3D printed bolus radiotherapy
3D Printed Bolus for Radiotherapy
Enhance clinical precision, efficiency, and patient care
Our Simple Bolus software module allows users to confidently create patient-specific accessories that significantly reduce air gaps, spare healthy tissue, and provide superior dose distribution compared to traditional methods.
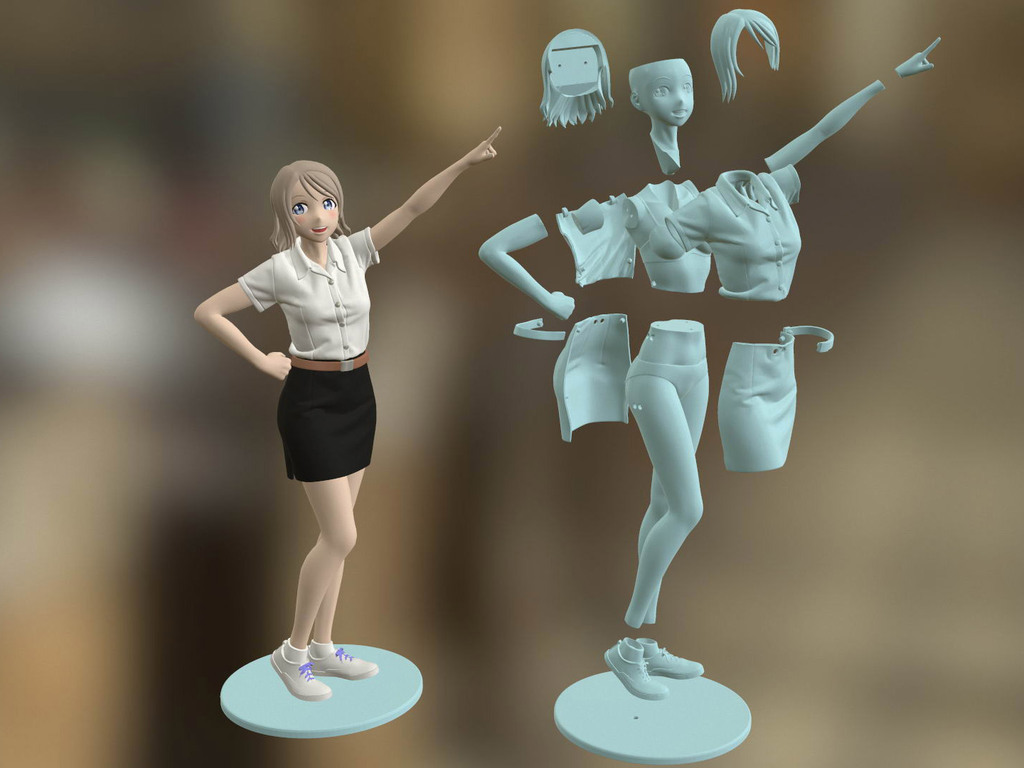
Our regulatory cleared software converts patient DICOM data into a digital model that can be 3D printed.
Key Benefits
Integration with clinical workflows enables users to create patient-specific bolus on demand using our turnkey 3D printing software solution backed by a regulatory cleared QMS.
- Patient-specific fit reduces air gaps and surface dose uncertainty compared to traditional sheet bolus.
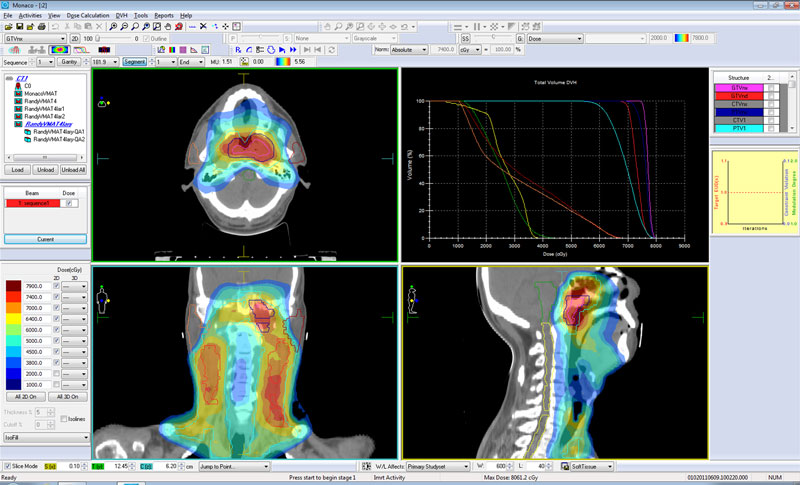
- The only regulated solution that allows users to customize a bolus, export the modified structure back into their TPS, and use the TPS to calculate dose.
- Eliminate the need for multiple, 3rd party software solutions that require excessive design time and do not have regulatory clearance.
- Confidence that what is planned in the TPS will result in a printed accessory that follows strict QA requirements used in radiation therapy.
- Adaptiiv software includes numerous post-processing features to ensure optimal and accurate bolus design:
- Smoothing: A smooth bolus surface improves patient comfort.
- Cropping: Improves printing success by creating a flat area for adhesion to the print bed.
- Patient ID: An unique patient identifier label can be printed directly onto the bolus.
- Cleaving: Cleave a bolus into two parts (at any angle) to treat complex patient anatomies, such as large extremities.
- In Vivo Dosimetry: Create and print dosimeter pockets directly within a bolus, enabling real-time recording of dose received by individual patients.

View / Download Product Brochure
3D Printed Moulds
We now offer an innovative and superior method to create soft and flexible patient-specific bolus. By listening to customer feedback, we developed a solution that allows users to easily create moulds that can be 3D printed and filled with flexible material to produce patient-specific bolus.
Learn more about this regulatory cleared process.
Step One
01
Create a plan + bolus in the TPS
Step Two
02
Modify the bolus in Adaptiiv software
Step Three
03
Verify the bolus in the TPS
Step Four
04
Create an STL file in Adaptiiv software
Step Five
05
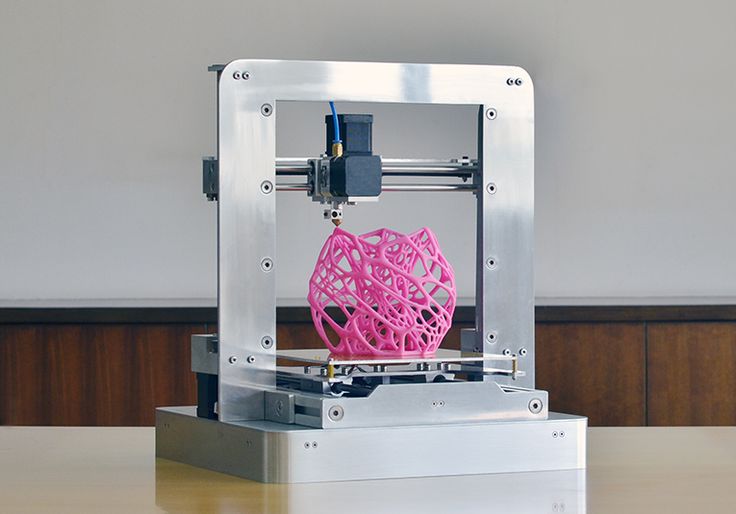
Print the bolus
What People Are Saying
Happy Customers
An individual was already 2 weeks into their treatment plan and the clinic was struggling with the time required to fabricate the device using standard sheet bolus. Since the patient was already undergoing treatment, we wanted to make the bolus as fast as possible. Using Adaptiiv’s software solution we were able to print the entire bolus overnight, ensuring it was ready for the next day’s treatment.
Since the patient was already undergoing treatment, we wanted to make the bolus as fast as possible. Using Adaptiiv’s software solution we were able to print the entire bolus overnight, ensuring it was ready for the next day’s treatment.
Brian Overshiner
Staff Radiation Therapist
Indiana University School of Medicine
We're Here For You
Every customer is encouraged to provide insight and feedback about our software to help influence our product road map. A dedicated team of software engineers, developers, and medical physicists can take your ideas, prototype them, and quickly turn them into reality.
How We Support Our Customers
We help every customer leverage our world-class product to achieve their desired clinical outcomes so they are more successful.
1
Identify key customer expectations
Every customer will approve their own plan
2
Map out processes to meet customer expectations
Establish path to success in advance
3
Define metrics for each expectation
Establish realistic and measurable metrics
4
Quantify a goal
Establish realistic goals to help assess performance
5
Assign responsibility
A dedicated individual (or team) will support every customer
6
Establish a schedule
We will ensure you stay on track
The Clinical Application of 3D-Printed Boluses in Superficial Tumor Radiotherapy
1. Fontenla DP, Napoli JJ, Hunt M, Fass D, McCormick B, Kutcher GJ. Effects of Beam Modifiers and Immobilization Devices on the Dose in the Build-Up Region. Int J Radiat Oncol Biol Phys (1994) 30(1):211–9. 10.1016/0360-3016(94)90537-1 [PubMed] [CrossRef] [Google Scholar]
Fontenla DP, Napoli JJ, Hunt M, Fass D, McCormick B, Kutcher GJ. Effects of Beam Modifiers and Immobilization Devices on the Dose in the Build-Up Region. Int J Radiat Oncol Biol Phys (1994) 30(1):211–9. 10.1016/0360-3016(94)90537-1 [PubMed] [CrossRef] [Google Scholar]
2. Mellenberg DE. Dose Behind Various Immobilization and Beam-Modifying Devices. Int J Radiat Oncol (1995) 32(4):1193–7. 10.1016/0360-3016(94)00371-Q [PubMed] [CrossRef] [Google Scholar]
3. Niroomand-Rad A, Javedan K, Rodgers JE, Harter KW. Effects of Beam Spoiler on Radiation Dose for Head and Neck Irradiation With 10-MV Photon Beam. Int J Radiat Oncol Biol Phys (1997) 37(4):935–40. 10.1016/s0360-3016(96)00538-x [PubMed] [CrossRef] [Google Scholar]
4. Hou Y, Song Y, Sun X, Jiang Y, He M, Li Y, et al.. Multifunctional Composite Hydrogel Bolus With Combined Self-Healing, Antibacterial and Adhesive Functions for Radiotherapy. J Mater Chem B (2020) 8(13):2627–35. 10.1039/c9tb02967b [PubMed] [CrossRef] [Google Scholar]
5. Dogan N, Glasgow GP. Surface and Build-Up Region Dosimetry for Obliquely Incident Intensity Modulated Radiotherapy 6 MV X Rays. Med Phys (2003) 30(12):3091–6. 10.1118/1.1625116 [PubMed] [CrossRef] [Google Scholar]
Dogan N, Glasgow GP. Surface and Build-Up Region Dosimetry for Obliquely Incident Intensity Modulated Radiotherapy 6 MV X Rays. Med Phys (2003) 30(12):3091–6. 10.1118/1.1625116 [PubMed] [CrossRef] [Google Scholar]
6. Xiang HF, Song JS, Chin DW, Cormack RA, Tishler RB, Makrigiorgos GM, et al.. Build-Up and Surface Dose Measurements on Phantoms Using Micro-MOSFET in 6 and 10 MV X-Ray Beams and Comparisons With Monte Carlo Calculations. Med Phys (2007) 34(4):1266–73. 10.1118/1.2710951 [PubMed] [CrossRef] [Google Scholar]
7. Turner JY, Zeniou A, Williams A, Jyothirmayi R. Technique and Outcome of Post-Mastectomy Adjuvant Chest Wall Radiotherapy-The Role of Tissue-Equivalent Bolus in Reducing Risk of Local Recurrence. Br J Radiol (2016) 89(1064):20160060. 10.1259/bjr.20160060 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Dias AG, Pinto DFS, Borges MF, Pereira MH, Santos JAM, Cunha LT, et al.. Optimization of Skin Dose Using In-Vivo MOSFET Dose Measurements in Bolus/Non-Bolus Fraction Ratio: A VMAT and a 3DCRT Study.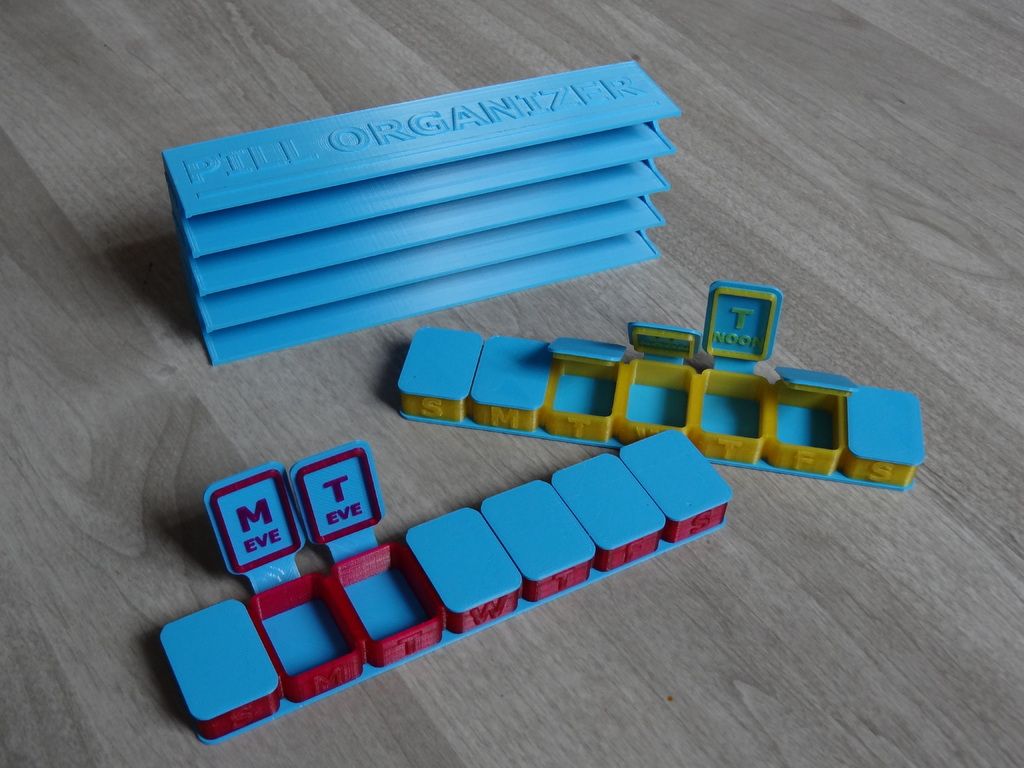 J Appl Clin Med Phys (2019) 20(2):63–70. 10.1002/acm2.12525 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J Appl Clin Med Phys (2019) 20(2):63–70. 10.1002/acm2.12525 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
9. Boman E, Ojala J, Rossi M, Kapanen M. Monte Carlo Investigation on the Effect of Air Gap Under Bolus in Post-Mastectomy Radiotherapy. Phys Med (2018) 55:82–7. 10.1016/j.ejmp.2018.10.023 [PubMed] [CrossRef] [Google Scholar]
10. Michiels S, Barragan AM, Souris K, Poels K, Crijns W, Lee JA, et al.. Patient-Specific Bolus for Range Shifter Air Gap Reduction in Intensity-Modulated Proton Therapy of Head-and-Neck Cancer Studied With Monte Carlo Based Plan Optimization. Radiother Oncol (2018) 128(1):161–6. 10.1016/j.radonc.2017.09.006 [PubMed] [CrossRef] [Google Scholar]
11. Zastrow M. 3D Printing Gets Bigger, Faster and Stronger. Nature (2020) 578(7793):20–3. 10.1038/d41586-020-00271-6 [PubMed] [CrossRef] [Google Scholar]
12. Attaran M. The Rise of 3-D Printing: The Advantages of Additive Manufacturing Over Traditional Manufacturing. Bus Horiz (2017) 60(5):677–88. 10.1016/j.bushor.2017.05.011 [CrossRef] [Google Scholar]
10.1016/j.bushor.2017.05.011 [CrossRef] [Google Scholar]
13. Tejo-Otero A, Buj-Corral I, Fenollosa-Artes F. 3D Printing in Medicine for Preoperative Surgical Planning: A Review. Ann BioMed Eng (2020) 48(2):536–55. 10.1007/s10439-019-02411-0 [PubMed] [CrossRef] [Google Scholar]
14. Murphy SV, De Coppi P, Atala A. Opportunities and Challenges of Translational 3D Bioprinting. Nat BioMed Eng (2020) 4(4):370–80. 10.1038/s41551-019-0471-7 [PubMed] [CrossRef] [Google Scholar]
15. Sun Z. Clinical Applications of Patient-Specific 3d Printed Models in Cardiovascular Disease: Current Status and Future Directions. Biomolecules (2020) 10(11):1–34. 10.3390/biom10111577 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Breitkreutz DY, Bialek S, Vojnovic B, Kavanagh A, Johnstone CD, Rovner Z, et al.. A 3D Printed Modular Phantom for Quality Assurance of Image-Guided Small Animal Irradiators: Design, Imaging Experiments, and Monte Carlo Simulations. Med Phys (2019) 46(5):2015–24. 10.1002/mp.13525 [PubMed] [CrossRef] [Google Scholar]
10.1002/mp.13525 [PubMed] [CrossRef] [Google Scholar]
17. Ji Z, Jiang Y, Guo F, Peng R, Sun H, Fan J, et al.. Safety and Efficacy of CT-Guided Radioactive Iodine-125 Seed Implantation Assisted by a 3D Printing Template for the Treatment of Thoracic Malignancies. J Cancer Res Clin Oncol (2020) 146(1):229–36. 10.1007/s00432-019-03050-7 [PubMed] [CrossRef] [Google Scholar]
18. Pablo-Navarro J, Sangiao S, Magen C, de Teresa JM. Diameter Modulation of 3D Nanostructures in Focused Electron Beam Induced Deposition Using Local Electric Fields and Beam Defocus. Nanotechnology (2019) 30(50):505302. 10.1088/1361-6528/ab423c [PubMed] [CrossRef] [Google Scholar]
19. Rooney MK, Rosenberg DM, Braunstein S, Cunha A, Damato AL, Ehler E, et al.. Three-Dimensional Printing in Radiation Oncology: A Systematic Review of the Literature. J Appl Clin Med Phys (2020) 21(8):15–26. 10.1002/acm2.12907 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
20. Canters RA, Lips IM, Wendling M, Kusters M, van Zeeland M, Gerritsen RM, et al. . Clinical Implementation of 3D Printing in the Construction of Patient Specific Bolus for Electron Beam Radiotherapy for Non-Melanoma Skin Cancer. Radiother Oncol (2016) 121(1):148–53. 10.1016/j.radonc.2016.07.011 [PubMed] [CrossRef] [Google Scholar]
. Clinical Implementation of 3D Printing in the Construction of Patient Specific Bolus for Electron Beam Radiotherapy for Non-Melanoma Skin Cancer. Radiother Oncol (2016) 121(1):148–53. 10.1016/j.radonc.2016.07.011 [PubMed] [CrossRef] [Google Scholar]
21. Kang D, Wang B, Peng Y, Liu X, Deng X. Low-Cost Iphone-Assisted Processing to Obtain Radiotherapy Bolus Using Optical Surface Reconstruction and 3D-Printing. Sci Rep (2020) 10(1):8016. 10.1038/s41598-020-64967-5 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Albantow C, Hargrave C, Brown A, Halsall C. Comparison of 3D Printed Nose Bolus to Traditional Wax Bolus for Cost-Effectiveness, Volumetric Accuracy and Dosimetric Effect. J Med Radiat Sci (2020) 67(1):54–63. 10.1002/jmrs.378 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Baltz GC, Chi PM, Wong PF, Wang C, Craft DF, Kry SF, et al.. Development and Validation of a 3D-Printed Bolus Cap for Total Scalp Irradiation. J Appl Clin Med Phys (2019) 20(3):89–96. 10.1002/acm2.12552 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10.1002/acm2.12552 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Dai G, Xu X, Wu X, Lei X, Wei X, Li Z, et al.. Application of 3D-Print Silica Bolus for Nasal NK/T-Cell Lymphoma Radiation Therapy. J Radiat Res (2020) 61(6):920–8. 10.1093/jrr/rraa084 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
25. Robar JL, Moran K, Allan J, Clancey J, Joseph T, Chytyk-Praznik K, et al.. Intrapatient Study Comparing 3D Printed Bolus Versus Standard Vinyl Gel Sheet Bolus for Postmastectomy Chest Wall Radiation Therapy. Pract Radiat Oncol (2018) 8(4):221–9. 10.1016/j.prro.2017.12.008 [PubMed] [CrossRef] [Google Scholar]
26. Park JM, Son J, An HJ, Kim JH, Wu HG, Kim JI. Bio-Compatible Patient-Specific Elastic Bolus for Clinical Implementation. Phys Med Biol (2019) 64(10):105006. 10.1088/1361-6560/ab1c93 [PubMed] [CrossRef] [Google Scholar]
27. Kong Y, Yan T, Sun Y, Qian J, Zhou G, Cai S, et al.. A Dosimetric Study on the Use of 3D-Printed Customized Boluses in Photon Therapy: A Hydrogel and Silica Gel Study. J Appl Clin Med Phys (2019) 20(1):348–55. 10.1002/acm2.12489 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J Appl Clin Med Phys (2019) 20(1):348–55. 10.1002/acm2.12489 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Hou YJ, Yu JP, Wang YQ, Liu HR, Li D, Xu JJ, et al.. Fabrication and Pre-Clinical Application of Patient-Specific 3D Silicone Rubber Bolus for Chest Wall. Chin J Radiat Oncol (2018) 27(9):835–8. 10.3760/cma.j.issn.1004-4221.2018.09.010 [CrossRef] [Google Scholar]
29. Park SY, Choi CH, Park JM, Chun M, Han JH, Kim JI. A Patient-Specific Polylactic Acid Bolus Made by a 3D Printer for Breast Cancer Radiation Therapy. PloS One (2016) 11(12):e0168063. 10.1371/journal.pone.0168063 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
30. Park K, Park S, Jeon MJ, Choi J, Kim JW, Cho YJ, et al.. Clinical Application of 3D-Printed-Step-Bolus in Post-Total-Mastectomy Electron Conformal Therapy. Oncotarget (2017) 8(15):25660–8. 10.18632/oncotarget.12829 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Craft DF, Kry SF, Balter P, Salehpour M, Woodward W, Howell RM. Material Matters: Analysis of Density Uncertainty in 3D Printing and Its Consequences for Radiation Oncology. Med Phys (2018) 45(4):1614–21. 10.1002/mp.12839 [PubMed] [CrossRef] [Google Scholar]
Material Matters: Analysis of Density Uncertainty in 3D Printing and Its Consequences for Radiation Oncology. Med Phys (2018) 45(4):1614–21. 10.1002/mp.12839 [PubMed] [CrossRef] [Google Scholar]
32. Hou Y, Song Y, Sun X, Jiang Y, He M, Li Y, et al.. Multifunctional Composite Hydrogel Bolus With Combined Self-Healing, Antibacterial and Adhesive Functions for Radiotherapy. J Mater Chem B (2020) 8(13):2627–35. 10.1039/c9tb02967b [PubMed] [CrossRef] [Google Scholar]
33. Su S, Moran K, Robar JL. Design and Production of 3D Printed Bolus for Electron Radiation Therapy. J Appl Clin Med Phys (2014) 15(4):4831. 10.1120/jacmp.v15i4.4831 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
34. Burleson S, Baker J, Hsia AT, Xu Z. Use of 3D Printers to Create a Patient-Specific 3D Bolus for External Beam Therapy. J Appl Clin Med Phys (2015) 16(3):5247. 10.1120/jacmp.v16i3.5247 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Ricotti R, Ciardo D, Pansini F, Bazani A, Comi S, Spoto R, et al.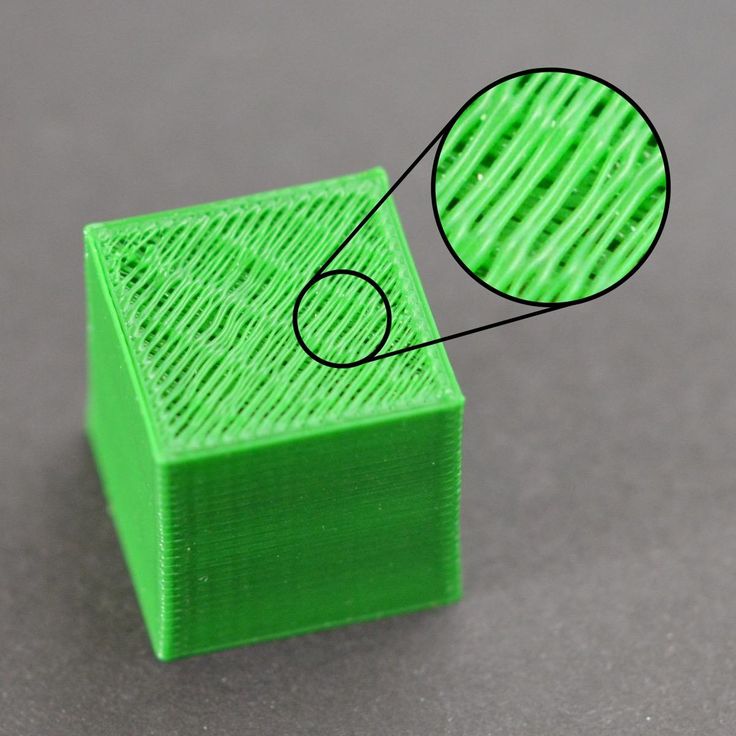 . Dosimetric Characterization of 3D Printed Bolus at Different Infill Percentage for External Photon Beam Radiotherapy. Phys Med (2017) 39:25–32. 10.1016/j.ejmp.2017.06.004 [PubMed] [CrossRef] [Google Scholar]
. Dosimetric Characterization of 3D Printed Bolus at Different Infill Percentage for External Photon Beam Radiotherapy. Phys Med (2017) 39:25–32. 10.1016/j.ejmp.2017.06.004 [PubMed] [CrossRef] [Google Scholar]
36. Kim SW, Shin HJ, Kay CS, Son SH. A Customized Bolus Produced Using a 3-Dimensional Printer for Radiotherapy. PloS One (2014) 9(10):e110746. 10.1371/journal.pone.0110746 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
37. Park JW, Yea JW. Three-Dimensional Customized Bolus for Intensity-Modulated Radiotherapy in a Patient With Kimura’s Disease Involving the Auricle. Cancer Radiother (2016) 20(3):205–9. 10.1016/j.canrad.2015.11.003 [PubMed] [CrossRef] [Google Scholar]
38. Zhao Y, Moran K, Yewondwossen M, Allan J, Clarke S, Rajaraman M, et al.. Clinical Applications of 3-Dimensional Printing in Radiation Therapy. Med Dosim (2017) 42(2):150–5. 10.1016/j.meddos.2017.03.001 [PubMed] [CrossRef] [Google Scholar]
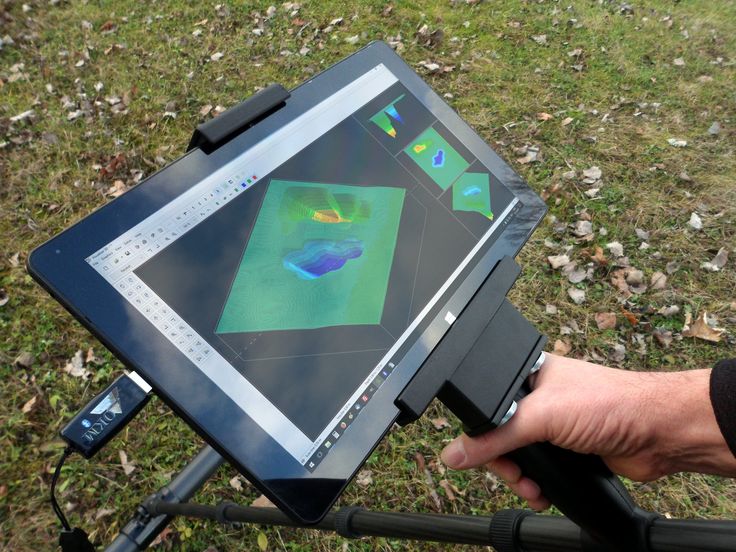
39. Park JW, Oh SA, Yea JW, Kang MK. Fabrication of Malleable Three-Dimensional-Printed Customized Bolus Using Three-Dimensional Scanner. PloS One (2017) 12(5):e0177562. 10.1371/journal.pone.0177562 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Fabrication of Malleable Three-Dimensional-Printed Customized Bolus Using Three-Dimensional Scanner. PloS One (2017) 12(5):e0177562. 10.1371/journal.pone.0177562 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Chiu T, Tan J, Brenner M, Gu X, Yang M, Westover K, et al.. Three-Dimensional Printer-Aided Casting of Soft, Custom Silicone Boluses (SCSBs) for Head and Neck Radiation Therapy. Pract Radiat Oncol (2018) 8(3):e167–74. 10.1016/j.prro.2017.11.001 [PubMed] [CrossRef] [Google Scholar]
41. Zou W, Fisher T, Zhang M, Kim L, Chen T, Narra V, et al.. Potential of 3D Printing Technologies for Fabrication of Electron Bolus and Proton Compensators. J Appl Clin Med Phys (2015) 16(3):4959. 10.1120/jacmp.v16i3.4959 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Zhang M, Zhao B, Yin JP, Liu S, Gao X, Qin S, et al.. Application of New Three-Dimensional Printed Tissue Compensators in Radiotherapy. Chin J Radiat Oncol (2017) 26(2):210–4. 10.3760/cma.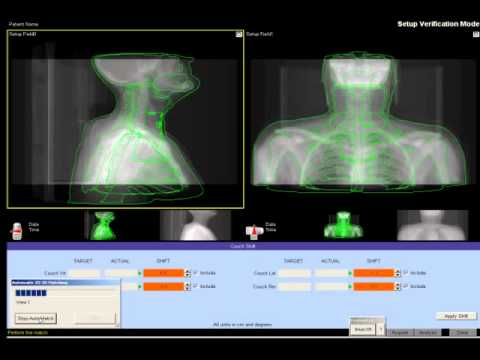 j.issn.1004-4221.2017.02.018 [CrossRef] [Google Scholar]
j.issn.1004-4221.2017.02.018 [CrossRef] [Google Scholar]
43. Butson MJ, Cheung T, Yu P, Metcalfe P. Effects on Skin Dose From Unwanted Air Gaps Under Bolus in Photon Beam Radiotherapy. Radiat Meas (2000) 32(3):201–4. 10.1016/S1350-4487(99)00276-0 [CrossRef] [Google Scholar]
44. Lukowiak M, Jezierska K, Boehlke M, Wiecko M, Lukowiak A, Podraza W, et al.. Utilization of a 3D Printer to Fabricate Boluses Used for Electron Therapy of Skin Lesions of the Eye Canthi. J Appl Clin Med Phys (2017) 18(1):76–81. 10.1002/acm2.12013 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
45. Hymes SR, Strom EA, Fife C. Radiation Dermatitis: Clinical Presentation, Pathophysiology, and Treatment 2006. J Am Acad Dermatol (2006) 54(1):28–46. 10.1016/j.jaad.2005.08.054 [PubMed] [CrossRef] [Google Scholar]
46. Bray FN, Simmons BJ, Wolfson AH, Nouri K. Acute and Chronic Cutaneous Reactions to Ionizing Radiation Therapy. Dermatol Ther (Heidelb) (2016) 6(2):185–206. 10.1007/s13555-016-0120-y [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Mendelsohn FA, Divino CM, Reis ED, Kerstein MD. Wound Care After Radiation Therapy. Adv Skin Wound Care (2002) 15(5):216–24. 10.1097/00129334-200209000-00007 [PubMed] [CrossRef] [Google Scholar]
Mendelsohn FA, Divino CM, Reis ED, Kerstein MD. Wound Care After Radiation Therapy. Adv Skin Wound Care (2002) 15(5):216–24. 10.1097/00129334-200209000-00007 [PubMed] [CrossRef] [Google Scholar]
48. Andic F, Ors Y, Davutoglu R, Baz Cifci S, Ispir EB, Erturk ME. Evaluation of Skin Dose Associated With Different Frequencies of Bolus Applications in Post-Mastectomy Three-Dimensional Conformal Radiotherapy. J Exp Clin Cancer Res (2009) 28:41. 10.1186/1756-9966-28-41 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
49. Lee N, Chuang C, Quivey JM, Phillips TL, Akazawa P, Verhey LJ, et al.. Skin Toxicity Due to Intensity-Modulated Radiotherapy for Head-and-Neck Carcinoma. Int J Radiat Oncol (2002) 53(3):630–7. 10.1016/S0360-3016(02)02756-6 [PubMed] [CrossRef] [Google Scholar]
50. Tieu MT, Graham P, Browne L, Chin YS. The Effect of Adjuvant Postmastectomy Radiotherapy Bolus Technique on Local Recurrence. Int J Radiat Oncol Biol Phys (2011) 81(3):e165–71. 10. 1016/j.ijrobp.2011.01.002 [PubMed] [CrossRef] [Google Scholar]
1016/j.ijrobp.2011.01.002 [PubMed] [CrossRef] [Google Scholar]
51. Pignol JP, Vu TT, Mitera G, Bosnic S, Verkooijen HM, Truong P. Prospective Evaluation of Severe Skin Toxicity and Pain During Postmastectomy Radiation Therapy. Int J Radiat Oncol Biol Phys (2015) 91(1):157–64. 10.1016/j.ijrobp.2014.09.022 [PubMed] [CrossRef] [Google Scholar]
52. Herst PM. Protecting the Radiation-Damaged Skin From Friction: A Mini Review. J Med Radiat Sci (2014) 61(2):119–25. 10.1002/jmrs.46 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
53. Pignol JP, Olivotto I, Rakovitch E, Gardner S, Sixel K, Beckham W, et al.. A Multicenter Randomized Trial of Breast Intensity-Modulated Radiation Therapy to Reduce Acute Radiation Dermatitis. J Clin Oncol (2008) 26(13):2085–92. 10.1200/JCO.2007.15.2488 [PubMed] [CrossRef] [Google Scholar]
54. Arenas M, Sabater S, Sintas A, Arguis M, Hernandez V, Arquez M, et al.. Individualized 3D Scanning and Printing for Non-Melanoma Skin Cancer Brachytherapy: A Financial Study for Its Integration Into Clinical Workflow.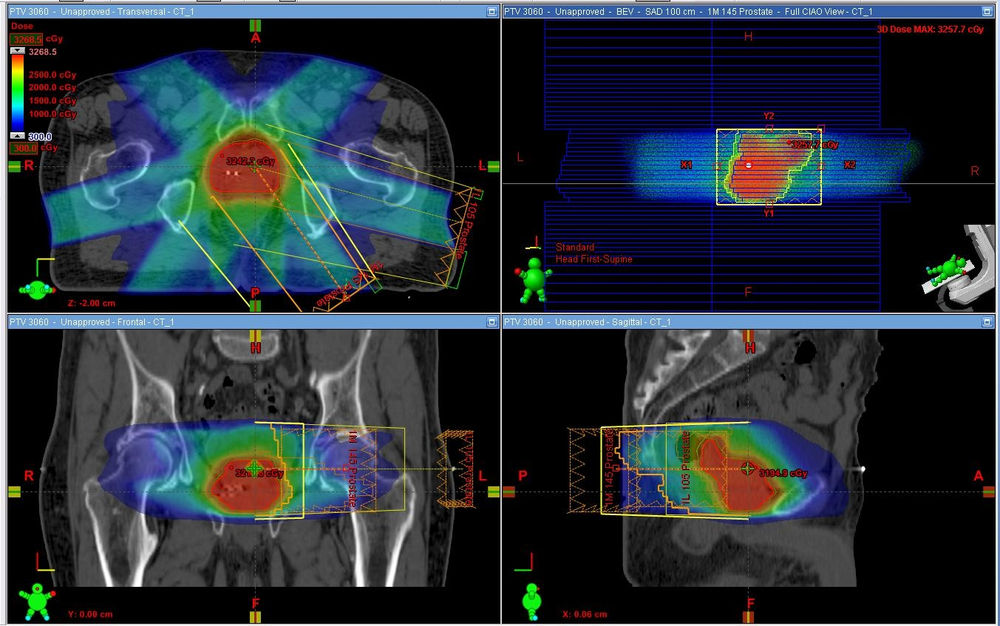 J Contemp Brachytherapy (2017) 9(3):270–6. 10.5114/jcb.2017.68134 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J Contemp Brachytherapy (2017) 9(3):270–6. 10.5114/jcb.2017.68134 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3D printing devices for radiation therapy using SLA technology
Application
Subscribe to the author
Subscribe
I do not want
1
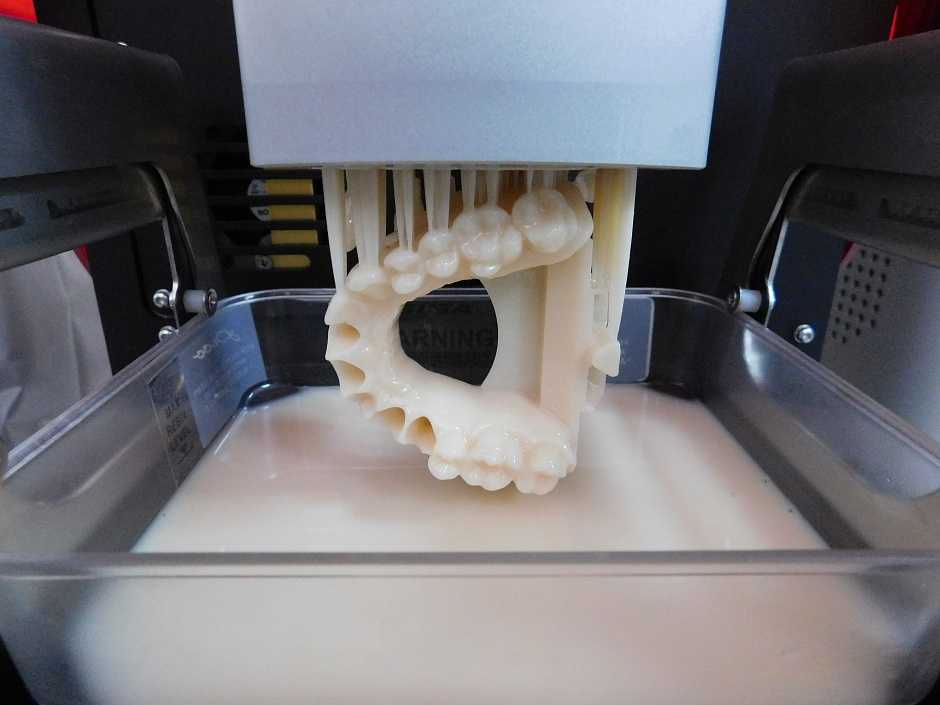
Bolus devices printed using the BIOMED CLEAR RESIN and BIREMD AMBER RSSIN.
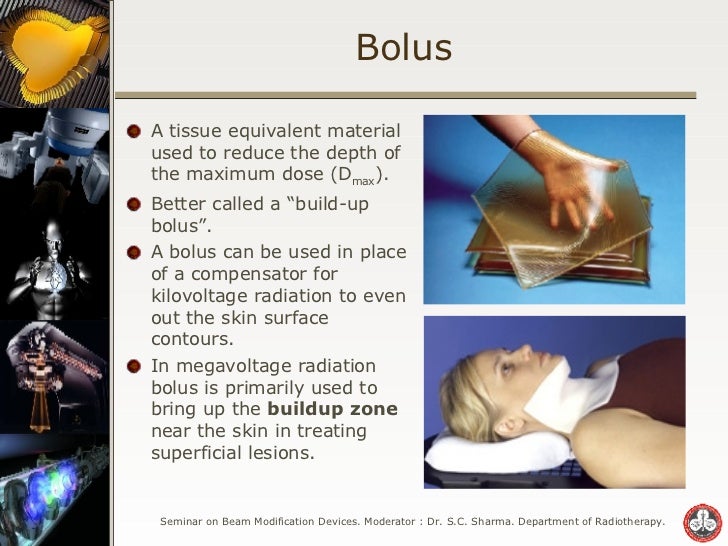
Cancer is one of the leading causes of death worldwide. Over time, doctors are increasingly turning to radiation therapy as a powerful means of fighting cancer and saving the lives of patients. However, radiation is toxic and dangerous if misused. Bolus materials are used to deliver targeted radiation doses to the affected superficial layers of the skin, helping medical professionals precisely control the dose of radiation to cancerous tissue while limiting the unwanted effects of radiation on healthy tissues.
With 3D printing rapidly gaining momentum in the hospital setting, it's worth asking if it's possible to 3D print a skin-friendly bolus that also fits the patient's unique anatomy.
The answer is definitely yes. Printed boluses are not only safe and accurate, they are in fact already being produced and used in hospitals around the world.
Formlabs recently invited Greg Gagnon, 3D Printer at Baystate Health, and Borko Basaryk, Senior Product Manager at Adaptiiv Medical Technologies Inc, to review the current state of bolus device 3D printing.
Printed bolus devices: problems and solutions
3D printed bolus with visible channels. The transparency of BioMed Amber Resin allows for improved device accuracy with excellent dose distribution of .
Conventional therapies present a range of challenges for healthcare professionals. This can worsen the patient's condition and lead to a decrease in the effectiveness of radiation therapy.
Some of the problems with how bolus devices are currently made are:
- The patient preparation procedure is quite complex and time consuming.
- Impossibility of adaptation or correction of anatomical disorders.

- Air gaps between accessory and skin may result in underdose.
- Manual production can be labor intensive and produce unpredictable results.
- The bolus must be formed and secured in place at each visit.
- Lack of qualified personnel who can create accessories.
- Materials such as the Freiburg patch can be expensive.
Traditional patient bolus sets can be rough, can take days to create, and involve hot wax and mesh over the face. They also require constant checks to make sure the radiant tubes are properly aligned. In addition, the traditional process requires highly skilled personnel trained in the use of bolus devices. This moment is exacerbated by the recent shortage of personnel in the United States, which is forcing hospitals to look for new methods of applying radiation therapy.
The solution to these problems is the in-house production of bolus devices using 3D printing. "Our goal is to create an applicator that fits the patient perfectly" says Basaryk.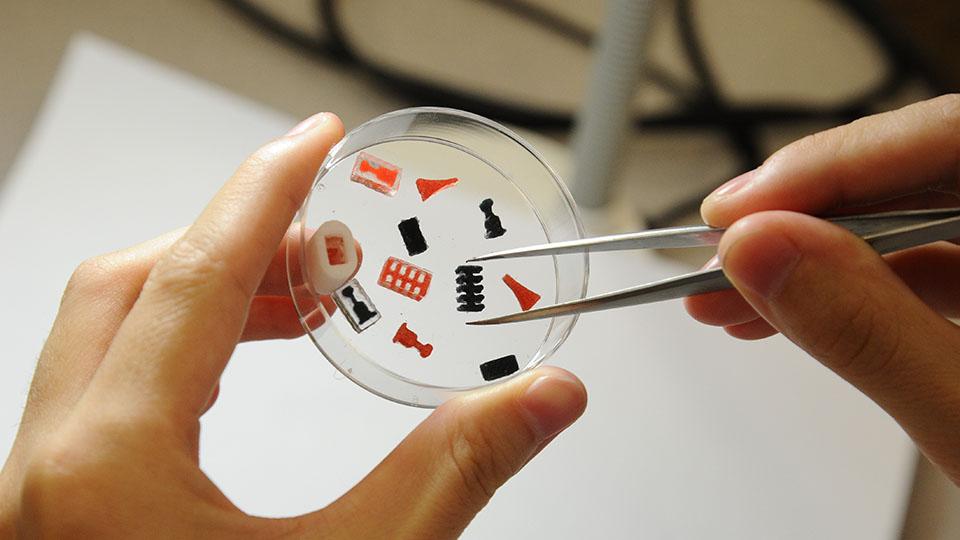 Although this has always been the goal of medical professionals, before the advent of their own 3D printers, this was simply not possible.
Although this has always been the goal of medical professionals, before the advent of their own 3D printers, this was simply not possible.
By using 3D printers to create bolus devices, hospitals benefit from:
- Patient-specific devices and eliminating manual device creation
- Improved device accuracy with superior dose distribution
- Various trajectory settings
- Wider staff capable of producing devices
- Less time required to design, manufacture and set up
- Reduce costs through significant cost savings.
Baystate Health, the largest hospital system in western Massachusetts, has made great strides by moving to 3D printed bolus devices. Gagnon told us that "Because our hospital has set up a shared portal to receive a patient file, I can produce a part in 24 hours. I usually request extra time, but sometimes it only takes eight hours to print. I can send a file from home to a printer in the office, and When I get to work, everything is ready. "
"
Ease of use was noted and Gagnon said: “The 3D printing process is very simple, we print the bolus device right on the platform. The resolution of 3D printing is so good that you don't need support within the channels."
While this workflow can be used with FDM 3D printers, SLA will provide more consistent printing across the entire device, never leaving gaps or air pockets in the print. Gagnon often turns to Clear Resin for his devices. Clear Resin is polished to near optical clarity, making it ideal for displaying interiors where tubes need to be placed.
FDM and SLA 3D printing for brachytherapy
Bolus devices can be 3D printed with FDM or SLA printers. So what's the difference?
- Fused Deposition Printing (FDM), also known as FFF, is the most widely used type of 3D printing at the consumer level. FDM 3D printers work by extruding thermoplastic filaments such as ABS (acrylonitrile butadiene styrene), PLA (polylactic acid) through a heated nozzle, melting the material and depositing the plastic layer by layer until the entire model is printed.

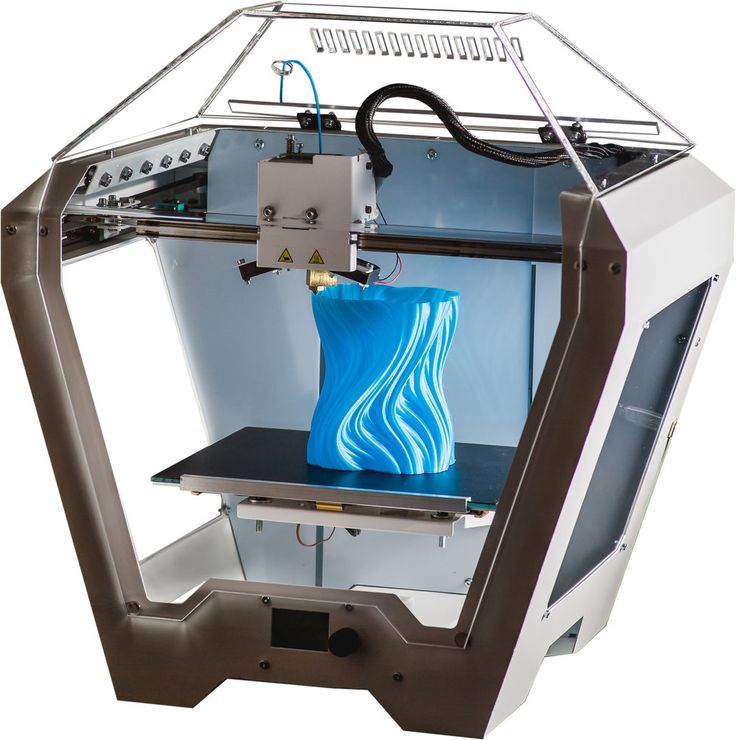
- Stereolithographic (SLA) 3D printers use a laser to cure liquid resin into hardened plastic in a process called photopolymerization. SLA 3D printers and resins have become extremely popular due to their ability to produce highly accurate, isotropic and waterproof prototypes and parts from a range of advanced materials with excellent performance and smooth surfaces. SLA 3D printing resin formulations have a wide range of optical, mechanical, and thermal properties that match those of standard, engineering, and industrial thermoplastics.
Learn more: Brachytherapy Case Study
You can access the full video featuring Greg Gagnon, 3D Printer at Baystate Health, and Adaptiiv Medical Technologies Inc Senior Product Manager Borko Basaryk at the link below ( part of the User Summit 2022 event archive). Here you can see a complete case study performed on an 80 year old male patient with bilateral tibial BCC. Gagnon also gives advice to hospital staff looking to make the case for 3D printing investments and talks about his workflow for creating bolus devices.
Watch
We will keep you updated!
Your iGo3D Russia team :)
Our groups in social networks:
Telegram
VKontakte
YouTube
The Korea Institute of Radiological and Medical Sciences uses a Pro2 Plus professional 3D printer with a dual extruder in their laboratory. The team, led by Dr. Jonah Choi, uses Pro2 Plus to manufacture several radiotherapy aids.
Reliable source of treatment tools
Traditional boluses (material to modify the penetration depth of irradiation), materials and technologies do not correspond to the exact anatomy of a particular patient. This results in air gaps between the patient and the bolus, which can reduce the amount of radiation absorbed by the patient's skin, ultimately reducing the effectiveness of therapy.
The Korea Institute of Radiological and Medical Sciences has implemented an application to create a 3D printed irradiation bolus tailored to the anatomy and geometry of each patient. This technology ensures that the bolus fits snugly against the skin without an air gap between them.
This technology ensures that the bolus fits snugly against the skin without an air gap between them.
In addition, the lab can print an exact replica of the patient's body part as a model for treatment planning. This ability to print any shape allows the team to create models that are hollow inside. Traditional tools often do not allow you to give the part the desired shape. In these cases, 3D printing helps a lot. This method of prototyping is fast and very convenient.
The stable and accurate performance of the Pro2 Plus allows you to print large boluses and visual models for accurate treatment. The quality of wearing by patients is improved. The Pro2 Plus' 60cm build area allows these models to be built in one go and saves John's team a lot of time, including joining parts.
Rapid experiments with material to create anti-radiation masks
Dr. John's team is investigating the effects of radiation on the experimental material to see if it can be used to make radiation masks.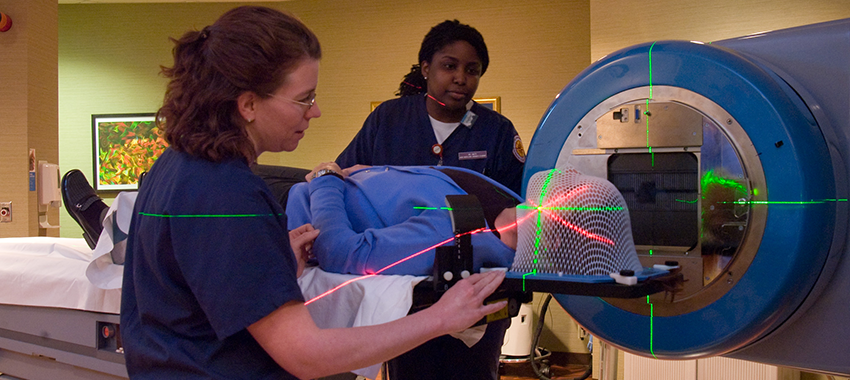 Such materials are expensive and difficult to process. Dr. Jonah decided to model them from a 3D printable material with the same density. The printed samples will be subjected to computed tomography, the electron density and homogeneity will be determined. Raise3D Pro2 Plus' high heating temperature allows the team to experiment with a wide variety of materials.
Such materials are expensive and difficult to process. Dr. Jonah decided to model them from a 3D printable material with the same density. The printed samples will be subjected to computed tomography, the electron density and homogeneity will be determined. Raise3D Pro2 Plus' high heating temperature allows the team to experiment with a wide variety of materials.
Advanced Research Opportunities
The Raise3D software, ideaMaker, allows you to create experimental models on the Pro2 Plus that can simulate many different levels of high detail and precision. For example, the ability to print part of the model allows you to determine the desired degree of infill or density of the object.
Future
Dr. John Choi's team is a classic example of 3D printing in radiation medicine. In addition, she saw even more value in the technology for expanding the use of certain materials. The team sees the next development step in the printing of flexible and metal models.