3D bone printing
Building Better Bones With 3D Printing
This article was originally published in the Northwestern University Feinberg School of Medicine News Center.
A Northwestern University research team has developed 3D printable ink that produces a synthetic bone implant that rapidly induces bone regeneration and growth. This hyper-elastic bone material is easily customizable to different shapes and could one day be especially useful in the treatment of bone defects in children.
Bone implantation surgery is never an easy process, but it is particularly painful and complicated for children. With both adults and children, bone is often harvested from elsewhere in the body to replace the missing bone, which can lead to other complications and pain. Metallic implants are sometimes used, but this is not a permanent fix for growing children.
“Adults have more options when it comes to implants,” said Ramille Shah, PhD, an assistant professor of Surgery in the Division of Organ Transplantation at Northwestern University Feinberg School of Medicine and of Materials Science and Engineering at the McCormick School of Engineering. “Pediatric patients do not. If you give them a permanent implant, you have to do more surgeries in the future as they grow. They might face years of difficulty.”
Shah and her team aim to change the nature of bone implants, and they particularly want to help pediatric patients. Adam Jakus, PhD, a postdoctoral fellow in Shah’s laboratory, is the first author of the study, which evaluated the material with human stem cells and within animal models.
Shah’s 3-D printed biomaterial is a mix of hydroxyapatite (a calcium mineral found naturally in human bone) and a biocompatible, biodegradable polymer. The material is majority hydroxyapatite, yet it is hyper-elastic, robust and porous at the nano, micro and macro levels. These unique properties have contributed to the printed structure’s great promise in in vivo animal models.
“Porosity is huge when it comes to tissue regeneration, because you want cells and blood vessels to infiltrate the scaffold,” Shah said. “Our 3-D structure has different levels of porosity that work to the advantage of its physical and biological properties.”
“Our 3-D structure has different levels of porosity that work to the advantage of its physical and biological properties.”
While hydroxyapatite has been proven to induce bone regeneration, it is also notoriously tricky to work with. Clinical products that use hydroxyapatite or other calcium phosphate ceramics are hard and brittle. To compensate for that, previous researchers created structures composed mostly of polymers, but this shields the activity of the bioceramic. Shah’s bone biomaterial, however, is 90 percent by weight hydroxyapatite and just 10 percent by weight polymer, and it still maintains its elasticity because of the way its structure is designed and printed. The high concentration of hydroxyapatite creates an environment that induces rapid bone regeneration.
“Cells can sense the hydroxyapatite and respond to its bioactivity,” Shah said. “When you put stem cells on our scaffolds, they turn into bone cells and start to up-regulate their expression of bone-specific genes.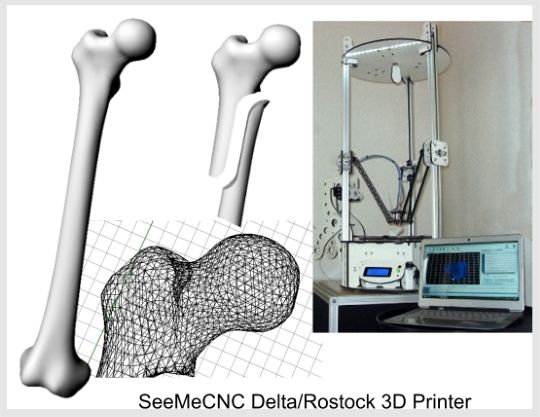 This is in the absence of any other osteoinducing substances. It’s just the interaction between the cells and the material itself.”
This is in the absence of any other osteoinducing substances. It’s just the interaction between the cells and the material itself.”
That’s not to say that other substances couldn’t be combined into the ink. Because the 3-D printing process is performed at room temperature, Shah’s team was able to incorporate other elements, such as antibiotics, into the ink.
“We can incorporate antibiotics to reduce the possibility of infection after surgery,” Shah said. “We also can combine the ink with different types of growth factors, if needed, to further enhance regeneration. It’s really a multi-functional material.”
One of the biggest advantages, however, is that the end product can be customized to the patient. In traditional bone transplant surgeries, the bone — after it’s taken from another part of the body — has to be shaped and molded to exactly fit the area where it is needed. Using Shah’s synthetic material, physicians would be able to scan the patient’s body and 3-D print a personalized product. Alternatively, due to its mechanical properties, the biomaterial also can be easily trimmed and cut to size and shape during a procedure. Not only is this faster, but also less painful compared to using autograft material.
Alternatively, due to its mechanical properties, the biomaterial also can be easily trimmed and cut to size and shape during a procedure. Not only is this faster, but also less painful compared to using autograft material.
Shah imagines that hospitals may one day have 3-D printers, where customized implants can be printed while the patient waits.
“The turnaround time for an implant that’s specialized for a customer could be within 24 hours,” Shah said. “That could change the world of craniofacial and orthopaedic surgery, and, I hope, will improve patient outcomes.”
CT-Bone | 3D printing real bone
Patients requiring skeletal augmentation, for example those with facial asymmetry resulting from either trauma or congenital defects, would be helped best with a bony implant made to match their anatomy. Typical bone augmentation implants are made from alloplastic materials (like PEEK or titanium) or the patient’s own bone is cut and repositioned. CT-Bone® is a bone-like customized implant that can be 3D printed and is converted to real bone by the patient.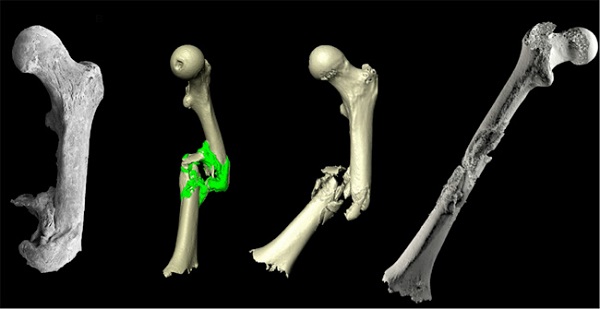
| 3D printed CT-Bone implant for mandible augmentation | 3D printed CT-Bone implant for zygoma augmentation |
After taking a CT-scan of the patient, a patient-specific implant is designed by our biomedical engineers in collaboration with the surgeon. This design perfectly fits on the anatomy of the patient, ensuring good bone-to-implant contact and facilitating bony ingrowth. The design is 3D printed in calcium phosphate, the main constituent of natural bone. The 3D printing process has a very high accuracy, resulting in implants that fit perfectly onto the bone of the patient, as designed. Even very complex shapes and designs can be 3D printed; for example 3D printing enables the production of implants with engineered (controlled) porosity, similar to natural bone. When implanted, CT-Bone® unifies with the patient’s own bone in the next months.
From CT-scan to 3D model to patient-specific implant design
Unlike other 3D printed ceramics (like Hydroxyapatite or Beta-TCP), CT-Bone® does not require a thermal process (sintering) to increase mechanical strength and therefore also displays better bony fusion (sintering increases crystallinity which adversely affects biodegradability).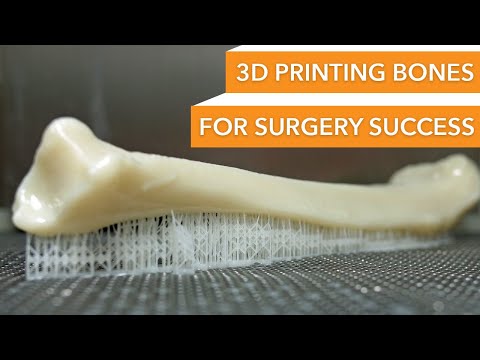 Sintering also causes shrinkage of ceramics which results in a non-optimal fit. Since CT-Bone® does not require sintering it displays better bony fusion and is dimensionally stable, so it keeps a perfect fit.
Sintering also causes shrinkage of ceramics which results in a non-optimal fit. Since CT-Bone® does not require sintering it displays better bony fusion and is dimensionally stable, so it keeps a perfect fit.
Other manufacturing methods typically produce random porosity, whereas the process of 3D printing allows complex shapes and 100% interconnected porosity.
CT-Bone® is brought to you by Xilloc in collaboration with Next21 (Tokyo, Japan) and is awaiting regulatory approval under the new MDR in Europe.
NOTICE
Due to overwhelming interest in CT-Bone®, we are unfortunately unable to answer everybody personally. However you can subscribe to our mailing list.
Comparison: Hydroxyapatite vs CT-Bone
A pre-clinical study clearly shows the difference between an implant from Hydroxyapatite and an implant from CT-Bone®. The CT-Bone® implant really fuses with the original bone. Clinical studies confirm excellent bony fusion (results available upon request).
Clinical studies confirm excellent bony fusion (results available upon request).
| Hydroxyapatite CT-Bone® | |
| Post-op | |
| 4 weeks post-op | |
| 24 weeks post-op |
Further histological investigations showed that in the hydroxyapatite, bone-like tissue was only found in some micropores close to the surface. In CT-Bone®, large bone-like tissues penetrated into the macropores, containing activated osteoclasts, fibroblasts and even blood vessels. In addition, bone marrow formation was observed containing erythroblasts and megakaryocytes.
Bioresorbable vs biodegradable
CT-Bone® is biodegradable by the patient’s osteoclasts and after 3 months CT-Bone® will be fused with the patient’s bone and will remodel in the osteo-cycle. CT-Bone® does not loose shape/volume over time and therefore should not be confused with a bioresorbable material that will be resorbed over time.
CT-Bone® does not loose shape/volume over time and therefore should not be confused with a bioresorbable material that will be resorbed over time.
How bones, vessels and organs are printed using 3D printers / Habr
In the early days of rapid prototyping, it was widely believed that 3D printing would transform all manufacturing, spurring a consumer revolution that would bring a printer into every home. This has not yet happened, however, as has happened with many of the latest technologies, rapid prototyping has found its application in a completely different area - in medicine.
Article from the Gizmodo website.
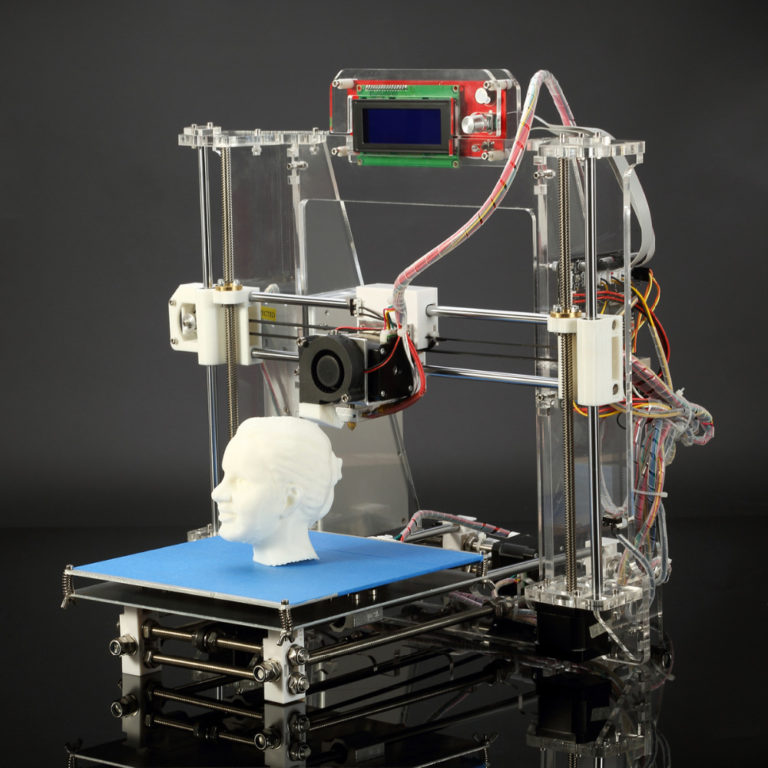
The research and projects below are some of the most interesting examples of the use of bioprinting and the use of computer-controlled machines to assemble biological matter using organic inks and ultra-strong thermoplastics. The range of application of bioprinting is very wide - from the reconstruction of the main parts of the human skull to the printing of scaffolds - scaffolds on which stem cells can develop into new bones. Read the details below.
The range of application of bioprinting is very wide - from the reconstruction of the main parts of the human skull to the printing of scaffolds - scaffolds on which stem cells can develop into new bones. Read the details below.
Skulls
Osteofab is a product of the company
Oxford Performance Materials. Initially, OPM entered the market by selling in its raw form a high-performance polymer often used in the manufacture of medical implants - a thermoplastic called polyetherketone ketone (PEKK), but over the past few years the company has become the first to master the use of this material, primarily in additive manufacturing . So, in February 2013, an American patient
installed FDA approved 3D skull implant. The casting and printing was carefully crafted to match the unique geometry of the patient's skull, of which 75% is now an implant.
Leather
The main problem with creating new skin using printing is the difficulty of recreating a specific shade from the entire possible spectrum. Given that our skin is unique, thin and subject to change, it is quite difficult to create an exact copy of it. There is a huge amount of interesting research on this topic, the essence of which cannot be put into a short story.
However, here are two of the most interesting: Scientist James Yoo of Wyke Forest University, with a grant funded by the US Department of Defense, is working on a machine that can print skin directly on burn victims. Another study is being carried out by scientists at the University of Liverpool, who are using carefully calibrated 3D scanners to obtain skin samples containing all of its finest nuances, which will allow more realistic implants to be printed later.
The research is still ongoing and the team plans to create a "skin sample database" of scanned samples that can be accessed from remote hospitals that do not have the cameras needed to scan a particular patient's skin.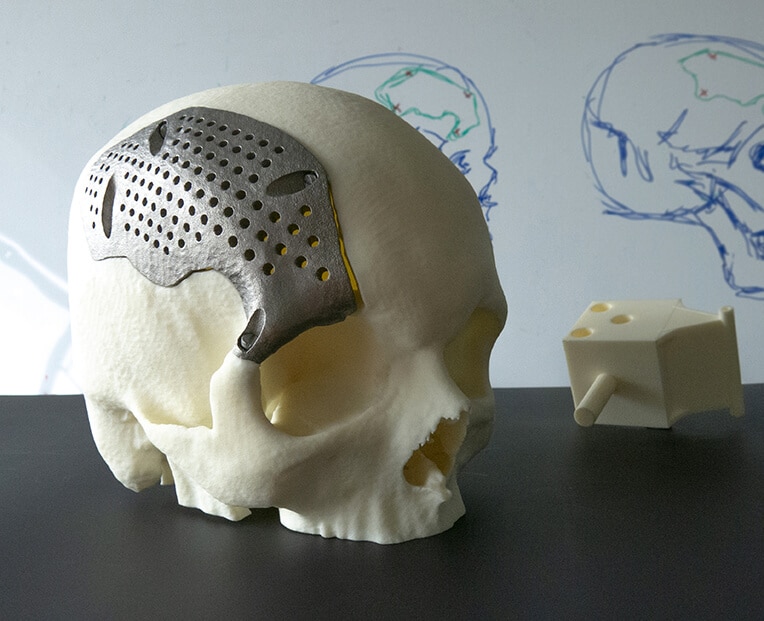 [ Gizmodo ; PhysOrg ]
[ Gizmodo ; PhysOrg ]
Noses and ears
The creation of prosthetic ears, noses and chins is often a painful, expensive and time-consuming process for both the patient and the doctor himself. British industrial designer Tom Fripp has worked with scientists at the University of Sheffield over the past 5 years to develop a cheaper and easier-to-make 3D printed facial prosthesis. The process of creating such a prosthesis includes 3D scanning the patient's face (which is much less painful than casting it), modeling the replacement part and printing it, which uses pigment, starch and medical silicone.
These prostheses have the added bonus that when they wear out (which they eventually will), they can be reprinted at a very low financial cost. [
The Guardian]
Prosthetic eyes
Fripp and a team at the University of Sheffield published the results of testing a similar process for making prosthetic eyes. Prosthetic eyes are expensive and, because they are hand-painted, can take months to make. Fripp Designs printers can produce 150 prosthetic eyes in an hour, and details such as iris color, size and number of blood vessels can be easily changed to suit the needs of the patient. [
Prosthetic eyes are expensive and, because they are hand-painted, can take months to make. Fripp Designs printers can produce 150 prosthetic eyes in an hour, and details such as iris color, size and number of blood vessels can be easily changed to suit the needs of the patient. [
]
Functional implants
As electronic devices — from drones to medical implants — get smaller, scientists are struggling to create batteries for them that are small enough, but with those could provide the necessary charge. However, a team of engineers from Harvard University is already printing microbatteries the size of a grain of sand using a 3D printer. Here's what the press release says:
“…researchers created an anode ink using nanoparticles of one lithium oxide compound, as well as a cathode ink made from nanoparticles of another kind of this compound. The printer applied ink to the teeth of two gold combs, thus creating a tightly connected structure of anodes and cathodes.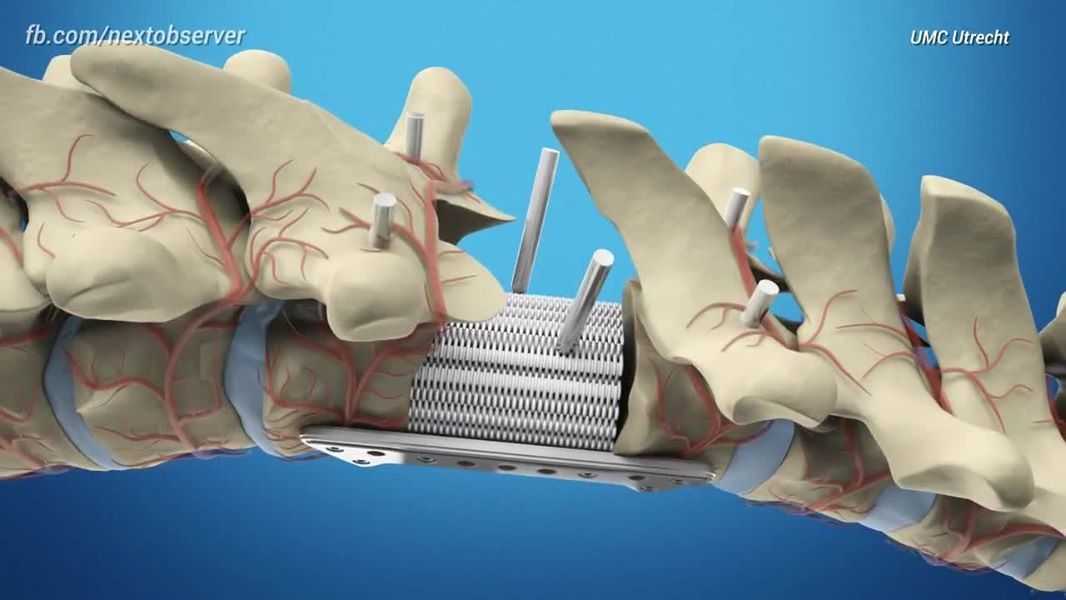 The scientists then placed the electrodes in a tiny container and filled it with an electrolyte solution to make a battery."
The scientists then placed the electrodes in a tiny container and filled it with an electrolyte solution to make a battery."
Over time, they will be able to charge medical implants, which are held back due to charging problems. [ Harvard ]
Bones
3D printed implants such as the jaw have been around for several years. However, a small group of researchers is conducting an experiment whose goal is to print real bones. For example, scientist Kevin Scheiksheff of the University of Nottingham invented a bioprinter that creates matrices from polylactic acid and gelatin alginate, which are then coated with stem cells.
The implanted matrices will gradually dissolve and be replaced by new growing bone: it will take approximately three months for the bone to completely transform. [ Forbes ]
Blood vessels and cells
We can already print
organs , but there is a serious problem in creating a functioning circulatory system.
German scientist Günther Tovar, head of the Fraunhofer Institute for Interfacial Engineering and Biotechnology, is working on a project called BioRap. His task is to use a 3D printer to print blood vessels, which uses a mixture of synthetic polymers and biomolecules. The printed circulatory systems are being tested on animals - they are not yet ready for introduction into the human body. However, they will eventually make organ transplants possible. [ Fraunhofer Institute ]
How do you see the future of 3D printing with living and substitute artificial materials for use in the human body? Will we soon be able to grow and replace full-fledged organs, such as the liver? Share your opinion in the comments.
what Tomsk scientists print on a 3D printer
3D printing technology, thanks to its unique ability to print almost anything, has already taken over the world. Scientists at the Research Center for Physical Materials Science and Composite Materials at Tomsk Polytechnic University (TPU) are developing improved materials for bone implants created using 3D printers.
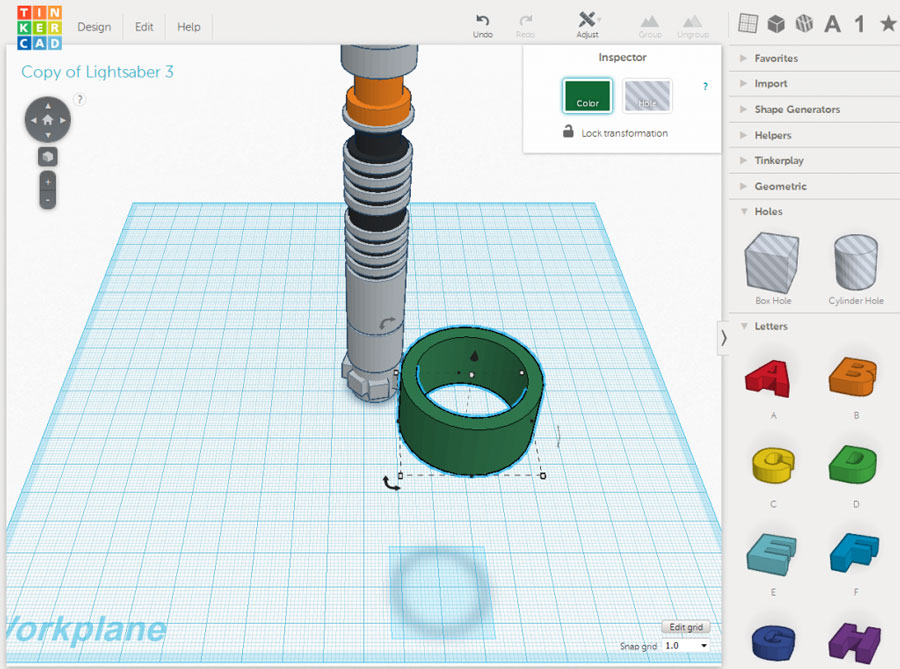
3D printing is an innovative technology for creating three-dimensional objects. A classic 3D printer works on the principle of layer-by-layer fusing modeling, when a three-dimensional image of a future object is divided into layers using software, from which it is then recreated. As a result, 3D printing is distinguished by a high speed of execution of orders, layouts for which, among other things, can be transferred online, which also saves time.
Now, thanks to 3D printing, almost any object can be created on a 3D printer: building materials, spacecraft parts, various implants and other medical products. At the same time, they can be printed from metal, plastic, unique biomaterials, etc.
Thus, employees of TPU Research Center "Physical Materials Science and Composite Materials" are developing bioinspired materials for 3D printing to replace bone defects.
According to Roman Surmenev, human bone tissue is a complex composite material with a structure organized at several levels and possessing unique mechanical characteristics. In turn, scientists work with mechanical metamaterials, manipulate their properties, such as density, to achieve similarities with human bone.
In turn, scientists work with mechanical metamaterials, manipulate their properties, such as density, to achieve similarities with human bone.
“We use pure titanium, or an alloy Ti-6Al-4V, which is approved for medical use, while changing its architectonics (construction. — Approx. ed.), which mimics the structure of bone,” he said.
Director of the Research Center "Physical Materials Science and Composite Materials" of the Tomsk Polytechnic University Roman Surmenev. Source: TPU press service
Thus, the addition of niobium ions significantly improves its mechanical and biological characteristics. Together with Russian and foreign partners, the employees of the center have already performed cellular and in vivo (on living organisms) experiments, which showed the promise of using such a titanium alloy.
How to print a bone
As Surmenev said, each person has his own physiological characteristics, therefore, in order to "print" a bone for him, it is necessary to perform a computed tomography of the area that needs to be replaced, and collect an anamnesis. This must be done by a healthcare professional.
This must be done by a healthcare professional.
“It is the surgeon or orthopedist who should contact us and set the task, knowing our capabilities,” he explained.
Then the developers perform a computer simulation of the future implant. “A mathematical three-dimensional model of the structure is being created, virtual engineering makes it possible to optimize the structure according to the required criteria. Next, a file is created with an extension suitable for the printer, the model is divided into layers and materialized by layer-by-layer build-up,” Surmenev explained.
After shaping the product, the powder is removed and special processing methods allow to achieve the optimal surface of the product. “At the last stage, it is necessary to make sure that all financial investments and the work of scientists have not been wasted, and indeed we are holding a unique product in our hands that will improve the patient’s life,” the scientist emphasized.
According to the principle of nature
“The term “additive technologies” (layer-by-layer building up and synthesis of an object using 3D technologies. — Ed.) appeared from the word “additive” — “to add,” says Surmenev. “This is what distinguishes 3D printing from traditional technologies where you need to subtract to get a design with complex geometry.”
— Ed.) appeared from the word “additive” — “to add,” says Surmenev. “This is what distinguishes 3D printing from traditional technologies where you need to subtract to get a design with complex geometry.”
In additive technologies, he says, the same approach is implemented as in wildlife, namely “top down” or “from big to small”. Nature created the surrounding world in a similar way - by layer-by-layer build-up, the scientist notes.
"You can pick up many epithets, but the stars really aligned, this technology is the best way to get materials with architectonics close to the structure of human tissue," the specialist is sure.
At the same time, he emphasizes that if we consider electron beam melting - the method by which they work in the center - then this technology is the most complicated in comparison with others.
“Requires a high quality powder, the presence of a vacuum during production, traditional post-processing does not allow to achieve the desired surface.