3D printing joint replacement
3D printing for joint reconstruction in compromised bone
Aug. 06, 2021
Pathological acetabular fracture and superior migration of the femoral head
Pathological acetabular fracture and superior migration of the femoral head
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, an anteroposterior X-ray of the right hip reveals pathological acetabular fracture and superior migration of the femoral head into the acetabular defect.
Pathological acetabular fracture with loss of the posterior wall and posterior column
Pathological acetabular fracture with loss of the posterior wall and posterior column
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, an obturator oblique X-ray of the pelvis shows a pathological acetabular fracture with loss of the posterior wall and posterior column, and posterior subluxation of the right hip joint.
Superior and posterior acetabular bone loss
Superior and posterior acetabular bone loss
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, an intraoperative photo reveals severe superior and posterior acetabular bone loss. Only the inferior aspect of the acetabulum resembles native anatomical architecture.
Final reconstruction
Final reconstruction
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, a postoperative X-ray shows the final reconstruction. A highly porous tantalum augment was placed in the superior acetabular defect, followed by insertion of a highly porous tantalum revision shell obtaining a press fit between the augment and the remaining pubis and ischium. An additional buttress augment, also made of highly porous tantalum, was applied as additional fixation to the intact ilium. A cemented stem total hip arthroplasty was also used, due to plans for future radiation treatments. After surgery, the patient experienced significant pain relief and regained the ability to walk.
An additional buttress augment, also made of highly porous tantalum, was applied as additional fixation to the intact ilium. A cemented stem total hip arthroplasty was also used, due to plans for future radiation treatments. After surgery, the patient experienced significant pain relief and regained the ability to walk.
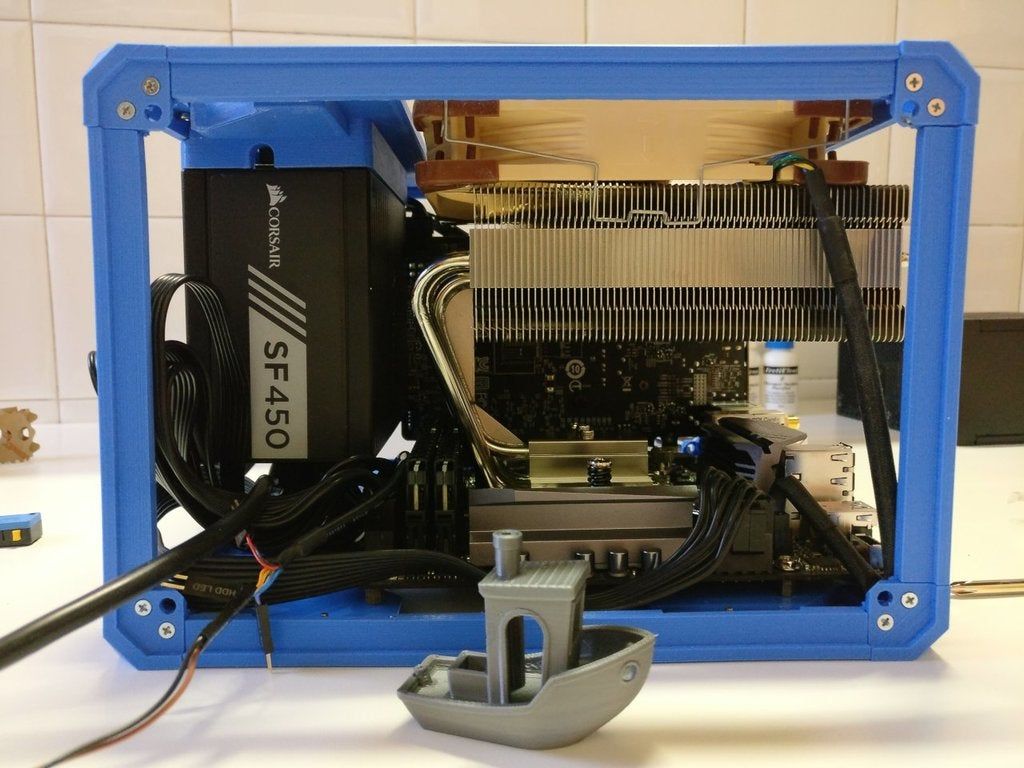
Joint reconstruction is particularly challenging in the setting of complex bony defects or radiation therapy. Mayo Clinic routinely uses 3D-printed models to optimize surgical outcomes for individual patients.
"This technology allows us to re-create a patient's bony defects and surgically correct them to restore joint function," says Cory G. Couch, M.D., an orthopedic surgeon at Mayo Clinic in Rochester, Minnesota, with fellowship training in orthopedic oncology and joint reconstruction. "We are able to model and fill in even very large bony defects created by tumors and tumor resections."
Mayo Clinic has the largest point-of-care additive manufacturing facility in the United States, staffed by radiologists and biomedical engineers. "They work in close conjunction with us," Dr. Couch says. "Complex joint reconstructions require multidisciplinary care from imaging experts and from radiation and medical oncologists, as well as orthopedic surgeons."
"They work in close conjunction with us," Dr. Couch says. "Complex joint reconstructions require multidisciplinary care from imaging experts and from radiation and medical oncologists, as well as orthopedic surgeons."
The 3D-printing technology is used in complex reconstructions of the knee, hip and pelvis for individuals with sarcoma or metastatic cancer. The technology also facilitates complex joint replacements associated with infection or the failure of a previous replacement joint.
The models are created using individual patients' CT scans or MRI or both and sterilizable materials. "In the operating room, we have the model on the table right next to the patient. That helps us to identify optimal implant placement or screw fixation," Dr. Couch says.
Arthroplasty and cancer care
Mayo Clinic commonly treats patients with bony defects due to cancer. Radiation and medical oncologists meet regularly with orthopedic surgeons to discuss patients and plan treatment.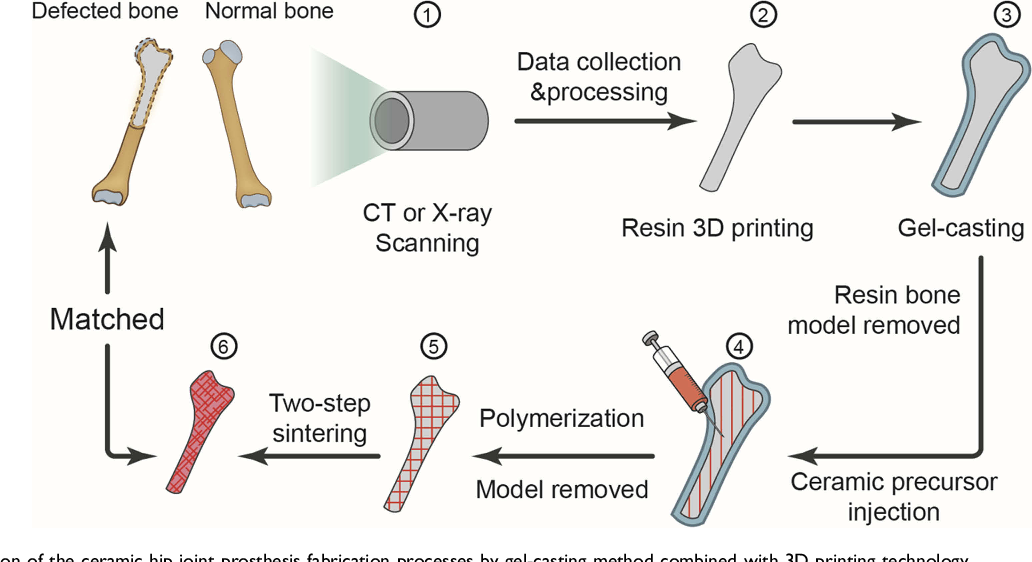 Surgical reconstruction of the hip or knee may precede or follow radiation treatment.
Surgical reconstruction of the hip or knee may precede or follow radiation treatment.
"We typically make these decisions based on the tumor type and location, but sometimes on a case-by-case basis," Dr. Couch says. "Sometimes having chemotherapy or radiation therapy upfront will reduce the size of the tumor, facilitate removal and optimize the maintenance of function."
Historically, patients having total hip arthroplasty after pelvic radiation experienced high rates of implant loosening when traditional uncemented acetabular components were used. But Mayo Clinic orthopedic researchers have found that 100% of modern, porous titanium components remained radiologically well fixed 10 years after implantation in patients having total hip arthroplasty after pelvic radiation. As described in the Journal of Arthroplasty, the mean overall pelvic radiation dose for the 33 patients in the study exceeded the radiation threshold for dose-related bone effects.
A separate study, described in The Journal of Bone and Joint Surgery, found that for patients with periacetabular metastatic disease, acetabular reconstruction using highly porous tantalum components provided a more durable construction and fewer complications compared with procedures using the cemented technique.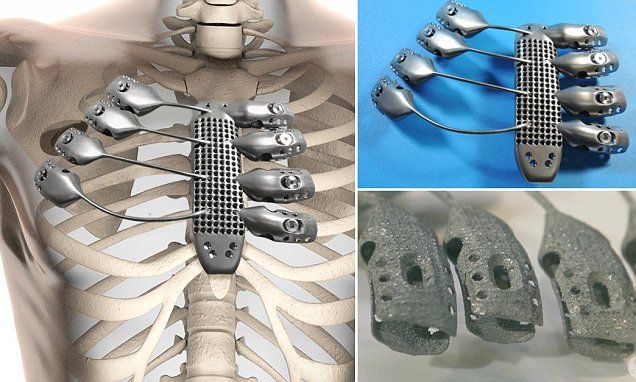
"Advances in medical care and radiotherapy mean that more cancer patients are living longer," Dr. Couch says. "Restoring patients' joints allows them to return to walking soon after surgery. The goal is for these patients to spend the remainder of their lives doing the things they want to do, relatively pain-free."
For more information
Wellings EP, et al. Contemporary porous titanium acetabular components for total hip arthroplasty after pelvic radiation. Journal of Arthroplasty. 2021;36:1714.
Houdek MT, et al. Comparison of porous tantalum acetabular implants and Harrington reconstruction for metastatic disease of the acetabulum. The Journal of Bone and Joint Surgery. 2020;102:1239.
How Does a 3D Printed Knee Replacement Work?
Medical professionals now use 3D printing to create titanium jaws, hearing aids, limbs, organs, and in the production of customized knee replacements.
Invented by Chuck Hull back in 1983, 3D printing is the process of using a printer to transform a digital three-dimensional model into a physical object.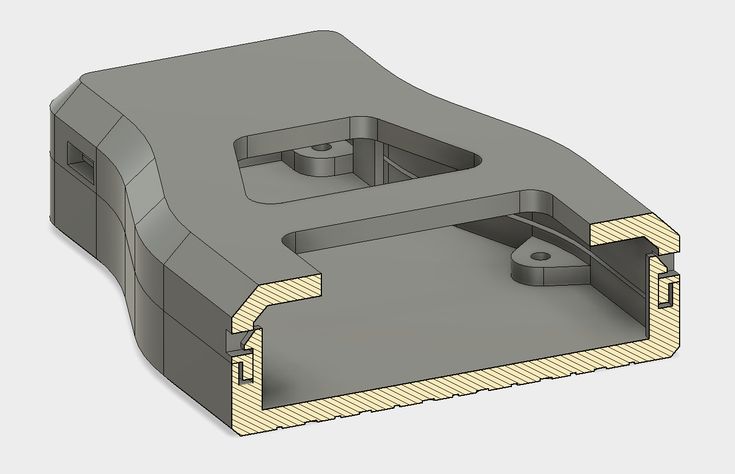 Learn how a 3D printed knee replacement works and how Conformis can transform a digital three-dimensional model into a physical object.
Learn how a 3D printed knee replacement works and how Conformis can transform a digital three-dimensional model into a physical object.
Additive Manufacturing
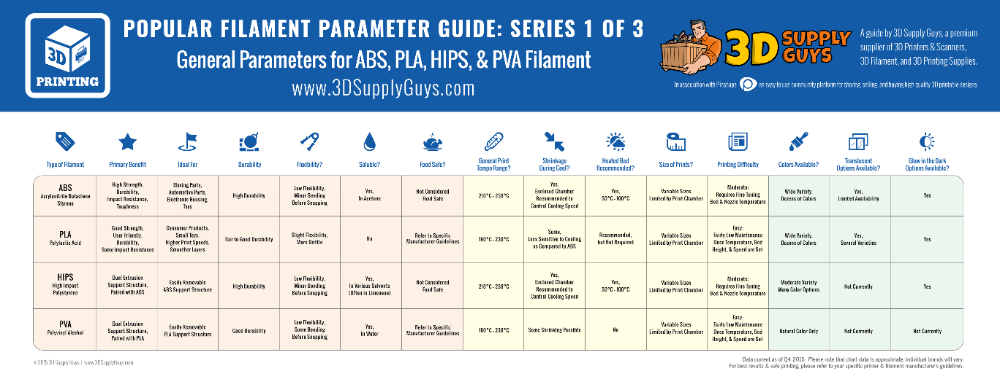
There are two basic types of manufacturing: subtractive and additive. In subtractive manufacturing, manufacturers start with a large block of material then shave away, or subtract, what they do not need.
Additive manufacturing is the direct opposite of subtractive manufacturing – manufacturers add layer upon layer of material to achieve the desired effect. 3D printing is additive manufacturing, as special print heads lay down layers of various materials to create products.
While subtractive processes have been the mainstay of manufacturing for decades and are still the norm, 3D printing and other additive manufacturing processes have distinct benefits. Subtractive manufacturing requires stripping away material, creating a great amount of waste, to make each component of a piece then assembling all the components to create the finished product. 3D printing allows manufacturers to create very complex products containing multiple materials with very little waste.
3D printing allows manufacturers to create very complex products containing multiple materials with very little waste.
A 3D printed knee replacement consists of:
- Nylon
- ABS plastic
- Resin
- Stainless steel
- Gold and silver
- Titanium
- Ceramic
- Gypsum
The ability to use a variety of materials allows manufacturers to make incredibly strong and complex items. Many of the materials, especially titanium, are suitable for use in medical devices because of their strength and lower risk for rejection. By building objects up in layers, 3D printing can produce objects that are hollow or extremely intricate.
3D Printed Knee Replacement: What We Print and Why
At Conformis, we use the latest in 3D printing (additive manufacturing) technology to create one set of surgical instrumentation, called iJigs, per patient. These instruments allow your surgeon to ensure that your customized implant is positioned correctly.
To create the iJigs, a robotic arm deposits a layer of powdered nylon onto a tray. A laser then outlines each patient-specific shape, fusing the powder into solid shapes. This process is repeated many times, until the layers have built up and the final shapes of the instruments are created. When the jigs are removed from the 3D printer, they are consolidated in one rectangular package. The individual pieces are then removed and sterilized before being packaged for shipment to your surgeon. We also use 3D printing to create the wax molds the metal implants are cast in.
What’s the benefit? Since each of our implants is customized to the patient, this process allows us to quickly build all the parts required for a knee replacement in a relatively short time. This also allows us to make updates to our implants more regularly since we don’t have existing inventory to use up first.
Click here to learn more about our technology and customization processes.
3D printed joints will help patients start a new life
Archive
Each new discovery guarantees even more amazing discoveries in the very near future.
 The media is literally seething with news about the deeds of scientists and doctors, the commission of which used to take decades.
The media is literally seething with news about the deeds of scientists and doctors, the commission of which used to take decades. Model (left) and printed joint (right)
One of the latest advances in medicine that would not have been possible without 3D printing has to do with joint replacement. Today, there are very few ways to manage joint pain, with joint replacement surgery being considered a last resort. All over the world, people suffer from manifestations of arthritis and joint pain. It is becoming increasingly clear that this issue needs special attention.
Joint 3D printer
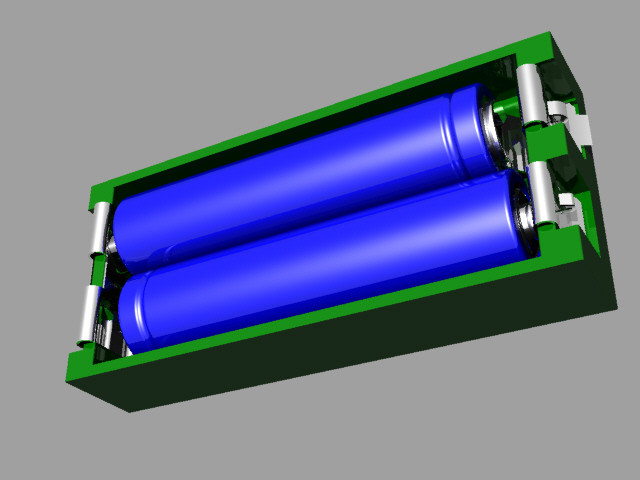
Artificial joints are usually made from plastics and metals, materials that the human body considers foreign. In addition, these materials are destroyed 10-20 years after the operation, and the joint again loses its functionality. In other words, the artificial joints that are currently being installed cannot be considered a reliable and long-term solution.
In an attempt to find relief from the acute pain that plagues so many people, physicians Rita Kandel, Mark Greenpas and Endras Nagy of the Samuel Lunenfeld Research Institute at Mount Sinai Medical Complex teamed up with bioengineers, biologists and surgeons in an attempt to explore the possibilities of using a patient's own tissues for creating new bones. As interest grew, Dr. Kandel began working with Drs. Pilliar and Dr. Toysercani of the University of Toronto and Waterloo to see if 3D printing could become a tool for creating joints. Here is how Dr. Kanel describes the essence of this interdisciplinary collaboration:
“First, Dr. Toisercani prints a biodegradable joint. Then we take the patient's stem cells and build up real tissue (cartilage, etc.) on this joint. The damaged joint is replaced with a joint made entirely of the patient's tissues. It's just incredible."
Dr. Rita Kandel of Mount Sinai Medical Complex
The 3D printing process begins with an x-ray of a patient's injured joint. The data obtained is converted into a three-dimensional computer model, which is immediately sent for printing. A 3D printer grows an exact copy of the joint from a special porous material. This material promotes cell growth and is easily overgrown with cartilage tissue. Gradually, the bone takes shape, and the material is destroyed. As a result, only the bone remains, which is no different from the original. Here is how Dr. Kandel describes the process and its benefits:
The data obtained is converted into a three-dimensional computer model, which is immediately sent for printing. A 3D printer grows an exact copy of the joint from a special porous material. This material promotes cell growth and is easily overgrown with cartilage tissue. Gradually, the bone takes shape, and the material is destroyed. As a result, only the bone remains, which is no different from the original. Here is how Dr. Kandel describes the process and its benefits:
“A joint is a highly complex, shaped structure, all of which work together to ensure painless movement of the knees and elbows. Thanks to 3D printing, we were able to create an implant that perfectly fits the damaged joint. Our work is a brilliant example of individualized medicine, because the tissues that make up these joints belong to the very patients who need surgery.”
At the moment, this method has not yet been sufficiently developed. Much more research and experimentation needs to be done before it will be possible to move on to the introduction of these operations into ordinary medical practice.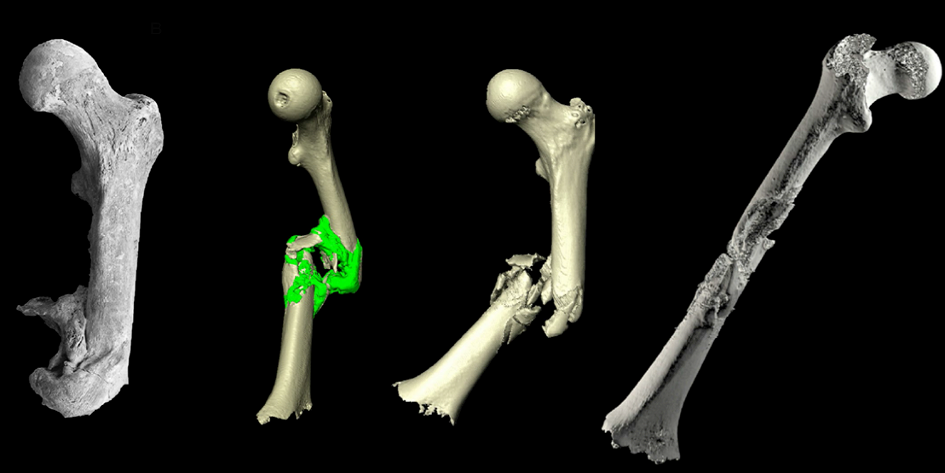 The medical team hopes to have the procedure tested on humans in the next few years. She is very optimistic about the future of 3D printed artificial joints.
The medical team hopes to have the procedure tested on humans in the next few years. She is very optimistic about the future of 3D printed artificial joints.
Article prepared for 3DToday.ru
Subscribe to the author
Subscribe
Don't want
1
The world's first ankle joint was reconstructed with a special 3D printed prosthesis (Rizzoli Bologna Hospital, Italy )
A patient was operated on in Italy who lost joint function after a motorcycle accident. After 13 years, a man can walk.
Operated in October at the Rizzoli Orthopedic Institute in Bologna, a 57-year-old patient who lost joint function after a traffic accident has returned to walking. Record-breaking surgery by the team of Professor Faldini.
Prof. Cesare Faldini, Director of the Orthopedic Clinic I, coordinated the team that performed the implantation of the prosthesis to replace the entire ankle: starting from the patient's anatomy, a 3D-printed implant was created to fit the patient perfectly.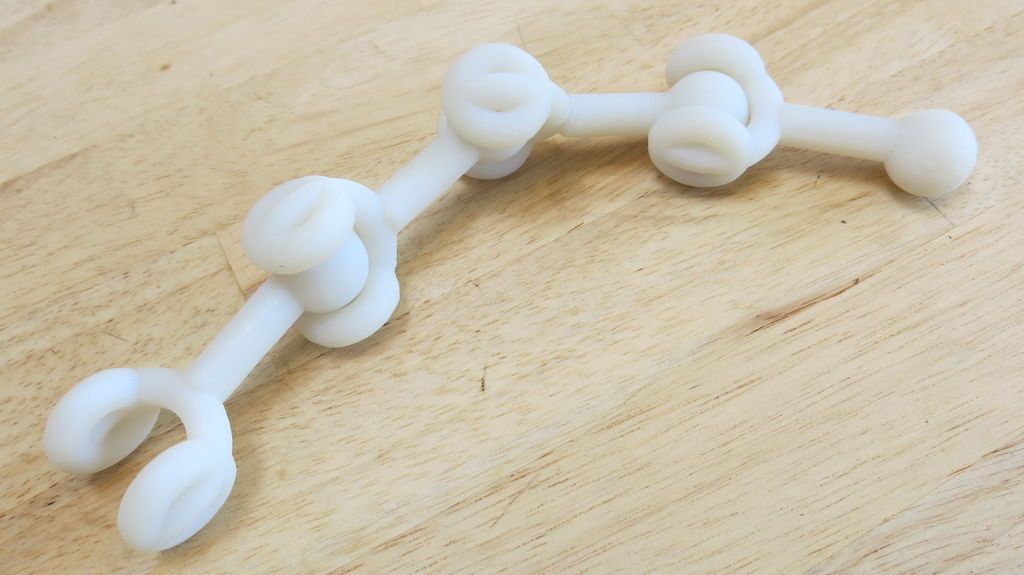
The technique was developed by thanks to a collaboration between orthopedic surgeons and engineers from Rizzoli and Alma Mater. The patient, a 57-year-old man from Lombardy, lost his ability to work in 2007 and was therefore no longer able to use his leg due to an accident. « Previously, he was considered inoperable due to an anatomical change in the ankle caused by an accident. Today, 13 years after the accident, - Professor Faldini explains - he walks regularly and feels good. This method, , explains Faldini, was created for patients who cannot get traditional prostheses and therefore risk not returning to walking . After the operation, which lasted about an hour, the patient got up and was scheduled for rehabilitation program .”
Today, thanks to a 3D-printed prosthesis, the 57-year-old patient is able again. « The Rizzoli intervention - explained Professor Faldini - represents an absolute innovation worldwide. This is the first time that an ankle implant prosthesis has retained ligament isometry. The prosthesis is 3D printed and implanted using a customized cutting guide technique that saves time and bone in a patient suffering from post-traumatic joint destruction ".
This is the first time that an ankle implant prosthesis has retained ligament isometry. The prosthesis is 3D printed and implanted using a customized cutting guide technique that saves time and bone in a patient suffering from post-traumatic joint destruction ".
The procedure was two stages : the patient had a computed tomography of the ankle in an upright position a few weeks before the operation. Following this examination, a careful 3D reconstruction made it possible to obtain a 3D model of the patient's leg and foot using software and procedures developed in the Rizzoli Movement Analysis Laboratory by the research team of engineer Alberto Lirdini.
Orthopedic surgeons and biomedical engineers simulated the computer intervention, working on the shape and size of each prosthetic component to fit the patient's specific anatomical characteristics, until finding the optimal combination of the astragalus and tibia components, the two bones that make up the ankle.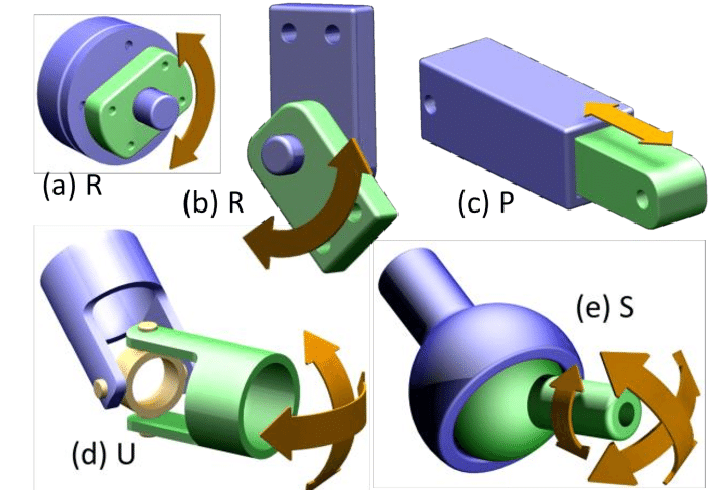
Once the geometry of the prosthesis and its ideal position had been established, a corresponding bone and plastic model was made in a 3D printer for final manual testing. Once the most satisfactory result for both the surgeon and the engineer had been achieved and confirmed, the actual prosthesis for the final implant was finally cast in chromium-cobalt-molybdenum alloy using ECM technology (electron beam melts the metal powder layer by layer according to the file) .
The last stage is the hospitalization of the patient. “ Surgery ,” the Rizzoli doctors emphasize, “, despite the complexity associated with the presence of a serious change in the anatomy, has become less invasive thanks to the use of personalized guides. These guides are built into the 3D printing and allow only a precise portion of the cartilage and accessory bone to be removed, preserving the bone needed to accommodate the prosthetic components.”
Both the tibia and the talus prepared in this way were able to optimally "receive" an individual prosthetic implant: already at the end of the operation in the operating room, the ideal position and excellent restoration of the arch of the ankle joint could be assessed.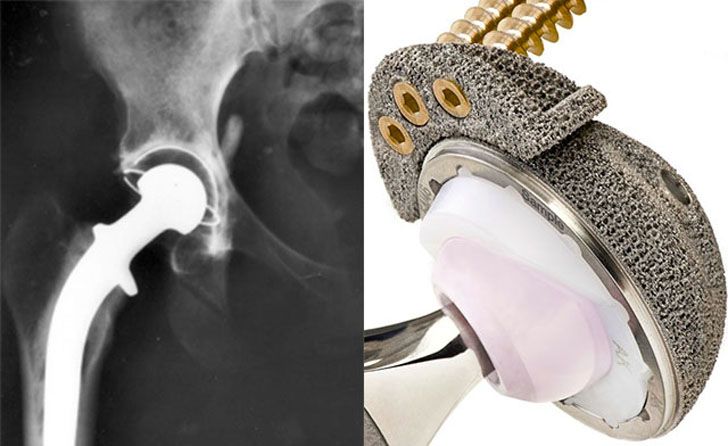
Personalized protocol
The postoperative protocol has also been modified thanks to the collaboration with the Rizzoli Department of Physical and Rehabilitation Medicine, headed by Prof. Maria Grazia Benedetti. « This strategy, developed for patients with disabilities due to serious accidents that caused irreparable damage to the articular function of the ankle joint , commented Rizzoli CEO Mario Cavalli, is also the result of a collaboration between Rizzoli, with its orthopedic surgeons, engineers , physiotherapists, as well as the institutes of anatomy and engineering of the University of Bologna. The development of various technological, engineering and medical skills coordinated in the IRCCS, the Scientific Institute of Hospitalization and Nursing, such as Rizzoli, has made it possible to provide a highly innovative clinical response to patients for whom, until today, surgery could not do anything to improve their disability ".
Source:
Computer, movement analysis laboratory Rizzoli
Other materials:
- A virtual model of the ISS, a laser breathalyzer and a 3D metal printer: how the production of Laser Systems works
- ANSYS will introduce more flexible software licensing and major updates in the new 2020 R1 release
- 3D printer or machine? Automotive Prototyping Methods Compared
- 3D Printing: The Healthcare Revolution
- Everything You Need to Know About 3D Printing Polycarbonate (PC)
Attention!
We accept news, articles or press releases
with links and images.
Learn more