3D printer knee replacement
A safer-than-ever joint replacement
Every year in the United States, more than one million people undergo total joint replacement surgeries. That number only increases as the older adult population grows and as the age at which people have these procedures drops. According to projections, by 2030 some four million Americans will receive new joints annually.
Joint replacement surgery is an effective solution for end-stage arthritis in terms of cost and clinical outcomes, but it’s not perfect. Minor variations in an implant’s placement and fit can make all the difference when it comes to residual joint pain after surgery; joint function; and the lifespan of the new joint.
Surgeons in Yale’s Department of Orthopaedics and Rehabilitation are pioneering computer modeling software and 3D printing to plan for and execute joint replacements with increased precision. The technologies reduce risks for older patients and lead to better outcomes and faster recovery.
3D technology in joint replacement surgery
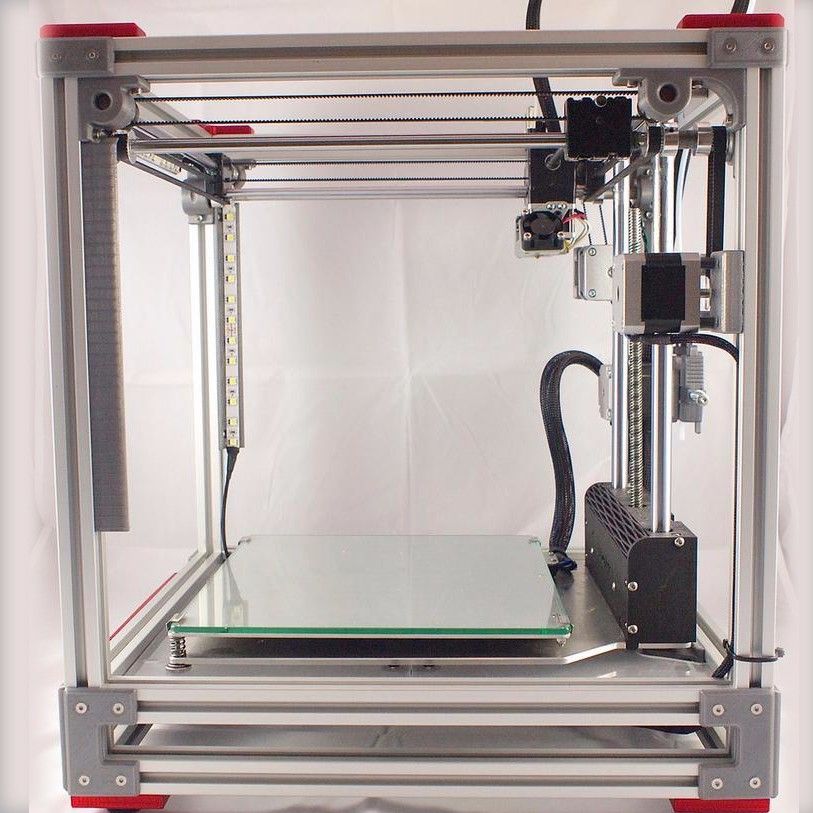
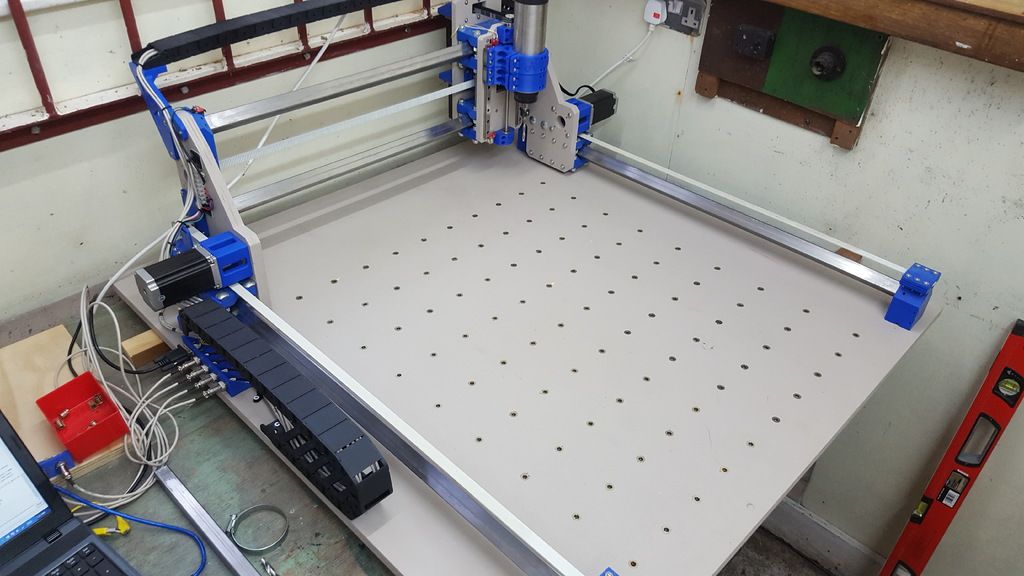
3D printing, also known as additive manufacturing, is the process of creating a three-dimensional object by layering the material into the desired shape. The printer dispenses liquefied building materials as if they were ink. The method uses less material than so-called subtractive manufacturing, in which an object is cut out of a larger piece of material. The beauty of the technology in orthopaedics is that a 3D printer can create custom implants and patient-specific surgical instrumentation based on imaging of a patient’s affected limb.
“A 3D-printed implant we source from vendors allows us to customize the size of the plastic insert and cut out the smallest amount of the patient’s bone,” said Mary O’Connor, MD, director of the Center for Musculoskeletal Care at Yale School of Medicine and Yale New Haven Health. “In knee replacement surgery, this type of implant is closer to normal anatomy of the original joint.”
“In knee replacement surgery, this type of implant is closer to normal anatomy of the original joint.”
Imaging studies also enable surgeons to generate 3D computer-simulated models of patients’ joints, such as a shoulder, and rehearse the surgery virtually with different off-the-shelf implants until they find the perfect one. Based on the virtual surgery, the surgeon can order 3D-printed patient-specific guides and cutting blocks to ensure precision in bone resection and placement of implants.
“In a shoulder replacement, millimeters or a few degrees can make the difference between a replacement that lasts decades and one that only lasts a few years. By generating a patient-specific guide based on a 3D model, we’re able to put the implant in the perfect position at the time of surgery,” said Ken Donohue, MD, assistant professor of orthopaedics and rehabilitation.
Custom-planned surgeries
In older adults, past injuries compounded by a lifetime of wear and tear can damage an ankle. But with the help of the subtalar joint just under the ankle, it can compensate for quite some time. This compensation has the downside of often causing severe deformities of the ankle joint itself. Eventually though, pain pushes a person to do something about it. By this point, the ankle has become so deformed and misaligned that it can be hard to visualize the original joint surface.
Raymond Walls, MD, assistant professor of orthopaedics and rehabilitation, uses preoperative CT scans and X-rays to determine the ideal alignment for ankle replacement surgery. For many years, ankle fusion was the only option for end-stage ankle arthritis because early implants did not perform well. “A better understanding of ankle kinematics as well as advances in implant technology and design means that current fourth-generation ankle replacements are now on a par with hip and knee implants,” said Walls.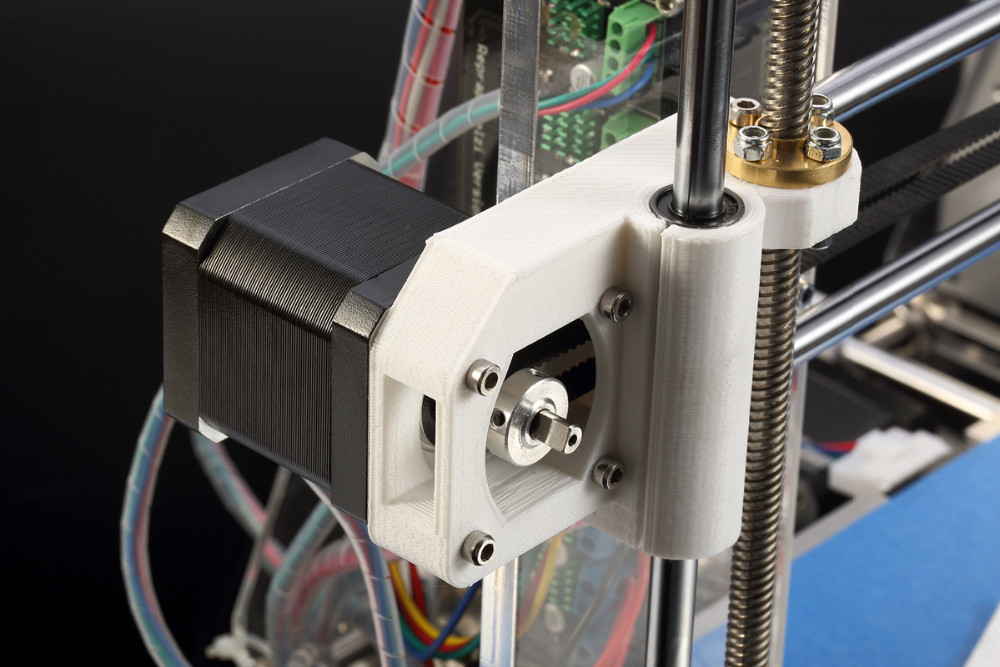
Walls works with Wright Medical Technology, a global medical device company. Wright provides a virtual 3D model of the perfectly aligned ankle with the implants inserted, and a surgical guide that identifies bone cysts and bone spurs that must be addressed to prevent early failure. After Walls approves the plan, he receives custom 3D printed patient-specific guides and a model of the patient’s arthritic joint. During surgery, the surgeon places the guides, which are developed for every patient to fit their unique anatomy, directly on the patient’s bone. This process determines the exact placement of the cutting blocks to remove the precise amount of bone required for the implants. It decreases the risk of implant malalignment, which was previously a common cause of failure.
“We can predict the result we’re going to get preoperatively, and it allows me to use a smaller incision with less soft tissue dissection,” said Walls. This prediction is safer for the patient; makes for a faster surgery; and in general, a faster recovery. A smaller incision also lowers the risk of wound complications and has a better cosmetic appearance once everything has healed.
This prediction is safer for the patient; makes for a faster surgery; and in general, a faster recovery. A smaller incision also lowers the risk of wound complications and has a better cosmetic appearance once everything has healed.
In shoulder replacement surgery, precision is crucial to the life of the implant. An implant that tilts too far back into the cup-shaped glenoid cavity can lead to early loosening and failure of the new joint. But a surgeon can’t visualize the placement of the original joint in surgery. “During surgery, you can’t see the scapula. You’re looking only at the surface of the glenoid. The relationship between the glenoid—the surface of the cup side of the joint—and the scapula is only known by diligent preoperative planning,” said Donohue.
For Donohue, that planning includes a 3D-printed model of the patient’s scapula. The model provides the surgeon with a unique opportunity to study the patient’s anatomy outside the body. Along with 3D computer modeling software, Donohue uses the model in preoperative planning as well as to run through the surgery in real time in the OR.
Along with 3D computer modeling software, Donohue uses the model in preoperative planning as well as to run through the surgery in real time in the OR.
“In the operating room, we will hold the model of the patient’s scapula or glenoid, and position the patient-specific guide on that model to make sure that we have the correct orientation,” he explains. “Then we put the patient-specific guide directly on the patient’s scapula to allow us to put the implant in the proper position.”
Improper placement of an implant is a preventable complication of total joint replacement surgery that 3D printing and modeling software can resolve, said Daniel Wiznia, MD, assistant professor of orthopaedics and rehabilitation. Wiznia was trained as a surgeon to use these technologies, along with robotics and computer navigation, and he believes that as future surgeons come through their training, these technologies will become the standard of care.
“Accuracy and precision are far higher when you’re using technology for a total knee replacement,” he said. “So, if you’re using computer navigation, robotics, or 3D-printed instruments, you will have a far more accurate, consistent result. You’re not going to have as many outliers where you might have positioned the implant in a less than perfect position otherwise.”
Custom-designed joints
Even with technological assistance for implant placement, off-the-shelf joints aren’t a perfect fit for everyone. After knee replacement surgery, patients may end up with what’s called “implant overhang,” in which the implant hangs over at least one side of the femur by three millimeters or more. “If there’s improper fit or sizing and the metal component of the knee replacement overhangs the native bone, that can be a source of residual pain,” O’Connor said.
Studies show that some 40% of men and a whopping 68% of women can have some degree of implant overhang. “Women do not do as well with knee replacement surgery as men,” O’Connor said. She addresses overhang and other potential drawbacks of off-the-shelf implants with 3D-printed knee implants. O’Connor works with Conformis, Inc., a Massachusetts-based manufacturer of custom-made joint replacements, to create personalized implants based on CT scans of patients’ legs from hip to ankle. The orthopaedic surgeon is particularly interested in getting this technology to women who could perhaps benefit most from the custom-designed joints.
“I see women in the clinic who share that they feel their orthopaedic surgeon didn’t listen to them regarding their knee pain. At Yale, we really try to listen and understand the impact of their knee pain on their quality of life,” she said. That was the case for Cheryl Elrick, of Clinton, Connecticut, who didn’t feel her previous orthopaedic surgeon was a good match for her. When she learned about a female surgeon who uses custom-made joint implants, she said, “It was a no-brainer.”
When she learned about a female surgeon who uses custom-made joint implants, she said, “It was a no-brainer.”
“It’s formed to your joint, it’s personalized. The tools, the inserts, are all specifically for you. Why would you do it any other way?” Elrick said. Elrick, who is 67, had lived with debilitating knee pain for 15 years. A registered nurse retired from the neonatal intensive care unit, she is a sought-after babysitter on her block. But less than a year ago, she couldn’t bear to walk across the street to her babysitting job. She had to drive the few hundred feet from her door to the neighbor’s. Now, just six months after her second knee surgery, Elrick is back to babysitting, walking her dog, gardening—all the things she had forgotten how to do without first loading up on ibuprofen. She forgets that she has artificial knee joints.
Elrick’s results may be due to stability that can be more reliably achieved with a custom knee implant. A custom implant, O’Connor said, gets the ligaments in the knee closest to the tension they had with the original joint. Achieving that perfect tension means a more stable joint throughout the range of motion—not just when the leg is held straight.
A custom implant, O’Connor said, gets the ligaments in the knee closest to the tension they had with the original joint. Achieving that perfect tension means a more stable joint throughout the range of motion—not just when the leg is held straight.
Elrick has nearly regained full range of motion in both her new knees. “It’s just incredible that I can do it,” she said. “Getting this knee replacement is the best thing I’ve ever done in my life, for sure—well, after getting married and after my two kids. It’s the fourth best thing.”
How 3D printing and robots improve knee replacement surgery
Stryker’s Triathlon implant has four components (from top): femur, patella (attached to the femur), liner, and tibia. Images: Stryker
Total knee replacement surgery has intrigued me since 1979, when my grandfather had the procedure performed on both knees. The prostheses of that era were designed to anatomically mimic the motion of a knee joint, making them superior to their hinge-action predecessors of the ’60s.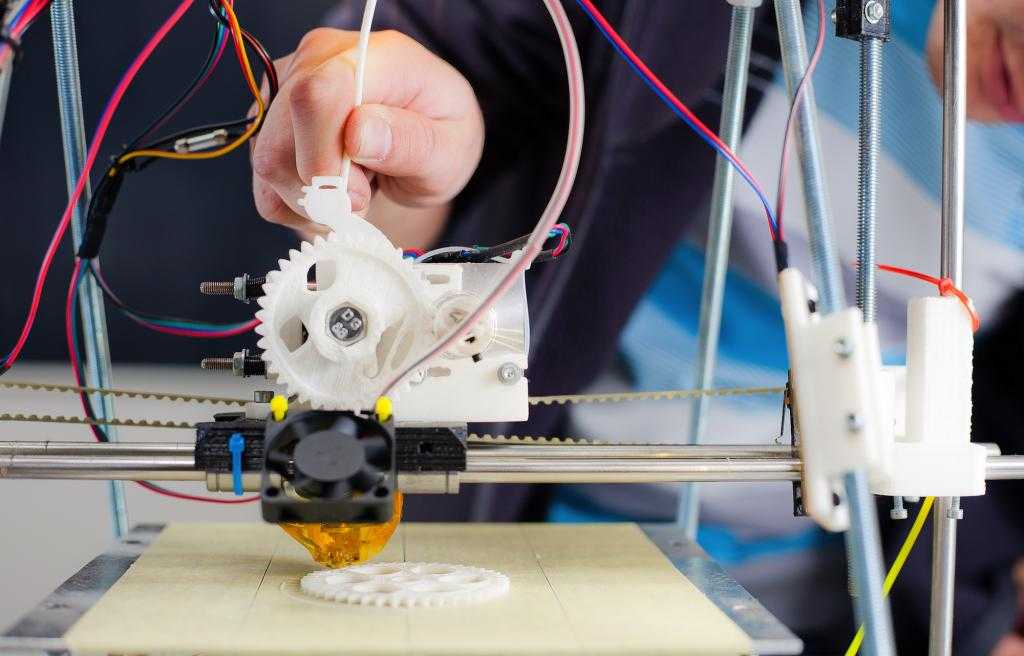
But as I’ve discovered since undergoing my own knee replacement surgery last November, today’s prostheses, surgical techniques, and patient outcomes have vastly improved since Gramps was rolled into the operating room. Advancements in what’s medically known as total knee arthroplasty (TKA) include materials developed specifically for implants and their 3D-printed components, as well as the use of surgical-assist robots.
To learn more about TKA and 3D printing’s role in producing implants, I contacted Stryker Corp., the manufacturer of my new knee and the robot that assisted with its implantation.
I spoke with Robert Cohen, president of Stryker’s Digital, Robotics, and Enabling Technologies entity. Cohen, who earned multiple engineering degrees at New Jersey Institute of Technology in the 1980s, has spent his career manufacturing implants. He also has unfettered enthusiasm for how digital technologies like 3D printing help engineers improve TKA surgery, with “help” being the operative word.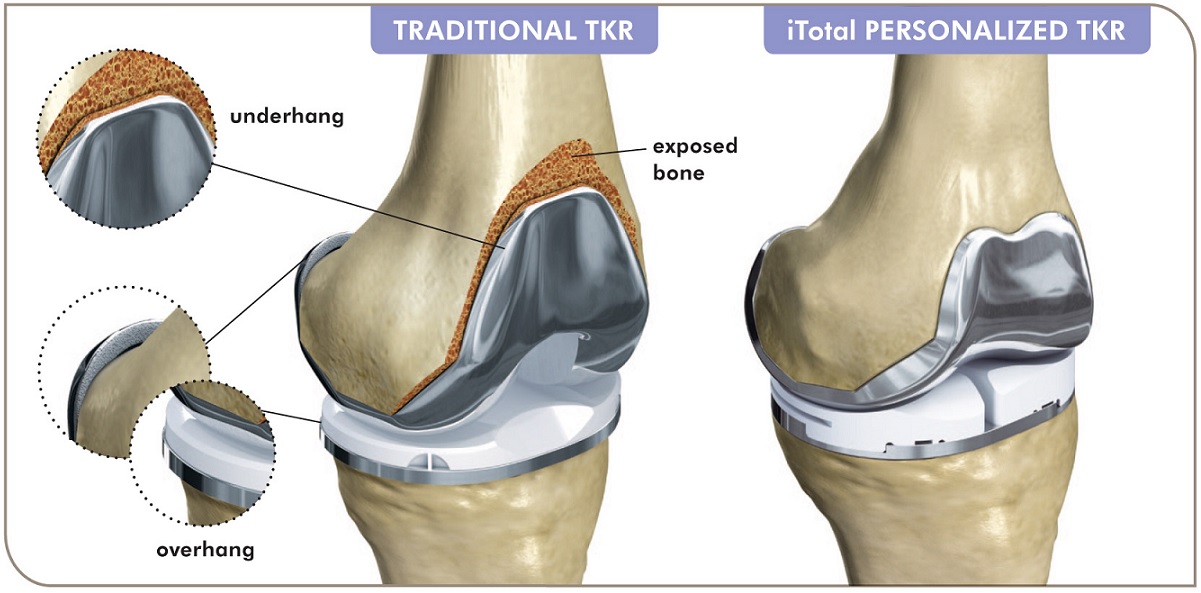
He describes additive manufacturing as a “tool” that aids engineers in discovering solutions to problems that can’t be solved by conventional manufacturing methods. “3D printing by itself is nothing but fancy printing—another way to manufacture.”
What drives innovation are the “skillsets of people who want to solve problems in new ways and come up with, in our case, new implants. 3D printing is the enabler that [makes their] designs reality,” he said.
Stryker began adopting additive manufacturing technologies in 2002. Besides knees, the global corporation headquartered in Kalamazoo, Mich., also 3D-prints hips, spinal cages, and other implantable devices. AM allows the company to produce prosthetic geometries that would be impossible or impractical to manufacture by traditional methods. An example is additively manufactured scaffolds that promote biologic fixation—the growth of bone into a prosthetic.
“3D printing is the only way to do that,” said Cohen. “Bone wants to grow into something. Instead of just doing a line-of-sight process, where you might drill holes, and say, ‘Hey, bone, I hope you grow into the holes.’ Now we can print a scaffold structure and bone will grow into it, and the scaffold has structural integrity at the same time. Just like a railroad trestle.”
Instead of just doing a line-of-sight process, where you might drill holes, and say, ‘Hey, bone, I hope you grow into the holes.’ Now we can print a scaffold structure and bone will grow into it, and the scaffold has structural integrity at the same time. Just like a railroad trestle.”
Growth of TKAs
I wasn’t the only passenger who boarded the TKA train last year. It’s estimated that more than 600,000 Americans annually receive the surgery—a figure expected to rise in the coming decade. The combined number of hip and knee replacement procedures in the U.S. is about 1 million yearly.
My surgical team at NorthShore Medical Group-Skokie, outside Chicago, used Stryker’s Triathlon total knee system and was assisted by the medical device manufacturer’s Mako surgical robot. The cementless implant incorporates a femur, tibia, patella, and polyethylene liner.
The Triathlon’s additive components are made from a titanium alloy Stryker developed for 3D printing.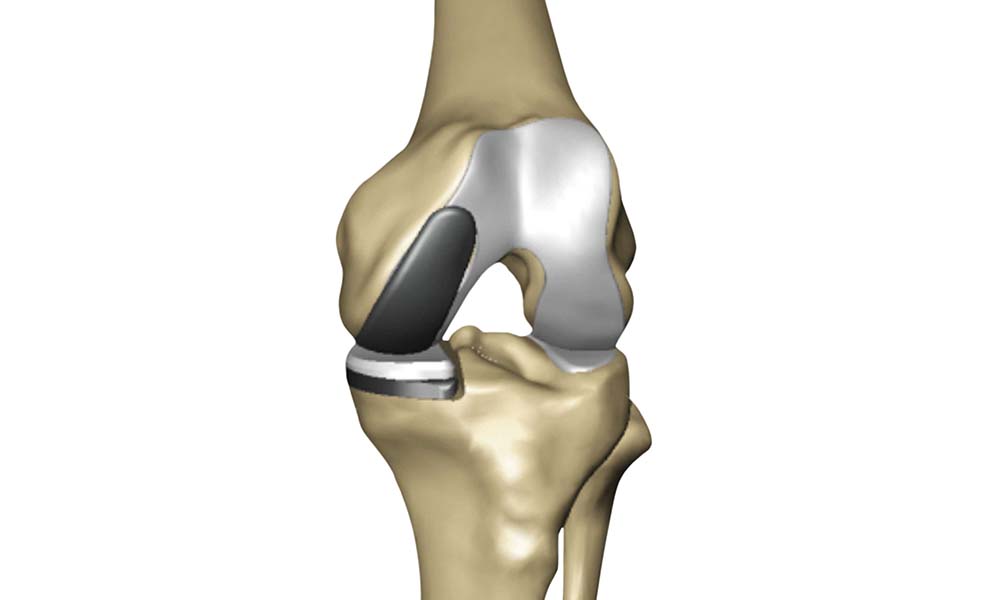
The use of cementless knees has grown rapidly the past few years. The reason is because bone cement, long used for TKA surgeries, is an interface that can break down, said Cohen. “It’s another opportunity for the implant to loosen.”
Stryker casts the femoral component of a Triathlon knee from cobalt chromium, a material that interacts well with the plastic liner. After casting, the femur is finish-machined and coated with sintering beads that promote bone ingrowth.
During TKA surgery, a series of box cuts are made on the patient’s femur. The two cuts on the end interface with the implant like a wedge being pounded into a piece of wood. “That’s the most stable surface ever,” said Cohen. “Think about it. You’re standing up, so you’re always sort of pushing the [bone] tighter into place.”
Producing the patella is a comparatively straightforward process. The metal-backed patella is fitted with a 3D-printed geometry made from Tritanium, a titanium alloy Stryker developed specifically for AM applications in which bone ingrowth is desirable.
Tritanium also is used to 3D-print the tibial baseplate. It forms a virtually fail-proof bond with the patient’s tibia using an interference-fit connection, a force that relies on friction to hold together two mating, tightly fitting objects. The main features of the metal baseplate’s design are four pegs and a keel.
Cohen said, “With additive manufacturing, we can put those posts and keel where they’ll all work together to create an interference fit.” It is “rock solid.” He added that machining the baseplate couldn’t be justified economically. “The cost would be outlandish.”
Manufacturing Overview
For AM applications, Stryker mostly uses direct metal laser sintering (DMLS) printers. “We were doing some electron-beam processes for larger metal parts,” said Cohen, “and we’re looking at different printers for [complex] jigs and fixtures and for disposable instruments and polymers. There are some polymers that could be used for an implant, and there are some polymers that could be single-use surgical instruments, depending on the material requirements. ”
”
Selecting and bringing a 3D printer online to build prostheses is a major undertaking. In the world of metal load-bearing implants, it would be unrealistic to buy a DMLS printer, plug it in, and expect to make an implant.
Printing metal implants requires learning to control the laser, melt pool, wattage and feeds, layering, and many other process parameters. “Because we’ve built competencies in those areas,” said Cohen, “we’re one of the few companies in health care, in the world, that has the capability to scale up and not just do small-run production.”
The corporation’s scaling capabilities have been augmented by its AMagine Institute, a global technology development center located in Cork, Ireland. Reportedly the world’s largest facility dedicated to additively manufacturing orthopedic components, Cohen said the institute’s production personnel 3D-print more than 1 million parts annually.
A view of how implant components fit on a patient.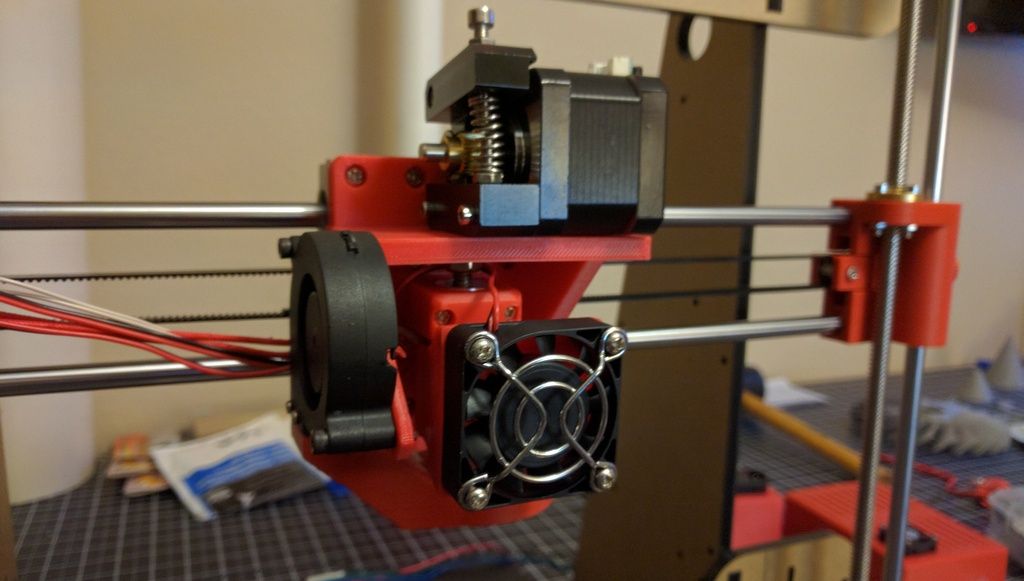
Robot-Assisted Surgeries
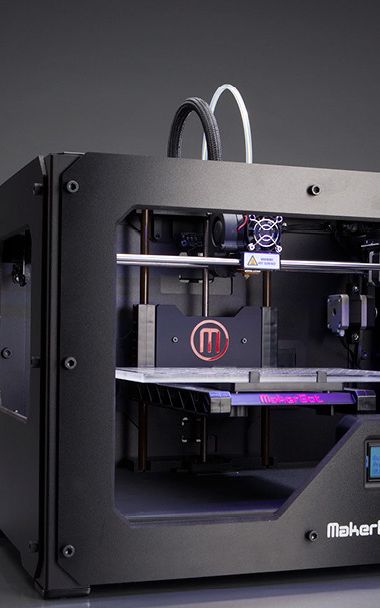
A much smaller though equally impressive sum is 1,000—the number of Mako robot-assist systems Stryker has placed in hospitals the past three years. A Mako robot, which costs more than $1 million, according to published reports, is used to implant Triathlon knees. The system determines final bone preparation and implantation steps to be executed with special Triathlon instruments.
Cohen said 42% of the primary knees that Stryker sells in the United States are implanted with a Mako robot. He expects the percentage to rise to 50% soon.
As is the case with learning to 3D-print TKA components, developing a surgical robot isn’t a task for the impatient or inexperienced. Cohen said, “We design the robots. We write the software, and we build the robots ourselves because nobody else can do it. We have worked on this for over a decade.”
A key benefit of the robotic system is that it provides the surgical team unprecedented amounts of data about the patient’s knee before and during surgery. The process starts with the hospital taking a CT scan of a patient’s knee prior to admittance. The hospital sends the scan to Stryker, which creates a virtual 3D model of the knee joint, tibia, femur, patella, cartilage, and ligaments. The scan also reveals useful information like the amount of arthritic damage the patient has incurred and joint-space narrowing caused by cartilage loss.
The process starts with the hospital taking a CT scan of a patient’s knee prior to admittance. The hospital sends the scan to Stryker, which creates a virtual 3D model of the knee joint, tibia, femur, patella, cartilage, and ligaments. The scan also reveals useful information like the amount of arthritic damage the patient has incurred and joint-space narrowing caused by cartilage loss.
The next step is to match the data with a virtual implant. Stryker team members position virtual models of the femur and tibia on the virtual bones and gather data on rotation, X-Y-Z axes, tilt, slant—“everything you could possibly need to match you is individualized,” Cohen explained. The team also re-establishes the patient’s joint line, in three dimensions.
“The purpose of the robot is to get your knee exactly on your joint line … and to make surfaces that last your lifetime,” said Cohen.
Once all the data is gathered, Stryker bundles it into a plan for the surgery that is sent to the surgeon. The plan is loaded into the robot before the patient enters the operating room. But it’s not the final surgical plan, Cohen pointed out. While the patient is under anesthesia, the surgeon bends the TKA knee and the robot tracks the bending action.
The plan is loaded into the robot before the patient enters the operating room. But it’s not the final surgical plan, Cohen pointed out. While the patient is under anesthesia, the surgeon bends the TKA knee and the robot tracks the bending action.
“So let’s say your ligaments are a little bit too loose, and the surgeon running the robot looks at the screen and says, ‘Ah, you know, the medial [collateral ligament] is a little bit lax. So we’re going to move the tibial component up a little bit, twist the femur, and now let’s flex the knee again—virtually—and see what the end surgery would look like in terms of flexion.’ ”
Once the plan has been fine-tuned and completely individualized, it’s locked in and surgery commences.
During the operation, the robot controls the motion of surgical instruments. For example, as the surgeon pushes a saw into a bone, the robot controls the plane of the blade and executes the cut with an accuracy and precision unseen in surgery before, said Cohen.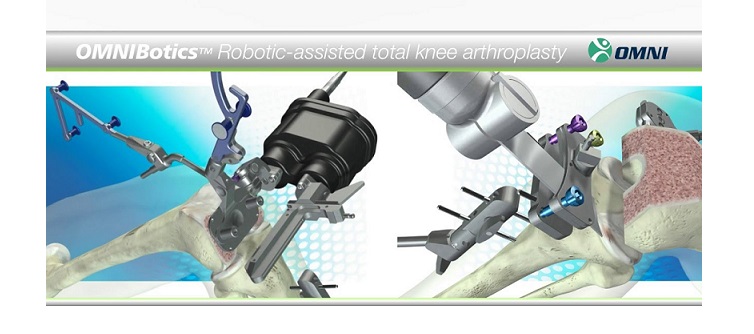
Robert Cohen, president of Stryker’s Digital, Robotics, and Enabling Technologies entity, has spent his entire career manufacturing prostheses.
The forward progress of the blade is controlled too. This prevents it from entering healthy tissue once the bone has been cut clean through. “We have haptics built into the robot arm,” said Cohen. “The saw stops automatically when you hit the bone’s boundary. We create a bubble, a safety zone.”
Better Outcomes
From the patient’s perspective, the biggest benefit of robot-assisted surgery is a shorter recovery time. This is largely a result of minimizing damage to healthy tissue and proper placement of the prosthetic.
Cohen said, “When you wake up [after surgery], you’re flexing in the right spot. You don’t have to relearn to walk, like in 1979 when implants were put in the wrong spot. Now you have less physical therapy sessions. You return to flexion earlier.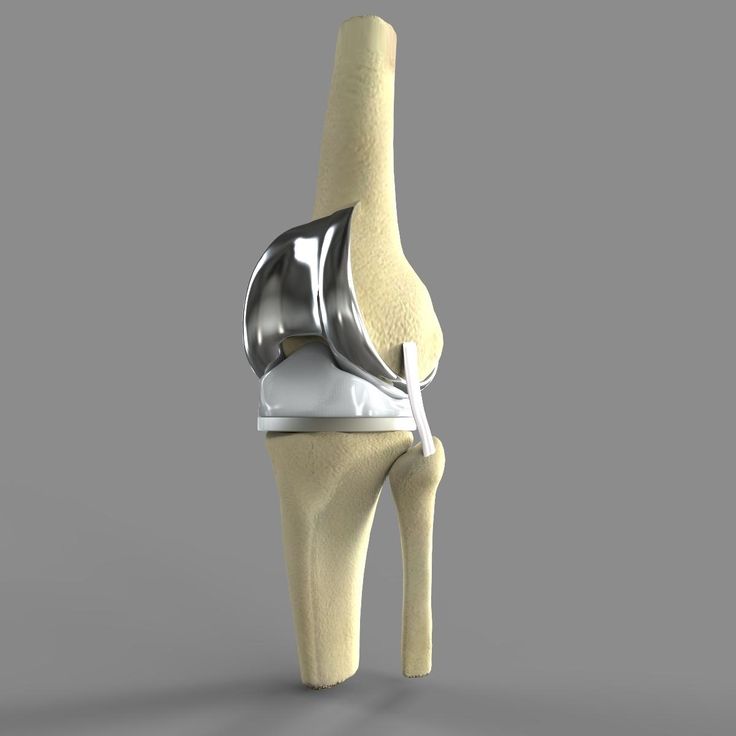 You get relief from pain sooner because you didn’t have as much soft-tissue trauma. You can go back to work sooner. You don’t have any of the health issues.
You get relief from pain sooner because you didn’t have as much soft-tissue trauma. You can go back to work sooner. You don’t have any of the health issues.
“There are fewer re-admissions and re-operations. You have higher patient satisfaction.”
Personal Outcome
TKA surgery is major surgery. More “majorly” than I imagined before entering the hospital last November. (A bit of unsolicited advice: If you’re contemplating knee surgery, don’t watch a YouTube video of the procedure before the operation. Wait until after.) My biggest takeaway from the experience is that the return to mobility was much faster than expected.
My grandfather was bed-ridden for more than a week after his TKA surgeries. He spent weeks in rehabilitation before he was able to walk—with the aid of a walker. And although the implants greatly enriched his life, he needed two canes to get around for the rest of his days.
The circumstances surrounding my TKA surgery were different than my grandfather’s.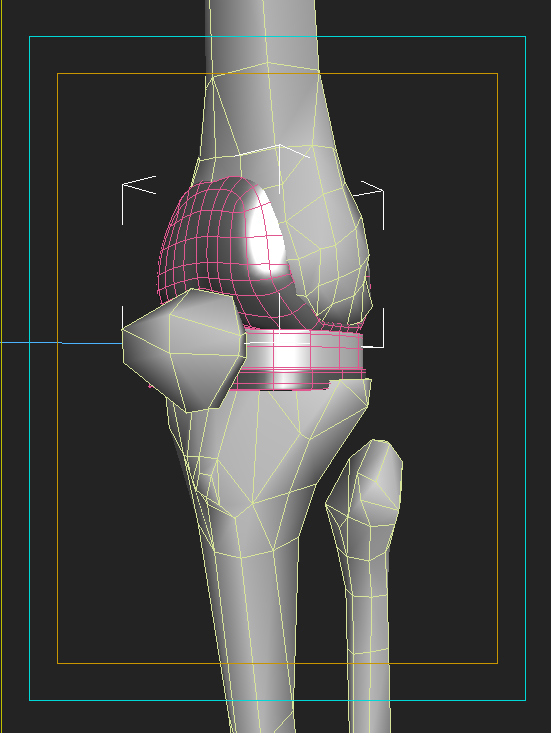 I was nearly 20 years younger, and I only had one knee operated on. I also was a “good” candidate for the surgery in that I was fit and had regularly done exercises to strengthen the muscles supporting the knee for the 15 years preceding the operation.
I was nearly 20 years younger, and I only had one knee operated on. I also was a “good” candidate for the surgery in that I was fit and had regularly done exercises to strengthen the muscles supporting the knee for the 15 years preceding the operation.
Still, eight hours after the procedure, I easily circumnavigated the orthopedic floor of the hospital with the assistance of a walker. I was discharged from the hospital 24 hours after surgery. And two days after the operation, on Thanksgiving Day, I was able to walk a half mile unaided.
It was a satisfying walk.
SIDEBAR
Knee implant surgery runs in the family
The Mako surgical robot helps prevent damage to healthy tissue and locates the knee implant correctly on the patient’s bones.
I’m not the first member of my family to take a prosthetic knee.
My grandfather had both knees replaced in 1979, at the age of 85. He became one of the earliest adopters of the then-rare procedure so he could continue to tend his garden. My mother-in-law had her knees replaced about 20 years ago, at 65, out of a desire to play tennis and tend to her grandchildren.
My mother-in-law had her knees replaced about 20 years ago, at 65, out of a desire to play tennis and tend to her grandchildren.
The reasons people choose to have total knee replacements today are different than they were 40 years ago. Robert Cohen, president of Stryker’s digital manufacturing entity, said the most common reason is to enhance mobility.
“Thirty years ago, a person 75 years old may have just wanted an implant to relieve pain,” he said. “Now, somebody 75, 80 years old wants to be able to walk a golf course ... sit on the floor with a grandkid and get up off the floor unaided.”
This desire has boosted the number of knee surgeries performed and attracted younger adults who want the procedure. Stryker has manufactured knees for individuals in their 40s, 30s, and even 20s, said Cohen. “We had someone who has a partial knee who rides in the Tour de France.”
No member of my family has qualified to compete for the yellow jersey, but those of us who have had the surgery were glad we did.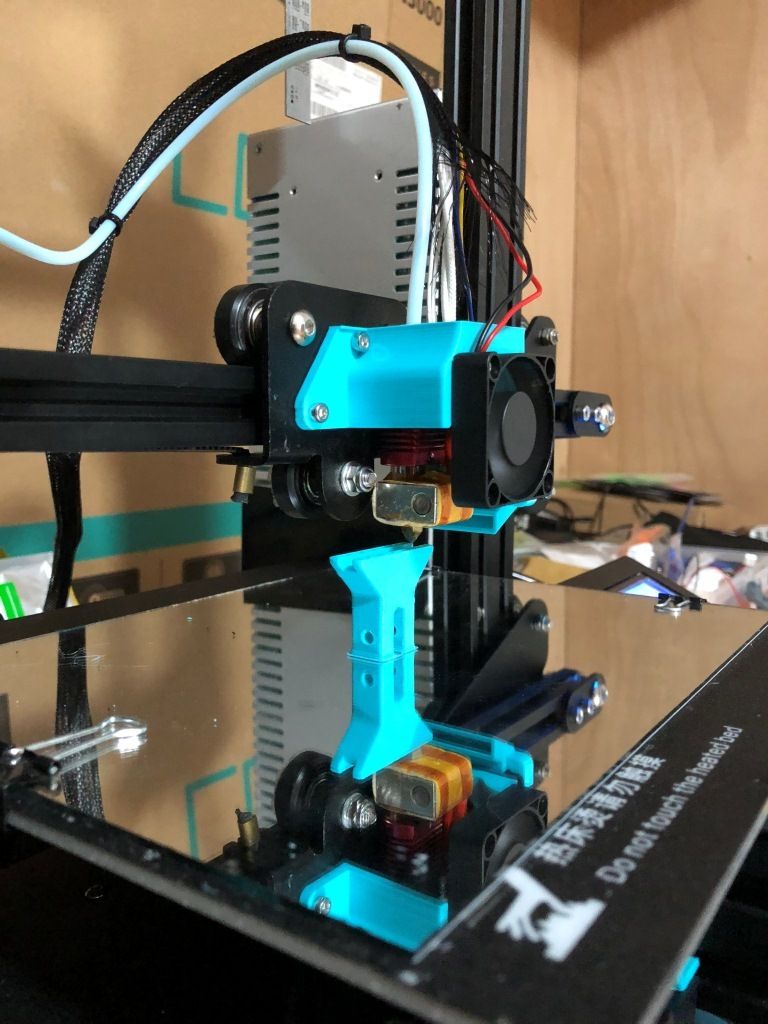 My grandfather worked in his garden until he died, at 96, and my mother-in-law still plays tennis and keeps up as best she can with her now-adult grandchildren.
My grandfather worked in his garden until he died, at 96, and my mother-in-law still plays tennis and keeps up as best she can with her now-adult grandchildren.
My main reason for having the procedure was to continue my regimen of walking three to five miles a day without pain. Five months after surgery, I’m back to walking three miles daily pain-free. –D. Nelson
Hip arthroplasty using a 3D printer for the first time in Israel
In recent years, a real revolution has taken place in the field of joint replacement in the world. Increasingly, scientists are talking about the possibilities of 3D technologies, which make it possible to design an accurate three-dimensional model of a human organ in accordance with its anatomy in a computer and print it from biological material. For the first time in Israel, the Soroka hospital performed a knee replacement operation using a modeled and printed joint.
Author Elena Levina
When traditional treatments - physiotherapy, drug therapy - do not help, when joint pain turns into a constant, ongoing nightmare - perhaps the next step should be surgery to replace the affected joint. In recent years, a real revolution has taken place in the field of joint replacement in the world.
In recent years, a real revolution has taken place in the field of joint replacement in the world.
Medical revolution - 3D technology
Increasingly, scientists are talking about the possibilities of 3D technologies, which make it possible to design an accurate three-dimensional model of a human organ in accordance with its anatomy in a computer and print it from biological material. For the first time in Israel, the Soroka hospital performed a knee replacement surgery using simulation.
When a joint replacement is required
If joint pains are repeated, and you know that the reason for this is not physical exertion on the limbs, then most likely we are talking about one or another type of arthritis - inflammation. Most often, diseased joints are in the lower extremities, in the knees, and the hip bones. Sometimes the only solution is surgical replacement of damaged joints.
The average age of patients with recurrent joint pain, other than injury or accident, is approximately 60 years or older. Due to natural wear and tear and degenerative processes in the body that occur with age. Joint replacements may also be needed for younger people who have suffered fractures and injuries from sports or accidents where surgery is the only option.
Due to natural wear and tear and degenerative processes in the body that occur with age. Joint replacements may also be needed for younger people who have suffered fractures and injuries from sports or accidents where surgery is the only option.
Joint replacement surgery with 3D printers already in Israel!
Ami Asis, a resident of the south of the country, was the first patient in Israel and one of the few in the world whose damaged joint was replaced with a new one created using a 3D printer. Ami, who for many years suffered from pain in the hip joint and lameness, had long dreamed of replacing the damaged joint, but he knew that such operations are very difficult, require high qualification and experience from the doctor, complications are possible due to inaccurate selection of the implant . Dr. Vadim Benkovich, head of the Department of Joint Replacement at the Soroka Hospital in Beersheba, suggested that he implant a 3D-printed implant.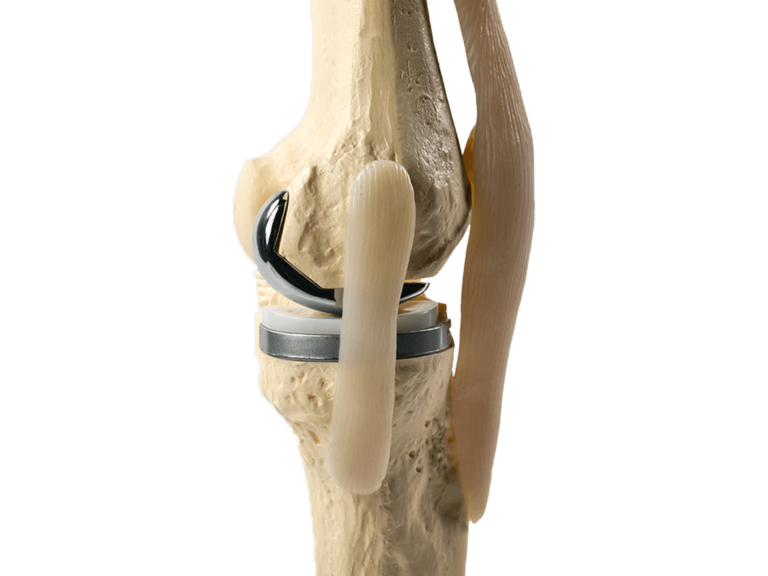 After some hesitation, Ami agreed to the procedure. The operation was performed at Soroka hospital in Beer Sheva and took about 30 minutes.
After some hesitation, Ami agreed to the procedure. The operation was performed at Soroka hospital in Beer Sheva and took about 30 minutes.
One-on-one model
Creating a prosthesis in accordance with the individual measurements of the patient, which would exactly repeat the anatomy of his joint, is the basis of a new method of creating an implant using 3D printers. Before the operation, the patient undergoes visual scanning procedures: MRI and CT, but not for a diagnostic examination, for which these procedures are intended, but to recreate an accurate three-dimensional model of the joint. This creates a one-on-one model of the problematic organ to be replaced. This exact copy allows doctors to plan all actions to the smallest detail, to select the adapted equipment suitable for each specific case. Orthopedics in Israel is advancing by leaps and bounds - the doctors of the country have tried various methods of surgery and materials from which implants were created.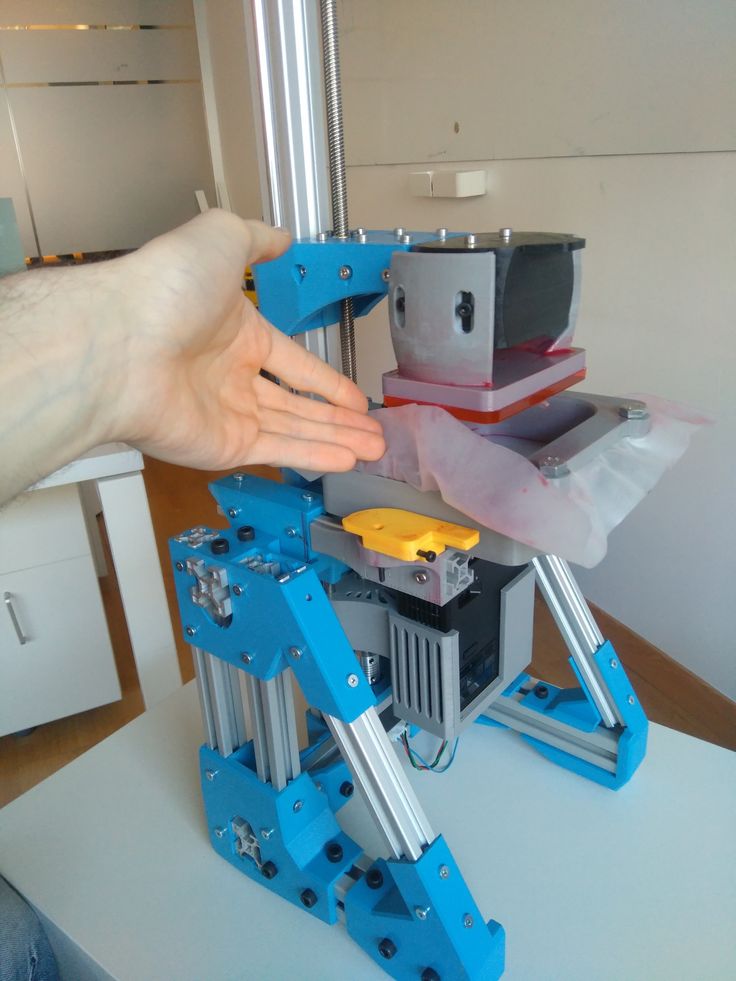 But the patient's recovery process was always very slow and painful.
But the patient's recovery process was always very slow and painful.
Benefits of using a 3D printer in orthopedics
The advantage of creating a joint model using a 3D printer is that it allows for a very high level of accuracy and reduces work time. This is important, first of all, because we are talking about the most precise "jewelry" operations, which are carried out in a short time and at a very high professional level. Speaking about the advantages of the method of joint replacement using "opened" organs, it is worth noting that, compared with previous methods, there are no traditional consequences of surgical intervention: tissue is less damaged, less blood loss, the patient recovers faster after surgery. In the case of Ami, we are talking about a fairly short time: only a month has passed since the surgery, he can already drive a car, move around, almost without limping, he has stopped taking analgesics for the last week.
Today, Israeli orthopedists are dreaming of the next stage - to perform the most complex operations on the spine, requiring, for example, the replacement of vertebrae, using 3D organ printing technologies.
Request a treatment quote
Watch video - 2:58 min.
D.R.A Medical Center
With D.R.A Medical Center you get the opportunity to use the services of the best Israeli doctors and receive effective treatment based on your individual needs at the most reasonable cost. Read more
Knee implants on a 3D printer: a new printing technique
Knee implants on a 3D printer
It is not news for a long time that one of the most useful areas of 3D printing for humans, in the future, is medicine. New ways of making prostheses and even organ fragments are constantly being developed. 3D printing can be extremely useful for surgeons and dentists. The development of this 3D printing industry does not stand still, researchers are hard at work on the invention of new printing methods in medicine and optimization of existing ones. For example, scientists create knee implants on a 3D printer that are significantly superior to their traditional counterparts.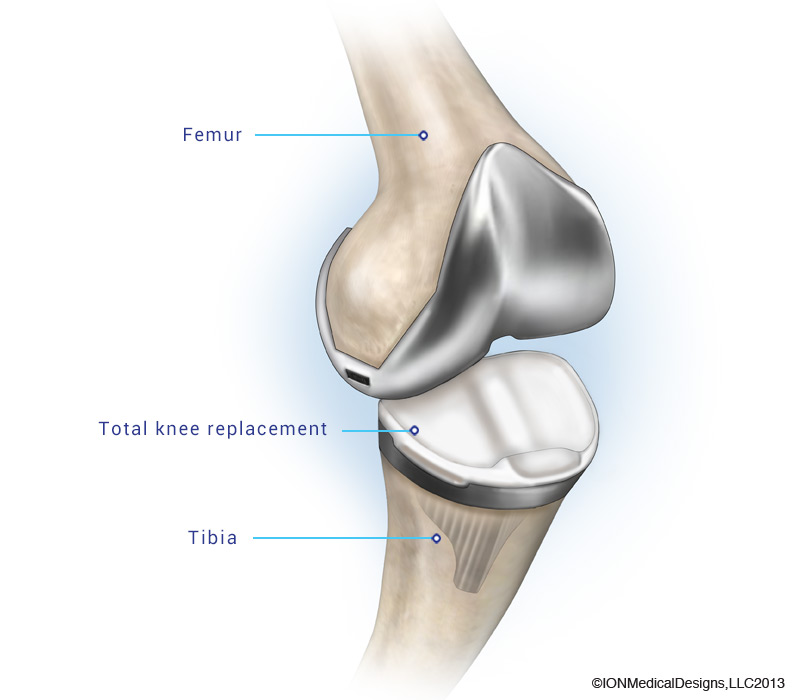
The American company ConforMIS, which specializes in the manufacture of knee prostheses, has developed a radical new technology iTotal. It allows you to create unique knee joints, which, thanks to 3D technologies, provide the ability to adapt to the characteristics of each individual. Knee implants on a 3D printer, created using this technology, contribute to faster healing of the operated area, reducing pain. They also provide greater mobility than standard prostheses currently used by surgeons.
3D printing of knee implants
The technology provided by ConforMIS is quite new, but has already proved to be very effective. Dr. Brian Guber, an American orthopedic surgeon formerly of ConforMIS's scientific advisory department, has been using the system for four years, long before it was widely publicized. During this time, he has gained an excellent reputation as a result of successful knee replacement surgeries; he accepted patients in need of surgery from all over the United States.
Recently, Dr. Huber invited reporters from the independent newspaper Seven Days to oversee one of the patella replacement procedures. The patient was a woman who had problems with her knees due to being overweight. Two months before the operation, a 3D scan of the patient's knee was performed to build a unique model in order to recreate an exact copy of the patella using a 3D printer. After removing the calyx, the doctor replaced it with a 3D printed cobalt-chromium alloy replica.
3D printed knee implants were not the only thing custom made for the patient. Surgical instruments have also been designed specifically based on the female anatomy. Such a well-established and responsible approach to business allowed the doctor to complete the operation in less than an hour. Incredibly, the patient, having gone to the operation at about 10:30, was already able to walk by the evening.
Most of Dr. Huber's patients leave the hospital within 24-48 hours, which is clearly a much shorter time than is required with standard knee prostheses.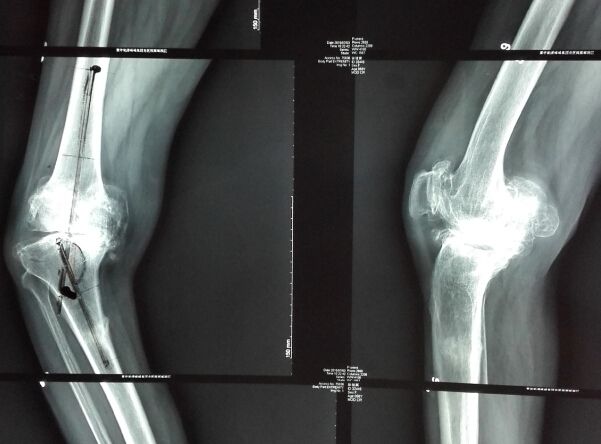 He has operated on many overtrained athletes, and less than five percent of his patients require physical rehabilitation.
He has operated on many overtrained athletes, and less than five percent of his patients require physical rehabilitation.
The future of knee implants on a 3D printer
The benefits of the ConforMIS system are clear. Conventional knee implants are made to measure general anatomy. And this is unthinkable, given how different people can be from each other. According to Dr. Huber, two-thirds of replacement knee prostheses are either too big or too small, limiting mobility and causing chronic pain. In addition to making them generally unprofitable, conventional implants often require additional removal of significant bone fragments. 3D printed knee implants offer the opportunity to save 25-30 percent more bone than standard knee replacements, as well as significantly reduce blood loss.
The role of 3D printing in medicine is truly enormous and new opportunities for its application continue to appear every day. After all, no other technology would allow such an accurate reproduction of the unique parts of the patient's body, especially bones and internal organs.