How is 3d printing used in the medical field
Introduction to Medical 3D Printing and 3D Printers for Healthcare
Personalized, precision medicine is on the rise. New tools and advanced technologies are bringing doctors closer to patients, delivering treatments and devices customized to better serve each unique individual.
Advances in medical 3D printing technology have made tremendous contributions to fields throughout healthcare. For patients, new tools and therapeutic methods developed through 3D printing can bring new degrees of comfort and personalization to treatment. For doctors, this newly accessible technology allows for a greater understanding of complex cases and provides new tools that can ultimately result in a higher standard of care.
From surgical planning models to 3D printed vasculature and bioreactors, read on to discover five ways 3D printing in healthcare is taking off and why many medical professionals are excited about the potential of 3D printing in the medical field. Then, learn about the most popular 3D printers for healthcare and how to choose a solution for specific use cases.
Webinar
Join Formlabs for this introduction to learn best practices for medical 3D printing and see the latest Formlabs Medical ecosystem, including multiple new medical-grade products!
Watch the Webinar Now
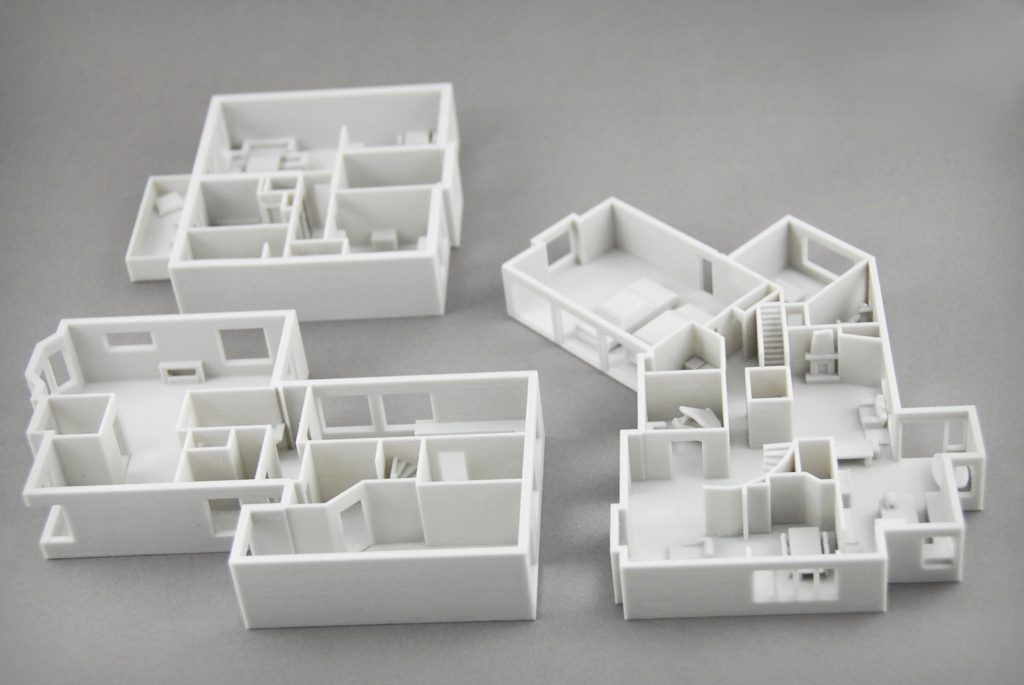
3D printed anatomical models from patient scan data are becoming increasingly useful tools in today’s practice of personalized, precision medicine. As cases become more complex and operating room efficiency becomes more important for routine cases, visual and tactile reference models can enhance understanding and communication within OR teams and with patients.
Healthcare professionals, hospitals, and research organizations across the globe are using 3D printed anatomical models as reference tools for preoperative planning, intraoperative visualization, and sizing or pre-fitting medical equipment for both routine and highly complex procedures that have been documented in hundreds of publications.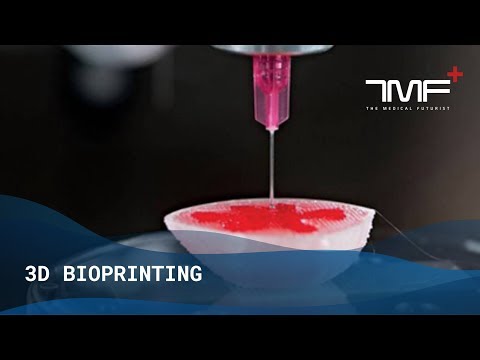
Producing patient-specific, tactile reference models from CT and MRI scans is affordable and straightforward with 3D printing. Peer-reviewed literature shows that they provide an additional view that helps physicians prepare better for surgeries, leading to drastically reduced time and cost in the operating room while improving patient satisfaction, lowering anxiety, and reducing recovery time.
Physicians can use patient-specific surgical models to explain the procedure beforehand, improving patient consent and lowering anxiety.
Learning from preoperative models can influence the course of treatment as well. This was true of the experience of Dr. Michael Eames. After replicating a young patient’s forearm bones, Dr. Eames realized the injury differed from what he’d previously thought.
Dr. Eames settled on a new, soft-tissue procedure—one that was much less invasive, decreased rehabilitation time, and produced far less scarring. Using the printed bone replica, Dr. Eames walked the young patient and his parents through the procedure and obtained their consent.
Eames walked the young patient and his parents through the procedure and obtained their consent.
The result? A surgery time of less than 30 minutes, instead of the initially planned surgery of three hours. This difference in surgery time led to an estimated $5,500 in cost avoidance for the hospital and meant the patient would need to spend less recovery time in postoperative care.
In the words of Dr. Alexis Dang, an orthopedic surgeon at the University of California San Francisco (UCSF) and the San Francisco Veteran's Affairs Medical Center: “Every one of our full-time orthopedic surgeons and nearly all of our part-time surgeons have utilized 3D printed models for care of patients at the San Francisco VA. We’ve all seen that 3D printing improves performance on game day.”
New biocompatible medical 3D printing materials have also enabled new surgical tools and techniques to be developed for the express purpose of further improving clinical experience during surgery. These include sterilizable fixation trays, contouring templates, and implant sizing models that can be used to size implants in the OR before the first cut, helping surgeons reduce time and increase accuracy of complex procedures.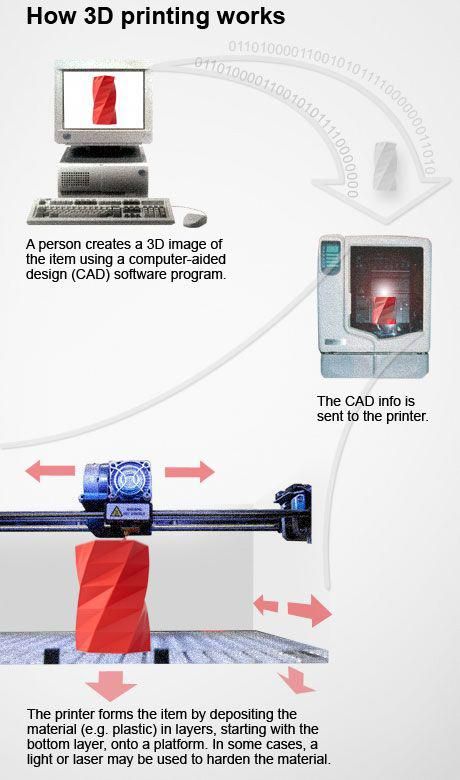
Anatomical model of a hand, including the 'skin' made out of an elastic 3D printing material.
Todd Goldstein, PhD, Instructor at the Feinstein Institute for Medical Research, is unequivocal in his estimation of how central 3D printing technology has become to his department. He estimates that if Northwell uses 3D printed models in 10-15% of its cases, it could save $1,750,000 a year.
“From medical device prototypes, complicated anatomical models for our children’s hospital, to creating training systems, and finally entering the dental clinic with implant surgical guides, [3D printing technology] has increased our capabilities and decreased our costs, all while allowing us to provide tools to treat patients that would be next to impossible to replicate without our go-to SLA 3D printer,” said Goldstein.
White Paper
Download our white paper for a practical walkthrough for physicians and technologists to get started creating 3D printed anatomicals models from patient scans, reviewing best practices for setting up a CT/MRI scan, segmenting datasets, and converting files to a 3D-printable format.
Download the White Paper
White Paper
In this webinar, Dr. Jonathan Morris, co-director of the Anatomic Modeling Laboratory and Neuroradiologist at the Mayo Clinic shares the history of 3D printing in medicine, and examines real-world case studies of how radiologists have successfully introduced 3D printing capabilities and programs into hospitals.
Watch the Webinar Now
3D printing has virtually become a synonym for rapid prototyping. The ease of use and low cost of in-house 3D printing has also revolutionized product development and many manufacturers of medical tools have adopted the technology to produce brand new medical devices and surgical instruments.
Over 90 percent of the top 50 medical device companies use 3D printing to create accurate prototypes of medical devices, jigs and fixtures to simplify testing, as well as directly 3D printing medical devices.
In the words of Alex Drew, a mechanical project engineer at DJO Surgical, a global provider of medical devices. “Before DJO Surgical brought the [Formlabs 3D printer] on board, we relied almost exclusively on outside print vendors for prototypes. Today, we are running four Formlabs machines, and the impact has been profound. Our rate of 3D printing has doubled, cost has been reduced by 70 percent, and the level of print detail allows for clear communication of designs with orthopedic surgeons.”
Medical device companies like Coalesce use 3D printing to create accurate prototypes of medical devices.
3D printing can accelerate the design process by iterating complex designs in days instead of weeks. When Coalesce was tasked to create an inhaler device that can digitally assess an asthma patient’s inspiratory flow profile outsourcing to service providers would have resulted in lengthy lead times for each prototype. Design files would have had to be painstakingly refined through various iterations before being sent off-site to be built.
Instead, desktop SLA 3D printing allowed Coalesce to keep the entire prototyping process in-house. The prototypes were fit for use in clinical studies and looked just like a finished product. In fact, when they showcased the device, their clients mistook the prototype for the final product.
Overall, in-house represented an enormous 80–90% reduction in lead time for prototypes. What’s more, the parts took only eight hours to print and could be finished and painted within a few days, while the same process would have taken a week or two through an external contractor.
White Paper
In this report, learn how Formlabs Medical helps medical device firms bring digital fabrication in-house, and get inspired through the examples of four companies currently creating groundbreaking devices using 3D printing.
Download the White Paper
Each year hundreds of thousands of people lose a limb, but only a subset of them get access to a prosthesis to recover its function.
Simple prostheses are only available in a few sizes, so patients must make do with what fits best, while custom-fit bionic devices designed to mimic the motions and grips of real limbs that rely on muscles in a person’s residual limb to control their functions are so expensive that they’re only accessible to patients with the best health insurance in developed countries. This particularly affects prostheses for children. As children grow and get into adventures, they inevitably outgrow their prostheses and require expensive repairs.
The difficulty is the lack of manufacturing processes that can produce custom parts affordably. But increasingly, prosthetists can take advantage of 3D printing’s much-noted design freedom to mitigate these high financial barriers to treatment.
Initiatives such as e-NABLE allow entire communities around the world to form around 3D printed prostheses. They’re driving an independent movement in prosthetic production by sharing information and open-source designs freely online, so patients can get a custom-designed prosthesis that is well-adapted for them for as little as $50.
Other inventors like Lyman Connor, take this one step further. With only a small facility of four desktop 3D printers, Lyman was able to complete and fit his first production prostheses. His ultimate objective? To create a customizable, fully bionic hand to be sold at a fraction of the current tens of thousands of dollars retail price tag for such advanced prostheses.
Elsewhere, researchers at MIT have also identified 3D printing as an optimal means of producing more comfortable prosthesis sockets.
Needless to say, the low cost of producing these prostheses, along with the freedom that comes with custom designs, has proved revelatory. Prostheses made with 3D printing can be turned around in as little as two weeks and then can be trialed and maintained at a much lower cost than their traditional counterparts.
As the costs continue to decrease and material properties improve, 3D printing will undoubtedly play an increasing role in this department of healthcare.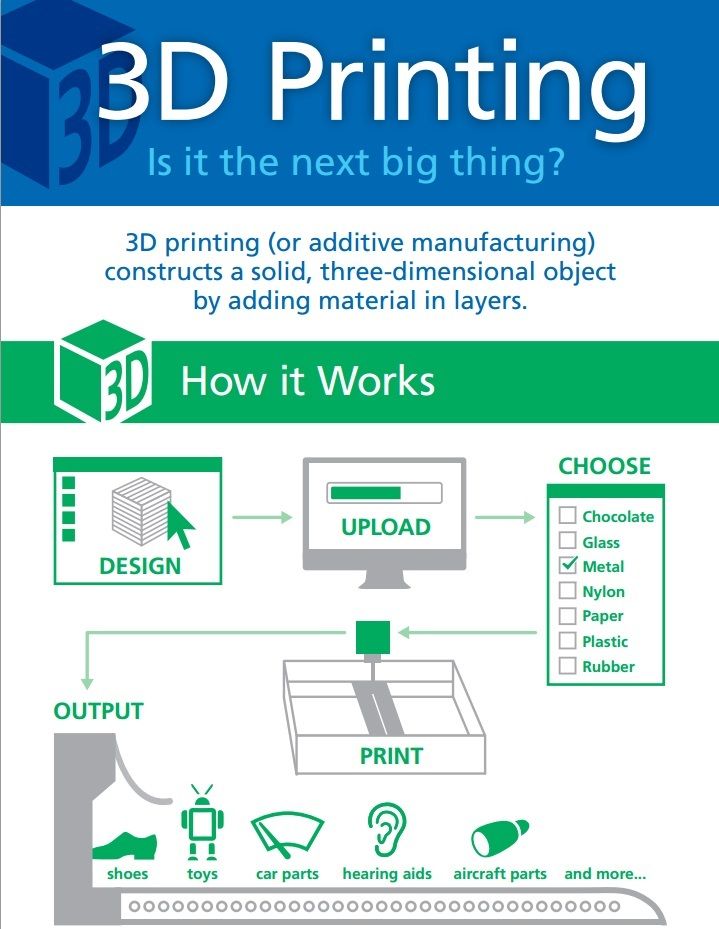
Many of the same high financial barriers to treatment seen in prosthetics are also native to fields such as orthoses and insoles. Like many other patient-specific medical devices, custom orthoses are often inaccessible due to their high cost and take weeks or months to get manufactured. With 3D printing, that no longer needs to be the case.
The example of Matej and his son Nik springs to our mind. Born prematurely in 2011, difficulties during childbirth caused Nik to have cerebral palsy, a condition that affects almost twenty million people worldwide. Matej was inspired by his son’s unwavering will to transcend the limitations of his condition, but he was faced with a choice between a standard, pre-made orthosis that would have been inadequate and uncomfortable for his son, or an expensive custom solution that would take weeks or months to be delivered, only to be made quickly obsolete by a growing child.
He decided to take matters into his own hands and sought out new solutions to achieve this goal. With the freedom offered by digital technologies including 3D scanning and 3D printing, Matej and Nik's physical therapists were able to experiment liberally and develop an entirely new innovative workflow for ankle foot orthoses (AFOs).
With the freedom offered by digital technologies including 3D scanning and 3D printing, Matej and Nik's physical therapists were able to experiment liberally and develop an entirely new innovative workflow for ankle foot orthoses (AFOs).
The resulting custom-made, 3D printed orthosis provided Nik with support, comfort, and correction precisely where it was needed, helping Nik to at last take his first independent steps. This custom orthotic device reprised the highly-adjusted finish of high-end orthotics, at a fraction of the price, and with no further adjustments required.
Professionals around the world are using 3D printing to reinvent patient- and customer-specific insoles and orthoses, as well as a range of other tools for improving physical therapy. In the past, the course of physical therapy using customized tools had proved difficult. Patients often faced long wait times and finished pieces that led to discomfort. 3D printing is on the path to change this status quo. 3D printed insoles and orthoses have proved to be a better fit, led to better therapeutic outcomes, and provided a greater degree of comfort and use for patients.
3D printed insoles and orthoses have proved to be a better fit, led to better therapeutic outcomes, and provided a greater degree of comfort and use for patients.
The conventional means of treating patients with grave organ failures currently involve using autografts, a graft of tissue from one point to another of the same individual's body, or organ transplants from a donor. Researchers in the fields of bioprinting and tissue engineering are hoping to soon change that and be able to create tissues, blood vessels, and organs on demand.
3D bioprinting refers to the use of additive manufacturing processes to deposit materials known as bioinks to create tissue-like structures that can be used in medical fields. Tissue engineering refers to the various evolving technologies, including bioprinting, to grow replacement tissues and organs in the laboratory for use in treating injury and disease.
With the help of high-precision 3D printing, researchers like Dr. Sam Pashneh-Tala from the University of Sheffield have brought new possibilities to tissue engineering.
To direct cellular growth so that the required tissue is formed, Dr. Pashneh-Tala grows living cells on a scaffold in the lab, that provides a template of the required shape, size, and geometry. For example, a tubular structure is needed to create a blood vessel for a cardiovascular patient. The cells will multiply and cover the scaffold, taking on its shape. The scaffold then gradually breaks down, leaving the living cells arranged into the shape of the target tissue, that is cultured in a bioreactor, a chamber that contains the developing tissue and can reproduce the internal environment of the body, to acquire mechanical and biological performance of organic tissue.
A 3D printed bioreactor chamber with a tissue-engineered miniature aorta growing inside. The tissue is cultured in the bioreactor to acquire the mechanical and biological performance of organic tissue.
This will empower scientists to create patient-specific vascular graft designs, improved surgical options and provides a unique testing platform for new vascular medical devices for those suffering from cardiovascular disease, that is currently the number one cause of death worldwide. Following that, the ultimate goal is to create blood vessels that are ready to be implanted into the patients. As tissue engineering uses cells that are taken from the patient requiring the treatment, it eliminates the possibility of rejection by the immune system—a major issue in conventional organ transplant procedures today.
Following that, the ultimate goal is to create blood vessels that are ready to be implanted into the patients. As tissue engineering uses cells that are taken from the patient requiring the treatment, it eliminates the possibility of rejection by the immune system—a major issue in conventional organ transplant procedures today.
3D printing has proven capable of responding to the challenges of producing synthetic blood vessels by solving the difficulties of recreating the precise shapes, sizes and geometries of the vessel required. Being able to closely match printed solutions to the specific needs of patients has proved revelatory.
In Dr. Pashneh-Tala’s words: “[Creating blood vessels through 3D printing] offers the potential for improved surgical options and even patient-matched blood vessel designs. Without access to high-precision, affordable 3D printing, creating these shapes would not be possible.”
We have seen exciting breakthroughs in biological materials suitable for use in 3D printers. Scientists are developing new hydrogel materials that have the same consistency as organ tissue that can be found in the human brain and lungs and can be compatible with various 3D printing processes. Scientists are hoping to be able to implant them onto an organ, to act as ‘scaffold’ onto which cells would be encouraged to grow.
Scientists are developing new hydrogel materials that have the same consistency as organ tissue that can be found in the human brain and lungs and can be compatible with various 3D printing processes. Scientists are hoping to be able to implant them onto an organ, to act as ‘scaffold’ onto which cells would be encouraged to grow.
While bioprinting fully functional internal organs such as hearts, kidneys, and livers still sounds futuristic, advancements with hybrid 3D printing techniques are happening at a very rapid rate.
Sooner or later, building biological matter in laboratory printers is expected to lead to the ability to generate new, fully functional 3D printed organs. In April 2019, scientists created the first 3D heart using a patient's biological materials at Tel Aviv University. The tiny replica was created using the patient’s own biological materials, engendering a complete match of the patient’s immunological, cellular, biochemical, and anatomical profile.
"At this stage, our 3D heart is small, the size of a rabbit's heart, but larger human hearts require the same technology," said Professor Tal Dvir.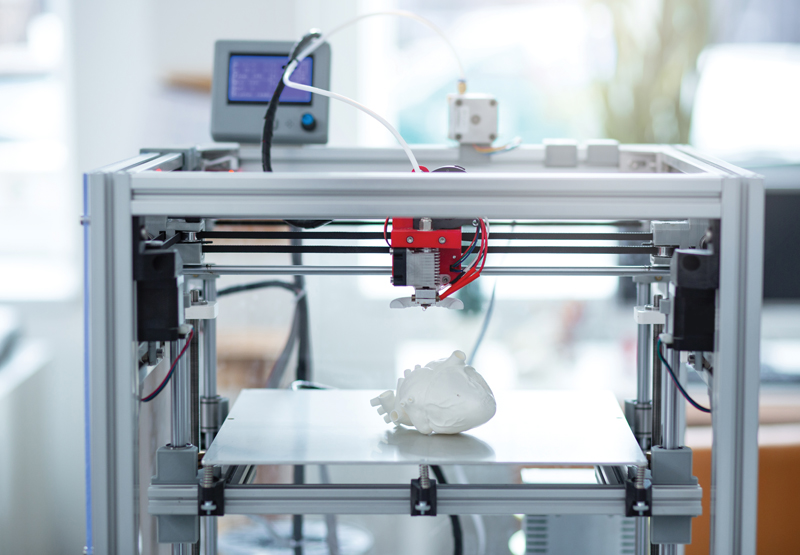
The first 3D bioprinted heart, created at the University of Tel Aviv.
When it comes to 3D printers for healthcare, not all methods are created equal. It is important to choose the right printing technology for specific use cases.
The most popular medical 3D printing technologies include stereolithography (SLA), selective laser sintering (SLS), and fused deposition modeling (FDM) for plastic parts, and direct metal laser sintering (DMLS) and selective laser melting (SLM) for metals.
SLA 3D printers use a laser to cure liquid resin into hardened plastic in a process called photopolymerization. SLA is one of the most popular processes among medical professionals due to its high resolution, precision, and material versatility.
-
Advantages of SLA
SLA parts have the highest resolution and accuracy, the clearest details, and the smoothest surface finish of all plastic 3D printing technologies. The main benefit of SLA, however, lies in its versatility.:quality(80)/images.vogel.de/vogelonline/bdb/1612700/1612740/original.jpg) SLA resin formulations offer a wide range of optical, mechanical, and thermal properties to match those of standard, engineering, and industrial thermoplastics.
SLA resin formulations offer a wide range of optical, mechanical, and thermal properties to match those of standard, engineering, and industrial thermoplastics.
SLA is a great option for highly detailed anatomical models, medical device prototypes requiring tight tolerances and smooth surfaces, as well as molds, tooling, patterns, and functional end-use parts. SLA also offers the widest selection of biocompatible materials for dental and medical applications. With Draft Resin, the Formlabs SLA printers are also the fastest options for 3D printing large prototypes, up to 10X faster than FDM.
SLA’s wide versatility comes with a slightly higher price tag than FDM, but it is still more affordable than all other 3D printing processes. SLA resin parts also require post-processing after printing, which includes washing the parts and post-curing.
SLA 3D printing offers a wide selection of 3D printing materials, including biocompatible materials, for a variety of medical and dental applications.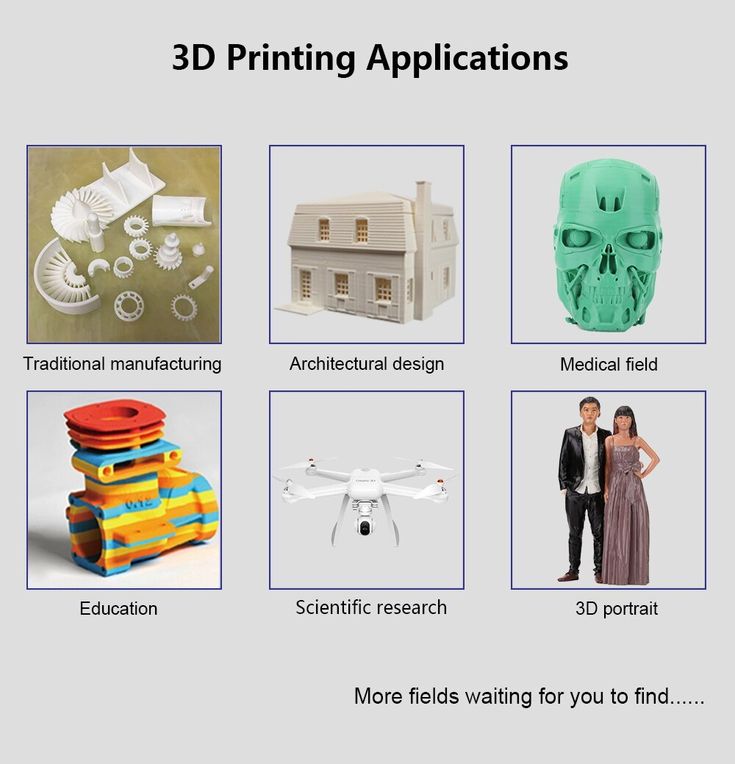
Sample part
See and feel Formlabs SLA quality firsthand. We’ll ship a free sample part to your office.
Request a Free Sample Part
Webinar
Join Formlabs and Nelson Labs for a deep dive into biocompatibility, including an introduction to our new materials and best practices for medical manufacturers from industry experts.
Watch the Webinar Now
SLS 3D printers use a high-powered laser to fuse small particles of polymer powder. The unfused powder supports the part during printing and eliminates the need for dedicated support structures, making SLS a particularly effective choice for complex mechanical parts.
Its ability to produce parts with excellent mechanical capabilities makes SLS the most common polymer additive manufacturing technology for industrial applications. Depending on the material, SLS nylon parts may also be biocompatible and sterilizable.
-
Advantages of SLS
Since SLS printing doesn’t require dedicated support structures, it’s ideal for complex geometries, including interior features, undercuts, thin walls, and negative features. Parts produced with SLS printing have excellent mechanical characteristics, with strength resembling that of injection-molded parts.
The most common material for SLS is nylon, a popular engineering thermoplastic with excellent mechanical properties. Nylon is lightweight, strong, and flexible, as well as stable against impact, chemicals, heat, UV light, water, and dirt. 3D printed nylon parts can also be biocompatible and not sensitizing, which means that they are ready to wear and safe to use in many contexts.
The combination of low cost per part, high productivity, established materials, and biocompatibility makes SLS a popular choice among medical device developers for functional prototyping, and a cost-effective alternative to injection molding for limited-run or bridge manufacturing.
SLS 3D printers have a higher entry price than FDM or SLA technologies. While nylon is a versatile material, material selection for SLS is also more limited than for FDM and SLA. Parts come out of the printer with a slightly rough surface finish and require media blasting for a smooth finish.
SLS 3D printing is ideal for strong, functional prototypes and end-use parts, such as prosthetics and orthotics.
Sample part
See and feel Formlabs SLS quality firsthand. We’ll ship a free sample part to your office.
Request a Free Sample Part
FDM, also known as fused filament fabrication (FFF), is a printing method that builds parts by melting and extruding thermoplastic filament, which a printer nozzle deposits layer by layer in the build area.
FDM is the most widely used form of 3D printing at the consumer level, fueled by the emergence of hobbyist 3D printers. Industrial FDM printers are, however, also popular with professionals.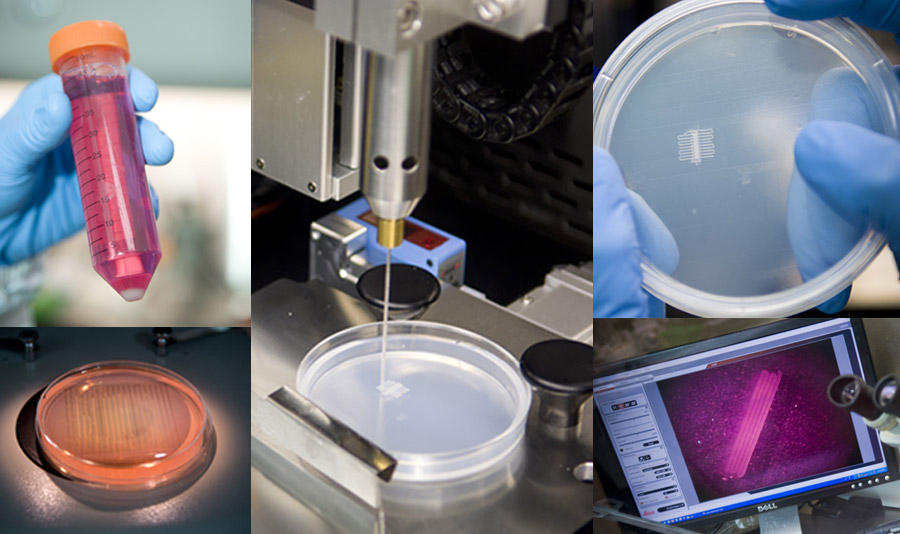
-
Advantages of FDM
FDM works with an array of standard thermoplastics, such as ABS, PLA, and their various blends. This results in a low price of entry and materials. FDM best suits basic proof-of-concept models and the low-cost prototyping of simpler parts. Some FDM materials are also biocompatible.
FDM has the lowest resolution and accuracy when compared to other 3D printing technologies for plastics such as SLA or SLS, which means that it is not the best option for printing complex designs or parts with intricate features, such as anatomical models. Higher-quality finishes require labor-intensive and lengthy chemical and mechanical polishing processes. Some industrial FDM 3D printers use soluble supports to mitigate some of these issues and offer a wider range of engineering thermoplastics, but they also come at a steep price. When creating large parts, FDM printing also tends to be slower than SLA or SLS.
Direct metal laser sintering (DMLS) and selective laser melting (SLM) 3D printers work similarly to SLS printers, but fuse metal powder particles together layer by layer using a laser instead of polymers.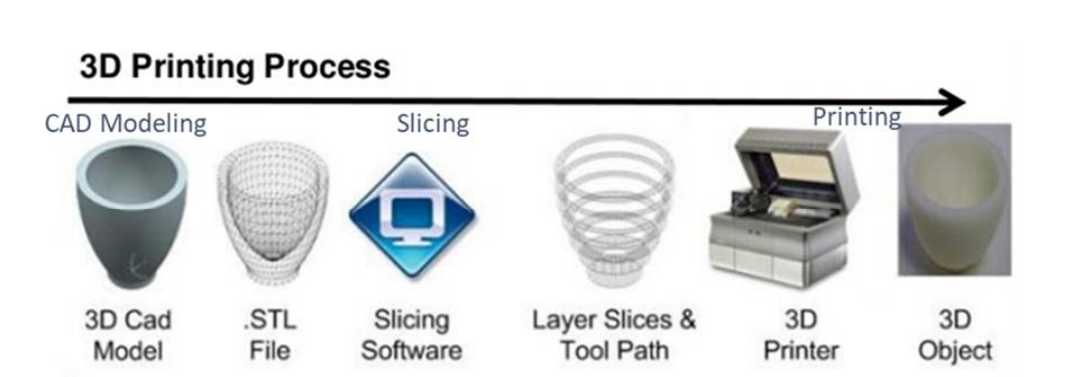
DMLS and SLM 3D printers can create strong, accurate, and complex metal products, making this process ideal for a variety of medical applications.
The biggest advantage of these processes is obviously the materials, as DMLS and SLM 3D printers are capable of producing high-performing end-use medical devices and components from metal. These processes can reproduce complex geometries and the finished products are strong, durable, and biocompatible. They can be used to manufacture generic implants (hips, knees, spine implants, etc.), custom implants for cancer or trauma treatment, dentures, as well as medical and orthopedic technology products.
While the prices of metal 3D printers have also begun to decrease, with costs ranging from $200,000 to $1 million+, these systems are still not accessible to most businesses. Metal 3D printing processes also have an involved and complex workflow.
Alternatively, SLA 3D printing is well-suited for casting workflows that produce metal parts at a lower cost, with greater design freedom, and in less time than traditional methods.
The table below highlights the 3D printing technologies that are best equipped to handle the different medical 3D printing applications.
| Stereolithography (SLA) | Selective Laser Sintering (SLS) | Fused Deposition Modeling (FDM) | Metal 3D Printing (DMLS, SLM) | |
|---|---|---|---|---|
| Build volume | Up to 300 x 335 x 200 mm (desktop and benchtop 3D printers) | Up to 165 x 165 x 300 mm (benchtop industrial 3D printers) | Up to 300 x 300 x 600 mm (desktop and benchtop 3D printers) | Up to 400 x 400 x 400 mm (large industrial DMLS/SLM) |
| Price range | Starting from $3,750 | Starting from $18,500 | Starting from $2,500 | Starting from $200,000 |
| Materials | Varieties of resin (thermosetting plastics). Standard, engineering (ABS-like, PP-like, silicone-like, flexible, heat-resistant, rigid), castable, dental, and medical (biocompatible). | Engineering thermoplastics, typically nylon and its composites (nylon is biocompatible + compatible with sterilization). | Standard thermoplastics, such as ABS, PLA, and their various blends. | Stainless steel, tool steel, titanium, cobalt chrome, and aluminum. |
| Ideal applications | Anatomical models, highly detailed prototypes requiring tight tolerances and smooth surfaces; molds, tooling, patterns, functional parts, dental and medical end-use devices. | Complex geometries, functional prototypes, short-run or bridge manufacturing of medical devices, including orthotics and prosthetics. | Basic proof-of-concept models, low-cost prototyping of simple parts. | Strong, durable parts with complex geometries, implants, dentures, medical and orthopedic components out of metal. |
Precise and affordable medical 3D printing processes are democratizing access to the technology, empowering healthcare professionals to develop new clinical solutions and quickly manufacture custom devices, and allowing physicians to deliver new treatments across the globe. As medical 3D printing technologies and materials continue to improve, they will pave the path for personalized care and high-impact medical applications.
As medical 3D printing technologies and materials continue to improve, they will pave the path for personalized care and high-impact medical applications.
Every medical facility should have access to the latest tools to improve care and provide the best patient experience. Get started now or expand your in-house production with Formlabs, a proven, cutting-edge partner in medical 3D printing.
Reach out to our medical experts to learn more about how in-house 3D printing can provide better treatment and supplement your current medical device design and manufacturing workflow.
Contact Our Medical Experts
Medical Applications of 3D Printing
3D printers are used to manufacture a variety of medical devices, including those with complex geometry or features that match a patient’s unique anatomy.
Some devices are printed from a standard design to make multiple identical copies of the same device. Other devices, called patient-matched or patient-specific devices, are created from a specific patient’s imaging data.
Commercially available 3D printed medical devices include:
- Instrumentation (e.g., guides to assist with proper surgical placement of a device),
- Implants (e.g., cranial plates or hip joints), and
- External prostheses (e.g., hands).
Scientists are researching how to use the 3D printing process to manufacture living organs such as a heart or liver, but this research is in early stages of development.
The 3D printing process can be accomplished using any of several different technologies. The choice of technology can depend on many factors including how the final product will be used and how easy the printer is to use. The most common technology used for 3D printing medical devices is called powder bed fusion. Powder bed fusion is commonly used because it works with a variety of materials used in medical devices, such as titanium and nylon.
FDA Powder Bed Fusion Printer
The powder bed fusion process builds a three-dimensional product from very fine metal or plastic powder, which is poured onto a platform and leveled carefully. A laser or electron beam then moves across the powder layer and melts the material it touches. Melted material fuses to the layer below it and to the powder around it to create a solid. Once a layer is completed, the platform moves down and one more layer of carefully leveled powder is placed on top.
A laser or electron beam then moves across the powder layer and melts the material it touches. Melted material fuses to the layer below it and to the powder around it to create a solid. Once a layer is completed, the platform moves down and one more layer of carefully leveled powder is placed on top.
The FDA has several 3D printers that help us better understand the capabilities of 3D printing of medical devices and the public health benefit of this technology. For example, the FDA has printers that use different printing technologies, including powder bed fusion, to evaluate what parts of the printing processes and workflows are critical to ensure quality of the finished medical device.
Patient-matched devices
While 3D printers are often used to create identical copies of the same device, they can also be used to create devices unique to a specific patient. Patient-matched (or patient-specific) devices are created specifically for the patient based on individual features, such as anatomy. They can be based on a template model that is matched to a patient using medical imaging. Patient-matching can be accomplished by techniques such as scaling of the device using one or more anatomic features from patient data.
They can be based on a template model that is matched to a patient using medical imaging. Patient-matching can be accomplished by techniques such as scaling of the device using one or more anatomic features from patient data.
The FDA regulates 3D printed medical devices through the same pathways as traditional medical devices; therefore they are evaluated according to the safety and effectiveness information submitted to us by the manufacturer. While traditionally manufactured medical devices come in discrete sizes, patient-matched devices can be made in a continuous range of shapes with pre-defined minimum and maximum specifications that we can use to review the devices in the same way as standard sized devices. For instance, the specification may define a minimum and maximum wall thickness or how sharp a curve can be to maintain device performance for its intended use.
There is a provision in federal law that exempts “custom” medical devices from FDA review, but patient-matched devices do not automatically meet all the requirements. For further information on custom device exemptions, please refer to the Custom Device Exemptions guidance.
For further information on custom device exemptions, please refer to the Custom Device Exemptions guidance.
Other uses of 3D printing
The use of 3D printing is not limited to medical devices. Other industries and government departments are also interested in its use. For instance, the U.S. Department of Energy (DOE) is investing resources to study 3D printing, and how it can be used to reduce waste by using fewer raw materials and require fewer manufacturing steps. DOE has compiled information on how 3D printing works, the different types of printers and for what they are used. For more information on how 3D printers work and the different printing technologies, visit the DOE’s How 3D Printers Work webpage.
Medical 3D printer overview
Use of 3D printing in medicine
Source: docwirenews.com
3D printing has been used in medicine since the early 2000s, when this technology was first used to make dental implants.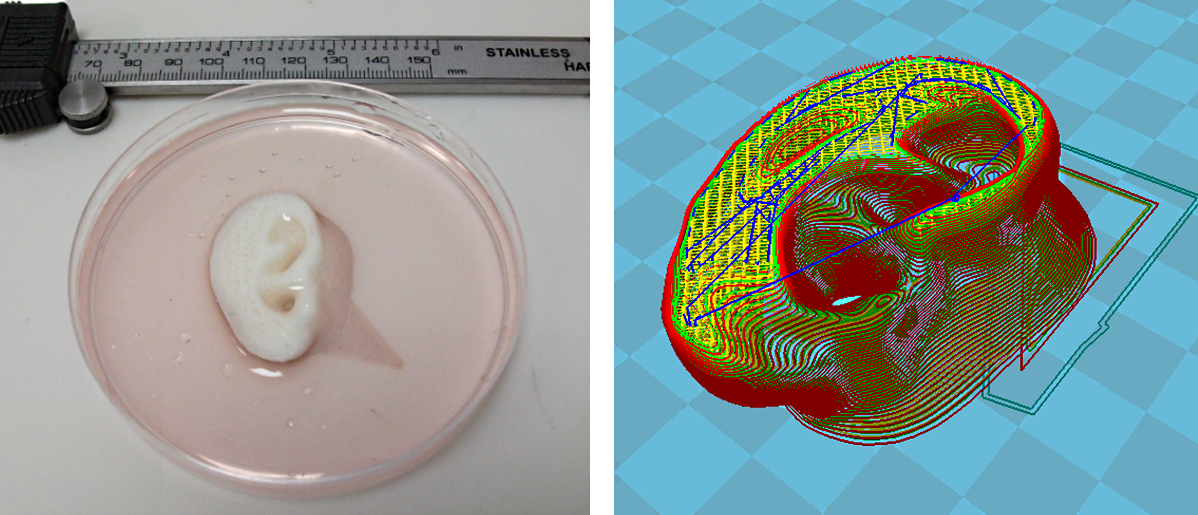 Since then, the use of 3D printing in medicine has expanded significantly, with doctors around the world describing ways to use 3D printing to produce ears, skeletal parts, airways, jawbones, eye parts, cell cultures, stem cells, blood vessels and vasculature, tissues and organs, new dosage forms and much more. nine0005
Since then, the use of 3D printing in medicine has expanded significantly, with doctors around the world describing ways to use 3D printing to produce ears, skeletal parts, airways, jawbones, eye parts, cell cultures, stem cells, blood vessels and vasculature, tissues and organs, new dosage forms and much more. nine0005
Source: zortrax.com
Using files with models for 3D printing provides an opportunity for the exchange of work among researchers. Instead of trying to reproduce the parameters described in scientific journals, doctors can use and modify ready-made 3D models. To this end, in 2014, the National Institutes of Health established the 3dprint.nih.gov exchange to facilitate the exchange of open source 3D models for medical and anatomical devices, custom equipment, and mock-ups of proteins, viruses, and bacteria. nine0005
Source: 3dprint.com
Modern medical use of 3D printing can be divided into several broad categories: tissue and organ fabrication, prostheses, implants and anatomical models, instrument printing, and pharmaceutical research.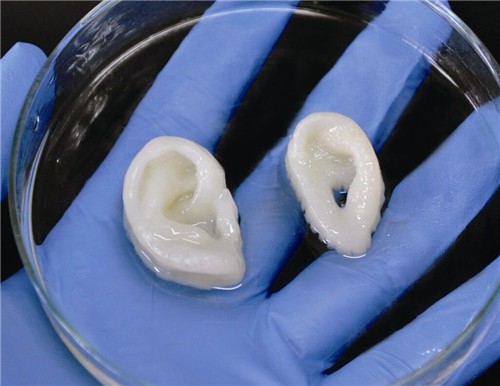
Top five uses for 3D printing in medicine
Operational preparation and student education
Source: 3dprint.com
Taking into account individual differences and features of the anatomy of a particular human body, it is possible to use 3D printed models for the preparation of surgical operations. Having a doctor have a tangible model of a particular patient's organ, made, for example, based on the results of CT (computed tomography) for study or to simulate an operation, significantly reduces the risk of medical errors.
Source: openbiomedical.org
The use of 3D models for training surgeons and students is preferable to training on cadavers, as it does not create problems in terms of availability and cost of objects.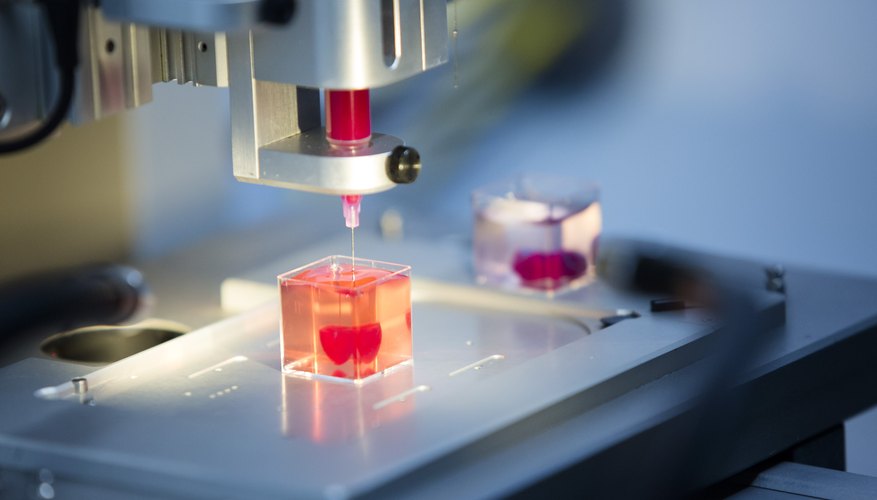 Cadavers often lack appropriate pathology, so they are more suitable for anatomy lessons than for presenting a patient with a disorder appropriate to the topic under study. Using 3D printing, you can create a model of any organ with any known pathology. nine0005
Cadavers often lack appropriate pathology, so they are more suitable for anatomy lessons than for presenting a patient with a disorder appropriate to the topic under study. Using 3D printing, you can create a model of any organ with any known pathology. nine0005
Source: ncbi.nlm.nih.gov
two-dimensional images.
Bioprinting of tissues and organs
Source: hbr.org
Bioprinting is one of the many types of 3D printing used in the medical field. Instead of printing using plastic or metal, bioprinters use a syringe dispenser to apply bioink (layers of living cells or a structuring base for them) to create artificial living tissue. In addition to being used as an alternative to donor tissues, such tissue constructs or organoids can be used for medical research.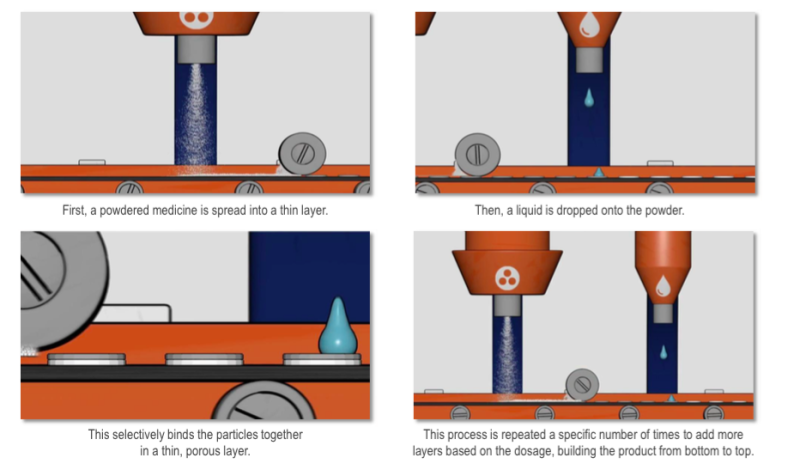 nine0005
nine0005
Source: press.ginkgo3d.com
Although 3D bioprinting systems can be laser, inkjet, or extrusion, inkjet bioprinting is the most common. Multiple printheads can be used to accommodate different types of cells (organ-specific, blood vessel cells, muscle tissue), which is a major challenge in the fabrication of heterocellular tissues and organs. 3D printing with biological materials can be used to regenerate tissues, and in the future, organs, directly on the patient. nine0005
Printing Surgical Instruments
Volt Grip Details, Source: bitegroup.nl
Today's surgeons are trying to perform operations with as little trauma to the patient as possible, so they very often require a personalized instrument. The use of 3D printing makes it possible to create such tools within hours.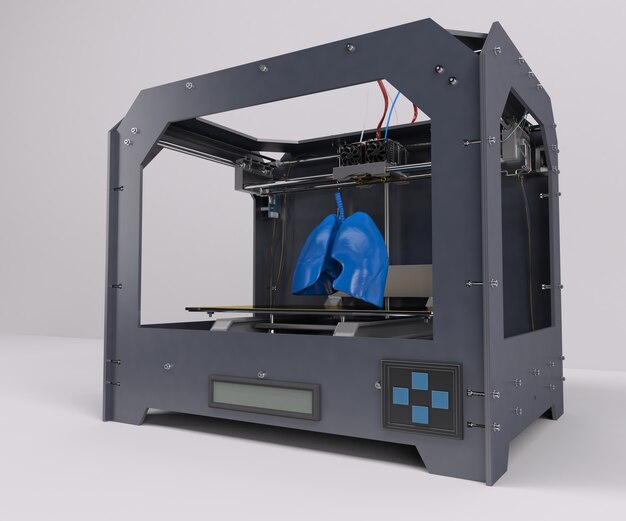
Volt capture model visualization, Source: bitegroup.nl
Now the doctor can independently modify the finished model, giving it the necessary size and shape for convenience and efficiency. Dentists can now create, for example, individual guides right in front of the patient, eliminating the possibility of damage to healthy teeth during prosthetics.
About the clamp Volt, from the photos above, read further in the section “Usage examples”.
Here's how students at Duke University in Durham, North Carolina create tools using metal 3D printing. nine0005
"Printing" drugs
Source: mdpi.com
3D printing technologies are already being used in pharmaceutical research and personalized medicine, and their scope is constantly expanding.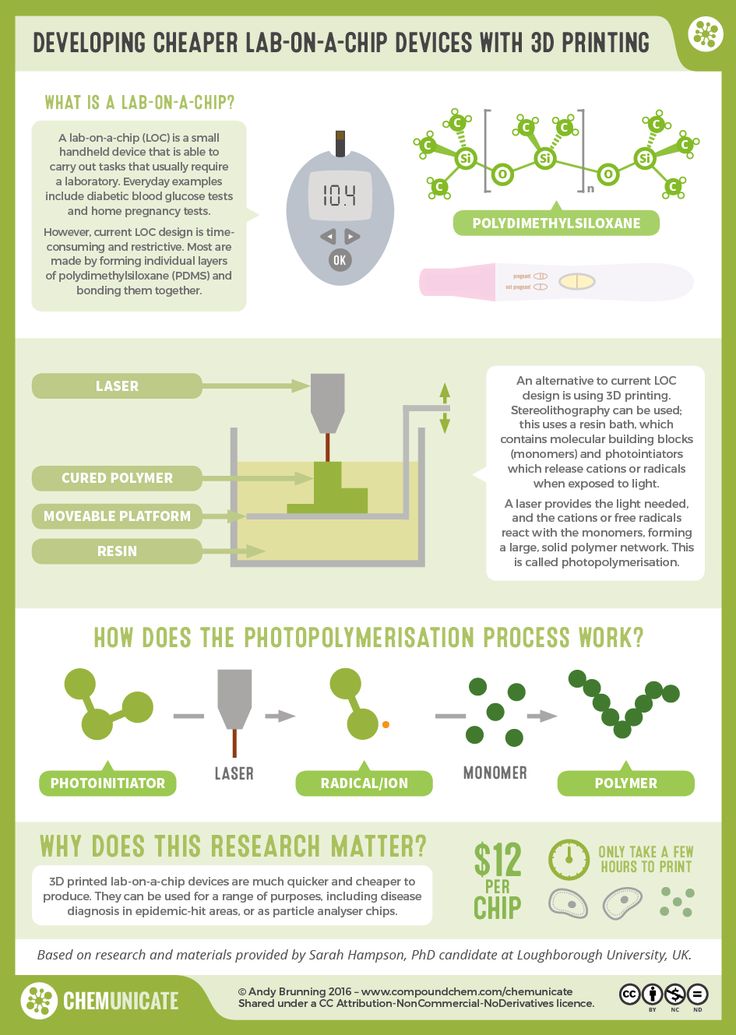 3D printing enables precise dose control of drugs and the production of dosage forms with complex drug release profiles and prolonged action. Now pharmacists can analyze a patient's pharmacogenetic profile and other characteristics such as age, weight, or gender to determine the optimal dose and sequence of medications. If necessary, the dose may be adjusted, depending on the clinical response. With 3D printing, it is possible to produce personalized medicines in completely new formulations, such as tablets containing multiple active ingredients, either as a single mixture or as complex multi-layered tablets. nine0005
3D printing enables precise dose control of drugs and the production of dosage forms with complex drug release profiles and prolonged action. Now pharmacists can analyze a patient's pharmacogenetic profile and other characteristics such as age, weight, or gender to determine the optimal dose and sequence of medications. If necessary, the dose may be adjusted, depending on the clinical response. With 3D printing, it is possible to produce personalized medicines in completely new formulations, such as tablets containing multiple active ingredients, either as a single mixture or as complex multi-layered tablets. nine0005
Prosthetics and Dentistry
Source: eos.info
3D printing has been successfully used in medicine for the manufacture of complex custom prostheses or surgical implants. Implants and prostheses of any possible geometry can be made by converting X-ray, MRI or CT images into a 3D printable model using special software.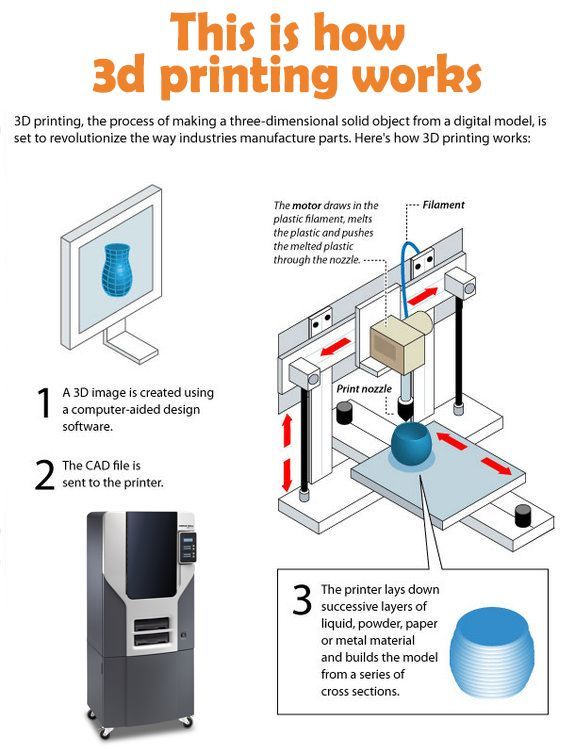
The rapid production of custom implants and prostheses solves a pressing problem in orthopedics, where standard implants often do not fit the patient. This is also true in neurosurgery: skulls are individually shaped, so it is difficult to standardize a cranial implant. Previously, surgeons had to use various tools to modify and fit implants, sometimes right during the operation. The use of 3D printers makes this procedure unnecessary. Additive technologies are especially in demand when it is necessary to urgently manufacture implants. nine0005
A real revolution in dentistry came with the advent of 3D technology.
Source: hypowerfuel.com
First, complete and accurate 3D scanning of the oral cavity is now possible. Secondly, the use of 3D printing has made it possible to create prostheses that absolutely fit the anatomy of the patient, without the need for a long and unpleasant fit. The radical reduction in the share of manual labor in the manufacture of prostheses or veneers has reduced the required tolerances in production, expanded the list of materials used and increased patient satisfaction with the results of the doctor's work. nine0005
The radical reduction in the share of manual labor in the manufacture of prostheses or veneers has reduced the required tolerances in production, expanded the list of materials used and increased patient satisfaction with the results of the doctor's work. nine0005
Application examples
Printing a model of the heart of a four-year-old patient, Zortrax M200 3D printer
In the photo: the assembled heart model. Source: zortrax.com
At the Medical University of Gdansk (Poland) to prepare for an operation to treat a complex congenital heart disease (Fallot's tetrad - malfunction of the pulmonary artery heart valve) in a four-year-old patient, specialists from the Department of Pediatric Cardiology and Congenital Heart Diseases , together with colleagues from the Department of Cardiac Surgery and Radiology, used the Zortrax M200 3D printer.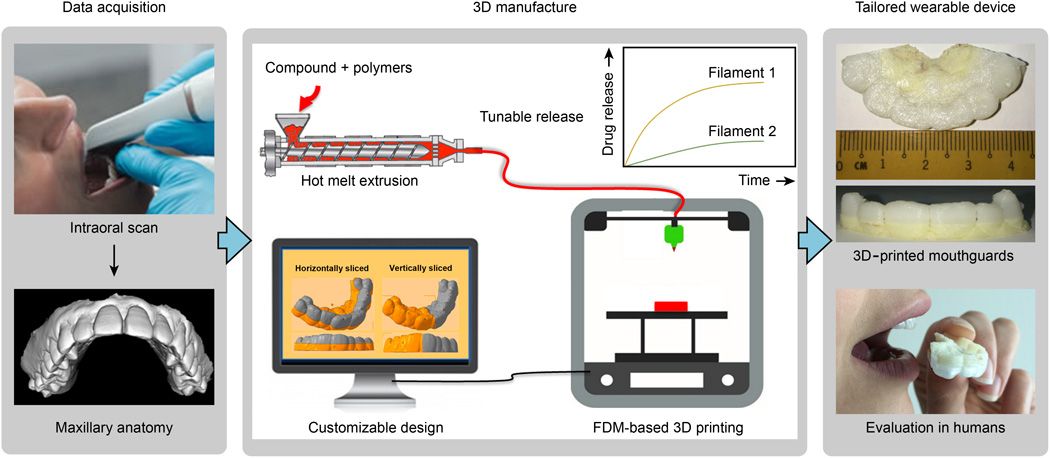 nine0005
nine0005
Photo: artificial pulmonary valve. Source: zortrax.com
The modern method of treatment consists in inserting a catheter through the femoral vein, through which an artificial valve is fed to the heart for implantation. This is a very complex operation that requires the doctor to have detailed knowledge of the individual characteristics of the patient's anatomy.
In the photo: a model of the heart during printing. Source: zortrax.com
Until now, doctors could only rely on a 3D model on a computer screen created from CT and MRI images, and such a reconstruction is not always enough to get a complete picture of the real organ and possible complications . nine0005
Source: zortrax.com
Having a highly detailed tactile model of a patient's living organ in preparation for surgery can be critical to its success.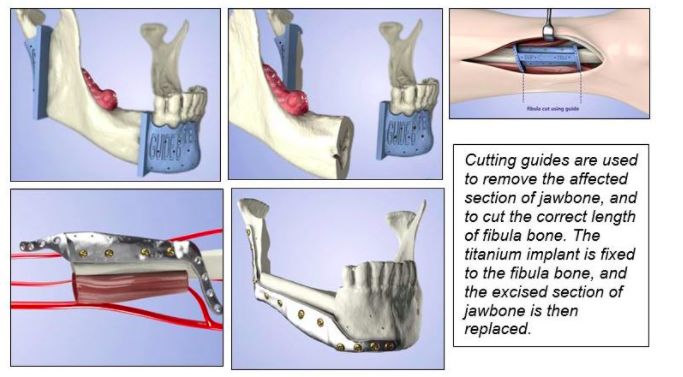 Even experienced surgeons have appreciated the potential of the new technology. Previously, it was difficult to notice individual features and deformations, now it has become tangible and accessible for closer study.
Even experienced surgeons have appreciated the potential of the new technology. Previously, it was difficult to notice individual features and deformations, now it has become tangible and accessible for closer study.
The model was printed within 24 hours. The Z-ULTRAT material was used to print the heart, and the Z-GLASS material was used to print the vessels. After a successful operation, the model was transferred to the University for student training. nine0005
Artificial corneas made on the Nano master SMP-III 3D bioprinter
Source: europepmc.org
In South Korea, about 2000 patients are waiting for corneal donation, and the waiting time for surgery is an average of six years. For patients who cannot find a suitable donor, it is possible to implant artificial corneas consisting of recombinant collagen and synthetic polymers. Unfortunately, they often do not take root and are not completely transparent.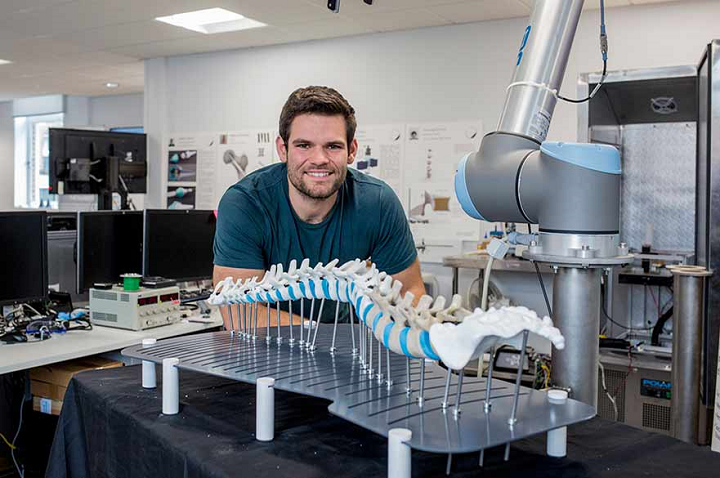 This is due to the special structure of the cornea in the form of lattice collagen fibrils, which has not yet been able to be reproduced. A team of researchers from Pohang University of Science and Technology and Kungpuk National University School of Medicine in South Korea have developed a method to 3D print an artificial cornea using patient tissue material. nine0005
This is due to the special structure of the cornea in the form of lattice collagen fibrils, which has not yet been able to be reproduced. A team of researchers from Pohang University of Science and Technology and Kungpuk National University School of Medicine in South Korea have developed a method to 3D print an artificial cornea using patient tissue material. nine0005
Source: ithl.co.kr
3D bioprinter with Nano master SMP-III microextrusion system, Musashi Engineering, Tokyo, Japan, with the following parameters:
-
print speed 130mm/min;
-
extrusion speed 0.0024 mm/s;
-
nozzle diameter 0.29 mm;
-
print temperature 4 °C.
The printed and biomaterial-filled cornea was then cultured in an incubator at 37 °C for four weeks. nine0005
nine0005
Source: europepmc.org
A 3D-printed artificial cornea made from decellularized corneal stroma and patient stem cells can completely replace a donor cornea in eye surgery. Since such a cornea is made up of materials derived from the patient's own tissues, it is completely compatible. Cellular 3D printing technology replicates the natural microenvironment of the eye, resulting in transparency similar to that of the human cornea. nine0005
Pohang University of Science and Technology Professor Jina Jang said:
"We are confident that this technology will restore vision to many patients suffering from corneal diseases."
Wake Forest Institute for Regenerative Medicine, mobile 3D printer for treating extensive wounds
the place of the damaged. In addition to the fact that this method is additionally traumatic for the victim, in some cases there may not be any healthy skin left on the body for use.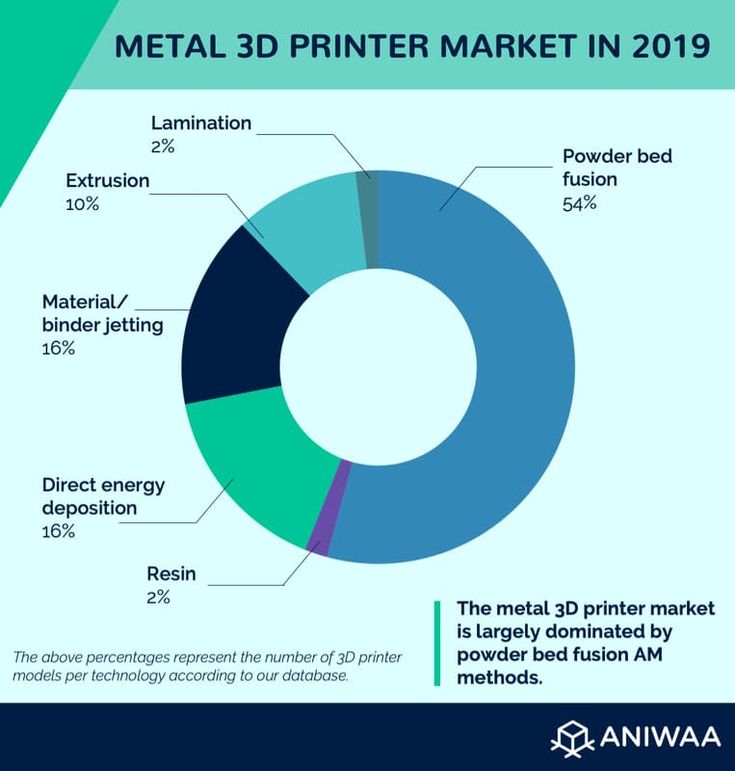 Wake Forest School of Medicine has developed a printer that can print skin cells grown from patient tissue directly onto a wound. nine0005
Wake Forest School of Medicine has developed a printer that can print skin cells grown from patient tissue directly onto a wound. nine0005
Source: 3dnatives.com
The ZScanner Z700 handheld 3D scanner is used to determine the size and depth of a wound. Based on this information, the 3D printer prints subcutaneous, dermal and epidermal skin cells at appropriate depths to completely cover the wound.
Source: 3dnatives.com
The 3D bioprinting system developed by scientists consists of a three-axis moving print head with eight 260 micron diameter nozzles with independent dispensers. Specifically for this device, the researchers created a bioink consisting of autologous dermal fibroblasts and epidermal keratinocytes in a hydrogel carrier. nine0005
Bite
Volt Bipolar Surgical Clamp for Laparoscopic Surgery stop bleeding during surgery. It was created for use in minimally invasive (sparing) surgery in 2016 and successfully tested on pig liver. nine0005
It was created for use in minimally invasive (sparing) surgery in 2016 and successfully tested on pig liver. nine0005
Source: bitegroup.nl
The design of the device allows easy adjustment of the shaft and tip geometry depending on the patient's anatomy and surgical requirements. Maneuverable shank - ±65° for lateral movements and ±85° up and down. Flexural stiffness of 4.0 N/mm for connection 1 and 4.4 N/mm for connection 2, significantly higher than previously available guided tools. The tip consists of two 3D printed titanium movable jaws with an opening angle of up to 170°. The instrument is connected to an Erbe electrosurgical unit and is able to successfully coagulate tissue at a temperature of 75 °C, reached in 5 seconds. nine0005
Conclusion
Source: intermercados.com.br
The use of additive technologies in medicine is expanding so rapidly that it is more like a revolution in healthcare.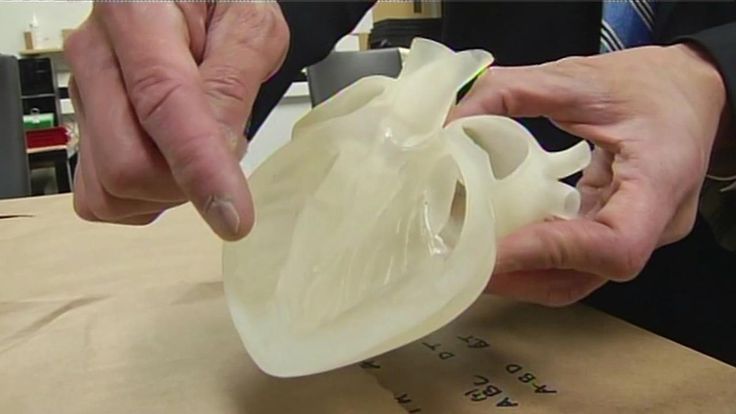 The use of 3D printing in medicine enables the individualization of medical devices, medicines and equipment, increases cost efficiency and labor productivity, reduces waiting times for patients and improves the availability of medical care. nine0005
The use of 3D printing in medicine enables the individualization of medical devices, medicines and equipment, increases cost efficiency and labor productivity, reduces waiting times for patients and improves the availability of medical care. nine0005
Source
Tags:
3D printing in medicine, dental implants, 3D printing for ear production, 3D printed models, Surgical instrument printing, Drug printing, Prosthetics and dentistry , Zortrax M20 3D Printer
5 innovative applications of 3D printing in medicine
Personalized and precise solutions in the medical field are becoming increasingly popular. New tools and advanced technologies bring doctors closer to patients by providing treatments and devices that meet the needs of each individual. nine0005
The expansion of 3D printing technologies in healthcare has made a huge contribution to improving the quality of medical services.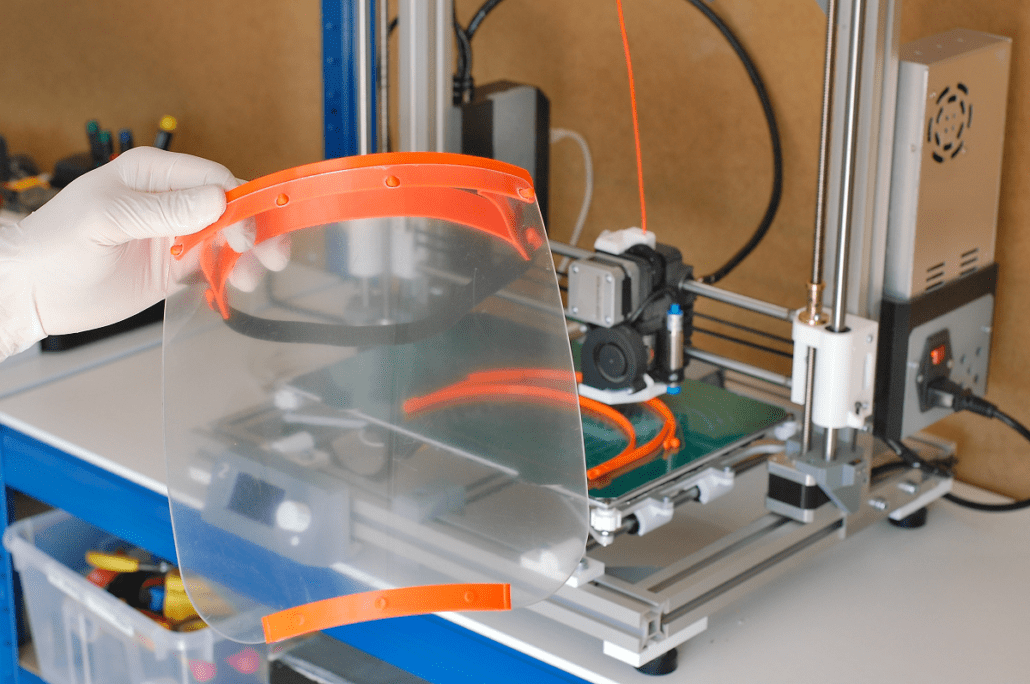 With new tools and treatment approaches developed using 3D printing, patients feel that their treatment becomes more comfortable and personal. For physicians, the new technology available allows them to better analyze complex cases and provides new tools that can ultimately raise standards of care.
With new tools and treatment approaches developed using 3D printing, patients feel that their treatment becomes more comfortable and personal. For physicians, the new technology available allows them to better analyze complex cases and provides new tools that can ultimately raise standards of care.
Later in this article, you'll learn about five areas, from models for surgical planning to vascular systems and bioreactors, in which 3D printing is used in healthcare, and why many healthcare professionals see great potential in this technology.
In today's medical practice, 3D printed anatomical models based on patient body scans are becoming more indispensable tools, as they provide more personalized and accurate treatment. As cases become more complex and standard case times become more important, visual and tactile anatomical models are helping surgeons to better understand their task, communicate more effectively, and communicate with patients more easily. nine0005
Medical professionals, hospitals and research institutes around the world use 3D printed anatomical models as a reference tool for preoperative planning, intraoperative imaging, and for sizing medical instruments or presetting equipment for both standard and very complex procedures, which is reflected in hundreds of scientific publications.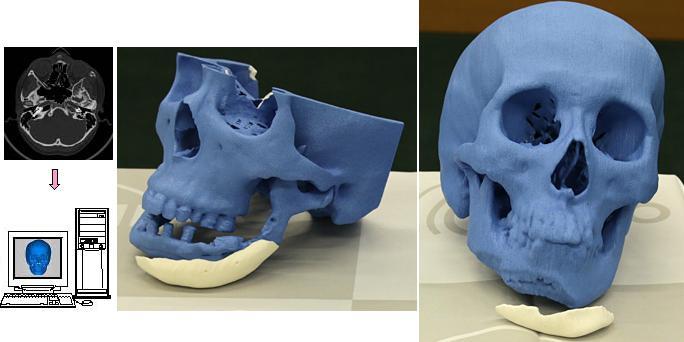
3D printing makes 3D printing affordable and easy to create customized patient anatomical models based on CT and MRI data. The peer-reviewed scientific literature demonstrates that they help clinicians better prepare for surgery, resulting in significant cost and time savings. At the same time, patient satisfaction is also increased through reduced anxiety and reduced recovery time. nine0005
Physicians can use individual patient anatomical models to explain the procedure to the patient, making it easier to obtain patient consent and reduce patient anxiety.
Preparation for surgery using preoperative models can also affect the effectiveness of the treatment. The experience of Dr. Michael Ames confirms this. After obtaining bone replications from the young patient's forearm, Dr. Ames realized that the injury was different from what he expected.
Based on this information, Dr. Ames chose a new soft tissue procedure that was much less invasive, reduced downtime, and resulted in much less scarring. Using imprinted bone replication, Dr. Ames explained the procedure to the young patient and his parents and obtained their consent. nine0005
Using imprinted bone replication, Dr. Ames explained the procedure to the young patient and his parents and obtained their consent. nine0005
Physicians can use patient-specific surgical models to explain the procedure beforehand, improving patient consent and lowering anxiety.
Result? The operation lasted less than 30 minutes instead of the originally planned three hours. With this reduction in operating time, the hospital avoided a cost of about $5,500 and the patient recovered faster.
According to Dr. Alexis Dang, Orthopedic Surgeon at UC San Francisco and Veterans Affairs Medical Center San Francisco: “All of our full-time orthopedic surgeons and almost all of our full-time surgeons part-time, used 3D printed models to treat patients at a Veterans Medical Center in San Francisco. We could all see that 3D printing improves the efficiency of our work.” nine0005
The advent of new biocompatible medical polymers for 3D printing has opened up opportunities for the development of new surgical instruments and techniques to further improve clinical operating procedures.![]() These include sterilizable trays, contoured surgical guides, and implant models that can be used to determine the size of an implant prior to surgery, helping surgeons reduce time and improve accuracy in complex procedures.
These include sterilizable trays, contoured surgical guides, and implant models that can be used to determine the size of an implant prior to surgery, helping surgeons reduce time and improve accuracy in complex procedures.
Anatomical model of a hand with elastic polymer skin for 3D printing. nine0005
Todd Goldstein, PhD, lecturer at the Feinstein Institute for Medical Research, is unequivocal about the importance of 3D printing technology to the work of his department. He estimates that if Northwell used 3D printed models 10% to 15% of the time, it could save $1,750,000 a year.
“Whether it's prototyping medical devices, complex anatomical models for our children's hospital, designing training systems, or making surgical templates for dental clinics, [3D printing technology] has increased our capabilities and reduced our costs in a variety of areas. In doing so, we were able to produce patient care instruments that would be nearly impossible to recreate without our highly sought-after stereolithography 3D printer,” says Goldstein.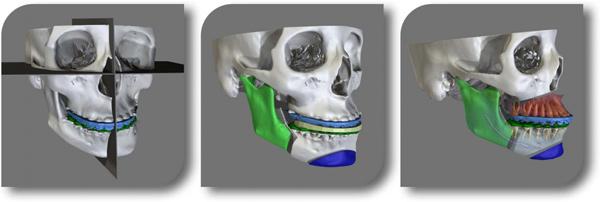 nine0005
nine0005
3D printing has become virtually synonymous with rapid prototyping. The ease of use and low cost of 3D printing in-house has also revolutionized product development, with many medical instrument manufacturers adapting the technology to produce entirely new medical devices and surgical instruments.
More than 90 percent of the top 50 medical device companies use 3D printing to create accurate medical device prototypes and fixtures and fittings to simplify testing. nine0005
According to Alex Drew, Principal Mechanical Engineer at DJO Surgical, an international medical device supplier, “Before DJO Surgical purchased [Formlabs 3D printer], we printed almost all of our prototypes outsourced. Today we are working with four Formlabs printers and are very pleased with the results. The speed of 3D printing has doubled, the cost has been reduced by 70%, and the level of detail allows you to effectively coordinate designs with orthopedic surgeons. nine0005
Medical companies such as Coalesce are using 3D printing to create accurate medical device prototypes.
3D printing helps speed up the design process by allowing complex designs to be iterated in days instead of weeks. When Coalesce was tasked with building an inhaler device that could digitally evaluate an asthma patient's inspiratory flow profile, outsourcing would result in a significant increase in production time for each prototype. Before sending the project files to a third party company for the physical implementation of the project, they would have to be carefully developed and carried through various iterations. nine0005
Instead, desktop stereolithographic 3D printing allowed Coalesce to handle the entire prototyping process in-house. The prototypes were suitable for use in clinical trials and looked just like the finished product. Moreover, when the company demonstrated the device, its customers mistook the prototype for the final product.
Overall, the introduction of in-house manufacturing resulted in an exceptional reduction in prototyping time by 80–90%.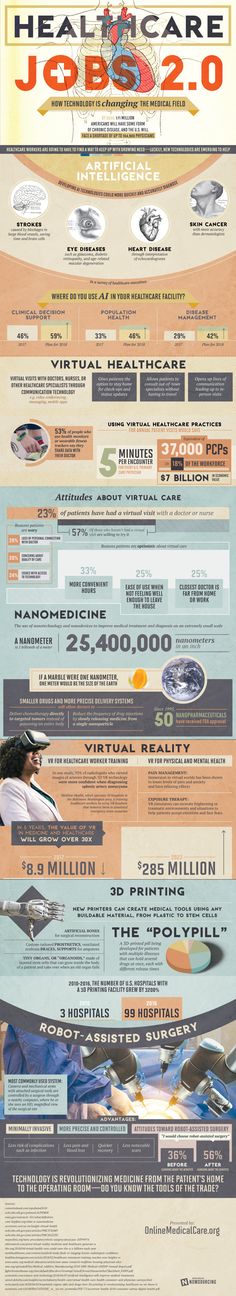 In addition, the models took only eight hours to print and were finished and painted in a matter of days, while outsourcing the same process would take a week or two.
In addition, the models took only eight hours to print and were finished and painted in a matter of days, while outsourcing the same process would take a week or two.
Hundreds of thousands of people lose limbs every year, but only a fraction of them are able to restore limb function with a prosthesis.
Conventional dentures are only available in a few sizes, so patients must adjust to what fits best. On the other hand, custom bionic prostheses that mimic the movements and grips of a real limb based on the impulses of the surviving limb muscles are so expensive that they can only be used by patients living in developed countries with the best medical insurance. In the case of children's prostheses, the situation is aggravated even more. Children grow up and inevitably outgrow their prostheses, which, as a result, require costly modifications. nine0005
The difficulty lies in the lack of manufacturing processes that would allow for individual orders at an affordable price.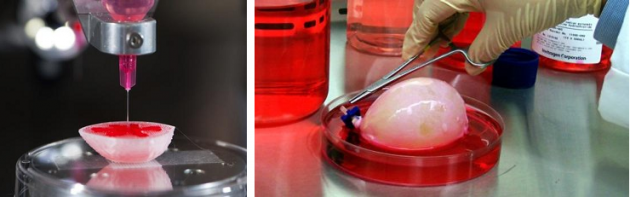 But increasingly, prosthetists are looking to reduce these high financial barriers to rehabilitation with the flexible design capabilities of 3D printing.
But increasingly, prosthetists are looking to reduce these high financial barriers to rehabilitation with the flexible design capabilities of 3D printing.
Initiatives like e-NABLE allow people around the world to learn about the possibilities of 3D printed prostheses. They are driving an independent movement in the prosthesis industry by offering information and free open source projects so that patients can get a custom-designed prosthesis for as little as $50. nine0005
Other inventors like Lyman Connor go even further. With only a small fleet of four desktop 3D printers, Lyman was able to fabricate and customize his first mass-produced prostheses. His ultimate goal? Create a customizable fully bionic arm that will cost incomparably less than similar prostheses that retail for tens of thousands of dollars.
Researchers at the Massachusetts Institute of Technology have also found that 3D printing is the best method for making more comfortable prosthetic sockets. nine0005
In addition, the low cost of manufacturing these prostheses, as well as the freedom that the ability to design custom designs brings, speaks for itself.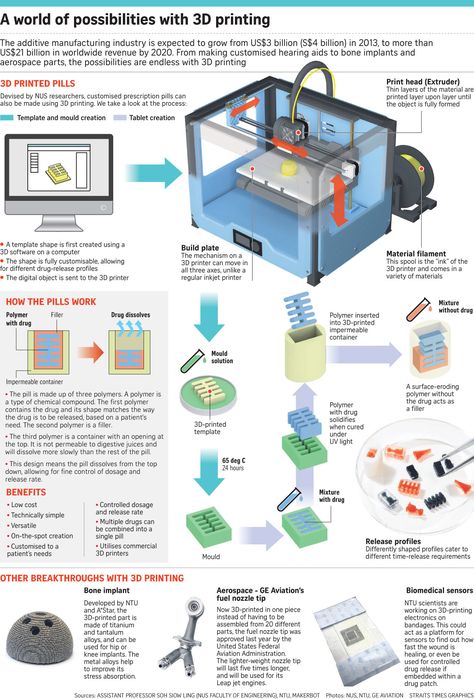 3D printed prostheses have a lead time of just two weeks, and then they can be tried and serviced at a much lower cost than traditional counterparts.
3D printed prostheses have a lead time of just two weeks, and then they can be tried and serviced at a much lower cost than traditional counterparts.
As costs continue to fall and material properties improve, the role of 3D printing in healthcare will no doubt become more important. nine0005
The same high financial barriers that are seen in prosthetics are common in the field of orthoses and insoles. Like many other patient-specific medical devices, custom orthoses are often not available due to their high cost and take weeks or months to manufacture. 3D printing solves this problem.
Confirmation is the example of Matej and his son Nick. Nick was born in 2011. Complications during preterm birth led to the fact that he developed cerebral palsy, a pathology that affects nearly twenty million people worldwide. Matei admired how determined his son was to overcome the limitations of his illness, but he was faced with a choice between a standard, off-the-shelf orthosis that would be uncomfortable for his son, or an expensive custom solution that would take weeks or months to manufacture and ship. , and from which the child would quickly grow. nine0005
, and from which the child would quickly grow. nine0005
He decided to take matters into his own hands and began to look for new ways to achieve his goal. Thanks to the opportunities provided by digital technologies, in particular 3D scanning and 3D printing, Matei and Nika's physiotherapists were able to develop a completely new innovative workflow for the manufacture of ankle orthoses through experiments.
The resulting 3D-printed, custom-fit orthosis that provides support, comfort, and motion correction helped Nick take his first steps on his own. This non-standard orthopedic device reproduced the functionality of the highest-class orthopedic products, at the same time it cost many times less and did not require any additional settings. nine0005
Professionals around the world are using 3D printing as a new method of manufacturing custom insoles and orthoses for patients and clients, as well as a range of other physiotherapy tools. In the past, the course of physiotherapy with the use of individual physiotherapy instruments carried many difficulties. Often there was a situation when patients had to wait a long time for a finished product, which at the same time did not provide proper comfort. 3D printing is step by step changing this status quo. Data confirms that 3D printed insoles and orthoses offer a more precise fit and lead to better therapeutic outcomes, which means greater comfort and benefit for patients. nine0005
Often there was a situation when patients had to wait a long time for a finished product, which at the same time did not provide proper comfort. 3D printing is step by step changing this status quo. Data confirms that 3D printed insoles and orthoses offer a more precise fit and lead to better therapeutic outcomes, which means greater comfort and benefit for patients. nine0005
Autografts, transplantation of tissue from one area of the body to another, or transplantation of a donor organ are the usual treatments for patients with severe organ damage. Researchers in bioprinting and tissue engineering hope to expand this list soon, adding on-demand fabrication of tissues, blood vessels, and organs.
3D bioprinting is an additive manufacturing process that uses materials known as bioink (a combination of living cells and a compatible substrate) to create tissue-like structures that can be used in medicine. Tissue engineering combines new technologies, including bioprinting, which allow growing replacement tissues and organs in the laboratory for use in the treatment of injuries and diseases.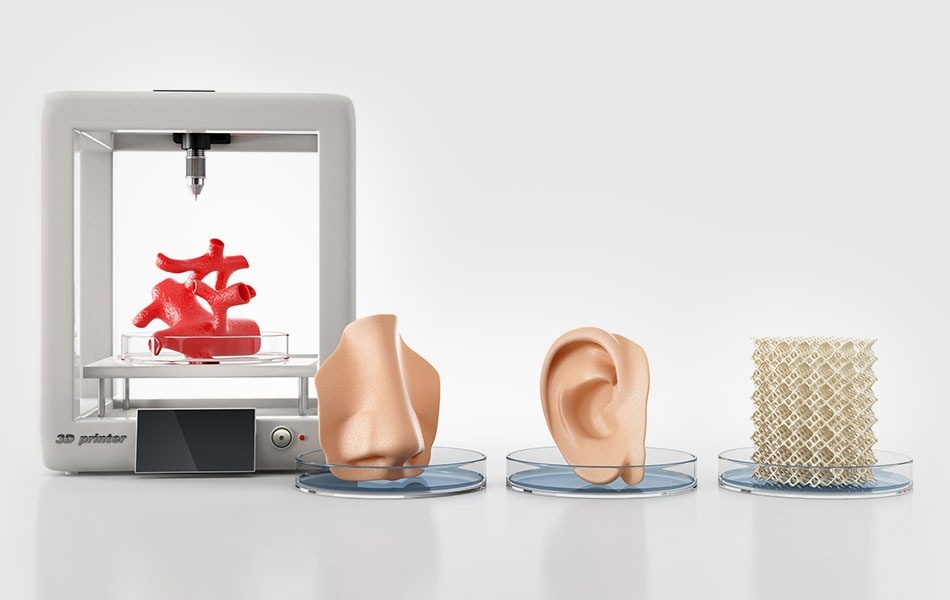 nine0005
nine0005
Using high-precision 3D printing, researchers such as Dr. Sam Pashne-Tala from the University of Sheffield are breaking new ground in tissue engineering.
In order to direct cell growth to form the necessary tissue, Dr. Pashne-Tala grows living cells on a laboratory scaffold that provides a template of the required shape, size and geometry. For example, to create a blood vessel for a patient with cardiovascular disease, a tubular structure is needed. The cells will multiply and cover the scaffold, taking on its shape. Then the scaffold is gradually destroyed, and the living cells take the form of the target tissue, which is cultured in a bioreactor - a chamber that contains the cultured tissue and can reproduce the internal environment of the body so that the cultured tissue acquires the mechanical and biological characteristics of organic tissue. nine0005
3D printed bioreactor chamber with tissue engineered aorta miniature inside. The tissue is cultured in a bioreactor to acquire the mechanical and biological characteristics of the organic tissue.
3D printed bioreactor chamber with tissue engineered aorta miniature inside. The tissue is cultured in a bioreactor to acquire the mechanical and biological characteristics of the organic tissue.
This will allow scientists to design patient-specific vascular grafts, expand surgical care, and provide a unique platform for testing new vascular medical devices for people suffering from cardiovascular disease, which is currently the leading cause of death worldwide. The ultimate goal is to create blood vessels that are ready for implantation in patients. Since tissue engineering uses cells taken from a patient in need of treatment, this eliminates the possibility of rejection by the immune system, which is the main problem of modern transplantology. nine0005
3D printing has proven its ability to solve the problems that exist in the production of synthetic blood vessels, in particular, the difficulty of recreating the required accuracy of the shape, size and geometry of the vessel. The ability of printed solutions to clearly reflect the specific characteristics of patients was a step forward.
The ability of printed solutions to clearly reflect the specific characteristics of patients was a step forward.
According to Dr. Pashne-Tal: “[Creating blood vessels using 3D printing] makes it possible to expand the possibilities of surgical care and even create designs of blood vessels for a specific patient. Without the existence of high-precision affordable 3D printing, the creation of such forms would not be possible.” nine0005
We are witnessing significant advances in the development of biological materials that can be used in 3D printers. Scientists are developing new hydrogel materials that have the same consistency as organ tissues present in the human brain and lungs, which can be used in a range of 3D printing processes. Scientists hope that they will be able to implant them into the body as a "scaffold" for cell growth.
Although bioprinting of fully functional internal organs such as the heart, kidneys and liver still looks futuristic, hybrid 3D printing at very high speed opens up more and more new horizons.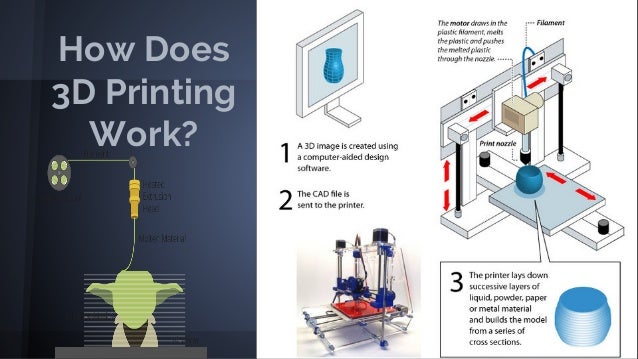 nine0005
nine0005
It is expected that sooner or later the creation of biological matter on laboratory printers will lead to the generation of new, fully functional 3D printed organs. In April 2019, scientists at Tel Aviv University 3D-printed the first heart using biological tissue from a patient. A tiny copy was created using the patient's own biological tissues, which made it possible to fully match the immunological, cellular, biochemical and anatomical profile of the patient. nine0005
“At this stage, the heart we printed is small, the size of a rabbit heart, but normal-sized human hearts require the same technology,” says Prof. Tal Dvir.
The first 3D bioprinted heart created at Tel Aviv University.
Precise and affordable 3D printing processes, such as desktop stereolithography, are democratizing access to technology, enabling healthcare professionals to develop new clinical solutions and quickly produce medical devices with individual characteristics, and doctors around the world to offer new types of therapy.