Surgery 3d printing
The clinical use of 3D printing in surgery
Review
. 2018 Sep;70(3):381-388.
doi: 10.1007/s13304-018-0586-5. Epub 2018 Aug 30.
Luigi Pugliese 1 , Stefania Marconi 2 , Erika Negrello 2 , Valeria Mauri 2 , Andrea Peri 3 , Virginia Gallo 3 , Ferdinando Auricchio 2 , Andrea Pietrabissa 3
Affiliations
Affiliations
- 1 Department of Surgery, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
[email protected].
- 2 Department of Civil Engineering and Architecture, University of Pavia, Pavia, Italy.
- 3 Department of Surgery, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
- PMID: 30167991
- DOI: 10.1007/s13304-018-0586-5
Review
Luigi Pugliese et al. Updates Surg. 2018 Sep.
. 2018 Sep;70(3):381-388.
doi: 10.1007/s13304-018-0586-5. Epub 2018 Aug 30.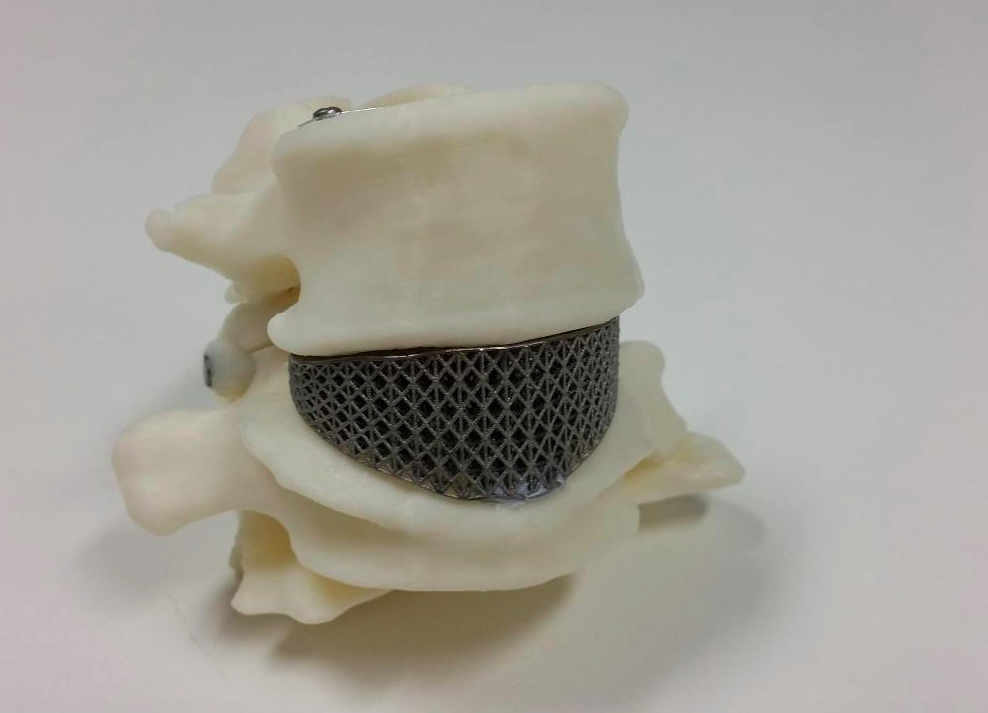
Authors
Luigi Pugliese 1 , Stefania Marconi 2 , Erika Negrello 2 , Valeria Mauri 2 , Andrea Peri 3 , Virginia Gallo 3 , Ferdinando Auricchio 2 , Andrea Pietrabissa 3
Affiliations
- 1 Department of Surgery, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy. [email protected].
- 2 Department of Civil Engineering and Architecture, University of Pavia, Pavia, Italy.
- 3 Department of Surgery, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.

- PMID: 30167991
- DOI: 10.1007/s13304-018-0586-5
Abstract
The use of 3D printing is gaining considerable success in many medical fields including surgery. Here, the technology was introduced for increasing the level of anatomical understanding thanks to the inherent characteristics of 3D printed models: these are highly accurate and customized reproductions, being obtained from own radiological imaging of patients, and are solid graspable objects allowing for free manipulation on part of the user. The resulting tactile feedbacks significantly help the comprehension of anatomical details, especially the spatial relations between structures. In this regard, they proved to be more effective than conventional 2D imaging and 3D virtual models. To date, an increasing number of applications have been successfully tested in many surgical disciplines, extending the range of possible uses to pre-operative planning, counselling with patients, education of students and residents, surgical training, intraoperative navigation and others; in recent years, 3D printing was also employed for creating surgical tools and reproducing anatomical parts to be used, respectively, as templates or guides for specific tasks of the surgery and individualized implantable materials in reconstructive procedures. Future expectations concern on one side the reduction of manufacturing costs and time to further increase the accessibility of 3D printing, while on the other the development of novel techniques and materials suitable for 3D printing of biological structures by which recreating the architecture and functionality of real human organs and tissues.
To date, an increasing number of applications have been successfully tested in many surgical disciplines, extending the range of possible uses to pre-operative planning, counselling with patients, education of students and residents, surgical training, intraoperative navigation and others; in recent years, 3D printing was also employed for creating surgical tools and reproducing anatomical parts to be used, respectively, as templates or guides for specific tasks of the surgery and individualized implantable materials in reconstructive procedures. Future expectations concern on one side the reduction of manufacturing costs and time to further increase the accessibility of 3D printing, while on the other the development of novel techniques and materials suitable for 3D printing of biological structures by which recreating the architecture and functionality of real human organs and tissues.
Keywords: 3D printing; Anatomy; Model; Surgery; Technology.
Similar articles
-
Value of 3D printing for the comprehension of surgical anatomy.
Marconi S, Pugliese L, Botti M, Peri A, Cavazzi E, Latteri S, Auricchio F, Pietrabissa A. Marconi S, et al. Surg Endosc. 2017 Oct;31(10):4102-4110. doi: 10.1007/s00464-017-5457-5. Epub 2017 Mar 9. Surg Endosc. 2017. PMID: 28281114
-
3D-printing techniques in a medical setting: a systematic literature review.
Tack P, Victor J, Gemmel P, Annemans L. Tack P, et al. Biomed Eng Online. 2016 Oct 21;15(1):115. doi: 10.1186/s12938-016-0236-4. Biomed Eng Online. 2016. PMID: 27769304 Free PMC article. Review.
-
Current Use of Three-dimensional Model Technology in Urology: A Road Map for Personalised Surgical Planning.

Porpiglia F, Amparore D, Checcucci E, Autorino R, Manfredi M, Iannizzi G, Fiori C; for ESUT Research Group. Porpiglia F, et al. Eur Urol Focus. 2018 Sep;4(5):652-656. doi: 10.1016/j.euf.2018.09.012. Epub 2018 Oct 4. Eur Urol Focus. 2018. PMID: 30293946 Review.
-
Three-dimensional Printing and Augmented Reality: Enhanced Precision for Robotic Assisted Partial Nephrectomy.
Wake N, Bjurlin MA, Rostami P, Chandarana H, Huang WC. Wake N, et al. Urology. 2018 Jun;116:227-228. doi: 10.1016/j.urology.2017.12.038. Epub 2018 May 22. Urology. 2018. PMID: 29801927
-
Creation of a novel simulator for minimally invasive neurosurgery: fusion of 3D printing and special effects.
Weinstock P, Rehder R, Prabhu SP, Forbes PW, Roussin CJ, Cohen AR.
 Weinstock P, et al. J Neurosurg Pediatr. 2017 Jul;20(1):1-9. doi: 10.3171/2017.1.PEDS16568. Epub 2017 Apr 25. J Neurosurg Pediatr. 2017. PMID: 28438070
Weinstock P, et al. J Neurosurg Pediatr. 2017 Jul;20(1):1-9. doi: 10.3171/2017.1.PEDS16568. Epub 2017 Apr 25. J Neurosurg Pediatr. 2017. PMID: 28438070
See all similar articles
Cited by
-
Additive Fabrication of a Vascular 3D Phantom for Stereotactic Radiosurgery of Arteriovenous Malformations.
Legnani E, Gallo P, Pezzotta F, Padelli F, Faragò G, Gioppo A, Gentili L, De Martin E, Fumagalli ML, Cavaliere F, Bruzzone MG, Milani P, Santaniello T. Legnani E, et al. 3D Print Addit Manuf. 2021 Aug 1;8(4):217-226. doi: 10.1089/3dp.2020.0305. Epub 2021 Aug 4. 3D Print Addit Manuf. 2021. PMID: 36654837 Free PMC article.
-
Three-dimensional computed tomography reconstruction in the era of digital personalized medicine.
Rocha-Júnior E, Pêgo-Fernandes PM. Rocha-Júnior E, et al. Sao Paulo Med J. 2023 Jan-Feb;141(1):1-3. doi: 10.1590/1516-3180.2022.14111125082022. Sao Paulo Med J. 2023. PMID: 36449968 Free PMC article. No abstract available.
-
Does using 3D printed models for pre-operative planning improve surgical outcomes of foot and ankle fracture fixation? A systematic review and meta-analysis.
Wood L, Ahmed Z. Wood L, et al. Eur J Trauma Emerg Surg. 2022 Nov 24. doi: 10.1007/s00068-022-02176-7. Online ahead of print. Eur J Trauma Emerg Surg. 2022. PMID: 36418394 Review.
-
Three-dimensional printing and 3D slicer powerful tools in understanding and treating neurosurgical diseases.
You Y, Niu Y, Sun F, Huang S, Ding P, Wang X, Zhang X, Zhang J.
 You Y, et al. Front Surg. 2022 Oct 14;9:1030081. doi: 10.3389/fsurg.2022.1030081. eCollection 2022. Front Surg. 2022. PMID: 36311943 Free PMC article. Review.
You Y, et al. Front Surg. 2022 Oct 14;9:1030081. doi: 10.3389/fsurg.2022.1030081. eCollection 2022. Front Surg. 2022. PMID: 36311943 Free PMC article. Review. -
Implementation of an In-House 3D Manufacturing Unit in a Public Hospital's Radiology Department.
García RI, Jauregui I, Del Amo C, Gandiaga A, Rodriguez O, Margallo L, Voces R, Martin N, Gallego I, Minguez R, Eguiraun H. García RI, et al. Healthcare (Basel). 2022 Sep 16;10(9):1791. doi: 10.3390/healthcare10091791. Healthcare (Basel). 2022. PMID: 36141403 Free PMC article.
See all "Cited by" articles
References
-
- Korean J Radiol. 2016 Mar-Apr;17(2):182-97 - PubMed
-
- Surg Radiol Anat.
 2016 Apr;38(3):361-7 - PubMed
2016 Apr;38(3):361-7 - PubMed
- Surg Radiol Anat.
-
- J Surg Educ. 2016 Mar-Apr;73(2):264-9 - PubMed
-
- Anat Sci Educ. 2016 May 6;9(3):213-21 - PubMed
-
- BMJ Simul Technol Enhanc Learn. 2018 Jan;4(1):27-40 - PubMed
Publication types
MeSH terms
Can 3D Printing Improve Your Medical Care? > News > Yale Medicine
So, you’re worried about getting, let’s say, a knee replacement. Will it be difficult? Will it hurt?
Will it be difficult? Will it hurt?
These are good questions. Every patient’s body is unique, and even the best surgeons do a bit of educated guessing to try to place a new knee as perfectly as possible. If the placement is even a bit off, there could be extra pain and stiffness, and it could take longer to recover.
But, what if, before your operation, your surgeon could make an exact replica of the parts of your knee—that’s your knee, as measured by your MRI and CT scan? Then, what if the surgeon could use it to plan the operation in advance and ensure precise placement of the new parts, which in turn means you’d have less pain, a speedy recovery, and a new knee that is just as good as the original? Better, actually.
That future is here. Some Yale Medicine surgeons now routinely use 3D printing (essentially producing a solid, three-dimensional object from a virtual digital model) to plan surgeries, design tools specific to an upcoming surgery and that particular patient’s anatomy, and even to print some of the parts used to replace defective ones in the body.
Daniel Wiznia, MD, a Yale Medicine orthopedic surgeon, is seeing significant improvements in his knee replacement patients since he started using 3D printing to plan their operations. He is one of several doctors who make regular use of a 3D printer at the Yale School of Engineering & Applied Science, a MakerBot machine that looks something like a microwave oven.
Vincent Wilczynski, deputy dean of the school and director of the Yale Center for Engineering Innovation & Design, remembers one of the first doctors who visited the lab several years ago, who used a printer to make a model of a 20-year-old patient’s knee tumor. “He printed the tumor every time the patient came in to get scanned, so the patient could hold the 3D model in his hands and feel how it was shrinking,” Wilczynski says.
There is more to come. Researchers are exploring ways to use 3D printing to make patient-specific transplant organs and eyes capable of translating light into electrical signals. While practical use of these things is still years away, researchers recently printed the world’s first 3D vascularized, engineered heart, using a patient’s own cells and biological materials.
While practical use of these things is still years away, researchers recently printed the world’s first 3D vascularized, engineered heart, using a patient’s own cells and biological materials.
Here are a few ways some Yale Medicine doctors are using 3D printing in patient care right now.
Easier, speedier knee replacement recovery
If you are having a knee replacement, 3D printing can make your surgery smoother, lessen the pain (which can be significant after knee surgery), and contribute to a quicker knee replacement recovery, Dr. Wiznia says. With this technology, your new knee can be implanted more accurately, leading to better biomechanics so the knee feels more natural when you move, with less wear on the implant, he adds.
“It’s a matter of precision,” Dr. Wiznia says, explaining that it lowers the risk of error compared to the traditional placement of a new knee. Following a 3D-printed model with cutting guides allows the surgeon to conduct surgery without significant positioning errors, he says.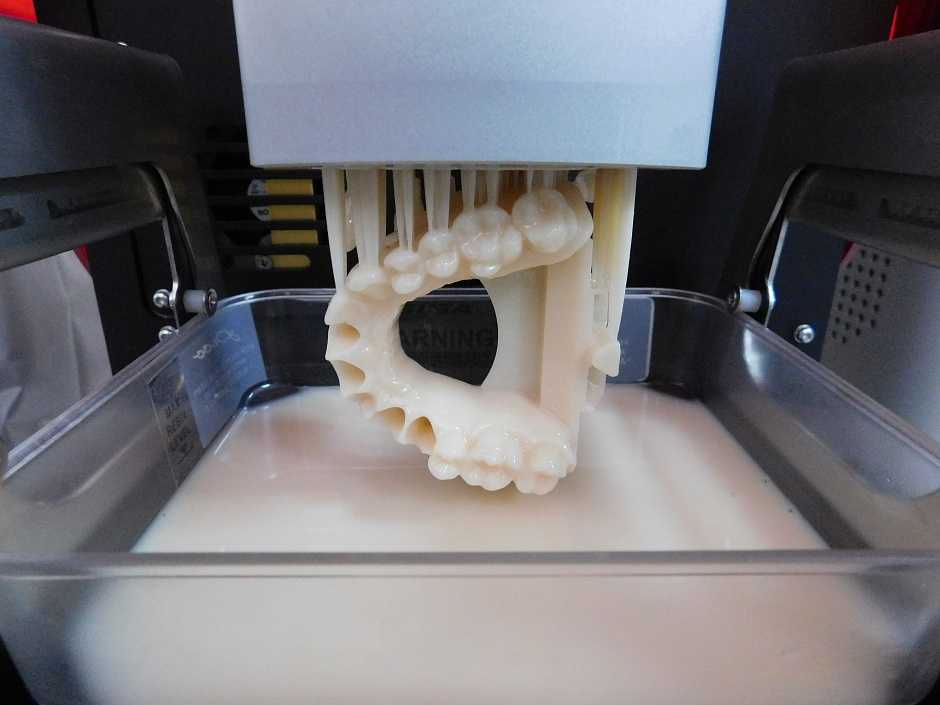
When he is planning a surgery, Dr. Wiznia feeds data from the patient’s MRI into a computer program, allowing him to use software to plan where he wants to place the new knee, how he wants it to fit on the bone, the sizes of the implants and how the knee should bend kinematically. Then, he converts the information into a format that can be fed into a 3D printer so it will custom print surgical instruments. “The beautiful thing is, you don’t have to cut as much when you do the operation,” he says. “I use smaller incisions, because I’ve already modeled how to position the implants. There is less stretching of the ligaments and soft tissue, so there is less pain, blood loss, and length of stay in the hospital.”
He predicts knees implanted this way will have a longer life span. He also says pre-planning with 3D printing allows him to shave as much as 20 to 25 minutes off the time it takes to perform a knee operation. For the patient, this means less anesthesia, fewer blood transfusions, and less tourniquet time, he says.
Planning operations with life-sized hand models
You slip on an ice patch and fall on your wrist, or you get mad and punch a wall. You can break a bone in your hand that way. Adnan Prsic, MD, a hand surgeon, decided it would be easier to fix this type of injury by first printing out a life-size model of your hand to better see what he and his residents will be working with. He has done this so many times he has amassed a collection of printed hands he keeps in a box in his office. Made of silicone, some are complete with "bones" inside made of varying types of plastics. If you bend a knuckle in one of these hands, you’ll hear a soft click (much like the legs in an old Barbie doll body). Dr. Prsic might “break” a bone inside the hand to simulate an injury.
Dr. Prsic is using 3D-printed hands in two ways. One is to help surgeons practice an especially complex hand surgery so they can better anticipate challenges. The second is to teach medical residents their craft—hand surgeons operate on small areas, so precision is key to sparing bone.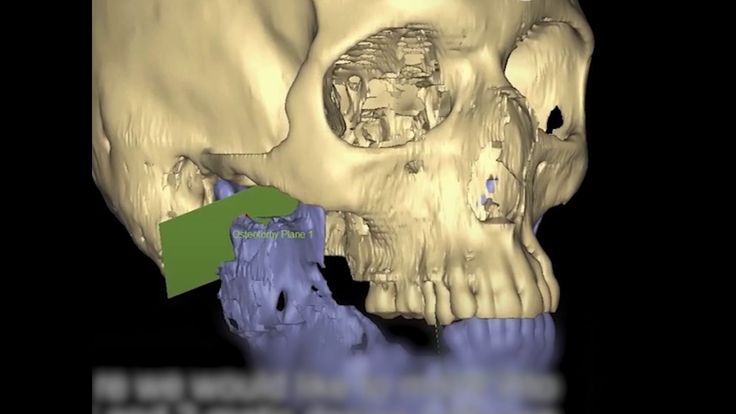 He is collaborating on this with plastic surgeon Albert Woo, MD, from the Alpert Medical School at Brown University.
He is collaborating on this with plastic surgeon Albert Woo, MD, from the Alpert Medical School at Brown University.
Other hand specialists have tried similar things with high-end 3D printers, but Dr. Prsic wants the capability to be available to anyone. So, he is making hands on the inexpensive MakerBot machine; he says each costs about $30, compared to $150 to make a hand on a more sophisticated machine. Inspired to become a hand surgeon in his native Bosnia, where he saw people come out of war with terrible hand injuries, Dr. Prsic says one of his future goals is to provide a model for inexpensive prosthetic hands that will be affordable for people in developing countries. He and Yale Medicine colleague James Clune, MD, are working on this together.
Easing anxiety when a birth defect is diagnosed
The more you can understand about a birth defect while the baby is in utero, the better you will be prepared to treat it, says Mert Ozan Bahtiyar, MD, director of the Yale Medicine Fetal Care Center. While it’s not currently possible to print out a model of a problem deep inside the body, like a heart defect, he envisions using 3D models of such problems as cleft palates and hand deformities. He believes these could be helpful psychologically to expectant parents.
While it’s not currently possible to print out a model of a problem deep inside the body, like a heart defect, he envisions using 3D models of such problems as cleft palates and hand deformities. He believes these could be helpful psychologically to expectant parents.
He also has printed a placenta to show prospective mothers who he treats with twin-to-twin transfusion syndrome, a condition characterized by an imbalance in blood flow due to placental vessel connections. “I show them what the surface of the placenta looks like and talk about how the procedure is done."
Producing these 3D parts for expectant parents is more difficult than creating models of hands or hips. Doctors use ultrasounds when they perform imaging for pregnant women because it does not harm the unborn baby. But software to convert ultrasound to a 3D-printable file format isn’t as readily available as it is for CT scans. So, Dr. Bahtiyar is working with Xenophon Papademetris, PhD, professor of Radiology & Biomedical Imaging and Biomedical Engineering at Yale School of Medicine, and Praneeth Sadda, a Yale medical student, to develop what he needs. His ultimate goal is to keep a 3D printer in his office so he can print out pictures during patient visits.
His ultimate goal is to keep a 3D printer in his office so he can print out pictures during patient visits.
“When I diagnose a fetal anomaly, the next step is counseling parents about how it will look,” says Dr. Bahtiyar, explaining that a 3D print is more powerful than an ultrasound, which provides a picture in two-dimensional black and white, with fields of gray. “I don’t think it will change the way we treat these problems. But pregnancy is not only the physical part, it is emotional as well, so maybe this will help a patient’s psyche. Maybe if they touch it, feel like it’s there, it makes them less anxious. It takes away the surprise.”
Restoring or adjusting to fix a face
Sometimes plastic surgeons are called upon to reposition a nose or create a stronger jaw, either for cosmetic purposes or to improve function. Besides repositioning parts of the face, their work may include facial reconstruction surgery and bone manipulation. Derek Steinbacher, DMD, MD, plastic surgeon and director of craniofacial medicine for Yale Medicine, has a varied collection of skulls, faces, and cutting guides, along with other 3D prints.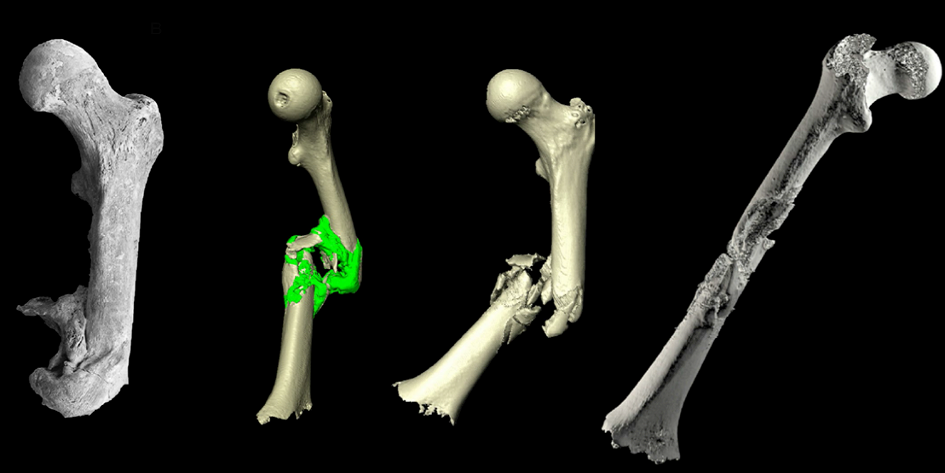 A leading expert in the use of 3D imaging and printing in plastic surgery, he uses these techniques to aid in his treatment of complex cases such as rebuilding sections of the face or skull, treating congenital skull abnormalities, and nasal, orthognathic, and facial aesthetics.
A leading expert in the use of 3D imaging and printing in plastic surgery, he uses these techniques to aid in his treatment of complex cases such as rebuilding sections of the face or skull, treating congenital skull abnormalities, and nasal, orthognathic, and facial aesthetics.
He has been using 3D printing routinely since he arrived at Yale almost nine years ago, and has used it for almost 2,000 cases. He says it has revolutionized these surgeries, taking the process from “eyeballing intraoperatively” to a high level of planned precision that makes his work far more efficient, reproducible, and accurate.
The first step in bony 3D planning and printing is for the patient to have a CT scan of the area where he will operate. “That is converted to a virtual 3D image that can be manipulated—like an architect who builds something by first working with a 3D model in digital space,” Dr. Steinbacher explains. “In our case, we analyze and manipulate the 3D anatomy and gain insight into the patient’s diagnosis, walk through possible reconstructive scenarios, choose the final plan, and then print models and guides. ”
”
Rhinoplasty (plastic surgery on the nose) is one operation where the approach is especially useful. “We look at a patient’s pre-existing nose, and we can see whether it is pointing left or right, or if it is somehow asymmetric. Then we manipulate it on the computer. There is some aesthetic and artistic preference that goes into it,” he says. “I also have to consider function.”
Dr. Steinbacher says, “it is possible from the 3D image to print a model of their nose or face with the actual expected post-op results.” He works closely with companies that specialize in this type of 3D printing. He has also printed actual parts to use as permanent implants in a new face, and plates that can be used to help move a jaw. Or, “if there is a tumor in the lower jaw, you can see exactly where that tumor is,” he says. He compares that with the opposite side of the face to see how he will reconstruct it once the tumor is removed.
Making complex operations for kids safer
A 3D model has prompted David Frumberg, MD, a pediatric orthopedic surgeon, to completely change the direction of a surgery that he has planned. Dr. Frumberg performs complicated surgeries for young children with such problems as limb and spinal deformities, as well as those with a variety of congenital or acquired conditions. He has used X-rays, CT scans, and MRI imaging to assess deformities and injuries and to plan an operation ahead of time, but he says 3D prints provide the most useful information.
Dr. Frumberg performs complicated surgeries for young children with such problems as limb and spinal deformities, as well as those with a variety of congenital or acquired conditions. He has used X-rays, CT scans, and MRI imaging to assess deformities and injuries and to plan an operation ahead of time, but he says 3D prints provide the most useful information.
“A life-size model of the actual bones that I can hold in my hand—there is something about it that changes everything,” he says. When he is planning a foot surgery, he is able to orient the model foot in different directions. “I can see what would happen if I shift one thing—or cut it one way as opposed to another during the surgery.”
Using a 3D-printed model was especially helpful when Dr. Frumberg performed foot and ankle surgery on a young girl from outside the U.S. with a rare congenital disorder that caused extreme abnormalities in her limb alignment. The girl did not have access to proper medical care as a child, and because doctors normally would have treated the issues when she was a toddler, there was no clear roadmap, he says. “If you are doing a surgery at this level of complexity, and you really need to know where all the bones are and maybe even practice, there is no better way.”
“If you are doing a surgery at this level of complexity, and you really need to know where all the bones are and maybe even practice, there is no better way.”
Dr. Frumberg says the models also seem to help children and families feel better about their procedures. When he was preparing to do a complicated operation on another girl’s foot, he showed her a 3D model he had printed, and drew on it with a Sharpie to show the various cuts he would make. “She was excited for the surgery after we did that,” Dr. Frumberg said. Later, he said, one of his medical students made a small 3D print of the model into a keychain she could keep.
Read more Yale Medicine newsRelated Specialists
new advances in surgical simulation
Implementation stories
Medicine
Author: Aleksey Chekhovich
Author: Aleksey Chekhovich
High-precision models for training specialists in the field of surgery | Comments of hospital surgeons | Sharebot 3D printers are reliable tools for innovation
Undoubtedly, 3D printing is one of the most advanced technologies of our era and, probably, in a few decades, these years will be remembered as the period of its formation.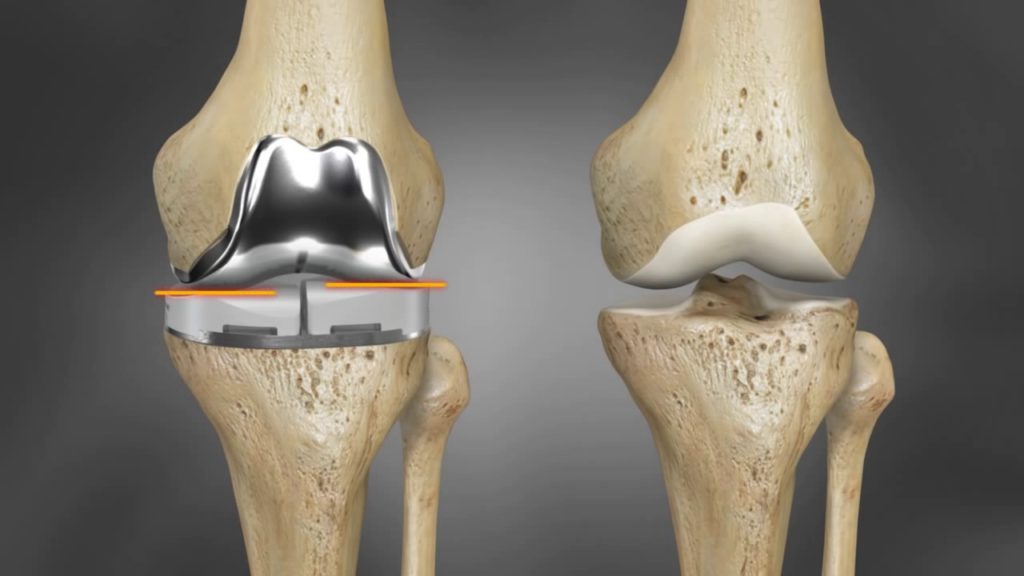 This is one of the most promising and revolutionary technologies that is used in various fields, in particular, in healthcare. Therefore, it is worth clarifying a few questions. For example, how can 3D printers contribute to the development of medicine and healthcare in general?
This is one of the most promising and revolutionary technologies that is used in various fields, in particular, in healthcare. Therefore, it is worth clarifying a few questions. For example, how can 3D printers contribute to the development of medicine and healthcare in general?
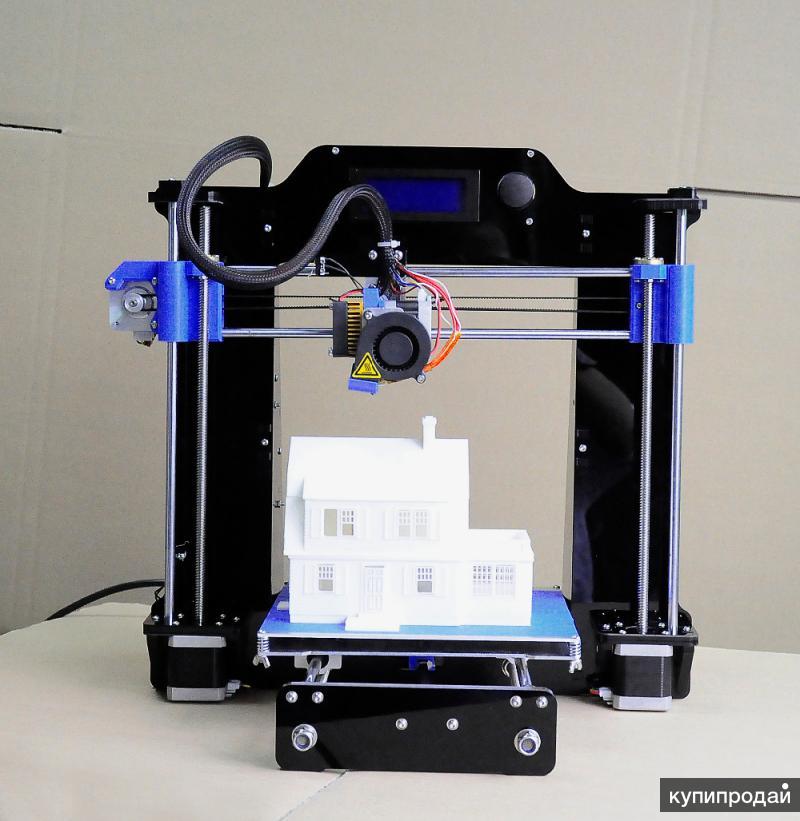
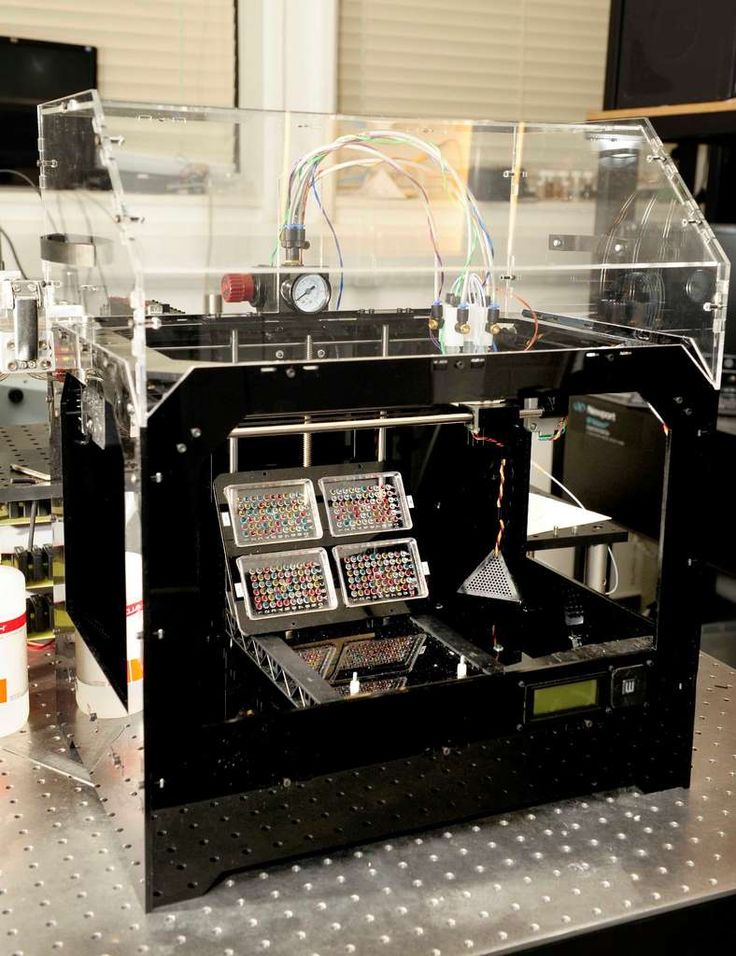
A good example is the unique project of the General Surgery Department of the Sacra Famiglia Fatebenefratelli Hospital in Erba (Lombardy, Italy), where, using the Sharebot 3D printer, it was possible to recreate real anatomical organs and structures to simulate basic surgical interventions, such as video laparoscopic cholecystectomy.
Meet sharebot.ru : all about innovative 3D solutions to optimize your business. Catalog of 3D printers based on the most popular additive technologies, tasks and applications, success stories, promotions, videos and other useful materials!
Liver and gallbladder segment models printed on a Sharebot 43 FDM printer
In collaboration with Sharebot, an experimental model of a segment of the liver and gallbladder was created using a special material (LAY-FOMM) produced in the form of a plastic thread. After immersion in water, this material, thanks to its two-component composition (rubber and PVA-based soluble part), becomes similar to organic tissues, which also allows surgical sutures to be applied. It was found that the degree of extensibility in combination with residual moisture after immersion in water is similar to organic counterparts.
After immersion in water, this material, thanks to its two-component composition (rubber and PVA-based soluble part), becomes similar to organic tissues, which also allows surgical sutures to be applied. It was found that the degree of extensibility in combination with residual moisture after immersion in water is similar to organic counterparts.
iQB Technologies experts recommend the article: Additive technologies in medicine: how to reduce risks to patients' health
Is your healthcare facility interested in implementing 3D technologies? Order free test services 3D printing and 3D scanning!
Leave a request
High-precision surgical training models
Thus, the surgeons of the hospital were able to reproduce the video laparoscopic cholecystectomy directly on the printed models. In practice, this involves removing the gallbladder without damaging the liver tissue. Performing surgery on a model pelvis (laparoscopic simulator) allows surgeons to master the correct technique, as well as experiment with new non-invasive methods of removal.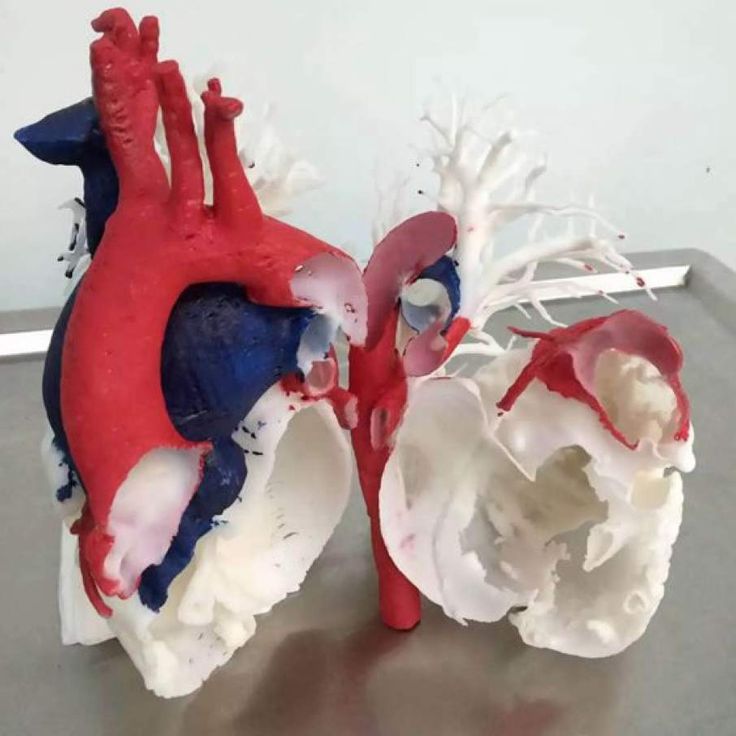
Pelvic Surgery Simulator
By simulating important surgeries on high-precision 3D-printed anatomical models, it has been possible to make a big step in the field of medical technology, which undoubtedly increases the chances of patients recovering with similar interventions.
We are interested in 3D printing in terms of practical training of a new generation of surgeons based on more advanced and accurate models.
Specialists of the General Surgery Department of the Sacra Famiglia Fatebenefratelli Hospital
Comments from surgeons at hospital
The peculiarity of the model developed by us is that there are two holes between the liver and the gallbladder, which make it possible to completely empty the gallbladder in order to then fill it with a colored liquid to simulate bile. Due to its elasticity, the liver is also used to develop the technical possibilities of applying laparoscopic and traditional sutures.
In each model, the liver and gallbladder are directly connected by supporting structures. Using a raft (a horizontal mesh of plastic located at the base of the model) and supports, we developed a model of the gallbladder, in which they, simulating the liver bed, allow us to model the plane of the liver section. This model includes only the gallbladder and saves consumables, which speeds up the 3D printing process.
Anatomical base with liver made of PLA plastic
We also reduced the space between the support and the gallbladder to make the area between them more complex and realistic. For more efficient placement inside the pelvis model (laparoscopic simulator), we created an anatomical base with a liver made of PLA plastic. It contains a soft sponge that mimics a real liver, into which a component of a 3D model of the gallbladder made of LAY-FOMM, an easy-to-use filament, has been inserted through the valve. This rigid model allows quick and easy replacement of LAY-FOMM gallbladder models.
Finally, we created an ellipsoidal cylindrical model with a vertical hole, which makes it possible to simulate intestinal sutures and anastomoses. 3D printing of this model does not require much time and money.
Models for testing intestinal sutures
We believe that this technology opens up diverse and broad possibilities. We intend to create models of other organs for high-precision simulation of a number of important surgical interventions. To do this, we need to learn how to perform 3D printing based on DICOM files in particularly complex or atypical cases sometimes encountered in clinical practice. In general, 3D printing with LAY-FOMM interested us in terms of technical perspectives and, most importantly, the practical training of a new generation of surgeons based on more advanced and accurate models.
Specialists of the Department of General Surgery
iQB Technologies Experts Recommend Article: 3D Printed Prostheses Transform Patients' Lives
Sharebot 3D Printers - Reliable Tools for Innovation
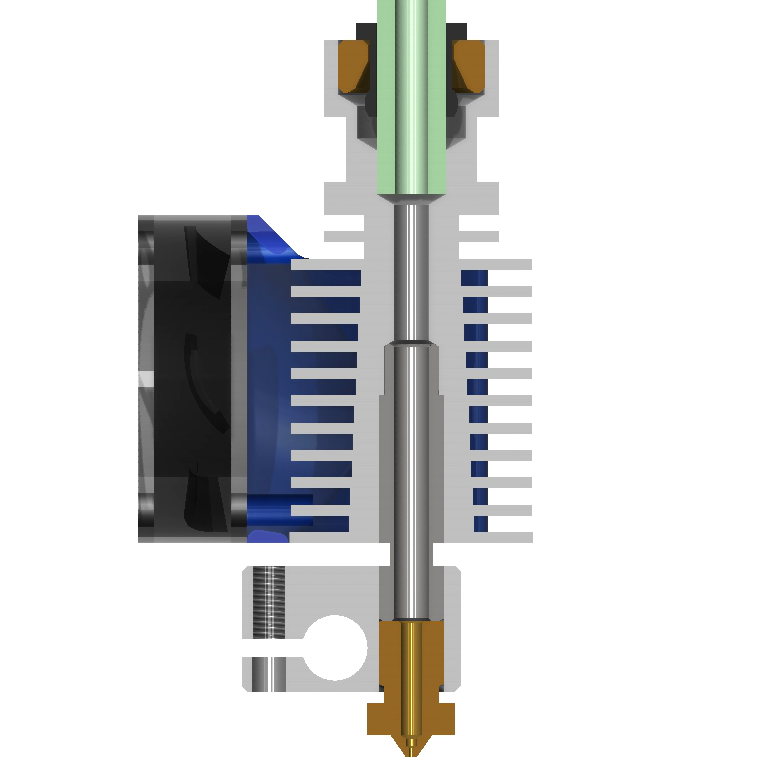
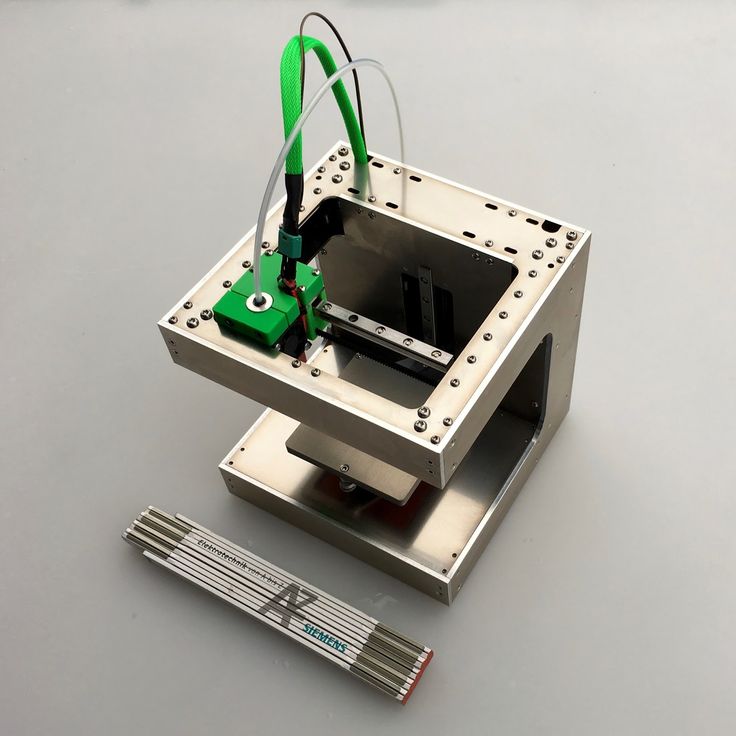
Fatebfratelli hospital staff use a Sharebot 43 compact professional 3D printer equipped with two autonomous extruders. The device allows you to print products of the most complex geometry with soluble supports. In addition, a system of mirroring and duplication is available when printing. The flexible printer platform maintains a temperature of 120°C, and the maximum heating temperature of the extruders reaches 300°C, which allows the use of technical and professional materials that meet a wide variety of physical, chemical and mechanical conditions, including high or low temperature, the presence of oil and gasoline, as well as impact and friction.
Printing process on Sharebot 43
The collaboration between Sharebot and the Department of General Surgery at the Fatebenefratelli Hospital in Erba has demonstrated the importance of introducing 3D printing, which opens up the possibility of creating new types of models and high-precision surgical simulators. This area is just one of the possible directions for the development of technology. Whether it's recreating organs for experimentation or printing implantable prostheses, 3D technology is becoming a key tool for medical innovation.
Sharebot is a young and innovative company working with four different 3D printing technologies: FDM, LCD, SLS and DMLS. Sharebot's R&D department keeps abreast of cutting-edge technologies by exploring their latest capabilities. More than 3500 printers of the company work worldwide, 160 of them are used at universities. Sharebot has a leading position in Europe and is the only supplier on the continent to offer four 3D printing technologies based on materials such as plastic filament, photopolymers, thermoplastic and metal powders.
Material provided by Sharebot
Article published on May 19, 2021, updated on January 17, 2023
How 3D printing is currently being used in spine surgery
Patient-specific anatomical models can help with surgical simulations, intra-ward discussions, patient consent discussions, and help reduce the associated costs of surgery.
Dr. Andrew Kanawati is an orthopedic surgeon at Westmead Hospital in Sydney with a particular interest in the clinical and research use of 3D printing. He has designed several custom 3D printed spinal guides for patients to assist in surgery and uses composite models made from several different Formlabs materials to plan complex surgeries.
3D printing of tumors
Historically, research in medical printing has focused on FDM printers due to their low price and ubiquitous market penetration in the past. Dr. Kanawati believes there is a huge advantage to using SLA 3D printing due to the superior material properties of the final parts. Material properties such as the ability to print waterproof models (which FDM cannot do) meant that higher quality medical devices could be printed and tested.
One day Dr. Kanawati was examining a patient who complained of pain in his legs. In his youth, the patient was diagnosed with a benign tumor. New MRI and CT showed that the tumor was growing towards the patient's spine. Pressing on the nerves, the tumor was a serious medical problem.
Every tumor is different and every patient is different. In complex cases involving the spinal cord and nerves, being able to explore a person's anatomy in 3D can be the difference between a successful operation or a failure.
Dr. Kanawati decided to use his Formlabs SLA 3D printer and proprietary resins. The complete model of the lower spine and tumor used 156 ml of Gray Resin, which is equivalent to only $23.
The patient's spine model was printed in just under 13 hours using just 156 ml of resin ($23).
A 360-degree physical model of the patient's spine and tumor helps surgeons reduce errors and improve treatment outcomes. The models help surgeons visualize and manipulate the points of contact between the tumor and nerve branches, giving them greater dexterity and confidence during surgery. This is the main advantage of 3D printing for spine surgery. Having their own SLA 3D printers allows surgeons to scan, segment and print models throughout the day. In emergency cases where time is of the essence, a 3D printed model can inform surgeons about decisions and give them extra confidence.
Having access to a 3D printed model helps with preoperative planning, allowing Dr. Kanawati to evaluate the feasibility of the operation. Less surgery time means less stress on the spinal cord without causing direct damage to the nervous system. It also allowed the team to better understand which stalk (a small, stem-like structure that connects an organ or other part of the human or animal body) is viable and how best to perform the surgery.
The nerves were printed with Elastic Resin and placed on the 3D printed bone model.
But Dr. Kanawati didn't finish the model. He demonstrated the possibilities of SLA 3D printing for medical applications using multiple materials on a single printer. Dr. Kanawati changed the Resin Tank with Gray Resin to a new one and began to create replicas of the patient's nerves from Elastic Resin. This allowed him to put nerves on the spinal model, which meant there were no surprises once the surgery began. He said: "We started operating on the patient from the back. During the operation, we couldn't see the nerves, but thanks to the 3D model we created, we knew exactly where they were."
Limited resource conservation
3D printing can help with more than just preoperative planning. Dr. Kanawati wanted to see if he could 3D print patient-specific cutting templates to use for precision laminectomy. According to Johns Hopkins, a laminectomy is a type of surgery in which a surgeon removes part or all of the spinal bone. This helps relieve pressure on the spinal cord or nerve roots that can be caused by injury, a herniated disc, a narrowing of the canal (spinal stenosis), or a tumor. According to the Health Care Cost and Use Project (HCUP) National Hospital Inpatient Sample (NIS), “annual laminectomy estimates average about 34 discharges per 100,000 adults from 1998 to 2008", which makes them a very common operation.
Dr. Kanawati again turned to his Formlabs 3D printer and Gray Resin, printing guides and a model of the spine on the same platform. After extracting and post-processing the models, he was able to screw the guides into the spine model to see if they fit. If any adjustments were required, they could easily be reprinted.
By running a full surgical simulation before examining a cadaver, the team can find problems with the cutting guides without wasting or risking a fresh cadaver. Considering that cadaveric material is a limited resource, reducing the number of failures in the preoperative testing phase is a source of significant cost savings.
The cutting guides have another advantage: they allow the use of high speed drills. Generally, high-speed drills are not allowed during operations, as they can damage the surrounding nerve elements if not properly oriented. But with a perfectly fitted 3D printed cutting guide, these drills are safe to use and greatly improve and speed up the operation.
Following this experience, Dr. Kanawati published a research paper on this topic titled "Development of new 3D printed 2-in-1 laminectomy guides with integrated pedicle screw drilling guides".
Find out how 3D printing is already impacting surgery
Dr. Kanawati is not the only medical professional using 3D printing to streamline workflows and improve outcomes in spinal surgery.
For example, Andrew Bowie is responsible for managing the 3D platform at the Royal Victorian Infirmary and Newcastle-based Freeman Hospitals, which are the first spinal centers in the UK. Bowie's team prints 3D anatomical models that help clinicians explain procedures to patients and families, helping to fully demonstrate risks and manage expectations. By doing a full surgical simulation before the operation, Mr Bowie was able to save over 120 minutes of time during the complex surgical procedure, which is around £8,000 of the hospital's funds. In addition, this process also contributed to the reduction of blood loss and improved communication with the surgical team throughout the procedure.
“Spine surgery can be extremely complex and no two procedures are the same.
Learn more