinting of fully functional complex internal organs is not possible, but research is ongoing (and not without success).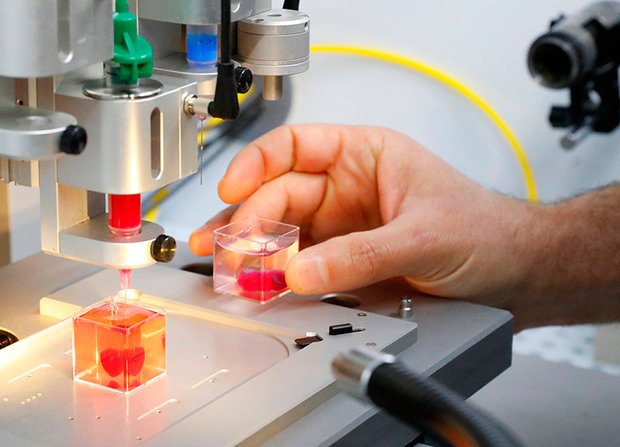
Bladder
For example, the bladder is already printed. In 2013, at Wake Forest University in the US, researchers successfully took cells from a patient's original, poorly functioning bladder, cultured them, and added additional nutrients. The 3D shape of the patient's bladder was then printed and the cultured cells soaked through it. The form was placed in an incubator and, when it reached the desired condition, it was transplanted into the patient's body. The mold will eventually collapse, leaving only the organic material. The same team successfully created viable urethras.
Physicians and scientists at the Wake Forest Institute for Regenerative Medicine (WFIRM) were the first in the world to create laboratory-grown organs and tissues that were successfully transplanted into humans. Right now they are working on growing tissues and organs for more than 30 different areas of the body, from the kidneys and trachea to cartilage and lungs. They also aim to accelerate the availability of these treatments to patients.
They also aim to accelerate the availability of these treatments to patients.
Scientists in Australia are doing similar research as well. They used human stem cells to grow a kidney organ that contains all the necessary cell types for a kidney. Such cells can serve as a valuable initial source for bioprinting more complex kidney structures.
MD, Professor of Urology, Professor of the Institute of Regenerative Medicine Anthony Atala shows a kidney created by a bioprinter. A modified desktop inkjet printer sprays cells instead of ink. The cells were cultured from the patient and the structural template for the kidney was obtained from the MRI (so it is the correct size and shape).
Using this technology, back in 2001, Atala printed and successfully transplanted a bladder into a young man, Jake.
Source: TedEd
Heart
Heart cells, laboratory-grown organelles. Source
Surprisingly, it is the human heart that can become one of the easiest organs to print, since, in fact, it is a pump with tubes. Of course, everything is not so simple, but many researchers believe that humanity will learn to print hearts before kidneys or liver.
Of course, everything is not so simple, but many researchers believe that humanity will learn to print hearts before kidneys or liver.
Researchers at the Wake Forest Institute for Regenerative Medicine in April 2015 created "organoids" - 3D printed fully functional, beating heart cells.
In April 2019, Israeli scientists printed the world's first 3D heart. It is still very small, the size of a cherry, but it is able to perform its functions. The 3D heart with blood vessels uses personalized "ink" of collagen, a protein that supports cell structures, and other biological molecules.
A Tel Aviv University researcher holds the world's first 3D printed heart on April 15, 2019.
Source: Haaretz
“This is the first time anyone anywhere has successfully designed and printed a whole heart with cells, blood vessels, ventricles and chambers,” said Tel Aviv University scientist Professor Tal Dvir.
So far, scientists have been able to print tissue from cartilage and the aortic valve, for example, but the challenge has been to create tissue with vascularity—the blood vessels, including capillaries, without which organs cannot survive, let alone function.
The Tel Aviv scientists started with human adipose tissue and separated the cellular and non-cellular components. They then reprogrammed the cells to become undifferentiated stem cells, which could then become cardiac or endothelial. Endothelium - a single layer of flat cells lining the inner surface of the heart cavities, blood and lymphatic vessels. Endothelial cells perform many functions of the vascular system, such as controlling blood pressure, regulating the components of blood clotting, and the formation of new blood vessels.
Non-cellular materials, including a large amount of proteins, were processed into a "personalized hydrogel" that served as "printing ink".
It will be years before this technology can create organs for efficient transplantation. However, the achievements of scientists in Tel Aviv are a huge milestone along the way.
Medical research and pharmacology
One of the key potential uses for bioprinted living materials is in the field of medical and drug research.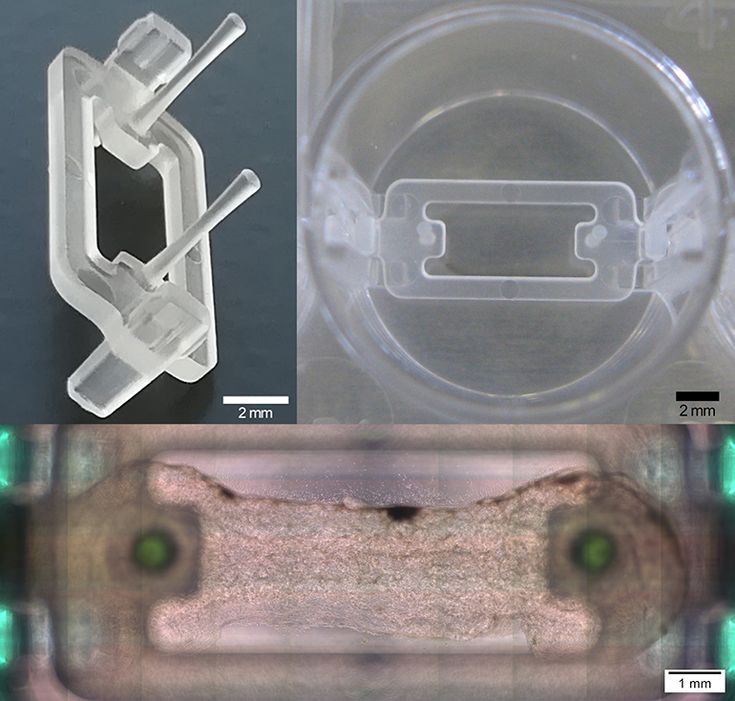 Bioprinted tissues have several cell types with different densities and key architectural features. This allows researchers to study the impact of various diseases on the body, the stages of disease progression and possible treatments in the natural microenvironment.
Bioprinted tissues have several cell types with different densities and key architectural features. This allows researchers to study the impact of various diseases on the body, the stages of disease progression and possible treatments in the natural microenvironment.
One of the most impressive developments in recent years is the development of a desktop brain at the ARC Center of Excellence in 2016. The researchers were able to use a 3D printer to create a 3D printed six-layer structure that includes nerve cells that mimic the structure of brain tissue.
This opens up huge potential benefits for researchers, pharmaceuticals and private companies, because it will allow them to test new products and drugs on tissue that accurately reflects the responses of human brain tissue, as opposed to animal samples, which may cause a completely different response. The desktop brain can also be used to further investigate diseases such as schizophrenia or Alzheimer's.
We are far from printing the brain, but the ability to arrange cells to form neural networks is a significant step forward. By allowing researchers to work with human tissue in real time, testing processes can be greatly accelerated and results can be more realistic and accurate. It will also reduce the need to use laboratory animals for medical tests and potentially dangerous human testing.
By allowing researchers to work with human tissue in real time, testing processes can be greatly accelerated and results can be more realistic and accurate. It will also reduce the need to use laboratory animals for medical tests and potentially dangerous human testing.
Medical simulators and data registries
Source: Simbionix
About 3,000 medical simulators are currently in use around the world to help doctors practice complex procedures. Virtual blood vessels, 3D printed organs... and no animal suffers!
The American company 3D Systems created an industry segment called VSP (Virtual Surgical Planning). This approach to personalized surgery combines expertise in medical imaging, surgical simulation and 3D printing. Surgeons using the Simbionix medical simulator for the first time often report feeling physical pain while empathizing with their virtual patient - the experience is so realistic. Organs and tissues look completely real.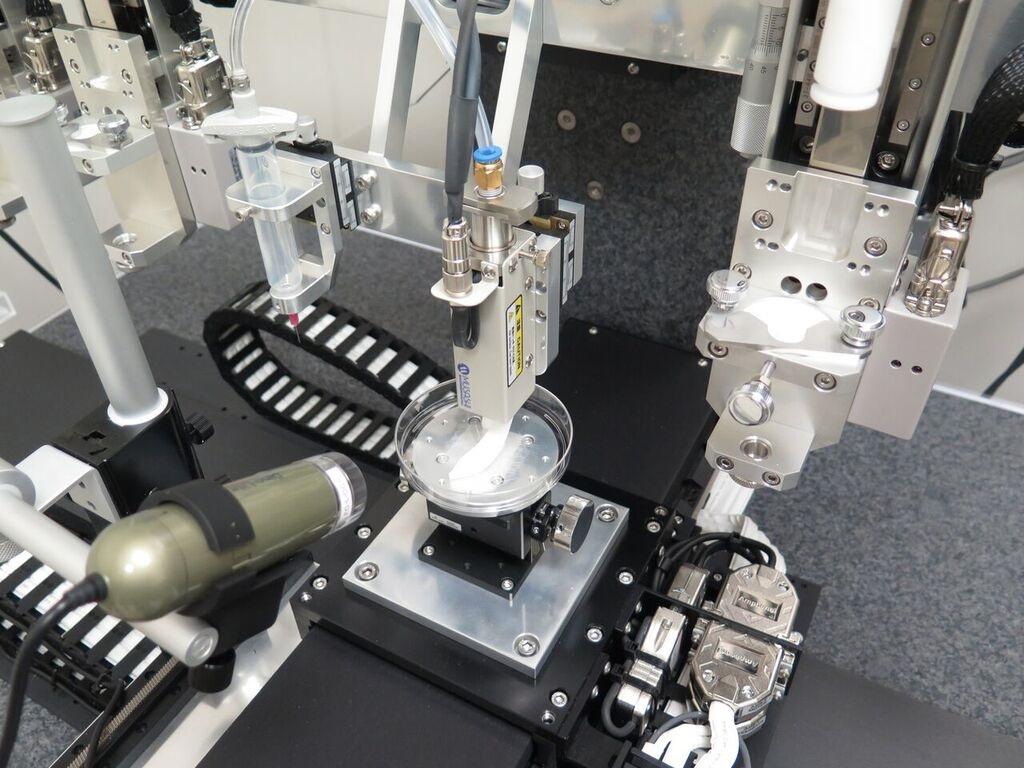 When stitching an organ, the surgeon sees on the screen a needle that enters the tissue, and pulls the thread. If the doctor does something wrong, the virtual blood vessels break and the organ begins to bleed. These simulators were developed by the Israeli company Symbionix, which was acquired by 3D Systems in 2014.
When stitching an organ, the surgeon sees on the screen a needle that enters the tissue, and pulls the thread. If the doctor does something wrong, the virtual blood vessels break and the organ begins to bleed. These simulators were developed by the Israeli company Symbionix, which was acquired by 3D Systems in 2014.
On September 3, 2019, the Radiology Society of North America (RSNA) and the American College of Radiology (ACR) announced the launch of a new 3D Medical Printing Clinical Data Registry to collect data on treatment outcomes using 3D printing at the point of care. This information will be a powerful tool to assess and improve patient care in real time, drive ongoing research and development, and inform patients and healthcare professionals about the best course of care.
“
“The creation of a joint RSNA-ACR 3D printing registry is essential to the advancement of clinical 3D printing. The registry will collect data to support the appropriate use of this technology and its implications for clinical decision making. ”
”
William Widock, Professor of Radiology at the University of Michigan and Chairman of the RSNA 3D Printing Special Interest Group (SIG)
According to RSNA, the information in the registry will allow for the necessary analysis to demonstrate the clinical value of 3D printing. Due to the wide variety of clinical indications, different technologies for creating physical models from medical images, and the complexity of the models, it is problematic to choose the optimal treatment method. The registry will help solve this problem.
Bioprinting software
Bioprinter and bioprinting software manufacturer Allevi introduced Allevi Bioprint Pro software on September 5, 2019. Built-in model generation and integrated slicing will allow you to focus more on experimenting, rather than setting up the printer. The program runs entirely in the cloud, which means you can create your biostructures, define materials, and track prints right from a web browser on any computer.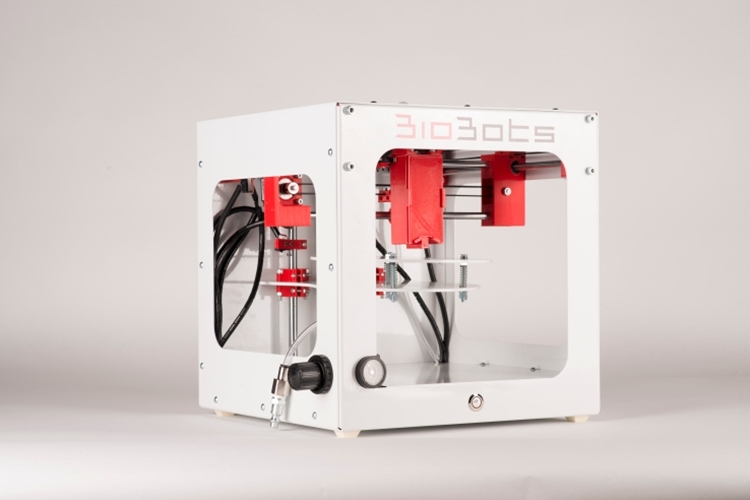
According to the development team, the new bioprinter with the above software is powerful and easy to use and represents another piece of the puzzle on the way to 3D printed organs.
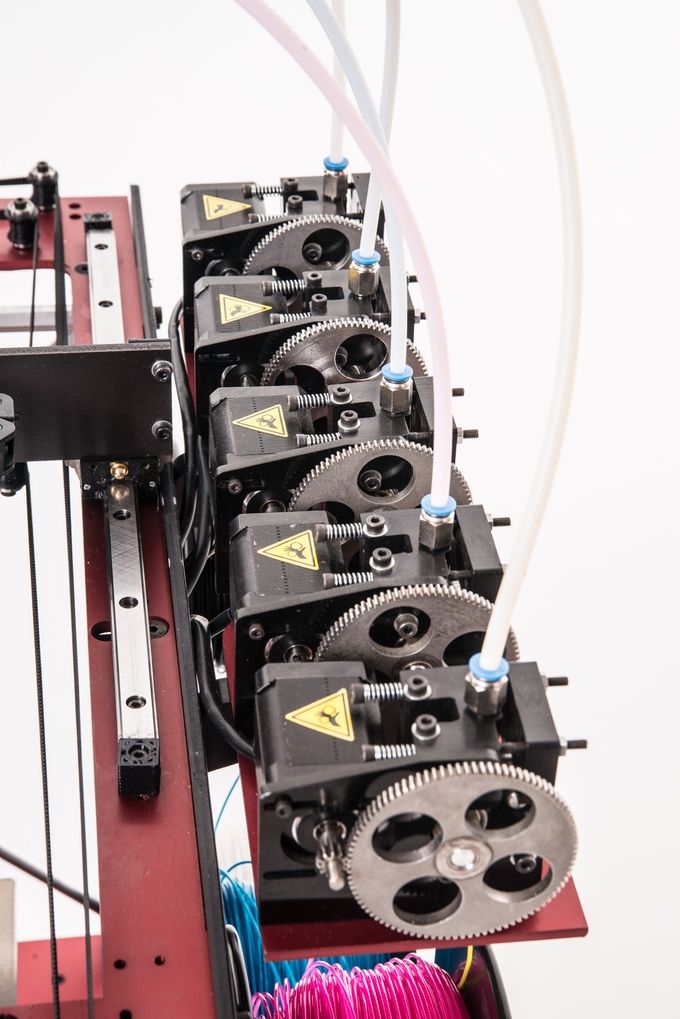
At the same time, CELLINK, the first bio-ink company, announced the launch of a new product to become the most flexible bio-printing platform on the market. The BIO X6 bioprinter, which has no analogues at the moment, has the ability to combine more bioprinting materials, cells and tools.
Why is this taking so long?
Complex body structure
The human body and its various components are much more complex than a plastic toy. The human organ has a complex network of cells, tissues, nerves, and structures that must be arranged in specific ways to function properly. From placing thousands of tiny capillaries in the liver to actually getting a printed heart that "beats" and contracts in the human body, there is still a lot of research and testing.
Legal regulation
In addition, bioprinting technologies, like all new medical treatments, must pass safety tests and due process of regulation before they become available.
Special software and hardware
It also takes time to develop special software and hardware. These programs can be written only with the appropriate data (medical, clinical, statistical, mathematical, and so on), which someone must first collect, analyze, systematize and digitize.
Working through all of these steps requires the integration of technologies from various fields, including engineering, biomaterials science, cell biology, physics, mathematics, and medicine. So we need to be a little more patient.
The main thing is to know that those who work in the field, doctors and engineers, programmers and scientists are making progress every day both in bioprinting technology itself and in understanding how it can be used and improved. Although we are not quite there yet, there is no doubt that medicine will be very different in 10-20 years, thanks also to bioprinting.
In brief
Bioprinting is an extension of traditional 3D printing.
Bioprinting can produce living tissue, bones, blood vessels, and possibly entire organs for use in medical procedures, medical training, and testing.
The cellular complexity of a living organism has made 3D bioprinting slower to develop than conventional 3D printing.
Bioprinting technology could enable the generation of patient-specific tissues to develop precise, targeted and fully personalized treatments.
We still have a long way to go before we can create fully functioning and viable organs for human transplantation.
Related materials: Russia was the first in the world to print living tissues in space using a bioprinter
5 most amazing things created using 3D printing
A rocket printed on a 3D printerwill go into orbit in 2021 "Exhibits touching is allowed”: how 3D printing is transforming museums
© Rusbase, 2019
Author: Nadezhda Aleinik
Cover photo: etonastenka, Depositphotos
3D bioprinting – how to create a transplantable organ?
Sergey Chapek, expert of the Research Laboratory of the DSTU "Engineering Technologies in Medicine", talks about how living tissues can be produced from hydrogel.
– What is 3 D bioprinting?
– 3D bioprinting is a technology for creating three-dimensional models on a cell basis using 3D printing. The technology consists in the fact that instead of the usual plastic for printing, we use hydrogel and living cells to create a three-dimensional structure (scaffold). Hydrogel is an artificial moisture-absorbing material based on hydrophilic natural polymers that promotes the accumulation and preservation of moisture. This hydrogel is used as a bioink, directly from the raw material from which the final product is obtained.
– What is the purpose of 3 D bioprinting?
“This is one of the most promising technologies for growing and producing tissues and, in the future, human organs. The production of a transplantable organ is one of the most important tasks facing science today. Millions of people suffer from injuries or damage to tissues and organs, such as peripheral nerve damage and heart attacks. But, unfortunately, the availability of organs for transplantation is very limited. To address this problem, tissue engineering aims to produce tissue and organ substitutes to improve existing treatment approaches. Advances in tissue engineering would mean that anyone with tissue or organ injury could go to the hospital, have an engineered replacement implanted in their body, and thereby completely restore the function of a healthy body. Of course, the cultivation of a full-fledged human or animal organ, in my opinion, will not be possible very soon. However, there is already a colossal breakthrough in this environment – the creation of microtissue for individual selection of drug therapy during the treatment of oncological diseases. We are talking about the treatment of complex diseases that require study and selection of drug therapy.
But, unfortunately, the availability of organs for transplantation is very limited. To address this problem, tissue engineering aims to produce tissue and organ substitutes to improve existing treatment approaches. Advances in tissue engineering would mean that anyone with tissue or organ injury could go to the hospital, have an engineered replacement implanted in their body, and thereby completely restore the function of a healthy body. Of course, the cultivation of a full-fledged human or animal organ, in my opinion, will not be possible very soon. However, there is already a colossal breakthrough in this environment – the creation of microtissue for individual selection of drug therapy during the treatment of oncological diseases. We are talking about the treatment of complex diseases that require study and selection of drug therapy.
- It turns out that bioprinting is a kind of junction of different disciplines?
- Exactly. Bioprinting is a vivid example of an interdisciplinary approach to solving complex problems. It combines chemistry, physics, biology and technical sciences, this is a kind of convergence of science and technology. To get a finished product, you need to understand its physical and biomechanical properties. I think that in the future there will be a profession, "engineer in the field of biological printing", which will become a logical development of the direction of tissue engineering. These will be interdisciplinary professionals with backgrounds from a variety of scientific fields.
It combines chemistry, physics, biology and technical sciences, this is a kind of convergence of science and technology. To get a finished product, you need to understand its physical and biomechanical properties. I think that in the future there will be a profession, "engineer in the field of biological printing", which will become a logical development of the direction of tissue engineering. These will be interdisciplinary professionals with backgrounds from a variety of scientific fields.
– How is 3 D bioprinting performed?
– The process can be divided into 3 main stages: pre-bioprinting, bioprinting, post-bioprinting. The first stage is preparatory, drawing up a model for printing. For example, our task is to print a three-dimensional organ. We take CT scans and compile them into a 3D model. The second stage is direct printing using bioink: we load the model into the printing program and get a construct consisting of a hydrogel and living cells.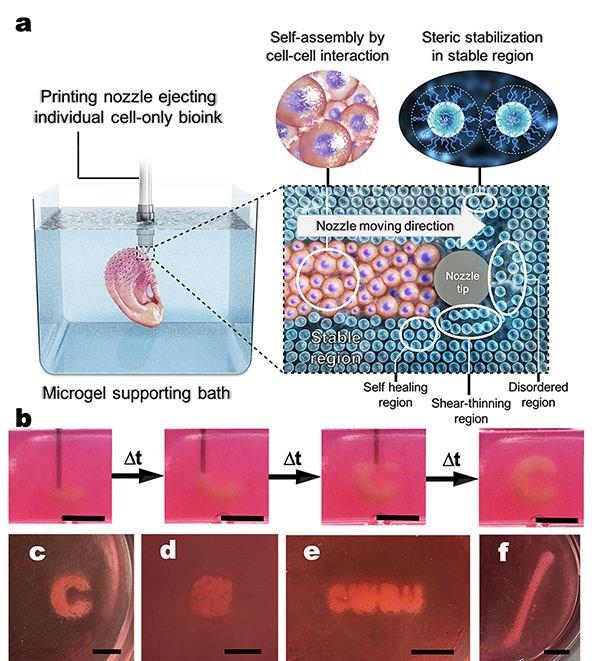 This process itself is very fast, it takes a maximum of several tens of minutes, depending on the complexity of the model. The third, post-bioprinting, we take the construct and place it in a CO2 incubator, where conditions are created, as in a living organism, that is, a temperature of 37 degrees and 5 percent carbon dioxide. Cells begin to grow, and as a result we get, for example, microtissue.
This process itself is very fast, it takes a maximum of several tens of minutes, depending on the complexity of the model. The third, post-bioprinting, we take the construct and place it in a CO2 incubator, where conditions are created, as in a living organism, that is, a temperature of 37 degrees and 5 percent carbon dioxide. Cells begin to grow, and as a result we get, for example, microtissue.
– Is it possible to use 3 D bioprinting in areas other than medicine?
– Yes, definitely. We are now actively working to expand the horizons of 3D bioprinting. Relatively recently, such a concept as green bioprinting appeared in the world, in which not animal and human cells, but plant cells are used as living cells in bioink. We have already carried out several successful experiments using the well-known unicellular green alga Chlorella 9 as a model organism.0317 (note - photo 2,3) . Why do we need it? First, chlorella can be used in the agro-industrial complex for plant germination. Secondly, chlorella has been actively used since the middle of the 20th century as an oxygen generator in closed ecosystems. To date, there are a number of scientific publications showing the possibility of using chlorella as an oxygen satellite for working with animal cells.
Secondly, chlorella has been actively used since the middle of the 20th century as an oxygen generator in closed ecosystems. To date, there are a number of scientific publications showing the possibility of using chlorella as an oxygen satellite for working with animal cells.
- How did you personally come to 3 D - bioprinting?
– Since 2016, I have been actively involved in additive technologies, and bioprinting is one of the types of such technologies in which we add material, and do not subtract, as in traditional types of production (milling, etc.). Already in 2016, I came to the conclusion that in order to achieve high-quality results, you need to leave your comfort zone. My comfort zone was exclusively engineering technology. Therefore, I decided to combine engineering technologies, the background that I already had, with biology and chemistry. The result was printers developed last year for scientific purposes. Already in 2019In 2009, we attended a scientific conference on 3D bioprinting in the city of Nantes (note - France), where we presented a model of a budget bioprinter. The production cost of such a printer is in the range of $150, while the cheapest commercial printer costs several thousand.
The production cost of such a printer is in the range of $150, while the cheapest commercial printer costs several thousand.
– What is currently happening in the field of 3 D -bioprinting in Russia and in the world?
– The industry is new, and today there are about 10 active companies in the world that produce full-fledged installations for 3D bioprinting. Just over 100 companies and entrepreneurs involved in 3D bioprinting have been registered. For the world market, this is very small. The market is quite complex: it is not enough to learn how to print any constructs, you need to understand what their future fate is, where it will be used. There is only one company in Russia that is actively involved in bioprinting - 3D Bioprinting Solutions. These are the founding fathers of Russian bioprinting, who have done a lot for 3D bioprinting and continue to develop it in our country. DSTU today is very active in this direction. We have many interesting projects planned.