3D printing human ears
Woman Gets New Ear Made of Her Own 3D-Printed Cells
June 2, 2022 – Doctors in the U.S. have successfully transplanted a 3D-printed ear implant that uses the patient’s cells.
The first “bioprinted living tissue implant” went to a 20-year-old woman, who was born with a small and misshapen ear. The implant was printed in a shape that matched her other ear and “will continue to regenerate cartilage tissue,” which will help it to look and feel like a natural ear, according to The New York Times.
3DBio Therapeutics, a regenerative medicine company based in New York City, is doing an early-stage clinical trial with patients who have microtia, a rare congenital disorder where one or both outer ears are absent or underdeveloped. The disorder affects about 1,500 babies born in the U.S. each year and typically has limited reconstruction options.
3DBio and the Microtia-Congenital Ear Deformity Institute, in Texas, did the human ear reconstruction using the AuriNovo implant, which received FDA designations for orphan drug and rare pediatric disease in 2019.
“As a physician who has treated thousands of children with microtia from across the country and around the world, I am inspired by what this technology may mean for microtia patients and their families,” Arturo Bonilla, MD, a pediatric ear reconstructive surgeon specializing in microtia who performed the surgery, said in a statement.
The clinical trial is looking at how safe and effective the AuriNovo implant will be, with the goal of replacing current ear reconstruction surgeries that require doctors to use rib cartilage or certain implants.
“The AuriNovo implant requires a less invasive surgical procedure than the use of rib cartilage for reconstruction,” Bonilla said. “We also expect it to result in a more flexible ear than reconstruction with a PPE [porous polyethylene] implant.”
3DBio announced the results of the patient’s surgery in a news release on Thursday, which didn’t include technical details of the procedure because of privacy reasons. The company said the FDA has reviewed the clinical trial design and set strict manufacturing standards. The data is expected to be published in a medical journal when the study is complete.
The data is expected to be published in a medical journal when the study is complete.
The manufacturing process begins by taking a small sample of the patient’s ear to create billions of cartilage cells. The living cells are then mixed with the company’s collagen-based “bio ink,” which is safe for the body. The 3D bio-printer uses that ink to create an object based on a digital model that copies the patient’s healthy ear.
The ear implant procedure, which was done in March, marks one of several recent breakthroughs in organ and tissue transplants, the Times reported. Numerous companies across the world are developing implants that use 3D-printed technology to help patients with deformities and other health issues.
With more research, the technology could be used to make other body parts, including spinal disks, noses, knee cartilage, rotator cuffs, and reconstructive tissue for lumpectomy procedures, 3DBio said. In the more distant future, 3D printing could potentially create vital organs, such as livers, kidneys, and pancreases.
The clinical trial, which is also enrolling patients at Cedars-Sinai Medical Center in Los Angeles, has included 11 volunteers ages 6 to 25 so far. The patients will be followed for 5 years to evaluate long-term safety and satisfaction.
A surgically implanted, 3D-printed ear marks a medical advance
Science News
3DBio Therapeutics, the company that manufactured the ear, said in a news release Thursday said the procedure had been a success.
An ear implant sits within cell culture media atop the metal base of a printer.3DBio TherapeuticsBy Evan Bush
In a first for medicine, a surgeon has successfully implanted an outer ear developed and 3D-printed in a laboratory.
A 20-year-old woman who was born with the congenital disorder microtia and had one misshapen ear received the new appendage in March, 3DBio Therapeutics, the company that manufactured the ear, said in a news release Thursday.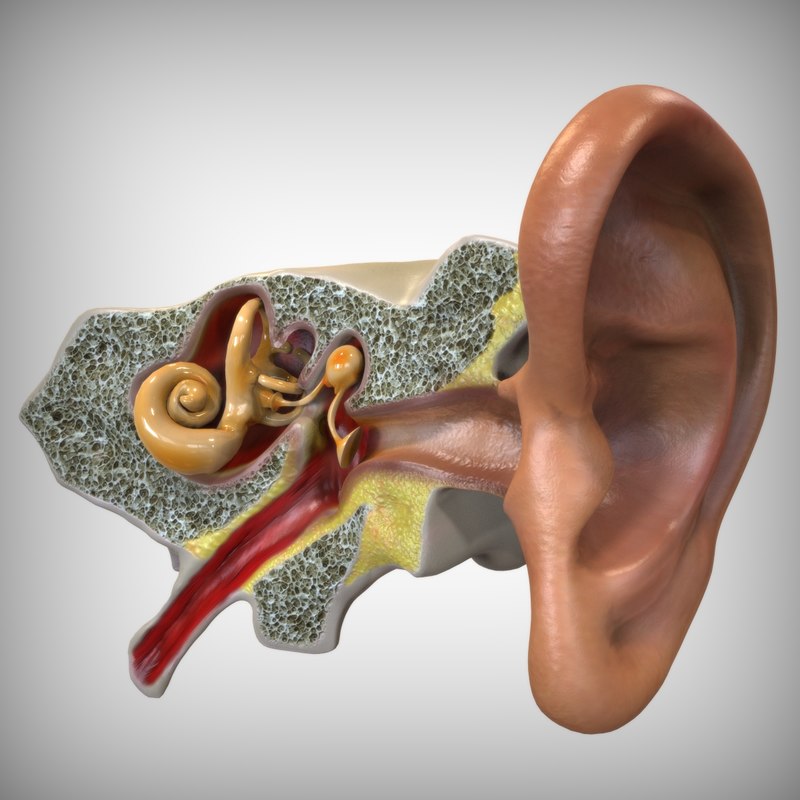 The ear was constructed from her own cells as a mirror replica of her other ear.
The ear was constructed from her own cells as a mirror replica of her other ear.
Outside experts said it is the first time that 3D-printed tissue had been implanted into a human body.
A collagen ear implant sample on display.3DBio Therapeutics“It’s a big milestone,” said Dr. Anthony Atala, the director of the Wake Forest Institute for Regenerative Medicine. “Ears have been implanted by hand. It’s now using a printer, which helps automate the process, which is important for the field.”
The milestone could open doors for investment and new excitement around 3D tissue printing, potentially paving the way for new therapies in regenerative medicine.
“I’m hoping these kinds of success will build enthusiasm and understanding this is moving from the realm of science fiction into reality,” said Adam Feinberg, a professor of biomedical engineering at Carnegie Mellon University and chief technology officer for Fluidform, a 3D bioprinting startup.
Microtia patients are born without outer ears or with appendages that are smaller and different in shape.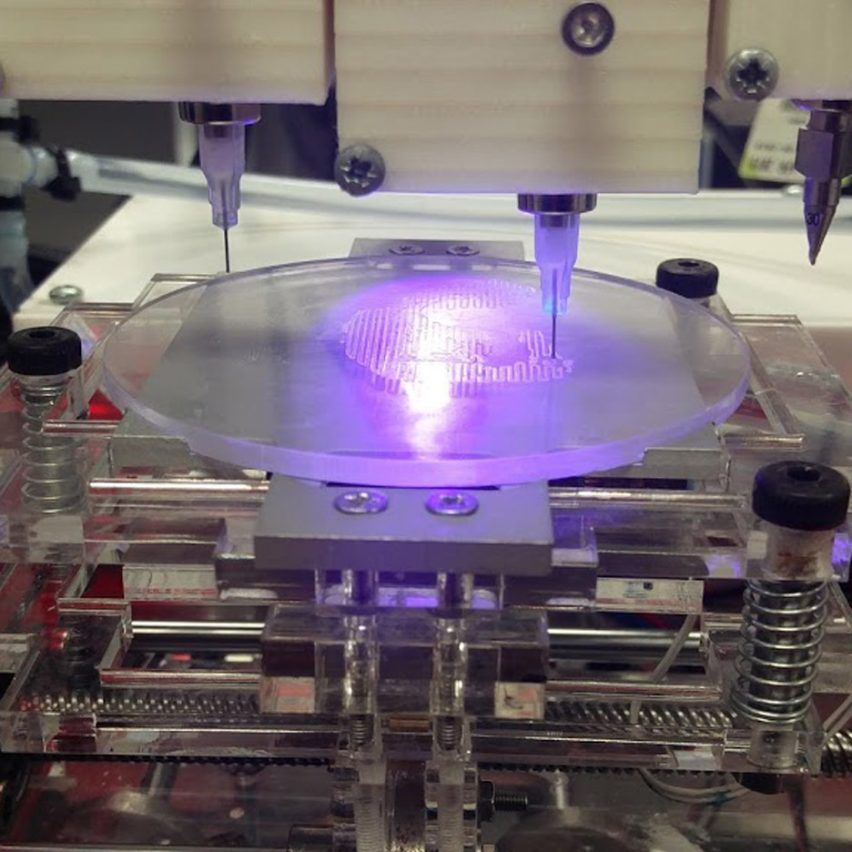
“A lot of these children experience psychological and social impacts from growing up without an outer ear,” said Dan Cohen, a co-founder and the CEO of 3DBio Therapeutics.
For microtia patients today, surgeons often carve into a child’s rib cage to shave off cartilage and then construct an ear.
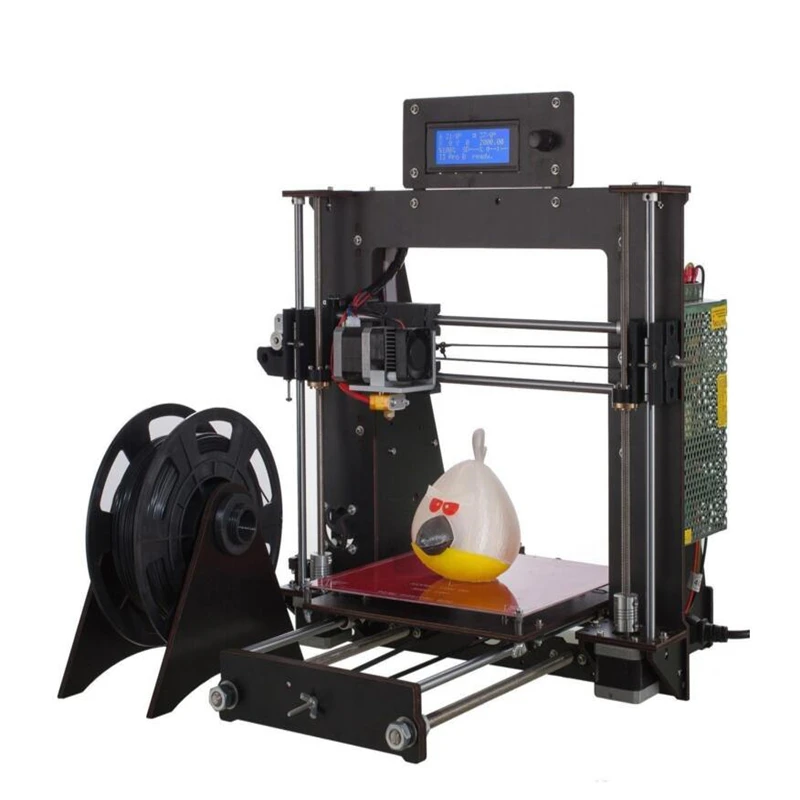
3D printing, in which a machine creates a three-dimensional object from raw materials, could reduce risks. The process is also used to create houses to recycled tools on the International Space Station.
To print an ear, 3DBio Therapeutics scientists first built a three-dimensional computer model, based on a scan of the woman’s other ear. Then, they cultured living cells and put them into a “bioink” made of collagen. A printer then deposited the bioink layer after layer to create the right shape — a mirror image of the woman’s ear. A final biodegradable shell shields the implant while it generates cartilage.
“In this case, you don’t have to go into the rib cage and expose the lungs to infection and have other surgical risks,” said Adetola Adesida, a professor in the department of surgery at the University of Alberta, who was not involved in the implant.
Implanting a printed ear is much the same procedure as typical, Cohen said. Dr. Arturo Bonilla, a San Antonio-based pediatric ear reconstructive surgeon specializing in microtia, performed the March surgery.
In a news release, Bonilla said he hoped 3D printing would become the new standard of care for microtia patients.
The implant was part of an ongoing clinical trial involving 11 patients.
Patient's ear before surgery, left, and patient's ear 30 days post surgery. Courtesy Dr. Arturo Bonilla / Congenital Ear InstituteThe company said it will share its clinical safety and efficacy data upon the trial’s completion. Without clinical trial data, the outside experts could not evaluate the methods used to construct the ear in detail. The outside experts who spoke with NBC News said the research appeared to be credible.
Feinberg said getting a green light from Food and Drug Administration regulators to pursue the research signals that the company has a reliable process.
The development of the ear could pave the way for more ambitious projects, Feinberg said.
“The ear is a relatively simple organ. It has some function. It does help funnel sound into the air,” Feinberg said. “We’re thinking of it mostly as a cosmetic outcome. The next step is to build more functional tissues or organs. It’s a much higher bar.”
3D printing technology could also help scientists scale regenerative medicine solutions that have been produced in laboratories but are not available broadly.
“3D printing is a really great tool to be able to automate the process,” Atala said. “It brings automation, reproducibility. It brings reliability. It brings decreased cost.”
Evan Bush
Evan Bush is a science reporter for NBC News. He can be reached at [email protected].
Printing organs: how ears, skin and noses are made with a 3D printer
- Natalka Pisnya
- BBC Russian Service, USA
it will help you sort things out.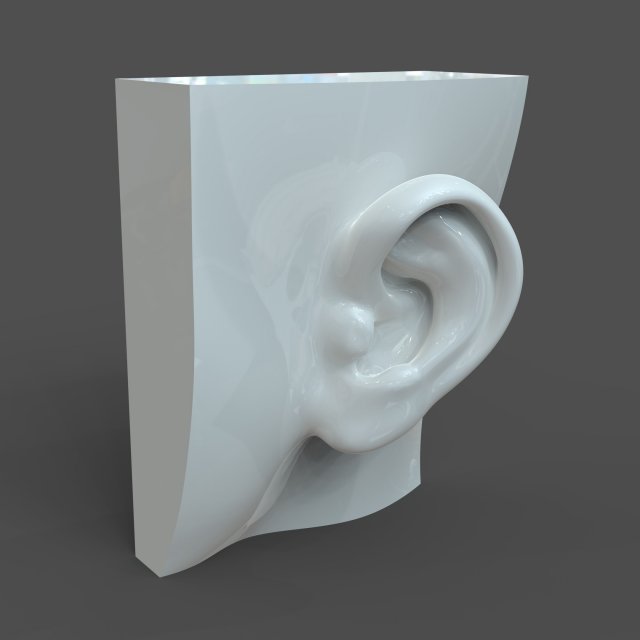
Image copyright, Masela family archive
Photo caption,Luc Masela with his parents one month after the artificial bladder transplant. year 2001.
Luc Masela, now 27, is an athlete with a degree in economics, works for a major exhibition company, travels a lot and recently met, in his words, "the most beautiful girl in the world." Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
Luke was born with spina bifida - and although he was able to walk, his bladder was severely damaged. By the age of 10, he almost did not leave hospitals: due to improper functioning of the bladder, fluid began to return to the boy's kidneys, doctors diagnosed an irreversible pathology of the organ.
You need JavaScript enabled or a different browser to view this content
Video caption,"3D printed" organs are here
Doctors offered the family two solutions: lifelong dialysis or the creation of a new bladder from a segment of the intestine. This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
The urologist in charge of the boy suggested that Masela's family take part in an experimental program to grow a new bladder from his own cells. Then, in 2001, it sounded like science fiction: only nine people took part in the program before Luke. Despite this, his family agreed.
"The essence of the operation was reduced to two stages: first, a piece of bladder tissue was taken from me, and over the next two months, cells were grown in the laboratory in order to grow a new healthy bladder from them," says Luke.
Photo copyright, Masela family archive
Photo caption,Luc Masela, 17 years after the artificial bladder transplant
Next was the transplant operation, which, according to him, lasted 16 hours. “I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
“I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
The operation was performed by Dr. Anthony Atala, Pediatric Regenerative Surgeon. In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like an ordinary organ, taking root thanks to Luke’s own cells.
- An animal capable of regrowing its head
- The birth of a chimera: why do scientists need a human-animal hybrid?
- Swedish company 3D prints body parts
Luke and Dr. Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.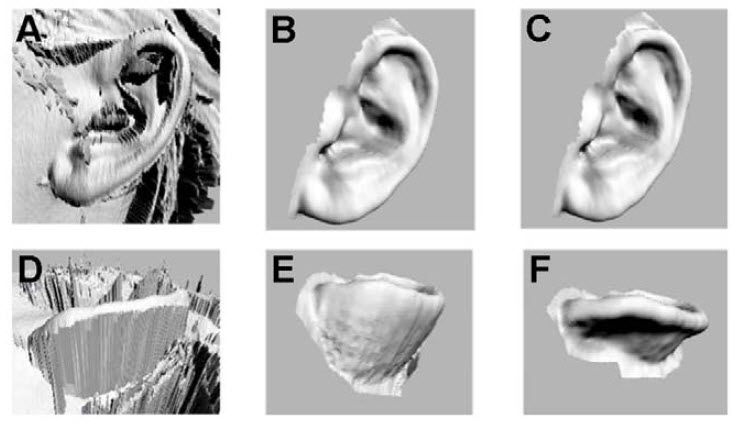
The professor took charge of the Wake Forest Institute of Regenerative Medicine in North Carolina in those 10 years, but Luke was never forgotten: his bladder was one of the most challenging and most successful projects in his early practice.
By 2018, Atala won the Christopher Columbus Award for "work on a discovery that will have a significant impact on society"; The Times and Scientific American magazines at various times named him "Physician of the Year", he was also recognized as "one of the 50 scientists on the planet who in the next 10 years will change the way we live and work."
How to print a new face
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
In the mid-2000s, Atala's team turned their attention to an ordinary household 3D printer and wrote special software for it, later specialized machines were created for the laboratory.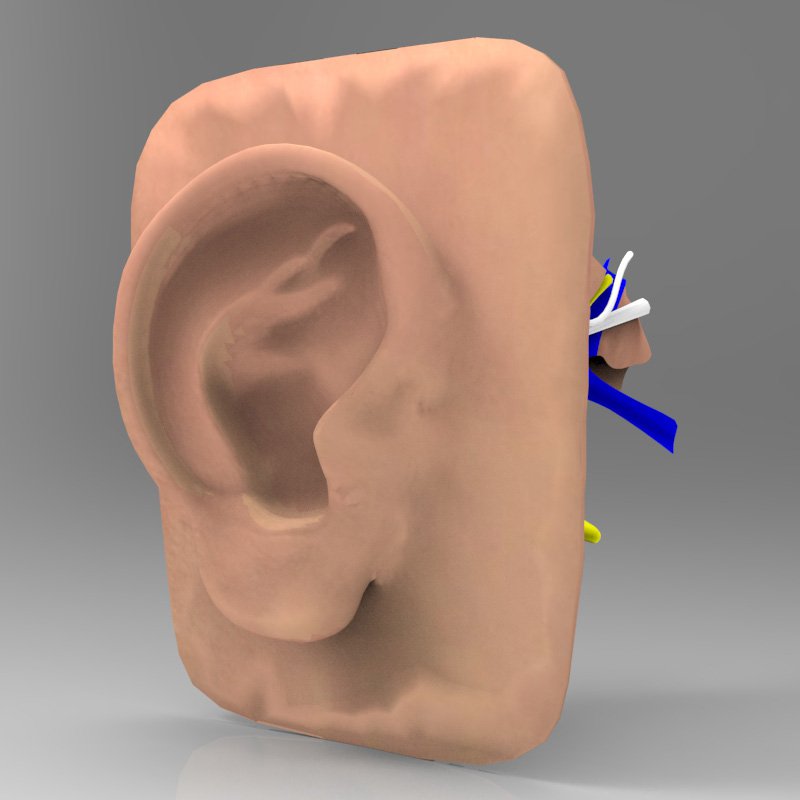 Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
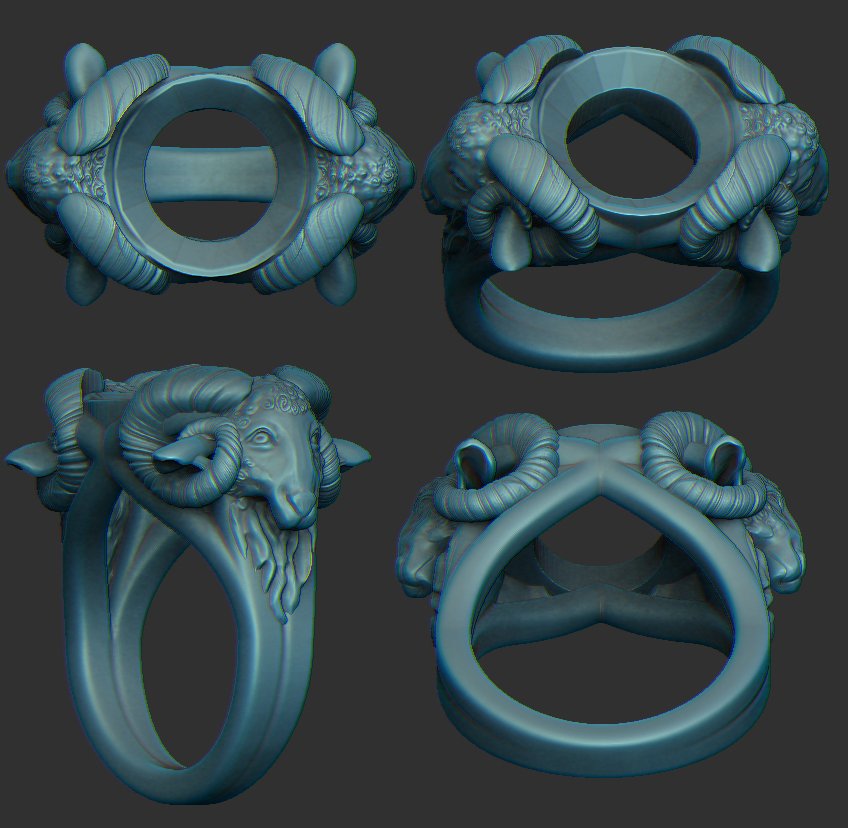
One of the team's latest achievements is ears and noses grown outside the human body.
The main customer and sponsor of Atala's developments is the US Department of Defense, and many of the patients are military victims of military operations.
It works like this: first, a CT scan of the ear or nose is done. One of Atala's assistants, Joshua Corpus, jokes that at this stage, people often ask to "improve" the shape of the nose if they thought theirs was too wide or hooked, and the ears if they were too wide.
After that, a special computer code is written, and the printing of the base of the organs begins.
For this, a bioabsorbable polymer, polycaprolactam, is used. At the same time flexible and durable, in the human body it disintegrates within four years.
After printing, the layers of polycaprolactam resemble lace; after transplantation, their place will be taken by a person's own cartilage tissue in a few years after transplantation.
Polycaprolactam is then saturated with a gel created from the patient's cells, cooled to -18 degrees Celsius - so the cells, according to scientists, are not damaged, they are "alive and happy."
Image caption,Printing a test kidney sample on a bioprinter
In order for the polymer and gel structure to take shape and become something more durable, ultraviolet light is used in the laboratory - it does not damage cells.
The future implant is printed for 4-5 hours, then it is finally formed and inserted under the epidermis.
Skin can also be grown: children affected by the fires were the first to participate in the early trials of Atala - after the "printing" of the skin, scientists observed the patients for several more years. The new skin did not crack, did not burst, and grew with the children.
The most difficult job, according to the scientist, is facial wounds: it’s not enough just to stretch the skin, you need to accurately calculate the geometry, align swelling, bone structure, and understand how a person will look after that.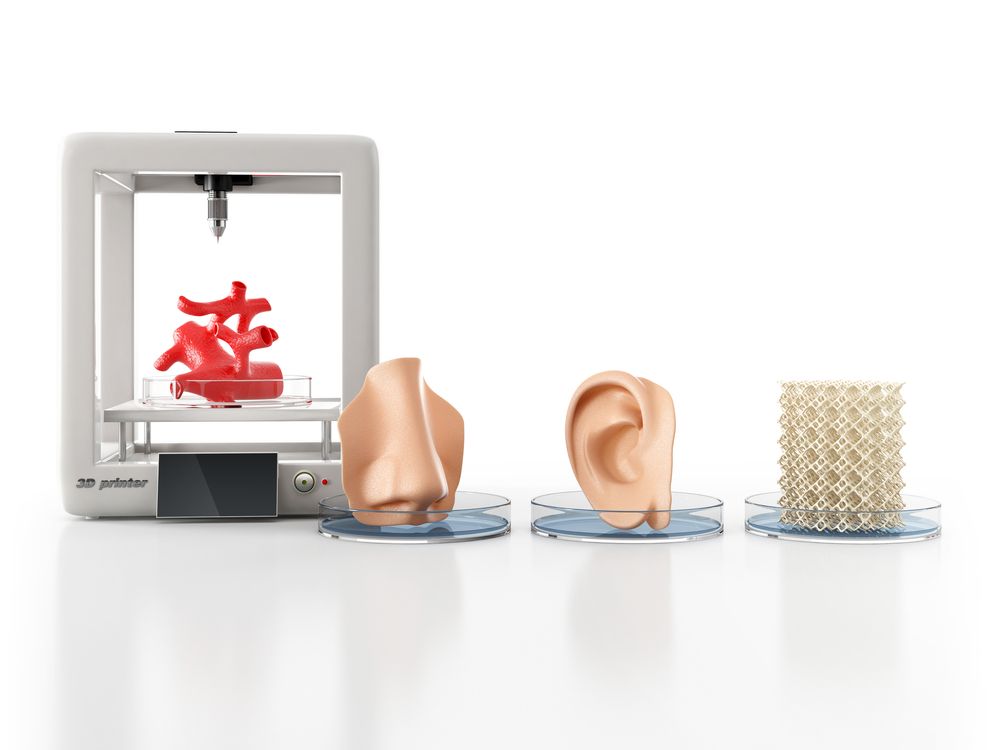
In addition to the skin and ears, Atala can "print" the bones of the jaws, grow blood vessels and cells of some organs - the liver, kidneys, lungs.
This technology is especially appreciated by oncologists: on the basis of patient cells, it is possible to recreate the body's response to various types of chemotherapy and observe the reaction to a particular type of treatment in the laboratory, and not on a living person.
But the liver, kidneys, lungs and heart are still being tested. Atala says he raised them in miniature, but creating organs from various tissues to real size requires a lot of additional research.
But, according to him, cells were grown in the laboratory and a vagina was created for a girl who was born several years ago with a congenital deformity of the genital organs - several years have passed since the transplant.
Image caption,Bioprinted polycaprolactam ear implant base
Atala smiles and adds that his team is also working on a working penis.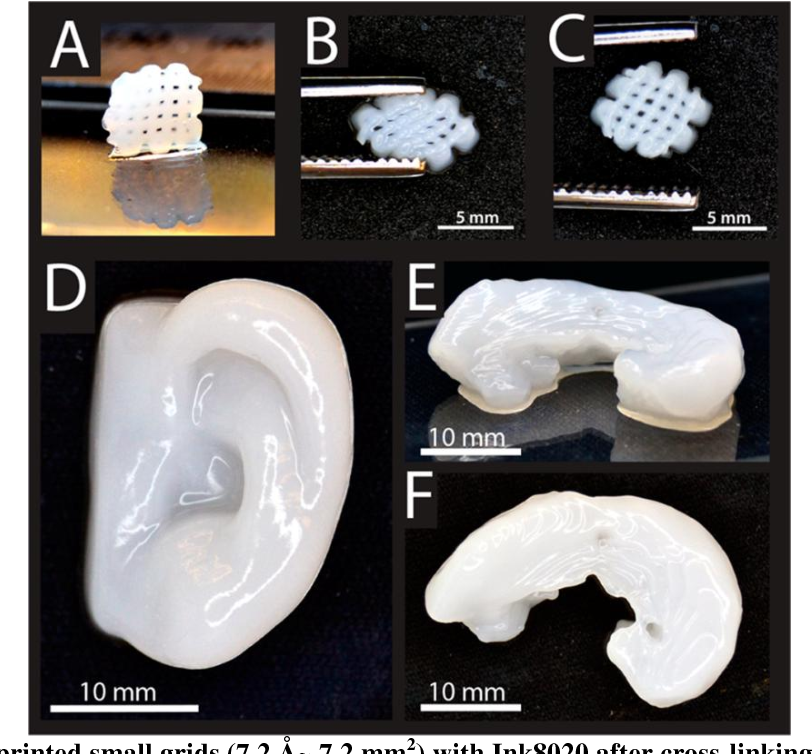 This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
Among others, Igor Vasyutin, a Russian post-graduate student of the First Moscow State Medical University (MGMU) named after Sechenov, is working on this under laboratory conditions. He is a cell biologist, Atala's right hand.
Vasyutin has been in the USA for about a year - he came on an exchange. He is ready to talk about the behavior of stem cells for hours, but becomes less verbose when it comes to Russian science.
Vasyutin's alma mater has not reached mass regeneration of human organs and is still training on animals: local scientists "printed" a mouse thyroid gland on a 3D printer.
However, they are also involved in the study of human organs. According to the head of the Institute of Regenerative Medicine at MSMU Denis Butnar, several years ago the Institute recreated a special engineering design of the buccal mucosa. She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
Test specimen of an ear implant exposed to ultraviolet light
In Russia, however, over the past few years, the Italian surgeon-transplantologist Paolo Macchiarini has been practicing - the man who was the first in history to perform an operation on transplanting a synthetic organ - a plastic tube that replaced the patient trachea.
- Paolo Macchiarini: the rise and fall of the famous surgeon
However, seven of his nine patients died, and the breathing tubes implanted in the remaining two subsequently had to be replaced with donor ones.
Several criminal cases were brought against him, including on charges of pressure on patients and fraud, and the world's leading doctors called Macchiarini's operations "ethical Chernobyl."
Will printed organs replace donors?
At the zenith of his career, Macchiarini argued that a new perspective is opening up for humanity: you can "print" any human organ on a printer, create an engineering structure from it, enriched with the patient's stem cells, and get the perfect prosthesis.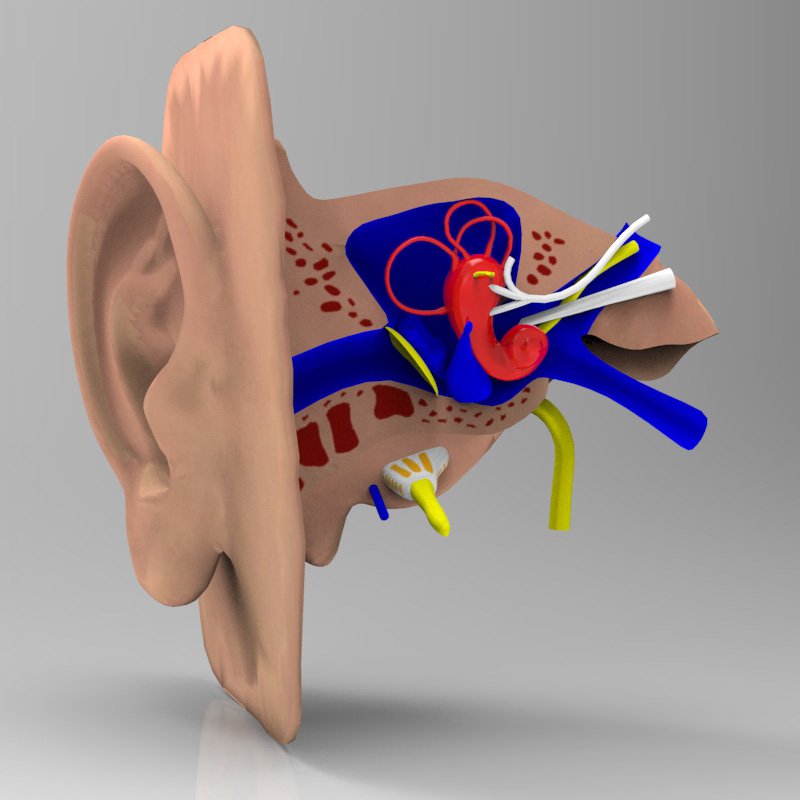
Be that as it may, complex human organs - the liver, kidneys, heart, lungs - have not yet been grown by any regenerative surgeon.
Bioprinting of the so-called simple organs, however, is already available in the USA, Sweden, Spain and Israel - at the level of clinical trials and special programs.
The US government is actively investing in such programs - in addition to Wake Forest, cooperating with the Pentagon, the Massachusetts Institute of Technology also receives significant amounts to recreate the functioning of the liver, heart and lungs.
Image caption,Skin application test on a burnt wound
According to Professor Jorge Raquela, a gastroenterologist at the Mayo Clinic Research Center, "Bioprinting is one of the most exciting branches of modern medicine, it has huge potential, and the turning point of the most important discoveries is already close."
Meanwhile, Pete Basillier, head of R&D at analytics firm Gartner, insists technology is advancing much faster than understanding the implications of 3D printing.
Such developments, according to Basilière, even if created with the best of intentions, give rise to a set of questions: what will happen when "improved" organs are created, the basis of which will not only be human cells - will they have "superpowers"? Will a regulatory body be created to monitor their production? Who will check the quality of these organs?
More than 150,000 Americans are on the waiting list for organ transplants every year, according to a report from the US National Library of Medicine. Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
- A 3D printer helped a cyclist who lost his jaw
- Genetically modified pigs - human organ donors?
- The world's first child who received both hands transplanted plays baseball
Most Americans are potential donors: upon obtaining a driver's license, they voluntarily answer the question of whether they agree to donate their organs in the event of a car accident or other dangerous incident . In case of consent, a small "heart" and the word "donor" appear in the corner of the document.
In case of consent, a small "heart" and the word "donor" appear in the corner of the document.
Professor Atala's driver's license is the same - despite all his achievements and faith in the press, he is ready to share his with others.
Neither the professor himself, nor his subordinates hide the fact that science is not yet able to "print" organs for thousands of those who need transplantation right now. According to him, it will take several decades to replace donor organs with grown ones at the mass market level.
The work of Atala and others in the field of regenerative medicine remains more probing than mainstream, and still tailored to the individual patient.
3D bioprinter prints ear through mouse skin
Scientists have created a 3D bioprinter that can print polymer molds with living cells through various tissues by polymerizing a biocompatible matrix using infrared light. The main advantage of such a printer is non-invasiveness: in order to print a polymer part, it is only necessary to introduce a blank solution into the right place. The technology is based on two-layer nanoinitiators - their inner part absorbs infrared light and emits ultraviolet light, and the outer layer starts polymerization under the action of ultraviolet light. To the authors of an article published in the journal Science Advances was able to print an ear-shaped structure under the skin of a living mouse and heal a closed wound with a stem cell patch.
The technology is based on two-layer nanoinitiators - their inner part absorbs infrared light and emits ultraviolet light, and the outer layer starts polymerization under the action of ultraviolet light. To the authors of an article published in the journal Science Advances was able to print an ear-shaped structure under the skin of a living mouse and heal a closed wound with a stem cell patch.
3D bioprinters print 3D structures from biocompatible materials with living cells, thus obtaining tissues and organs for transplantation. This technology has great potential in reconstructive surgery, but its use is limited by the need for invasive work on open tissues and injuries. To open access to internal injuries, it is necessary to damage the surrounding tissues, so non-invasive methods are preferred; they are also needed in plastic surgery.
Relatively non-invasive bioprinting is possible with photopolymerization, when a liquid material solidifies under the action of light. Ultraviolet and blue light is used to print tissues and organs, but radiation in this range does not penetrate deep into tissues. An alternative technology could be polymerization under the action of infrared light - it passes through living tissues and is already used for controlled release of drugs, 3D imaging and optogenetics.
Ultraviolet and blue light is used to print tissues and organs, but radiation in this range does not penetrate deep into tissues. An alternative technology could be polymerization under the action of infrared light - it passes through living tissues and is already used for controlled release of drugs, 3D imaging and optogenetics.
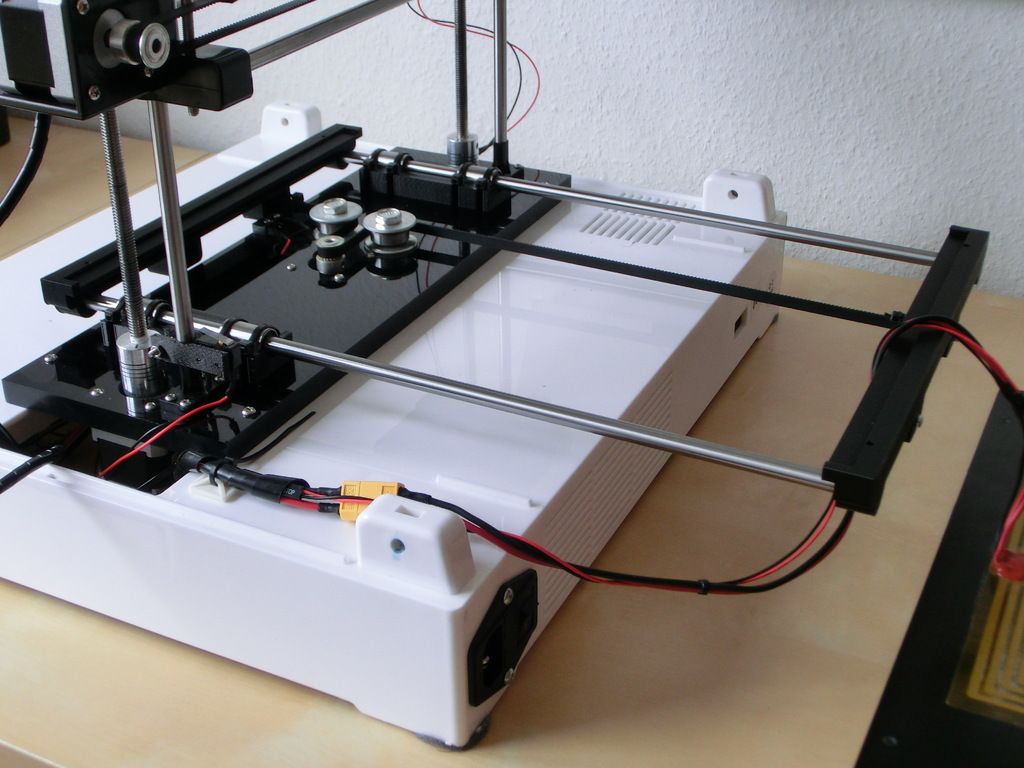
Scientists from Belgium, China and the United States under the leadership of Maling Gou of Sichuan University have created a 3D bioprinting technology based on near-infrared photopolymerization. A device with a system of micromirrors directs a laser beam through the skin and starts the polymerization of monomeric biocompatible ink at the desired point. The reaction nanoinitiators are assembled from two layers: the inner part of the particles absorbs infrared light and emits it in the ultraviolet range, and the outer layer consists of a photoinitiator that absorbs all the ultraviolet and polymerizes the monomers into a hydrogel.
To begin with, various hydrogel figures were printed using the system, including through the skin of a mouse or muscle tissue of a pig with a thickness of 0. 5 mm, and even in vivo through the skin of a live mouse. In the latter case, before printing, the animals were injected subcutaneously with a solution of monomers, and within a week after the procedure, the condition of the surrounding tissues was assessed.
5 mm, and even in vivo through the skin of a live mouse. In the latter case, before printing, the animals were injected subcutaneously with a solution of monomers, and within a week after the procedure, the condition of the surrounding tissues was assessed.
Both directly and through living tissues in vitro or in vivo was able to print figures of various shapes. Within a week, the hydrogel construct printed under the skin of a mouse did not cause damage or inflammation of the surrounding tissues.
The authors of the work suggested that the technology can be used to restore the auricle with its defects (congenital or resulting from trauma). An artificial human ear with living cells was printed in vitro , and then the technology was tested on mice. To reproduce the correct shape, a healthy copy of the ear was mirrored. Then, chondrocytes (cartilage cells) were added to the monomeric solution and it was polymerized through the skin in the shape of an ear. Cell viability was assessed seven days later by fluorescent staining of live chondrocytes, and then a structure of the same shape was printed under the skin of a live mouse.
Cell viability was assessed seven days later by fluorescent staining of live chondrocytes, and then a structure of the same shape was printed under the skin of a live mouse.
In culture inside the artificial ear, more than 80 percent of chondrocytes remained alive after seven days. In vivo , the subcutaneous hydrogel ear retained its shape for a month, while chondrocytes survived in polymer lacunae and secreted collagen.
Finally, 3D bioprinting has been used to heal closed injuries with soft tissue damage. To do this, a polymer skeleton was printed inside a closed wound of muscle tissue from a solution with adipose tissue stem cells. After 10 days, the scientists analyzed wound healing and muscle tissue formation in comparison with control animals, whose injuries were not treated in any way.
The wound, in which the appropriately shaped hydrogel patch with stem cells was printed, healed by 80 percent in 10 days, and only 40 percent in control animals (p < 0.