3D printing biological materials
Novel Biomaterials Used in Medical 3D Printing Techniques
1. Belhabib S., Guessasma S. Compression performance of hollow structures: From topology optimisation to design 3D printing. Int. J. Mech. Sci. 2017;133:728–739. doi: 10.1016/j.ijmecsci.2017.09.033. [CrossRef] [Google Scholar]
2. Guessasma S., Nouri H., Roger F. Microstructural and Mechanical Implications of Microscaled Assembly in Droplet-based Multi-Material Additive Manufacturing. Polymers. 2017;9:372. doi: 10.3390/polym9080372. [CrossRef] [Google Scholar]
3. Ligon S.C., Liska R., Stampfl J., Gurr M., Mülhaupt R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017;117:10212–10290. doi: 10.1021/acs.chemrev.7b00074. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Liu T., Guessasma S., Zhu J., Zhang W., Nouri H., Belhabib S. Microstructural defects induced by stereolithography and related compressive behaviour of polymers. J. Mater. Process. Technol. 2018;251:37–46. doi: 10.1016/j.jmatprotec.2017.08.014. [CrossRef] [Google Scholar]
5. Mandrycky C., Wang Z., Kim K., Kim D.H. 3D bioprinting for engineering complex tissues. Biotechnol. Adv. 2016;34:422–434. doi: 10.1016/j.biotechadv.2015.12.011. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Rezwan K., Chen Q.Z., Blaker J.J., Boccaccini A.R. Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials. 2006;27:3413–3431. doi: 10.1016/j.biomaterials.2006.01.039. [PubMed] [CrossRef] [Google Scholar]
7. Godbey W.T., Atala A. In vitro systems for tissue engineering. Ann. N. Y. Acad. Sci. 2002;961:10–26. doi: 10.1111/j.1749-6632.2002.tb03041.x. [PubMed] [CrossRef] [Google Scholar]
8. Dong L., Wang S.J., Zhao X.R., Zhu Y.F., Yu J.K. 3D-printed poly (ϵ-caprolactone) scaffold integrated with cell-laden chitosan hydrogels for bone tissue engineering. Sci. Rep. 2017;7:13412. doi: 10.1038/s41598-017-13838-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
9. Shim J.-H., Won J.-Y., Park J.-H., Bae J.-H., Ahn G., Kim C.-H., Lim D.-H., Cho D.-W., Yun W.-S., Bae E.-B., et al. Effects of 3D-Printed Polycaprolactone/β-Tricalcium Phosphate Membranes on Guided Bone Regeneration. Int. J. Mol. Sci. 2017;18:899. doi: 10.3390/ijms18050899. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Shim J.-H., Won J.-Y., Park J.-H., Bae J.-H., Ahn G., Kim C.-H., Lim D.-H., Cho D.-W., Yun W.-S., Bae E.-B., et al. Effects of 3D-Printed Polycaprolactone/β-Tricalcium Phosphate Membranes on Guided Bone Regeneration. Int. J. Mol. Sci. 2017;18:899. doi: 10.3390/ijms18050899. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Mills D., Tappa K., Jammalamadaka U., Weisman J., Woerner J. The Use of 3D Printing in the Fabrication of Nasal Stents. Inventions. 2017;3:1. doi: 10.3390/inventions3010001. [CrossRef] [Google Scholar]
11. Weisman J.A., Nicholson J.C., Tappa K., Jammalamadaka U., Wilson C.G., Mills D.K. Antibiotic and chemotherapeutic enhanced three-dimensional printer filaments and constructs for biomedical applications. Int. J. Nanomed. 2015;10:357–370. [PMC free article] [PubMed] [Google Scholar]
12. Tappa K., Jammalamadaka U., Ballard D.H., Bruno T., Israel M.R., Vemula H., Meacham J.M., Mills D.K., Woodard P.K., Weisman J.A. Medication eluting devices for the field of OBGYN (MEDOBGYN): 3D printed biodegradable hormone eluting constructs; a proof of concept study. PLoS ONE. 2017;12:e0182929. doi: 10.1371/journal.pone.0182929. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
PLoS ONE. 2017;12:e0182929. doi: 10.1371/journal.pone.0182929. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
13. Horst D.J., Tebcherani S.M., Kubaski E.T., De Almeida Vieira R. Bioactive Potential of 3D-Printed Oleo-Gum-Resin Disks: B. papyrifera; C. myrrha; and S. benzoin Loading Nanooxides—TiO2, P25, Cu2O; and MoO3. Bioinorg. Chem. Appl. 2017;2017:6398167. doi: 10.1155/2017/6398167. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Weisman J., Jammalamadaka U., Tappa K., Mills D. Doped Halloysite Nanotubes for Use in the 3D Printing of Medical Devices. Bioengineering. 2017;4:96. doi: 10.3390/bioengineering4040096. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Goyanes A., Det-Amornrat U., Wang J., Basit A.W., Gaisford S. 3D scanning and 3D printing as innovative technologies for fabricating personalized topical drug delivery systems. J. Control. Release. 2016;234:41–48. doi: 10. 1016/j.jconrel.2016.05.034. [PubMed] [CrossRef] [Google Scholar]
1016/j.jconrel.2016.05.034. [PubMed] [CrossRef] [Google Scholar]
16. Goyanes A., Wang J., Buanz A., Martínez-Pacheco R., Telford R., Gaisford S., Basit A.W. 3D Printing of Medicines: Engineering Novel Oral Devices with Unique Design and Drug Release Characteristics. Mol. Pharm. 2015;12:4077–4084. doi: 10.1021/acs.molpharmaceut.5b00510. [PubMed] [CrossRef] [Google Scholar]
17. Shen S., Wang H., Xue Y., Yuan L., Zhou X., Zhao Z., Dong E., Liu B., Liu W., Cromeens B., et al. Freeform fabrication of tissue-simulating phantom for potential use of surgical planning in conjoined twins separation surgery. Sci. Rep. 2017;7:11048. doi: 10.1038/s41598-017-08579-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Huang J.-J., Ren J.-A., Wang G.-F., Li Z.-A., Wu X.-W., Ren H.-J., Liu S. 3D-printed “fistula stent” designed for management of enterocutaneous fistula: An advanced strategy. World J. Gastroenterol. 2017;23:7489–7494. doi: 10.3748/wjg.v23.i41.7489. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
19. Almeida C.R., Serra T., Oliveira M.I., Planell J.A., Barbosa M.A., Navarro M. Impact of 3-D printed PLA- and chitosan-based scaffolds on human monocyte/macrophage responses: Unraveling the effect of 3-D structures on inflammation. Acta Biomater. 2014;10:613–622. doi: 10.1016/j.actbio.2013.10.035. [PubMed] [CrossRef] [Google Scholar]
Almeida C.R., Serra T., Oliveira M.I., Planell J.A., Barbosa M.A., Navarro M. Impact of 3-D printed PLA- and chitosan-based scaffolds on human monocyte/macrophage responses: Unraveling the effect of 3-D structures on inflammation. Acta Biomater. 2014;10:613–622. doi: 10.1016/j.actbio.2013.10.035. [PubMed] [CrossRef] [Google Scholar]
20. Rhee S., Puetzer J.L., Mason B.N., Reinhart-King C.A., Bonassar L.J. 3D Bioprinting of Spatially Heterogeneous Collagen Constructs for Cartilage Tissue Engineering. ACS Biomater. Sci. Eng. 2016;2:1800–1805. doi: 10.1021/acsbiomaterials.6b00288. [CrossRef] [Google Scholar]
21. Laronda M.M., Rutz A.L., Xiao S., Whelan K.A., Duncan F.E., Roth E.W., Woodruff T.K., Shah R.N. A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nat. Commun. 2017;8:15261. doi: 10.1038/ncomms15261. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Markstedt K., Mantas A., Tournier I., Martínez Ávila H. , Hägg D., Gatenholm P. 3D Bioprinting Human Chondrocytes with Nanocellulose–Alginate Bioink for Cartilage Tissue Engineering Applications. Biomacromolecules. 2015;16:1489–1496. doi: 10.1021/acs.biomac.5b00188. [PubMed] [CrossRef] [Google Scholar]
, Hägg D., Gatenholm P. 3D Bioprinting Human Chondrocytes with Nanocellulose–Alginate Bioink for Cartilage Tissue Engineering Applications. Biomacromolecules. 2015;16:1489–1496. doi: 10.1021/acs.biomac.5b00188. [PubMed] [CrossRef] [Google Scholar]
23. Nguyen D., Hägg D.A., Forsman A., Ekholm J., Nimkingratana P., Brantsing C., Kalogeropoulos T., Zaunz S., Concaro S., Brittberg M., et al. Cartilage Tissue Engineering by the 3D Bioprinting of iPS Cells in a Nanocellulose/Alginate Bioink. Sci. Rep. 2017;7:658. doi: 10.1038/s41598-017-00690-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Tan Z., Parisi C., Di Silvio L., Dini D., Forte A.E. Cryogenic 3D Printing of Super Soft Hydrogels. Sci. Rep. 2017;7:16293. doi: 10.1038/s41598-017-16668-9. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
25. Lee J.-S., Hong J.M., Jung J.W., Shim J.-H., Oh J.-H., Cho D.-W. 3D printing of composite tissue with complex shape applied to ear regeneration. Biofabrication. 2014;6:24103. doi: 10.1088/1758-5082/6/2/024103. [PubMed] [CrossRef] [Google Scholar]
2014;6:24103. doi: 10.1088/1758-5082/6/2/024103. [PubMed] [CrossRef] [Google Scholar]
26. Phillippi J.A., Miller E., Weiss L., Huard J., Waggoner A., Campbell P. Microenvironments Engineered by Inkjet Bioprinting Spatially Direct Adult Stem Cells Toward Muscle- and Bone-Like Subpopulations. Stem Cells. 2008;26:127–134. doi: 10.1634/stemcells.2007-0520. [PubMed] [CrossRef] [Google Scholar]
27. Duan B., Hockaday L.A., Kang K.H., Butcher J.T. 3D bioprinting of heterogeneous aortic valve conduits with alginate/gelatin hydrogels. J. Biomed. Mater. Res. A. 2013;101:1255–1264. doi: 10.1002/jbm.a.34420. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Fedorovich N.E., Alblas J., de Wijn J.R., Hennink W.E., Verbout A.J., Dhert W.J.A. Hydrogels as Extracellular Matrices for Skeletal Tissue Engineering: State-of-the-Art and Novel Application in Organ Printing. Tissue Eng. 2007;13:1905–1925. doi: 10.1089/ten.2006.0175. [PubMed] [CrossRef] [Google Scholar]
29. Hsieh F. -Y., Lin H.-H., Hsu S. 3D bioprinting of neural stem cell-laden thermoresponsive biodegradable polyurethane hydrogel and potential in central nervous system repair. Biomaterials. 2015;71:48–57. doi: 10.1016/j.biomaterials.2015.08.028. [PubMed] [CrossRef] [Google Scholar]
-Y., Lin H.-H., Hsu S. 3D bioprinting of neural stem cell-laden thermoresponsive biodegradable polyurethane hydrogel and potential in central nervous system repair. Biomaterials. 2015;71:48–57. doi: 10.1016/j.biomaterials.2015.08.028. [PubMed] [CrossRef] [Google Scholar]
30. Suntornnond R., An J., Chua C.K. Roles of support materials in 3D bioprinting. Int. J. Bioprint. 2017;3:83–89. doi: 10.18063/IJB.2017.01.006. [CrossRef] [Google Scholar]
31. Poldervaart M.T., Goversen B., de Ruijter M., Abbadessa A., Melchels F.P.W., Öner F.C., Dhert W.J.A., Vermonden T., Alblas J. 3D bioprinting of methacrylated hyaluronic acid (MeHA) hydrogel with intrinsic osteogenicity. PLoS ONE. 2017;12:e0177628. doi: 10.1371/journal.pone.0177628. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
32. Sa M.-W., Nguyen B.-N.B., Moriarty R.A., Kamalitdinov T., Fisher J.P., Kim J.Y. Fabrication and evaluation of 3D printed BCP scaffolds reinforced with ZrO2 for bone tissue applications.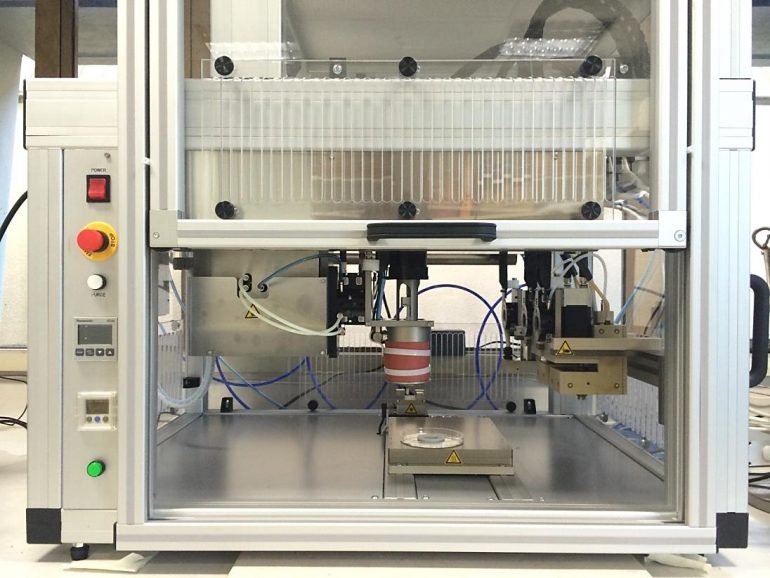 Biotechnol. Bioeng. 2017:1–11. doi: 10.1002/bit.26514. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Biotechnol. Bioeng. 2017:1–11. doi: 10.1002/bit.26514. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. Qi X., Pei P., Zhu M., Du X., Xin C., Zhao S., Li X., Zhu Y. Three dimensional printing of calcium sulfate and mesoporous bioactive glass scaffolds for improving bone regeneration in vitro and in vivo. Sci. Rep. 2017;7:42556. doi: 10.1038/srep42556. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
34. Sun M., Liu A., Shao H., Yang X., Ma C., Yan S., Liu Y., He Y., Gou Z. Systematical Evaluation of Mechanically Strong 3D Printed Diluted magnesium Doping Wollastonite Scaffolds on Osteogenic Capacity in Rabbit Calvarial Defects. Sci. Rep. 2016;6:34029. doi: 10.1038/srep34029. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Wang Y., Wang K., Li X., Wei Q., Chai W., Wang S., Che Y., Lu T., Zhang B. 3D fabrication and characterization of phosphoric acid scaffold with a HA/β-TCP weight ratio of 60:40 for bone tissue engineering applications. PLoS ONE. 2017;12:e0174870. doi: 10.1371/journal.pone.0174870. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2017;12:e0174870. doi: 10.1371/journal.pone.0174870. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
36. Sandler N., Määttänen A., Ihalainen P., Kronberg L., Meierjohann A., Viitala T., Peltonen J. Inkjet printing of drug substances and use of porous substrates-towards individualized dosing. J. Pharm. Sci. 2011;100:3386–3395. doi: 10.1002/jps.22526. [PubMed] [CrossRef] [Google Scholar]
37. Uddin M.J., Scoutaris N., Klepetsanis P., Chowdhry B., Prausnitz M.R., Douroumis D. Inkjet printing of transdermal microneedles for the delivery of anticancer agents. Int. J. Pharm. 2015;494:593–602. doi: 10.1016/j.ijpharm.2015.01.038. [PubMed] [CrossRef] [Google Scholar]
38. Strobel L.A., Rath S.N., Maier A.K., Beier J.P., Arkudas A., Greil P., Horch R.E., Kneser U. Induction of bone formation in biphasic calcium phosphate scaffolds by bone morphogenetic protein-2 and primary osteoblasts. J. Tissue Eng. Regen. Med. 2014;8:176–185. doi: 10.1002/term.1511. [PubMed] [CrossRef] [Google Scholar]
39. Inzana J.A., Trombetta R.P., Schwarz E.M., Kates S.L., Awad H.A. 3D printed bioceramics for dual antibiotic delivery to treat implant-associated bone infection. Eur. Cells Mater. 2015;30:232–247. doi: 10.22203/eCM.v030a16. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Inzana J.A., Trombetta R.P., Schwarz E.M., Kates S.L., Awad H.A. 3D printed bioceramics for dual antibiotic delivery to treat implant-associated bone infection. Eur. Cells Mater. 2015;30:232–247. doi: 10.22203/eCM.v030a16. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Boehm R.D., Miller P.R., Daniels J., Stafslien S., Narayan R.J. Inkjet printing for pharmaceutical applications. Mater. Today. 2014;17:247–252. doi: 10.1016/j.mattod.2014.04.027. [CrossRef] [Google Scholar]
41. Asadi-Eydivand M., Solati-Hashjin M., Shafiei S.S., Mohammadi S., Hafezi M., Osman N.A.A. Structure; properties; and in vitro behavior of heat-treated calcium sulfate scaffolds fabricated by 3D printing. PLoS ONE. 2016;11:e0151216. doi: 10.1371/journal.pone.0151216. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Inzana J.A., Olvera D., Fuller S.M., Kelly J.P., Graeve O.A., Schwarz E.M., Kates S.L., Awad H.A. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials. 2014;35:4026–4034. doi: 10.1016/j.biomaterials.2014.01.064. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Biomaterials. 2014;35:4026–4034. doi: 10.1016/j.biomaterials.2014.01.064. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
43. Farzadi A., Solati-Hashjin M., Asadi-Eydivand M., Osman N.A.A. Effect of layer thickness and printing orientation on mechanical properties and dimensional accuracy of 3D printed porous samples for bone tissue engineering. PLoS ONE. 2014;9:e108252. doi: 10.1371/journal.pone.0108252. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. Wickström H., Hilgert E., Nyman J., Desai D., Şen Karaman D., de Beer T., Sandler N., Rosenholm J. Inkjet Printing of Drug-Loaded Mesoporous Silica Nanoparticles—A Platform for Drug Development. Molecules. 2017;22:2020. doi: 10.3390/molecules22112020. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
45. Meess K.M., Izzo R.L., Dryjski M.L., Curl R.E., Harris L.M., Springer M., Siddiqui A.H., Rudin S., Ionita C.N. 3D Printed Abdominal Aortic Aneurysm Phantom for Image Guided Surgical Planning with a Patient Specific Fenestrated Endovascular Graft System. Proc. SPIE Int. Soc. Opt. Eng. 2017;10138:101380P. [PMC free article] [PubMed] [Google Scholar]
Proc. SPIE Int. Soc. Opt. Eng. 2017;10138:101380P. [PMC free article] [PubMed] [Google Scholar]
46. Kuroda S., Kobayashi T., Ohdan H. 3D printing model of the intrahepatic vessels for navigation during anatomical resection of hepatocellular carcinoma. Int. J. Surg. Case Rep. 2017;41:219–222. doi: 10.1016/j.ijscr.2017.10.015. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Li B., Wei H., Zeng F., Li J., Xia J.J., Wang X. Application of A Novel Three-dimensional Printing Genioplasty Template System and Its Clinical Validation: A Control Study. Sci. Rep. 2017;7:5431. doi: 10.1038/s41598-017-05417-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
48. Gear J.I., Cummings C., Craig A.J., Divoli A., Long C.D.C., Tapner M., Flux G.D. Abdo-Man: A 3D-printed anthropomorphic phantom for validating quantitative SIRT. EJNMMI Phys. 2016;3:17. doi: 10.1186/s40658-016-0151-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
49. Zein N.N., Hanouneh I. A., Bishop P.D., Samaan M., Eghtesad B., Quintini C., Miller C., Yerian L., Klatte R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transplant. 2013;19:1304–1310. doi: 10.1002/lt.23729. [PubMed] [CrossRef] [Google Scholar]
A., Bishop P.D., Samaan M., Eghtesad B., Quintini C., Miller C., Yerian L., Klatte R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transplant. 2013;19:1304–1310. doi: 10.1002/lt.23729. [PubMed] [CrossRef] [Google Scholar]
50. Waran V., Narayanan V., Karuppiah R., Owen S.L.F., Aziz T. Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons. J. Neurosurg. 2014;120:489–492. doi: 10.3171/2013.11.JNS131066. [PubMed] [CrossRef] [Google Scholar]
51. Mitsouras D., Lee T.C., Liacouras P., Ionita C.N., Pietilla T., Maier S.E., Mulkern R.V. Three-dimensional printing of MRI-visible phantoms and MR image-guided therapy simulation. Magn. Reson. Med. 2017;77:613–622. doi: 10.1002/mrm.26136. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
52. Lan Q., Chen A., Zhang T., Li G., Zhu Q., Fan X., Ma C., Xu T. Development of Three-Dimensional Printed Craniocerebral Models for Simulated Neurosurgery. World Neurosurg. 2016;91:434–442. doi: 10.1016/j.wneu.2016.04.069. [PubMed] [CrossRef] [Google Scholar]
World Neurosurg. 2016;91:434–442. doi: 10.1016/j.wneu.2016.04.069. [PubMed] [CrossRef] [Google Scholar]
53. Sander I., Liepert T., Doney E., Leevy W., Liepert D. Patient Education for Endoscopic Sinus Surgery: Preliminary Experience Using 3D-Printed Clinical Imaging Data. J. Funct. Biomater. 2017;8:13. doi: 10.3390/jfb8020013. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
54. Dwivedi D.K., Chatzinoff Y., Zhang Y., Yuan Q., Fulkerson M., Chopra R., Brugarolas J., Cadeddu J.A., Kapur P., Pedrosa I. Development of a Patient-specific Tumor Mold Using Magnetic Resonance Imaging and 3-Dimensional Printing Technology for Targeted Tissue Procurement and Radiomics Analysis of Renal Masses. Urology. 2017 doi: 10.1016/j.urology.2017.08.056. in press. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
55. Miller J.S., Stevens K.R., Yang M.T., Baker B.M., Nguyen D.-H.T., Cohen D.M., Toro E., Chen A.A., Galie P.A., Yu X., et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat. Mater. 2012;11:768–774. doi: 10.1038/nmat3357. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Nat. Mater. 2012;11:768–774. doi: 10.1038/nmat3357. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
56. Kolesky D.B., Truby R.L., Gladman A.S., Busbee T.A., Homan K.A., Lewis J.A. 3D bioprinting of vascularized; heterogeneous cell-laden tissue constructs. Adv. Mater. 2014;26:3124–3130. doi: 10.1002/adma.201305506. [PubMed] [CrossRef] [Google Scholar]
57. Hinton T.J., Jallerat Q., Palchesko R.N., Park J.H., Grodzicki M.S., Shue H.-J., Ramadan M.H., Hudson A.R., Feinberg A.W. Three-dimensional printing of complex biological structures by freeform reversible embedding of suspended hydrogels. Sci. Adv. 2015;1:e1500758. doi: 10.1126/sciadv.1500758. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
58. Hassana B.O., Guessasma S., Belhabib S., Nouri H. Explaining the Difference between Real Part and Virtual Design of 3D Printed Porous Polymer at the Microstructural Level. Macromol. Mater. Eng. 2016;301:566–576. doi: 10.1002/mame.201500360. [CrossRef] [Google Scholar]
59. Ventola C.L. Medical Applications for 3D Printing: Current and Projected Uses. Pharm. Ther. 2014;39:704–711. [PMC free article] [PubMed] [Google Scholar]
Ventola C.L. Medical Applications for 3D Printing: Current and Projected Uses. Pharm. Ther. 2014;39:704–711. [PMC free article] [PubMed] [Google Scholar]
3D Printing of Biomaterials - Carpmaels & Ransford
Following our article on the role and challenges for the IP system in the world of 3D printing (or additive manufacturing), we are now going to focus on the specific field of 3D bioprinting. While many of the fundamental principles of conventional 3D printing apply to 3D bioprinting, such as the use of a CAD file to provide information to the 3D printer that forms the articles, due to the materials used and their potential applications, an additional set of issues must now be considered.
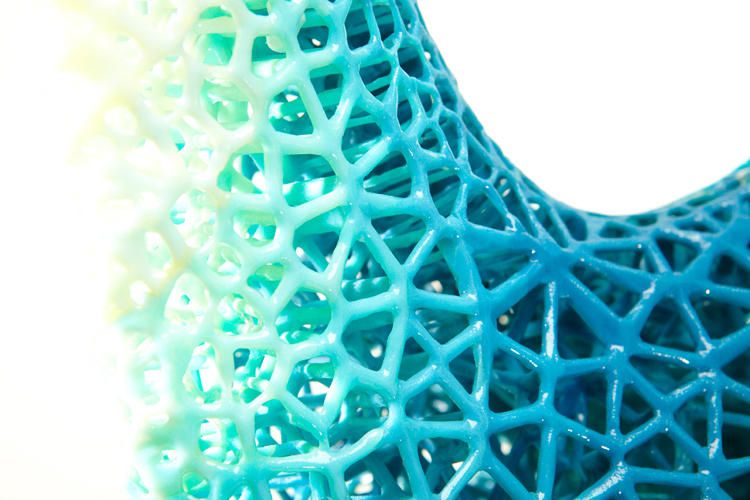
Bioprinting falls within an emerging yet significant application of 3D printing in the field of MedTech, encompassing aspects of biomaterials as well as medical devices. While 3D printing has solidified its place in the production of prostheses and biomedical devices, more recent developments have identified materials that, upon printing, afford tissue-like structures that can mimic natural products.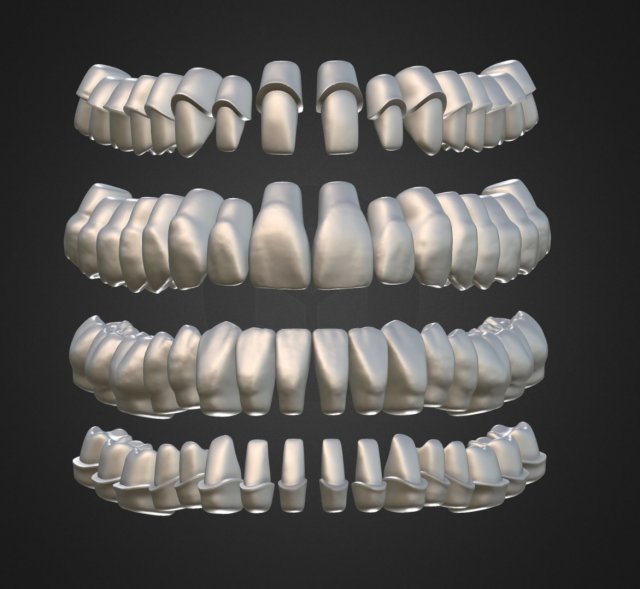 These new “bioinks” can be used to make functional organs and tissue structures and may include tissues, cells and other biomolecules (e.g., growth factors) that are printed to create scaffold-free cell-based structures. Bioinks can also include biocompatible materials that, upon printing, form scaffold-like structures within which the cells propagate. These biocompatible materials include hydrogels having specific properties that allow them to be extruded at temperatures required for maintaining living cells while undergoing gelation during printing to form the scaffold.
These new “bioinks” can be used to make functional organs and tissue structures and may include tissues, cells and other biomolecules (e.g., growth factors) that are printed to create scaffold-free cell-based structures. Bioinks can also include biocompatible materials that, upon printing, form scaffold-like structures within which the cells propagate. These biocompatible materials include hydrogels having specific properties that allow them to be extruded at temperatures required for maintaining living cells while undergoing gelation during printing to form the scaffold.
The use of 3D bioprinting to produce biodegradable structures and implantable medical devices has the potential to reduce the costs and improve the treatment options available for a range of medical conditions. Examples of applications include skin grafts for the treatment of burns, as well as synthetic tissues for use in in vitro drug testing[1]. One goal would be to 3D print entire organs suitable for implantation[2].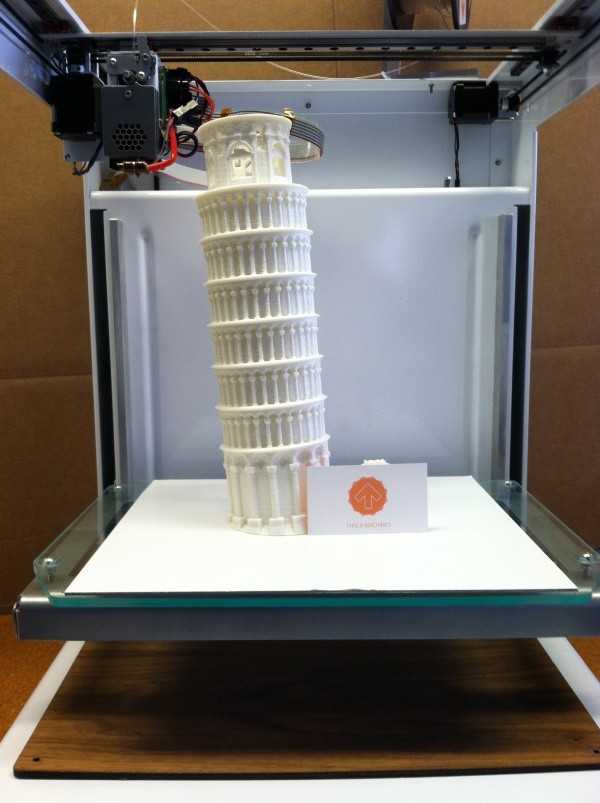
With any new technology, there is a need for robust IP protection to provide security and encourage investment. Patents are an obvious choice in this instance, as they can provide protection for the “bioink” compositions, the processes and equipment used in printing itself, as well as the end products (or products obtained by the specific 3D bioprinting process, protected using so-called “product-by-process” claims). Reflecting the development in this field is the increasing number of filed and granted patent applications, as shown in Figures 1 and 2. With the number of applications increasing consistently since 2015, we might expect this trend to continue into the next decade. Companies filing in this area include Sichuan Revotek Co. Ltd, BICO (of whom CELLINK are a subsidiary), T&R Biofab, Medtronic, 3D Systems, Inc., and Ricoh Company.
Fig. 1. 3D printed biomaterial PCT, and EP applications filed by yearFig. 2. 3D printed biomaterial granted EP patents by yearWhile these technologies present myriad opportunities, they can also present challenges for the IP system, both in terms of how to effectively protect new inventions (via patents, designs, copyright etc. ), and how to enforce the rights against third parties. General challenges relating to enforcement of IP rights in 3D printing technology have been previously discussed in our related article. In addition to these general issues, inventions relating to 3D bioprinting present several specific challenges.
), and how to enforce the rights against third parties. General challenges relating to enforcement of IP rights in 3D printing technology have been previously discussed in our related article. In addition to these general issues, inventions relating to 3D bioprinting present several specific challenges.
Bioinks and 3D Printed Biological Tissue
Exciting scientific developments have been taking place in the field of materials science, particularly with regard to biomaterials for medical devices and their application in 3D printing. Biologically active inks can be used to control and direct cell behaviour, and can therefore be used in the manufacture of complex tissue structures for regenerative medicine. Claims directed to bioinks, and the resulting 3D printed tissue structures, must satisfy the standard patentability criteria of novelty, inventive step, and being capable of industrial application. Although many bioink components, particularly biocompatible scaffold-forming materials, are known in the art, innovation may lie in the combination of these well-known components with living cells.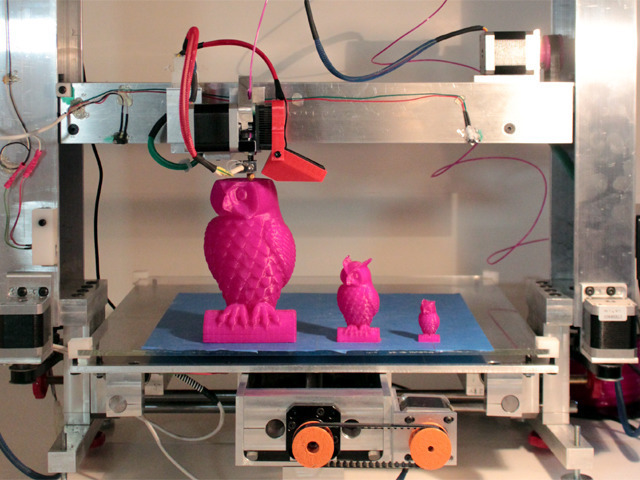 Composition claims can therefore be crafted so as to satisfy the requirements of patentability. For example, a particular combination of hydrogels may provide unexpected improvements in a cell-containing composition, such as a reduction in shear force experienced by cells during printing, the provision of nutrients to cells post-printing, or the enhancement of the mechanical properties of the resulting tissue.
Composition claims can therefore be crafted so as to satisfy the requirements of patentability. For example, a particular combination of hydrogels may provide unexpected improvements in a cell-containing composition, such as a reduction in shear force experienced by cells during printing, the provision of nutrients to cells post-printing, or the enhancement of the mechanical properties of the resulting tissue.
Moreover, while 3D printed bone implants have been around for some time, challenges exist in implementing the technology for soft tissues, for example in vascularisation and innervation of the biological tissue. Companies are continuing to advance in this area with 3D bioprinting being developed for use in human organ printing[3]. The bioinks in this case may include living cells or tissue in addition to the scaffold-forming materials, or as a standalone composition. As the technology emerges, it may be necessary to consider whether and to what extent it is possible to protect these natural materials, particularly if it becomes possible to 3D print bioinks comprising cells and natural materials alone. Cell-based bioinks and the resulting 3D bioprinted tissue structures would likely qualify as patentable subject-matter at the EPO; materials found in nature are, at least in principle, patentable under Article 5(2) of the Biotech Directive (incorporated into Rule 29(2) EPC), which confirms that “an element isolated from the human body or otherwise produced by means of a technical process, including the sequence or partial sequence of a gene, may constitute a patentable invention, even if the structure of that element is identical to that of a natural element.” It is notable that the approach in Europe is more patentee-friendly than in the US, where human organisms and products of nature are typically ineligible for patent protection.
Cell-based bioinks and the resulting 3D bioprinted tissue structures would likely qualify as patentable subject-matter at the EPO; materials found in nature are, at least in principle, patentable under Article 5(2) of the Biotech Directive (incorporated into Rule 29(2) EPC), which confirms that “an element isolated from the human body or otherwise produced by means of a technical process, including the sequence or partial sequence of a gene, may constitute a patentable invention, even if the structure of that element is identical to that of a natural element.” It is notable that the approach in Europe is more patentee-friendly than in the US, where human organisms and products of nature are typically ineligible for patent protection.
Of particular importance in the field of soft-tissue engineering are stem cells, due to their ability to differentiate into the desired cell type. 3D bioprinting processes can be used to control the outcome of stem cell differentiation[4]. The protection of bioinks comprising stem cells would need further consideration, since in Europe, Article 53(a) EPC and Rule 28(1)(c) EPC prohibit claims to the use of human embryos (and thus human embryonic stem cells (hESCs)) for industrial or commercial purposes under grounds of morality. However, the EPO Guidelines for Examination allow protection for certain types of hESCs, such as those derived from parthenogenetically activated human oocytes.
However, the EPO Guidelines for Examination allow protection for certain types of hESCs, such as those derived from parthenogenetically activated human oocytes.
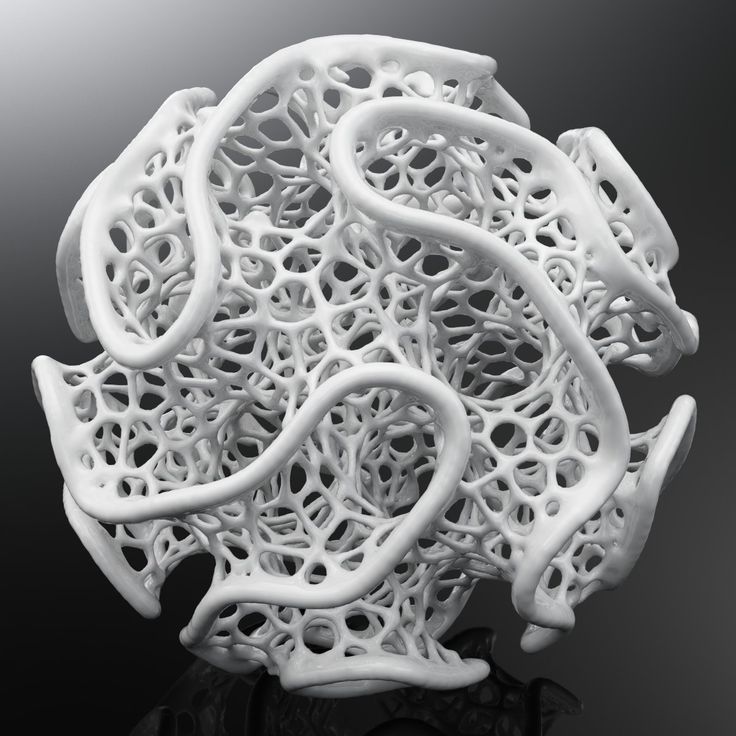
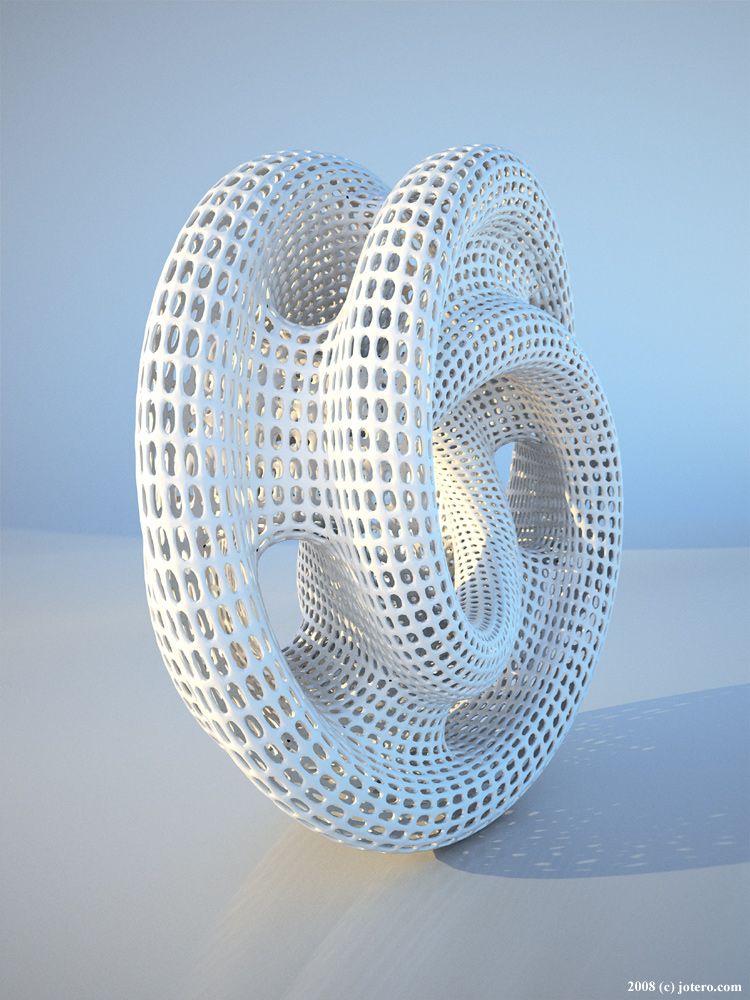
Given the technological developments needed to support the advancement of 3D bioprinting, protection for the scaffolds, implants or full-scale organs “obtained by” 3D printing (product-by-process claims) as well as for the products per se is conceivable. Regardless of whether a product or product-by-process claim is utilised, the products themselves must be novel. 3D bioprinting may give rise to structures with controlled porosity, permeability, or mechanical properties, as well as bespoke arrangements of cells and scaffold materials, or highly mature biological functions, such that structural and/or functional features may be used to distinguish over, e.g., natural tissues or organs.
Medical Use Claims
It is entirely feasible that the innovation of a bioink or a 3D bioprinted article lies in its medical use, that is, it provides a therapeutic effect. Protecting known bioinks or 3D printed biomaterials may therefore be achieved via Article 54(5) EPC, which states that claims to the use of a known “substance or composition” may be patentable provided that the use is not known in the art. However, this raises the question of whether the bioink or printed material would be considered a “substance or composition”.
Protecting known bioinks or 3D printed biomaterials may therefore be achieved via Article 54(5) EPC, which states that claims to the use of a known “substance or composition” may be patentable provided that the use is not known in the art. However, this raises the question of whether the bioink or printed material would be considered a “substance or composition”.
Under the EPO’s Guidelines for Examination, a material qualifies under this provision provided that it is the active agent or ingredient in a specific medical use and if the therapeutic effect can be ascribed to its chemical properties. In practice, this means that 3D printed materials which aid in the regeneration of tissues by virtue merely of its porous or permeable structure, for example, would be considered a device rather than a substance or composition, and thus not covered by the provisions of Article 54(5) EPC. In contrast, if a 3D printed material produces a regenerative effect on tissue that could be attributed to its chemical properties (e. g., biomolecules, chemical entities, etc.), it would be considered as a “substance or composition” in the sense of Article 54(5) EPC. The wide range of applicable materials that could be used in 3D bioprinting gives rise to a high degree of flexibility and versatility in producing therapeutic products, which should not be overlooked when seeking to obtain patent protection.
g., biomolecules, chemical entities, etc.), it would be considered as a “substance or composition” in the sense of Article 54(5) EPC. The wide range of applicable materials that could be used in 3D bioprinting gives rise to a high degree of flexibility and versatility in producing therapeutic products, which should not be overlooked when seeking to obtain patent protection.
3D Bioprinting Methods
Claims to conventional 3D printing processes, for example, to the 3D printing of a new prosthesis, will rarely be excluded from patentability under the EPC. However, as companies continue to advance this technology, particularly in the field of organ-level regenerative medicine, it can be envisaged that in situ bioprinting will evolve. These systems eliminate the artificial environment need for printing, e.g., in a sterile lab setting using a bioreactor, such that the human body behaves as the bioreactor. Moreover, in situ bioprinting could overcome problems associated with 3D bioprinting using bioreactors, including reducing the risk of contamination or breakage that can occur when handling and implanting the products.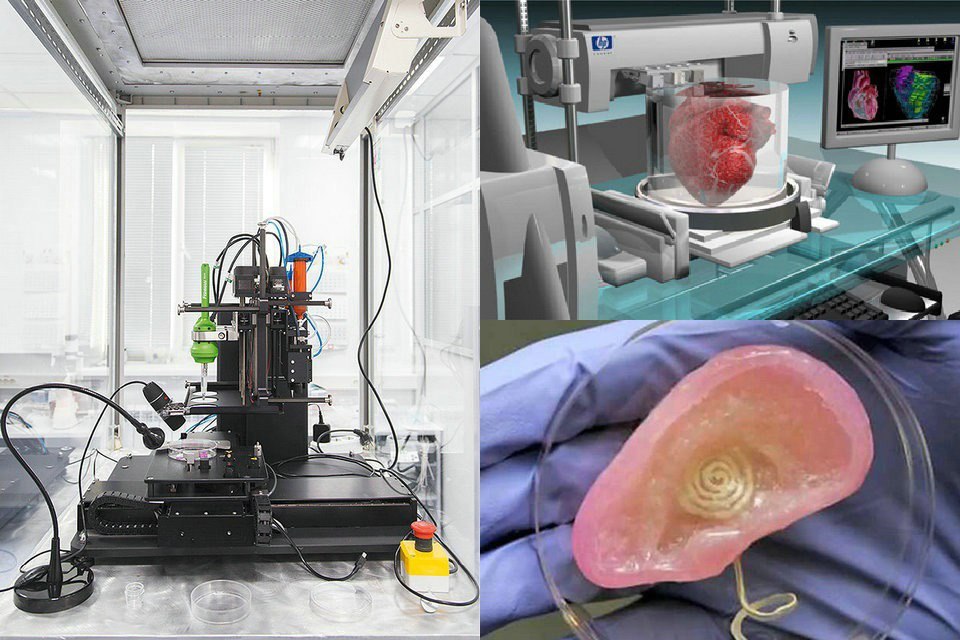 Several different approaches to in situ bioprinting have already been developed and patent applications are starting to be filed. While claims to new equipment and/or bioinks used in in situ bioprinting would be eligible for patentability, applicants should be aware of the potential exclusions that may apply in this setting, in particular, Article 53(c) EPC which prohibits claims to methods of treatment of the human or animal body by surgery or therapy. Thus, while a claim to a method of 3D bioprinting a skin graft may be patentable, skin regeneration which takes place directly onto a patient may fall foul of this exclusion.
Several different approaches to in situ bioprinting have already been developed and patent applications are starting to be filed. While claims to new equipment and/or bioinks used in in situ bioprinting would be eligible for patentability, applicants should be aware of the potential exclusions that may apply in this setting, in particular, Article 53(c) EPC which prohibits claims to methods of treatment of the human or animal body by surgery or therapy. Thus, while a claim to a method of 3D bioprinting a skin graft may be patentable, skin regeneration which takes place directly onto a patient may fall foul of this exclusion.
Applicants should consider the EPO’s criteria for assessing Article 53(c), wherein a method is excluded if, when carried out, “maintaining the life and health of the subject is important and which comprises and encompasses an invasive step representing a substantial physical intervention on the body which requires medical expertise to be carried out and which entails a substantial health risk even when carried out with required professional care and expertise” (G1/07). Whether or not a claim to an in situ bioprinting method is excluded under these provisions will typically be assessed on a case-by-case basis, taking into account the relative risk to the patient and the necessity for a surgeon to perform the procedure. Relevant EPO Case Law in this regard held that a process involving the removal and subsequent return of blood to patient was excluded under Article 53(c) EPC,[5] as it required “professional medical expertise”.
Whether or not a claim to an in situ bioprinting method is excluded under these provisions will typically be assessed on a case-by-case basis, taking into account the relative risk to the patient and the necessity for a surgeon to perform the procedure. Relevant EPO Case Law in this regard held that a process involving the removal and subsequent return of blood to patient was excluded under Article 53(c) EPC,[5] as it required “professional medical expertise”.
Accordingly, while in situ bioprinting has the potential to play a key role in organ formation and regeneration, careful consideration should be given when drafting to cover related methods where the manufacture takes place in the human body. Claims may need to be adapted to focus on, e.g., the method of operating the device or the device itself, as well as any specific bioinks that are used in such processes.
Summary
3D bioprinting is an emerging field with great potential for improving the treatment options for a range of conditions.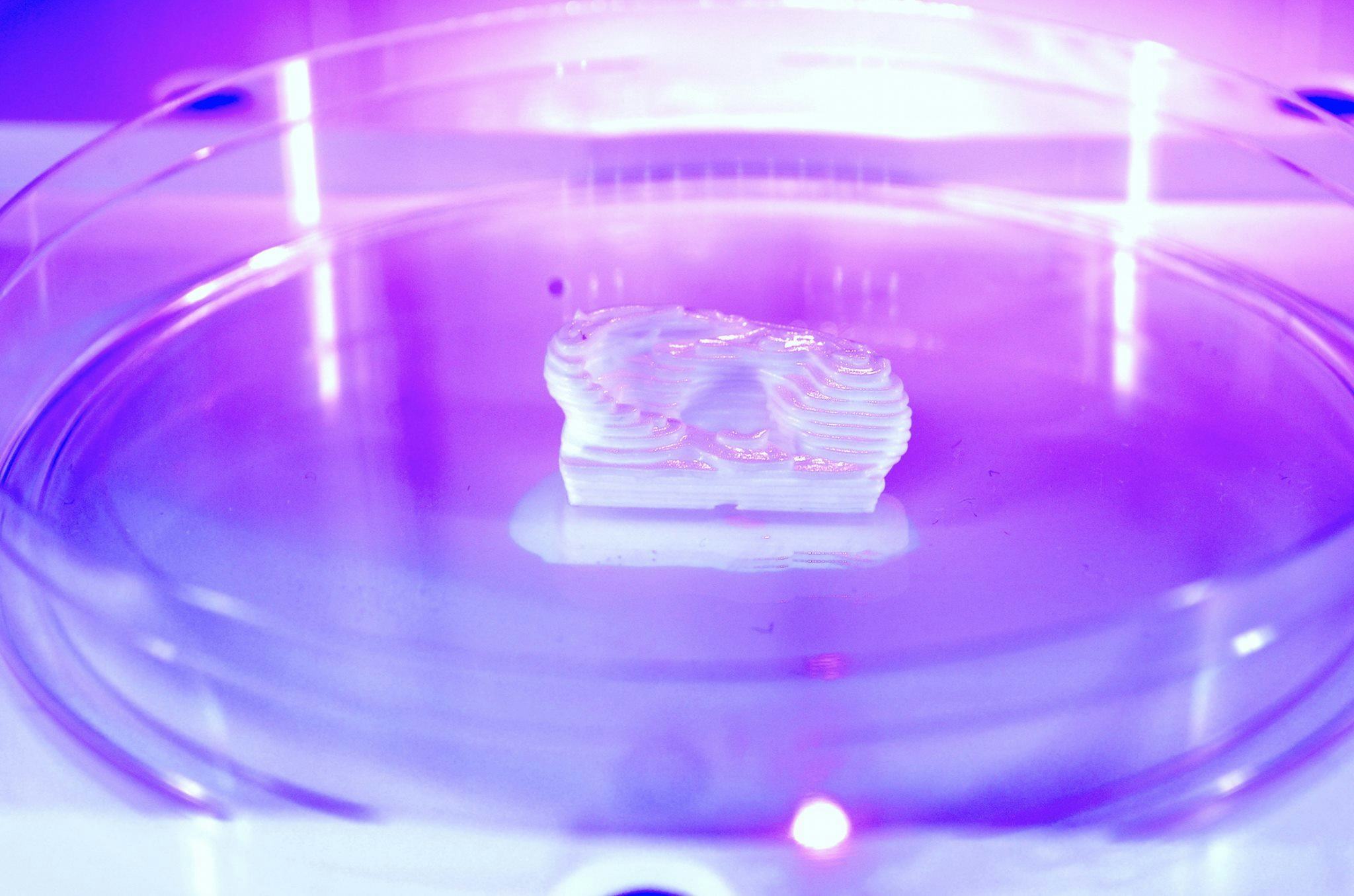 The technology can be used to produce new materials and therapies through the printing of bioinks comprising cells and biomolecules, with or without scaffold-forming materials. Applicants in this area will want to protect the bioinks themselves and the 3D printed products that result, as well as the equipment and associated methods of use. While claims to methods of bioprinting as well as to biomaterials used in methods of treatment may be patentable, applicants should be aware to avoid any exclusions. If you would like to discuss these issues in more detail, please let us know.
The technology can be used to produce new materials and therapies through the printing of bioinks comprising cells and biomolecules, with or without scaffold-forming materials. Applicants in this area will want to protect the bioinks themselves and the 3D printed products that result, as well as the equipment and associated methods of use. While claims to methods of bioprinting as well as to biomaterials used in methods of treatment may be patentable, applicants should be aware to avoid any exclusions. If you would like to discuss these issues in more detail, please let us know.
[1] Active players in this area include T&R Biofab, CELLINK (in partnership with AstraZeneca), and Prellis (in partnership with Sanofi), who develop 3D printed organoids for this purpose.
[2] Companies pursing this goal include CELLINK, 3D Systems, Medtronic, United Therapeutics, Ricoh, and Organovo
[3] Volumetric Biotechnologies and 3D Systems 3D printing platform for human organ printing (3D Systems Announces Acquisition of Volumetric Biotechnologies | 3D Systems)
[4] 3D bioprinting using stem cells (nature.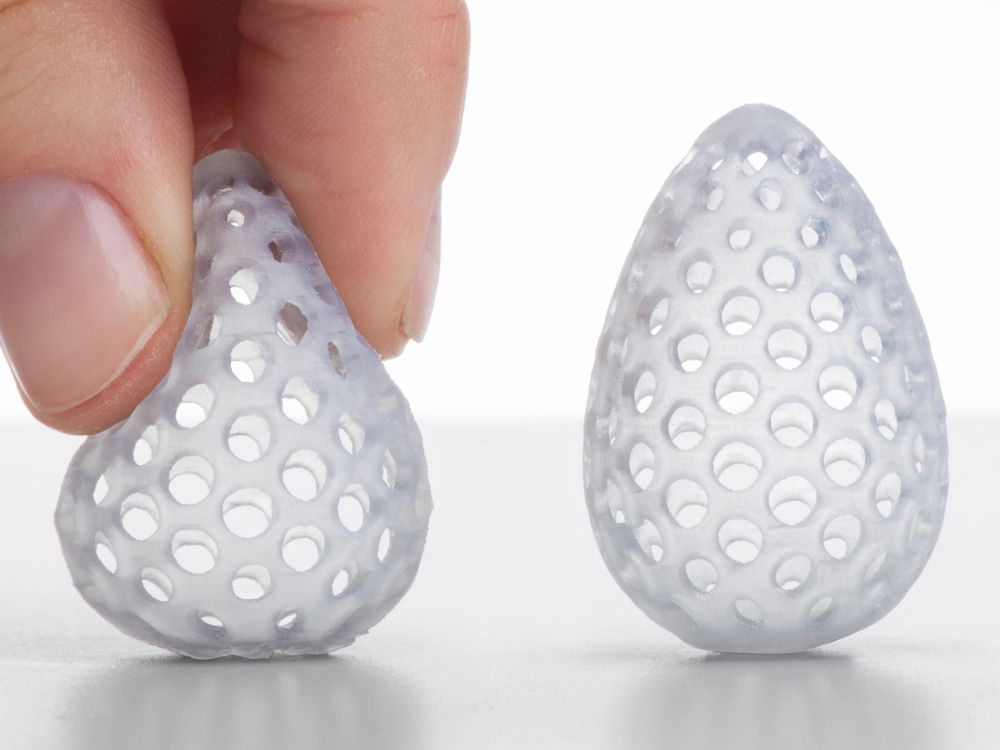 com)
com)
[5] T1695/07, which applies G1/07.
Bioprinter: 3D printing of organs
3D bioprinting is an advanced technology that saves lives and helps create new medicines. What is the peculiarity and complexity of developments, who is engaged in them and what successes have already been made - this will be discussed in the material. We will also get acquainted with all the methods of bioprinting known today.
- How bioprinters print and what is 3D bioprinting
- The first biological 3D printer
- 3D bioprinting technologies
- Multimaterial Multinozzle 3D (MM3D) Technology, Wyss Institute
- Sound-Induced Morphogenesis (SIM) Technology, mimiX Biotherapeutics
- Biopixlar Bioprinter, Fluicell
- CELLINK Bioprinters
- Bioprinter that creates micro-human ears for patients University of Wollongong
- Bioink
- 3D Bioprinting Solutions
- What do 3D bioprinters print?
- Where do they print?
- 3D bioprinters in Russia
How bioprinters print and what is 3D bioprinting
3D bioprinting is the creation of 3D models using biomaterial, which includes living cells. It is used to reproduce complex structures such as skin tissue or blood vessels.
It is used to reproduce complex structures such as skin tissue or blood vessels.
Model cells are taken from the patient and cultured until their mass is sufficient to create a bioink. The resulting ink is loaded into the printer, which prints the desired model.
Getting enough cells is not always possible, so seaweed or porcine collagen protein comes to the rescue. Stem cells are also used, which have the ability to become any cell in the body.
The first biological 3D printer
The first serial bioprinter was released by the American company Organovo by the end of 2009. The Australian company Invetech became its industrial partner. Thanks to joint efforts, the machine was born, which in 2010 printed the first full-fledged blood vessel.
Organovo representatives decided to move away from the idea of growing organs in a test tube and suggested that it would be much more efficient to print it. They came up with the NovoGen technology, which regulated all the interactions between the biological component of the process and its mechanical part. Invetech was involved to implement the idea. The collaboration resulted in a compact device with an intuitive interface.
Invetech was involved to implement the idea. The collaboration resulted in a compact device with an intuitive interface.
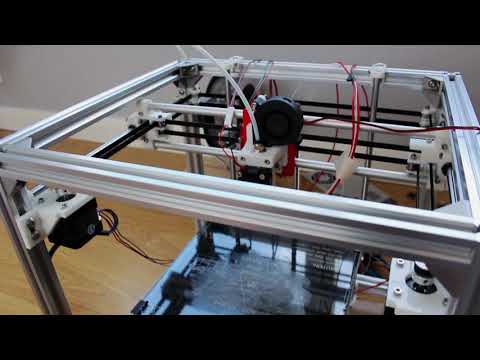
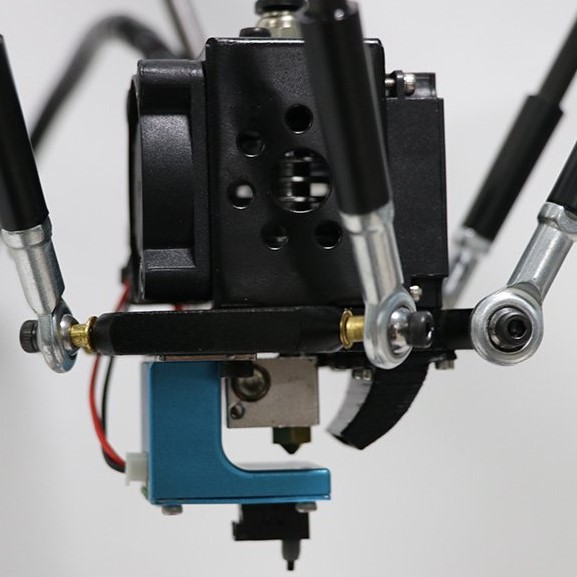
The printer had two printheads. One was filled with the necessary biomaterial, the second - with auxiliary components (collagen supporting the hydrogel, growth factors). Printing accuracy reached micrometers, which played an important role in the correct placement of cells.
3D bioprinting technologies
There are several technologies and approaches being developed and applied in the field of bioprinting. Scientists and researchers from private companies and institutions work on each of them.
Technology Multimaterial Multinozzle 3D (MM3D), Wyss Institute
The technology developed at the institute is based on the use of fast moving high pressure valves. The applied method makes it possible to switch between materials up to 50 times per second. This speed is faster than you can see with the naked eye.
The printheads themselves are 3D printed, so they can be easily customized to your specific needs.

The technology is suitable for manufacturing complex objects, including moving robots. The method significantly speeds up the creation of complex models, because the printheads can use several nozzles at once.
Sound-Induced Morphogenesis (SIM) Technology by mimiX Biotherapeutics
Swiss technology is based on the reproduction of well-defined biological patterns, which are self-assembled into functional tissues using sound waves. The method embodies a highly efficient sequence for reproducing organized and dense cellular structures.
The mimiX technology uses sound waves. The space for growing cells is formed around a given type of speaker. Depending on the shape of the cup and the sound produced, structures of various shapes, such as gratings, are formed.
The creation of such a method serves an important purpose - the availability and speed of playback, which can be carried out in any room.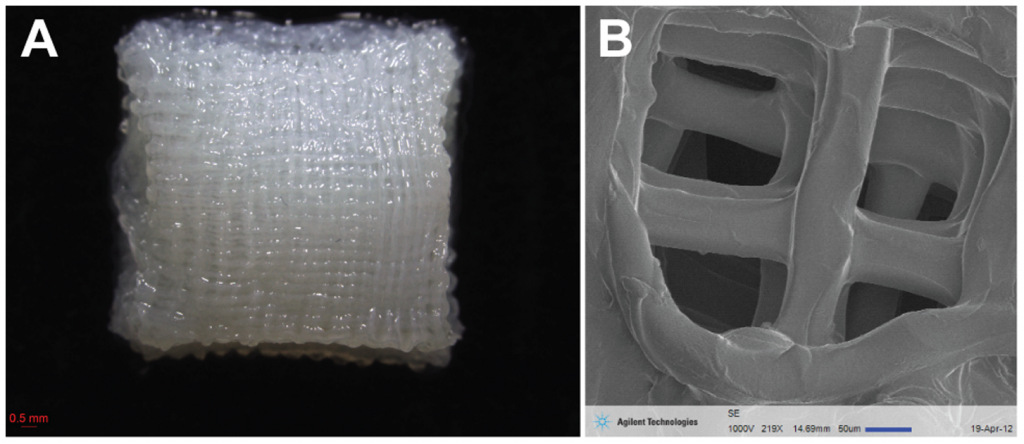 Prior to the invention of the SIM, bioprinting was available for scientific research. For clinical, it has become too complicated and lengthy. Now this has changed.
Prior to the invention of the SIM, bioprinting was available for scientific research. For clinical, it has become too complicated and lengthy. Now this has changed.
Fluicell Biopixlar Bioprinter
Swedish-based Fluicell focuses on creating platforms for studying cell behavior. Her method of work makes it possible to make complex structures that mimic tissue, in which the location of individual cells is controlled by a gamepad. The workflow is similar to a video game.
The company uses the micro-jet technique. Thanks to the micro jet tube and the precision of the pump during the direction of the biomaterial to the printing zone, it gives micro-level control over the material. Because of this, systems scale to the macro level naturally. High resolution prints are produced.
The method makes it possible to reproduce multicomponent structures, while the material can be created in the printer itself. This approach eliminates the need for laboratory preparation.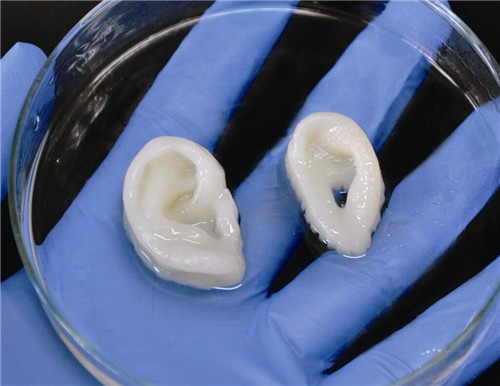 The mixing progress of different materials is controlled in the microfluidic chamber. The result is a 3D printed finished structure, which was created without the use of gels and scaffolds.
The mixing progress of different materials is controlled in the microfluidic chamber. The result is a 3D printed finished structure, which was created without the use of gels and scaffolds.
The technical capabilities of this method make it ideal for processing scarce materials such as biopsy specimens, stem cells and primary cells.
CELLINK Bioprinters
CELLINK is a Swedish company that develops bioprinting technologies for applications in various fields, including cosmetics and medicine. The principles generated by the organization work to create skin tissue, cartilage, liver and other products.
In 2019, the manufacturer launched two models of bioprinters on the market - Bio X6 and Lumen X. The first one is designed for creating constructs with any type of cells. With it, you can reproduce any tissue found in the body. The company focuses on quick results and combining a large number of materials.
The Bio X6 has 6 printheads built in with CELLINK Clean Camera Technology. It is equipped with a smart interchangeable head method and two powerful fans to create excess air pressure inside the chamber. The user gets the opportunity to combine several materials in one print with a structure of increased complexity.
It is equipped with a smart interchangeable head method and two powerful fans to create excess air pressure inside the chamber. The user gets the opportunity to combine several materials in one print with a structure of increased complexity.
The second Lumen X unit is the result of a collaboration with the American company Volumetric. This is a startup focused on creating bioprinters using SLA technology. The device has a low cost and modest dimensions. At the same time, it has high printing accuracy and excellent performance. Such characteristics are especially important for the creation of vascular structures. Lumen X gets the job done 10 times faster than its competitors under the same conditions.
Bioprinter for Microtia patients creating human ears, University of Wollongong
Myctoria is a congenital defect associated with developmental arrest of the outer ear. It is found during pregnancy. Since the structure of the ear has a specific shape, the treatment of its deformity causes serious difficulties. According to the creators of the bioprinter, the new technology is leading to a revolution in helping children with microtia.
According to the creators of the bioprinter, the new technology is leading to a revolution in helping children with microtia.
The Australian University of Wollongong created the Alek 3D printer. It prints human ears for further use in reconstructive surgery. Stem cells serve as the basis for bioink. The creation of ears on a bioprinter looks very promising, since the method allows you to design a transplant according to the shape of the patient's face and do it in a fairly short time. The technology excludes the search for donors to take a piece of cartilage, the work is based on the use of the patient's natural tissues.
Bioink
Manufacturers are developing not only the technology and design of printing machines, but also materials that can be used to create complex structures and entire organs.
Allevi Liver Tissue Ink
The complexity of reproducing the liver lies in the fact that it has many important functions for life. There are more than five hundred of them. A small number of manufacturers are able to create bio-ink for the liver that will meet all the necessary conditions.
A small number of manufacturers are able to create bio-ink for the liver that will meet all the necessary conditions.
The American company Allevi is one such company. The drug, which makes it possible to reproduce tissue-like structures that mimic the natural characteristics of tissues, can be freely purchased through the Allevi online store.
Biogelx Synthetic Bioink
Biogelx is a company from Scotland. It is based in a laboratory at the University of Strathclyde in Glasgow. The direction of the company is the research and creation of artificial materials for bioprinting.
Hydrogel ink has a unique chemical and physical variability. It allows you to accurately recreate a variety of tissue parameters. As a result, cells are able to interact in an almost natural environment.
Ink helps keep cells alive. They provide a simple crosslinking technique and viscosity control as well as a high degree of reproducibility. Due to its positive technical abilities, the material is compatible with a wide range of 3D bioprinters.
Due to its positive technical abilities, the material is compatible with a wide range of 3D bioprinters.
Hydrogel with mineral nanoparticles, University of Texas
American development from the staff of the University of Texas (TAMU). Scientists have created a material in the form of a hydrogel. It contains mineral nanoparticles. They have the ability to carry out protein preparations to control the behavior of cells. Inks of this kind help in the field of creating tissues containing blood vessels.
Developers have been developing hydrogel bioinks based on the inert polymer PEG (polyethylene glycol). Printing with this type of ink is difficult due to its low viscosity. In the course of research, it turned out that silicate nanoparticles effectively increase the degree of viscosity, while almost not changing the other technical parameters of the printed material. Thus, TAMU workers have created a new class of hydrogels.
Bio-ink for artificial leather printing, Renseller Polytechnic Institute
The production of high-quality skin imitations after burns and other wounds has occupied the minds of bioengineers for many years. There are 2 ways to treat serious skin lesions. The first is the use of autologous skin grafts. Healthy tissue is taken from the patient and transplanted to damaged areas, while fresh wounds are formed and, in general, the procedure is quite unpleasant and painful.
There are 2 ways to treat serious skin lesions. The first is the use of autologous skin grafts. Healthy tissue is taken from the patient and transplanted to damaged areas, while fresh wounds are formed and, in general, the procedure is quite unpleasant and painful.
The second method is to use skin substitutes made from foreign materials, such as bovine collagen. Such imitations do not completely cover deep wounds and are very different from natural skin.
Skin resurfacing technology from a collaboration between Rensselaer Polytechnic Institute (RPI) and Yale University promises to revolutionize skin grafting. They created bio-ink using living human cells. The material helps in reproducing artificial skin, which later itself recreates the system of blood vessels.
3D Bioprinting Solutions
3D Bioprinting Solutions is the only bioprinting company in Russia. The company was founded in 2013. One of the co-founders was the co-founder of INVITRO - Alexander Ostrovsky.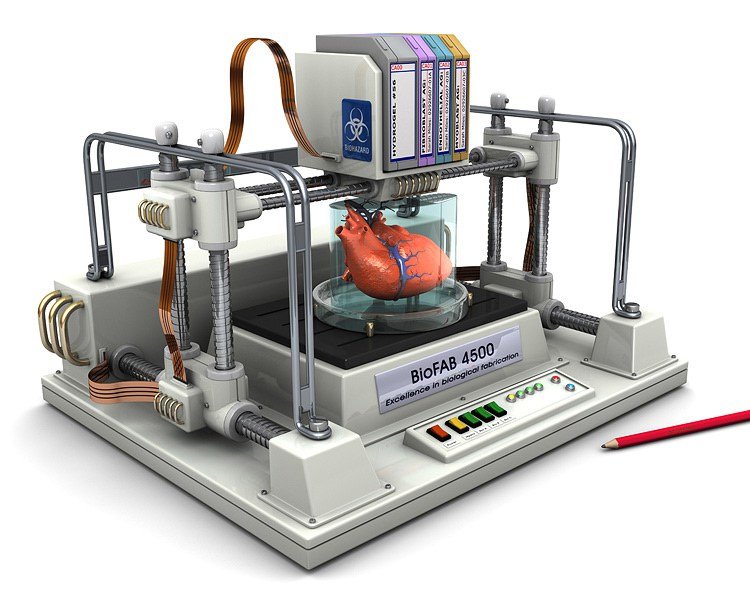 His specialty is a resuscitator.
His specialty is a resuscitator.
In 2014, the laboratory presented the first bioprinter made in Russia. He received the name FABION. According to the list of the use of various printed materials, this device is one of the leaders in the field of multifunctional devices.
In early 2015, the company created and successfully transplanted a mouse thyroid organ construct. In 2016, researchers produced a printhead that can automatically feed tissue spheroids for 3D bioprinting. The development was applied in the new version of the device - FABION-2.
After the release of an updated version of the device, the company's specialists focused on creating a printer that uses a new working methodology, different from previous solutions. It was the principle of magnetic levitation and the ability of microtissues to self-assemble from tissue spheroids. A fully functioning magnetic assembly saw the light of day by the spring of 2017.
At the end of the summer of 2017, cooperation with the state company Roscosmos began. The laboratory has signed a contract for the implementation of a space biofabrication experiment aboard the Russian part of the ISS. Scientists have begun to develop the Organ.Avt printer capable of working in zero gravity.
The laboratory has signed a contract for the implementation of a space biofabrication experiment aboard the Russian part of the ISS. Scientists have begun to develop the Organ.Avt printer capable of working in zero gravity.
The Magnetic Bioprinter experiment started at the end of 2018. In its course, models of human bone and cartilage tissue, as well as the mouse thyroid gland, were printed. To carry out the work, the Soyuz MS-11 crew members underwent appropriate training at the 3D Bioprinting Solutions laboratory.
In addition to bioprinters, the company has developed a line of multifunctional collagen products - Wiscoll. It is suitable for use in any 3D bioprinter. Bioink is used for a wide range of biofabrication experiments. The product is a concentrated solution of collagen of the first type of the highest degree of purification. It is immediately ready for use.
What do 3D bioprinters print?
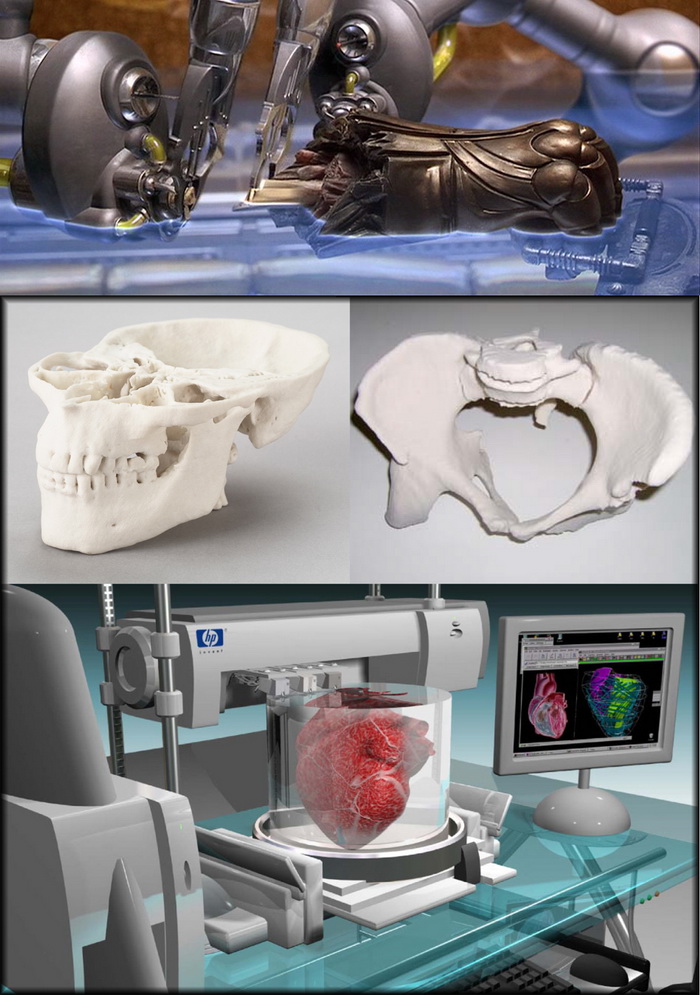
Printing organs
Printing fully functional complex internal organs is not yet possible, although research is ongoing in this area.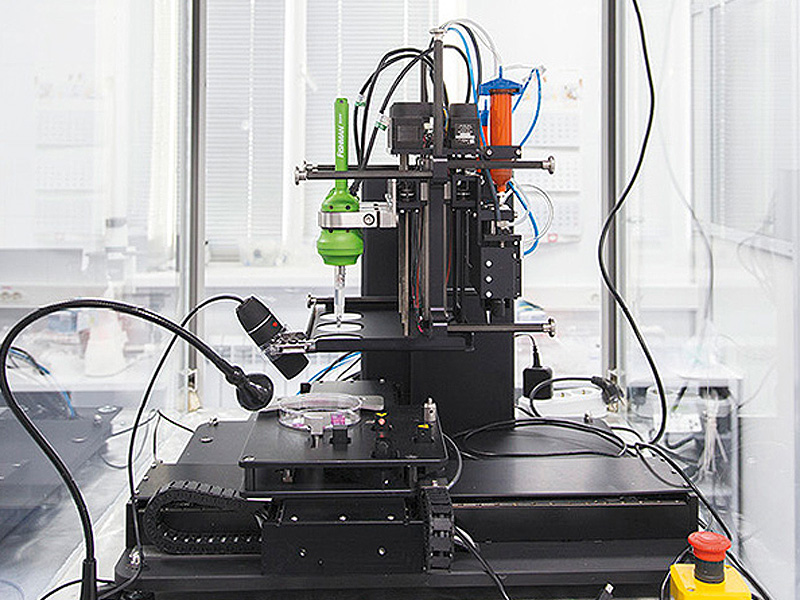 For example, the bladder has already managed to reproduce. It happened in 2013 in the USA (Wake Forest University).
For example, the bladder has already managed to reproduce. It happened in 2013 in the USA (Wake Forest University).
Scientists have extracted raw material from a patient's poorly functioning organ, nurtured them and added nutrients. Next, they reproduced the shape of the bladder according to the parameters of the patient and cultured cells impregnated through it. The model was placed in an incubator, brought to the required condition and transplanted into a human. Over time, it collapsed, leaving completely organic material in its place.
The same team produced viable urethras. Research is ongoing and breakthroughs are being made in the creation of the kidneys, liver and heart.
Printing of tissues and vessels
The human body is pierced by tens of thousands of kilometers of capillaries, arteries and veins. Over time, they wear out, and scientists are conducting research on the possibility of their full replacement. Creating body parts on a bioprinter is impossible without reproducing viable blood vessels. Technologies make it possible to create materials designed for further favorable independent development of blood vessels.
Technologies make it possible to create materials designed for further favorable independent development of blood vessels.
Surgical practice
Surgeons got the opportunity to practice on operations on organs and tissues that look 100% real. This happens both with the help of virtual prototyping and with the use of 3D printed models.
New drug testing
Bioprinted tissue has multiple cell types with different densities and key architectural features. This makes it possible to conduct research on the impact of diseases on the body, as well as to work out various methods of treatment.
Where do they print?
Organizations that offer organ printing or sell bioprinters:
- 3D Bioprinting Solutions - Russia, Moscow. Specializes in frameless printing, created two printers - FABION and FABION-2. Develops his own method of organoprinting.
- Organovo - USA, San Diego. Produces and sells liver tissue to pharmaceutical companies.
 In 2009, the first mass-produced bioprinter, Novogen, was released.
In 2009, the first mass-produced bioprinter, Novogen, was released. - BioBots - USA, Louisville. A startup that introduced a cheap bioprinter for commercial use in 2013. Available BioBot BASIC. Work is underway on the second version of the device.
- Cyfuse Biomedical - Japan, Tokyo. The company produced the Regenovo bioprinter, which can be used to create skin tissues and grow blood vessels.
3D bioprinters in Russia
So far, bioprinting devices in Russia are represented by only one company created by the co-founder of the INVITRO network - 3D Bioprinting Solutions. Ongoing research on the Russian part of MSCs under weightless conditions gives researchers hope that unique data will be obtained, on the basis of which new drugs will be developed.
Scientists are also optimistic about the creation of functional complex organs of the human body, saying that they will appear already in the current century.
Emerging technologies in the field of bioprinting make it possible to draw the following conclusions:
- 05 May 2020
- 10274
Get expert advice
Organ printing: how 3D bioprinting technology has advanced and what hinders its development
Rusbase
November 12, 2019
The artificial creation of human skin, tissue and internal organs may sound like science fiction, but most of it is happening right now. In research centers and hospitals around the world, advances in 3D printing and bioprinting are providing new opportunities for human treatment and scientific research.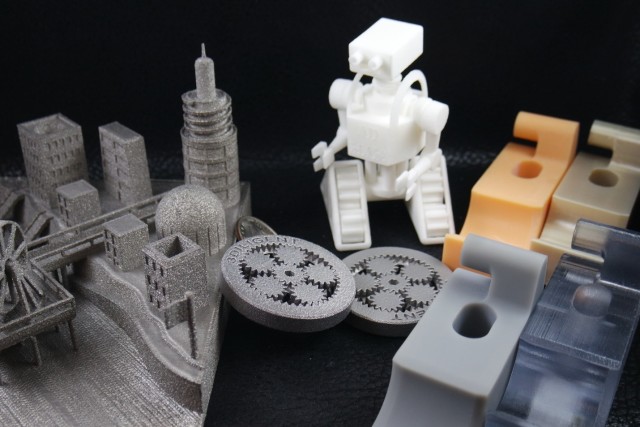 In the coming decades, bioprinting could be the next major milestone in healthcare and personalized medicine.
In the coming decades, bioprinting could be the next major milestone in healthcare and personalized medicine.
Let's talk about bioprinting technology, the latest advances in the industry and the limitations that professionals face.
How a 3D Printer Works
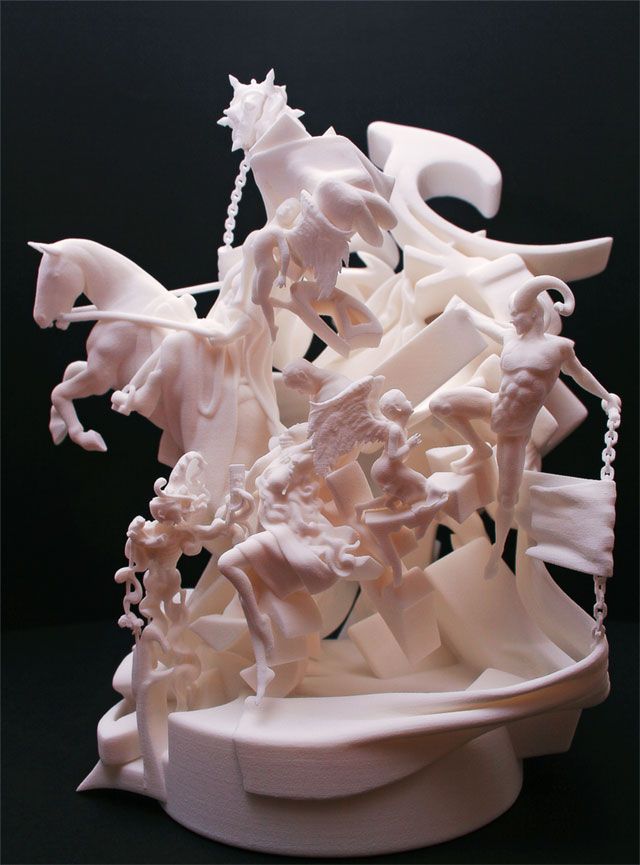
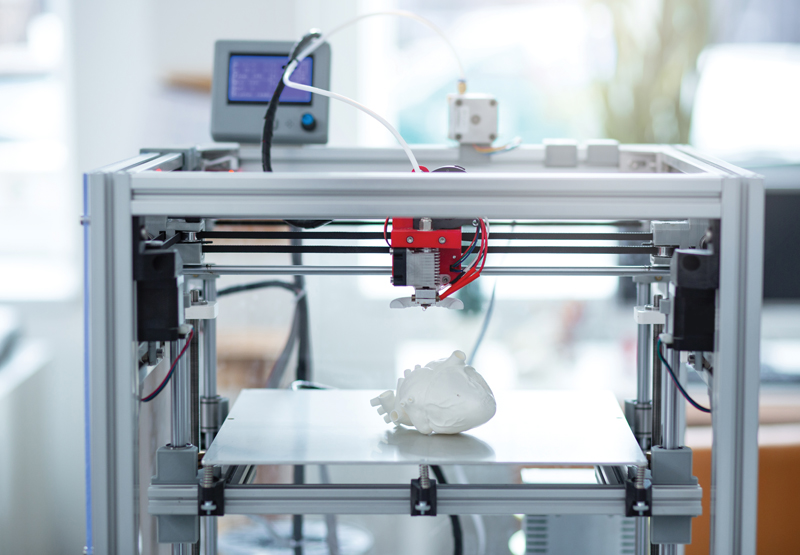
Traditional printers, like the one you have at home or office, work in two dimensions. They can print text or images on a flat surface (usually paper) using the x (horizontal) and y (vertical) dimensions. 3D printers add another dimension - depth (z). During the printing process, the printer heads can move up and down, left and right, back and forth, but instead of delivering ink to paper, they distribute various materials - polymers, metal, ceramics and even chocolate - until the "print" of a holistic, voluminous object , layer by layer in a process known as "additive manufacturing".
To create a 3D object, you need a blueprint for it, a digital file created with modeling software. After its creation, the computer-generated model is sent to the printer. Your chosen material is loaded into the machine and ready to be heated to easily flow out of the printer nozzle. As the printer reads the plan, its head moves, depositing successive layers of the selected material to create the final product.
After its creation, the computer-generated model is sent to the printer. Your chosen material is loaded into the machine and ready to be heated to easily flow out of the printer nozzle. As the printer reads the plan, its head moves, depositing successive layers of the selected material to create the final product.
As each layer is printed, it is solidified either by cooling or by mixing two different solutions delivered by the printer head. The new layers precisely lay down on the previous ones to make a stable, cohesive element. In this way, you can create almost any shape, including a moving one.
3D printing allows you to create objects with geometric structures that would be difficult or impossible to make in other ways. A wide range of products are already being created using 3D printers, including jewelry, clothing, toys, and high-end industrial products. Even a 10-year-old Moscow schoolboy has learned how to work with a 3D printer: he prints 3D figures to order and sells them through Instagram.
How a bioprinter works
Bioprinters work in much the same way as 3D printers, with one key difference - they deposit layers of biomaterial, which can include living cells, to create complex structures such as blood vessels or skin tissue.
Living cells? Where do they get them? Every tissue in the body is made up of different types of cells. The required cells (kidney, skin, and so on) are taken from the patient and then cultured until there are enough of them to create "bio-ink" that is loaded into the printer. This is not always possible, therefore, for some tissues, stem cells are taken that are capable of becoming any cell in the body (organism), or, for example, porcine collagen protein, seaweed and others.
Often used in bioprinting is chitosan, a polysaccharide obtained from the external skeleton of mollusks (eg shrimp) or by fermenting fungi. This material has high biocompatibility and antibacterial properties.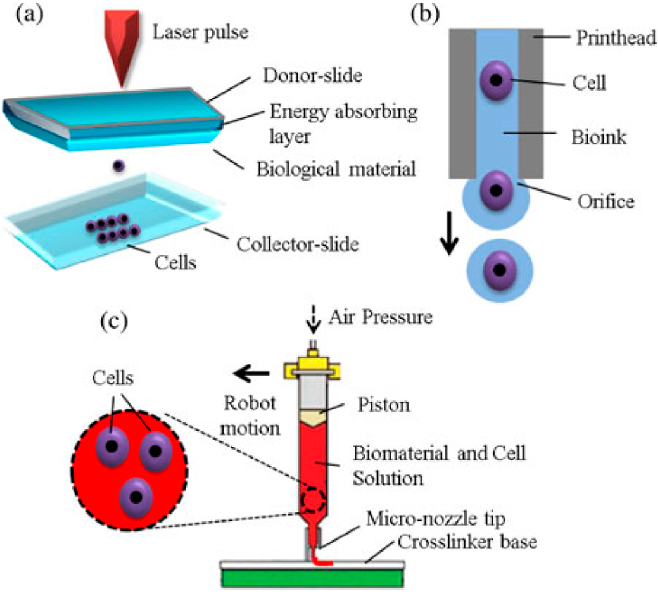 Its disadvantage is the low rate of gelation. Another popular material is a polysaccharide isolated from seaweed called agarose. Its advantages are high stability and the possibility of non-toxic cross-linking during research. However, this biomaterial does not decompose and has poor cell adhesion (the ability of cells to stick together with each other and with other substrates).
Its disadvantage is the low rate of gelation. Another popular material is a polysaccharide isolated from seaweed called agarose. Its advantages are high stability and the possibility of non-toxic cross-linking during research. However, this biomaterial does not decompose and has poor cell adhesion (the ability of cells to stick together with each other and with other substrates).
Collagen, a primary structural protein found in the skin and other connective tissues, has a high biological significance. It is the most abundant protein in mammals and a major component of connective tissue. Its disadvantages for bioprinting include the property of acid solubility. More information about biomaterials can be found here.
Based on computer designs and models, often scans and MRIs taken directly from the patient, the printer heads place the cells exactly where they are needed and within a few hours an organic object is built from a large number of very thin layers.
Organovo bioprinter creates tissues that mimic the structure and composition of various human organs
Source: Pbs. org
org
Scaffolding for ear or nose replacement at Wake Forest University in Winston-Salem, North Carolina
Source: CBS News
Computer displays an image of a "scaffold" for the human ear, created in the laboratory of Wake Forest University in Winston-Salem, North Carolina
Source: CBS News
Typically more than just cells are needed, so most bioprinters also supply some sort of organic or synthetic "glue" - a soluble gel or collagen scaffold to which cells can attach and grow. This helps them form and stabilize in the correct shape. Surprisingly, some cells can take the correct position on their own without any "scaffolding". How do they know where to go? How do embryonic cells develop in the uterus, or does adult tissue move to repair damage? Same here.
Universities, researchers and private companies around the world are involved in the development of bioprinting technologies. Let's take a look at some of the amazing things they are working on.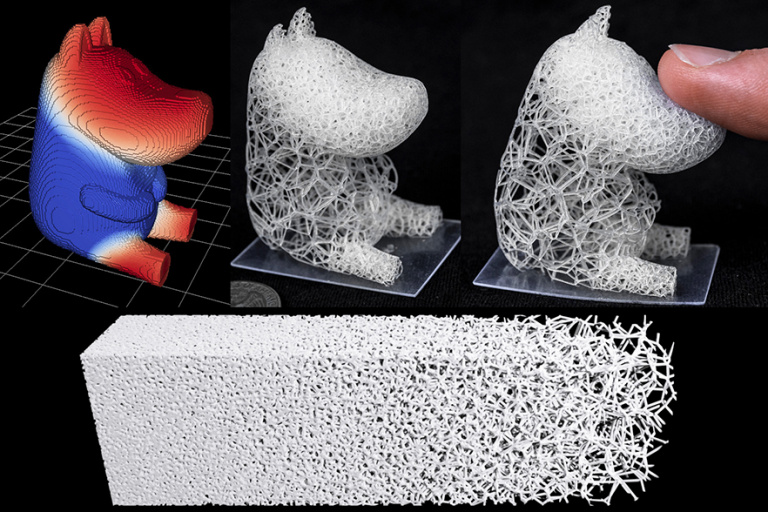
Bioprinting in Russia
3D Bioprinting Solutions is a biotechnology research laboratory founded by medical company INVITRO. The activity of the laboratory is the development and production of bioprinters and materials in the field of three-dimensional bioprinting and scientific research. August 23, 20193D Bioprinting Solutions laboratory sent a new batch of cuvettes to the ISS to continue experiments on bioprinting in space, which began in 2018. This was reported in the press center of the laboratory. This time it is planned to use organic and inorganic components to assemble bone tissue on the world's first space bioprinter Organ.Aut.
Symposium "Biofabrication in space"
Source: Zdrav.Expert
Organ.Aut magnetic bioprinter
Source: Zdrav.Expert
The astronauts will also grow protein crystals and experiment with printing biofilms of bacteria to study their behavior in zero gravity. Russian scientists expect to receive unique scientific data that can be applied in the development of new drugs.
Scientific director of 3D Bioprinting Solutions and leading researcher of the Institute of Regenerative Medicine, Candidate of Medical Sciences Vladimir Mironov, in his speech at the Department of Anatomy of Sechenov University on September 2, noted: “Living cells, tissues and human organs will be synthesized already in the current century. To do this, morphological sciences, such as microscopic anatomy and histology, must be digitized or digitalized, that is, digitized and made available for computer programs of robotic bioprinters, since without digital models it is impossible to print human tissues and organs.”
Bioprinting in the world
Every year, millions of people around the world need a bone transplant. Modern bone grafts often use cement-based synthetic material in combination with the patient's own bone. However, the use of these materials has a number of limitations - some transplants caused rejection and inflammatory processes in patients.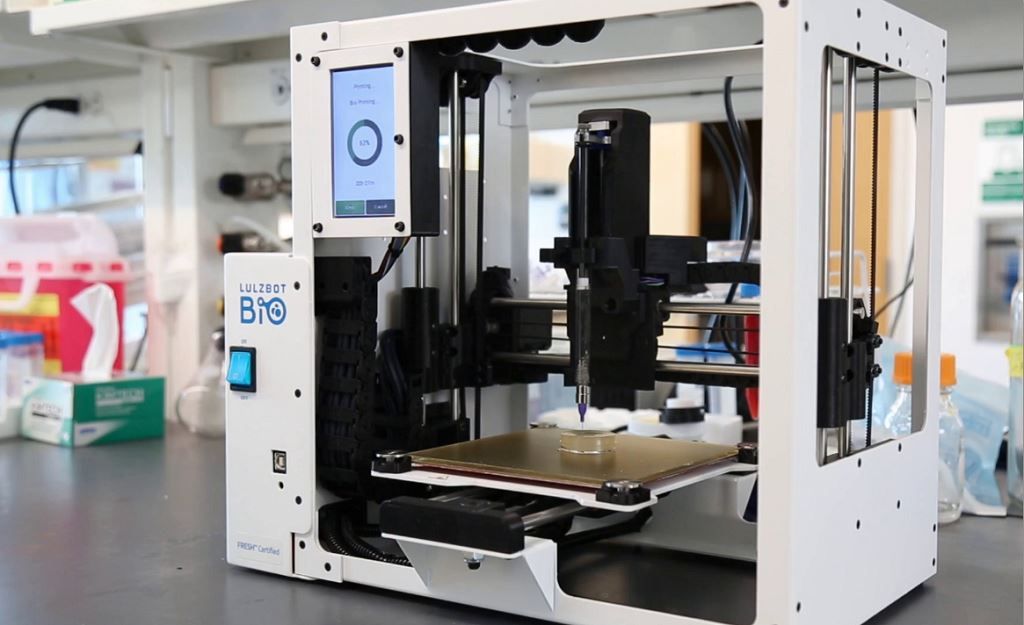 Reproduction of the natural bone-cartilage "interface" has also been problematic.
Reproduction of the natural bone-cartilage "interface" has also been problematic.
However, a team at Swansea University in 2014 developed a bioprinting technology that allows the creation of an artificial bone prosthesis in the exact shape of the desired bone, using a biocompatible material that is both durable and regenerative. At the same time, scientists from the University of Nottingham in England were working on similar studies.
It takes about two hours to print a small bone. Therefore, surgeons can do it right in the operating room. This part of the bone is then covered with adult stem cells that can develop into almost any other type of cell. This is combined with bio-ink from the printer, a combination of polylactic acid (which provides mechanical strength to the bone) and alginate, a gel-like substance that serves as a shock-absorbing material for cells. The final product is then implanted into the body, where it will completely disappear within about three months and be replaced by new bone.
Researchers hope that in the future, bioprinted bones can be created with sufficient reliability to support complex spinal reconstruction, and that the bone material will be further improved to increase its compatibility with cartilage cells.
Source: ETH Zurich
Successful 3D printing of human cartilage may soon completely replace artificial implants for people in need of reconstructive surgery. Back in 2015, scientists in Zurich developed technology that would allow hospitals to print a full-size human nose implant in less than 20 minutes. They believe that any cartilage implant can be made using their technique.
Researcher Matti Kesti described the technology as follows:
“
“A serious car accident can cause the driver or passenger to suffer complex nose injuries. The nose can be restored by creating a 3D model on a computer. At the same time, a biopsy of the patient is performed and cartilage cells are removed from the victim's body, such as from a knee, a finger, an ear, or fragments of a broken nose. The cells are spawned in the laboratory and mixed with the biopolymer. From this suspension, a model of nasal cartilage is created using a bioprinter, which is implanted into the patient during surgery. In the process, the biopolymer is used simply as a mold. It is subsequently broken down by the body's own cartilage cells. And in a couple of months it will be impossible to distinguish between the graft and the person’s own nasal cartilage.”
The cells are spawned in the laboratory and mixed with the biopolymer. From this suspension, a model of nasal cartilage is created using a bioprinter, which is implanted into the patient during surgery. In the process, the biopolymer is used simply as a mold. It is subsequently broken down by the body's own cartilage cells. And in a couple of months it will be impossible to distinguish between the graft and the person’s own nasal cartilage.”
Matti Kesti
Since the implant was grown from the body's own cells, the risk of rejection will be much lower than for an implant made of, say, silicone. An additional advantage is that the bioimplant grows with the patient, which is especially important for children and young people.
If a person is severely burned, healthy skin can be taken from another part of the body and used to cover the affected area. Sometimes intact skin is missing.
Researchers at Wake Forest School of Medicine have successfully designed, built and tested a printer that can print skin cells directly onto a burn wound. The scanner very accurately determines the size and depth of damage. This information is sent to a printer and skin is printed to cover the wound. Unlike traditional skin grafts, it only takes a patch of skin one-tenth the size of a burn to grow enough cells to print. While this technology is still in the experimental stage, the researchers hope that it will be widely available within the next five years.
The scanner very accurately determines the size and depth of damage. This information is sent to a printer and skin is printed to cover the wound. Unlike traditional skin grafts, it only takes a patch of skin one-tenth the size of a burn to grow enough cells to print. While this technology is still in the experimental stage, the researchers hope that it will be widely available within the next five years.
As already mentioned, 3D printers print products in layers, and since the skin is a multi-layered organ with different types of cells, it is well suited for this type of technology. However, researchers still have a lot of problems to solve, in particular, how to prevent damage to cells from the heat generated by the printer. And of course, like most parts of the human body, the skin is more complex than it first appears—there are nerve endings, blood vessels, and a host of other aspects to consider.
Blood vessels
Biomechanical engineer Monica Moya holding a Petri dish with printed alginate-based biotubes. Biotubes can act as temporary blood vessels similar to blood vessels that help create a patch of living tissue.
Biotubes can act as temporary blood vessels similar to blood vessels that help create a patch of living tissue.
Source: embodi3D
With tens of thousands of miles of veins, arteries and capillaries in the human body, researchers are working to replace them if they ever wear out. The creation of viable blood vessels is also essential for the proper functioning of all other potential bioprinted body parts.
Biomechanical Engineer Monica Moya of Livermore National Laboratory. Lawrence uses bioprinting to create blood vessels. The materials created by her bioprinters are engineered to allow small blood vessels to develop on their own.
This development takes time, so vials of cells and other biomaterials are printed to help deliver vital nutrients to the printed environment. After a while, self-assembled capillaries connect with bioprinted tubes and begin to deliver nutrients to cells on their own, mimicking the work of these structures in the human body.
Internal organs
Many researchers hope that in 20 years the lists of patients waiting for organ transplants will become a thing of the past. They envision a world where any organ can be printed and transplanted in just a few hours, without rejection or complications, because these organs will be created from body cells according to the individual characteristics of each patient. Currently, bioprinting of fully functional complex internal organs is not possible, but research is ongoing (and not without success).
Bladder
For example, the bladder is already printed. In 2013, at Wake Forest University in the US, researchers successfully took cells from a patient's original, poorly functioning bladder, cultured them, and added additional nutrients. The 3D shape of the patient's bladder was then printed and the cultured cells soaked through it. The form was placed in an incubator and, when it reached the desired condition, it was transplanted into the patient's body. The mold will eventually collapse, leaving only the organic material. The same team successfully created viable urethras.
The mold will eventually collapse, leaving only the organic material. The same team successfully created viable urethras.
Physicians and scientists at the Wake Forest Institute for Regenerative Medicine (WFIRM) were the first in the world to create laboratory-grown organs and tissues that were successfully transplanted into humans. Right now they are working on growing tissues and organs for more than 30 different areas of the body, from the kidneys and trachea to cartilage and lungs. They also aim to accelerate the availability of these treatments to patients.
Scientists in Australia are doing similar research as well. They used human stem cells to grow a kidney organ that contains all the necessary cell types for a kidney. Such cells can serve as a valuable initial source for bioprinting more complex kidney structures.
MD, Professor of Urology, Professor of the Institute of Regenerative Medicine Anthony Atala shows a kidney created by a bioprinter. A modified desktop inkjet printer sprays cells instead of ink. The cells were cultured from the patient and the structural template for the kidney was obtained from the MRI (so it is the correct size and shape).
A modified desktop inkjet printer sprays cells instead of ink. The cells were cultured from the patient and the structural template for the kidney was obtained from the MRI (so it is the correct size and shape).
Using this technology, back in 2001, Atala printed and successfully transplanted a bladder into a young man, Jake.
Source: TedEd
Heart
Heart cells, laboratory-grown organelles. Source
Surprisingly, it is the human heart that can become one of the easiest organs to print, since, in fact, it is a pump with tubes. Of course, everything is not so simple, but many researchers believe that humanity will learn to print hearts before kidneys or liver.
Researchers at the Wake Forest Institute for Regenerative Medicine in April 2015 created "organoids" - 3D printed fully functional, beating heart cells.
In April 2019, Israeli scientists printed the world's first 3D heart. It is still very small, the size of a cherry, but it is able to perform its functions.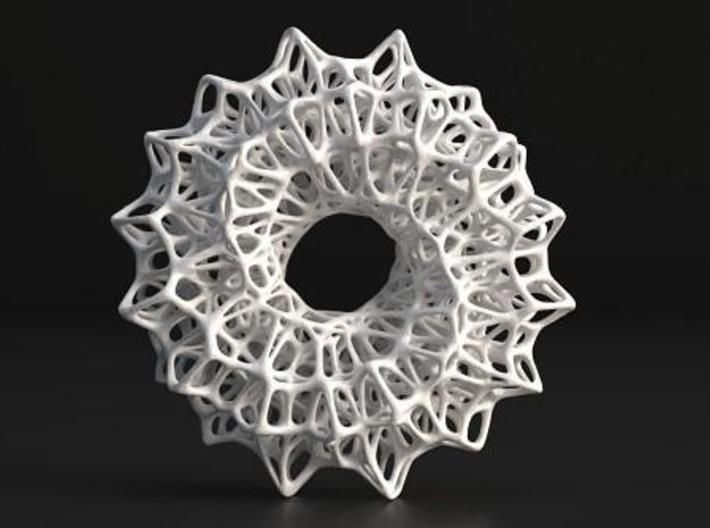 The 3D heart with blood vessels uses personalized "ink" of collagen, a protein that supports cell structures, and other biological molecules.
The 3D heart with blood vessels uses personalized "ink" of collagen, a protein that supports cell structures, and other biological molecules.
A Tel Aviv University researcher holds the world's first 3D printed heart on April 15, 2019.
Source: Haaretz
“This is the first time anyone anywhere has successfully designed and printed an entire heart with cells, blood vessels, ventricles and chambers,” said Tel Aviv University scientist Professor Tal Dvir.
So far, scientists have been able to print tissue from cartilage and the aortic valve, for example, but the challenge has been to create tissue with vascularity—the blood vessels, including capillaries, without which organs cannot survive, let alone function.
The Tel Aviv scientists started with human adipose tissue and separated the cellular and non-cellular components. They then reprogrammed the cells to become undifferentiated stem cells, which could then become cardiac or endothelial.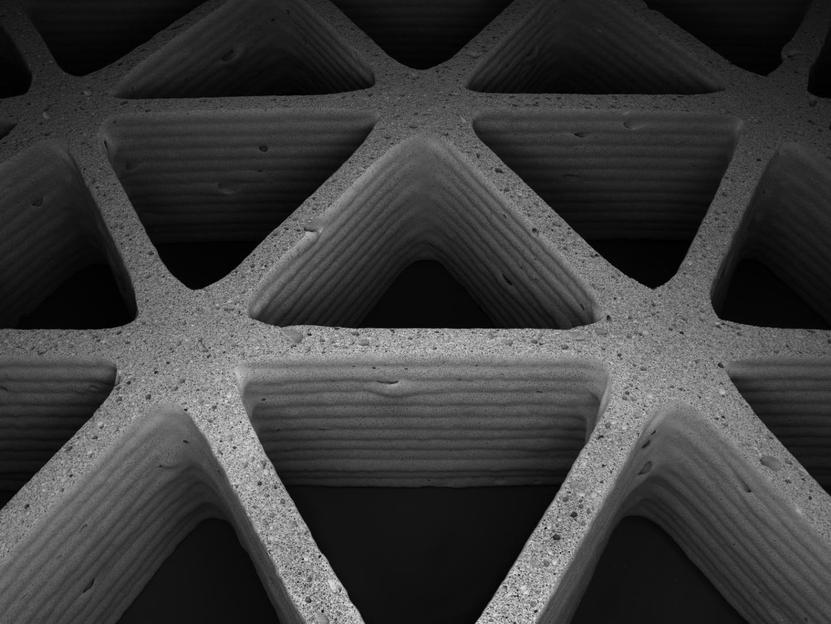 Endothelium - a single layer of flat cells lining the inner surface of the heart cavities, blood and lymphatic vessels. Endothelial cells perform many functions of the vascular system, such as controlling blood pressure, regulating the components of blood clotting, and the formation of new blood vessels.
Endothelium - a single layer of flat cells lining the inner surface of the heart cavities, blood and lymphatic vessels. Endothelial cells perform many functions of the vascular system, such as controlling blood pressure, regulating the components of blood clotting, and the formation of new blood vessels.
Non-cellular materials, including a large amount of proteins, were processed into a "personalized hydrogel" that served as "printing ink".
It will be years before this technology can create organs for efficient transplantation. However, the achievements of scientists in Tel Aviv are a huge milestone along the way.
Medical research and pharmacology
One of the key potential uses for bioprinted living materials is in the field of medical and drug research. Bioprinted tissues have several cell types with different densities and key architectural features. This allows researchers to study the impact of various diseases on the body, the stages of disease progression and possible treatments in the natural microenvironment.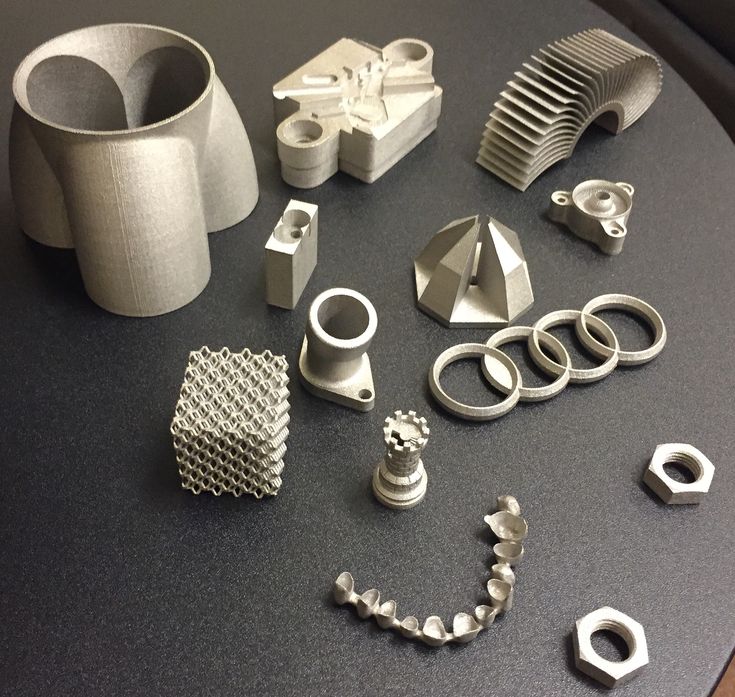
One of the most impressive developments in recent years is the development of a desktop brain at the ARC Center of Excellence in 2016. The researchers were able to use a 3D printer to create a 3D printed six-layer structure that includes nerve cells that mimic the structure of brain tissue.
This opens up huge potential benefits for researchers, pharmaceuticals and private companies, because it will allow them to test new products and drugs on tissue that accurately reflects the responses of human brain tissue, as opposed to animal samples, which may cause a completely different response. The desktop brain can also be used to further investigate diseases such as schizophrenia or Alzheimer's.
We are far from printing the brain, but the ability to arrange cells to form neural networks is a significant step forward. By allowing researchers to work with human tissue in real time, testing processes can be greatly accelerated and results can be more realistic and accurate.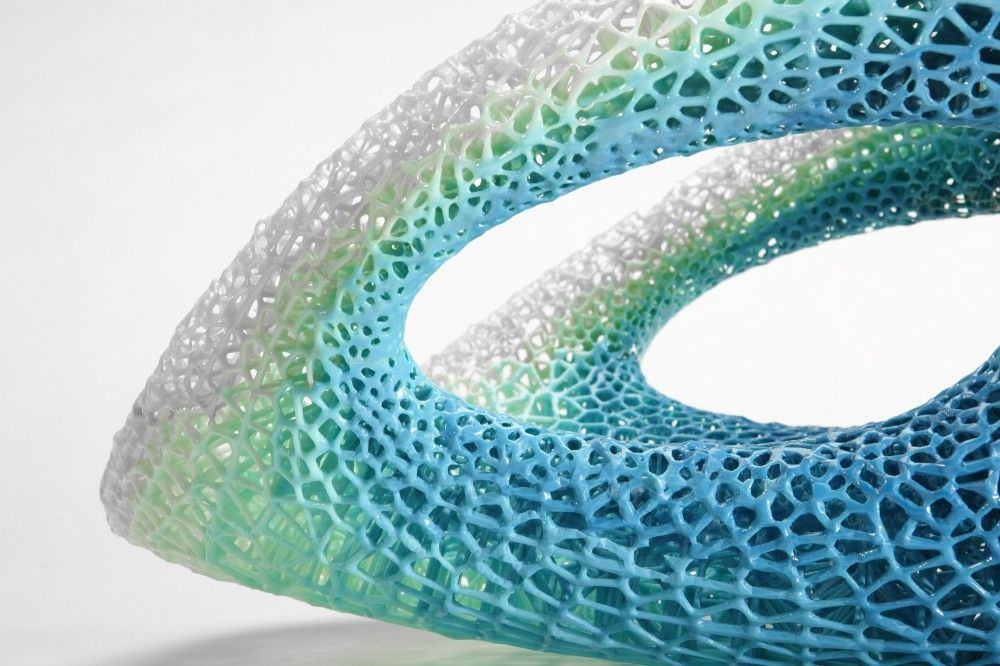 It will also reduce the need to use laboratory animals for medical tests and potentially dangerous human testing.
It will also reduce the need to use laboratory animals for medical tests and potentially dangerous human testing.
Medical simulators and data registries
Source: Simbionix
Around 3,000 medical simulators are currently in use around the world to help doctors practice complex procedures. Virtual blood vessels, 3D printed organs... and no animal suffers!
The American company 3D Systems created an industry segment called VSP (Virtual Surgical Planning). This approach to personalized surgery combines expertise in medical imaging, surgical simulation and 3D printing. Surgeons using the Simbionix medical simulator for the first time often report feeling physical pain while empathizing with their virtual patient - the experience is so realistic. Organs and tissues look completely real. When stitching an organ, the surgeon sees on the screen a needle that enters the tissue, and pulls the thread. If the doctor does something wrong, the virtual blood vessels break and the organ begins to bleed.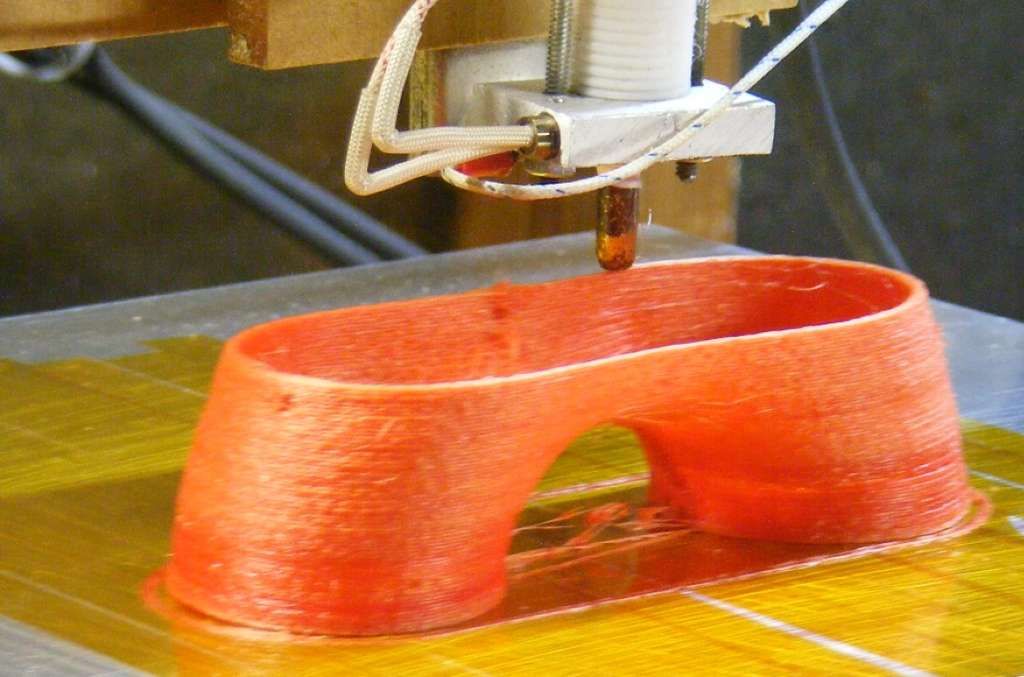 These simulators were developed by the Israeli company Symbionix, which was acquired by 3D Systems in 2014.
These simulators were developed by the Israeli company Symbionix, which was acquired by 3D Systems in 2014.
On September 3, 2019, the Radiology Society of North America (RSNA) and the American College of Radiology (ACR) announced the launch of a new 3D Medical Printing Clinical Data Registry to collect data on treatment outcomes using 3D printing at the point of care. This information will be a powerful tool to assess and improve patient care in real time, drive ongoing research and development, and inform patients and healthcare professionals about the best course of care.
“
“The creation of a joint RSNA-ACR 3D printing registry is essential to the advancement of clinical 3D printing. The registry will collect data to support the appropriate use of this technology and its implications for clinical decision making.”
William Widock, Professor of Radiology at the University of Michigan and Chairman of the RSNA 3D Printing Special Interest Group (SIG)
According to RSNA, the information in the registry will allow for the necessary analysis to demonstrate the clinical value of 3D printing. Due to the wide variety of clinical indications, different technologies for creating physical models from medical images, and the complexity of the models, it is problematic to choose the optimal treatment method. The registry will help solve this problem.
Due to the wide variety of clinical indications, different technologies for creating physical models from medical images, and the complexity of the models, it is problematic to choose the optimal treatment method. The registry will help solve this problem.
Bioprinting software
Bioprinter and bioprinting software manufacturer Allevi introduced Allevi Bioprint Pro software on September 5, 2019. Built-in model generation and integrated slicing will allow you to focus more on experimenting, rather than setting up the printer. The program runs entirely in the cloud, which means you can create your biostructures, define materials, and track prints right from a web browser on any computer.
According to the development team, the new bioprinter with the above software is powerful and easy to use and represents another piece of the puzzle on the way to 3D printed organs.
At the same time, CELLINK, the first bio-ink company, announced the launch of a new product to become the most flexible bio-printing platform on the market.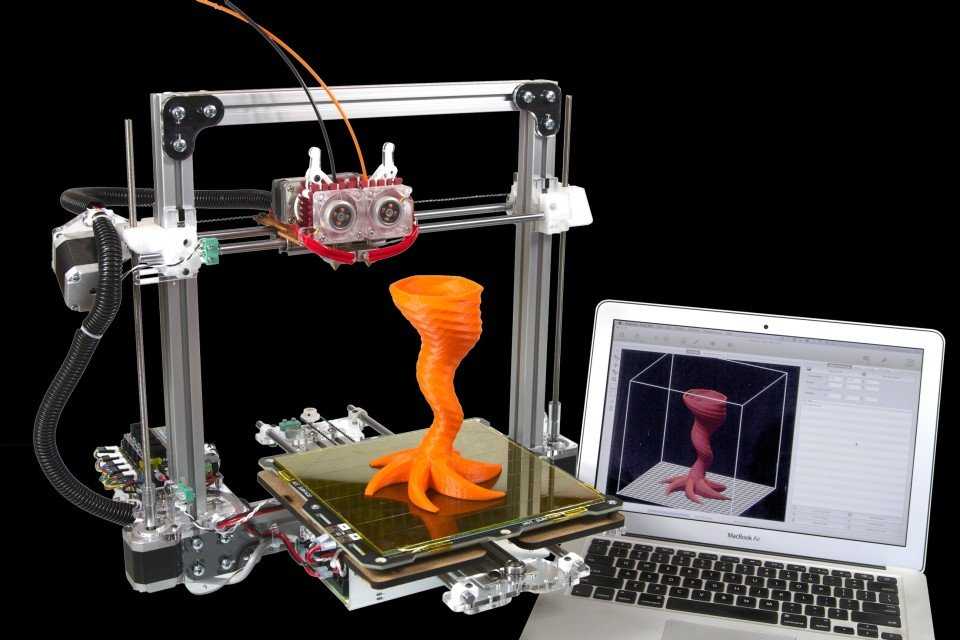 The BIO X6 bioprinter, which has no analogues at the moment, has the ability to combine more bioprinting materials, cells and tools.
The BIO X6 bioprinter, which has no analogues at the moment, has the ability to combine more bioprinting materials, cells and tools.
Why is this taking so long?
Complex structure of the body
The human body and its various components are much more complex than a plastic toy. The human organ has a complex network of cells, tissues, nerves, and structures that must be arranged in specific ways to function properly. From placing thousands of tiny capillaries in the liver to actually getting a printed heart that "beats" and contracts in the human body, there is still a lot of research and testing.
Legal regulation
In addition, bioprinting technologies, like all new medical treatments, must pass safety tests and due process of regulation before they become available.
Special software and hardware
It also takes time to develop special software and hardware. These programs can be written only with the appropriate data (medical, clinical, statistical, mathematical, and so on), which someone must first collect, analyze, systematize and digitize.
Working through all of these steps requires the integration of technologies from various fields, including engineering, biomaterials science, cell biology, physics, mathematics and medicine. So we need to be a little more patient.
The main thing is to know that those who work in the field, doctors and engineers, programmers and scientists are making progress every day both in the bioprinting technology itself and in understanding how it can be used and improved. Although we are not quite there yet, there is no doubt that medicine will be very different in 10-20 years, thanks also to bioprinting.
In brief
Bioprinting is an extension of traditional 3D printing.
Bioprinting can produce living tissue, bones, blood vessels, and possibly entire organs for use in medical procedures, medical training, and testing.
The cellular complexity of a living organism has made 3D bioprinting slower to develop than conventional 3D printing.