Dr atala 3d printing
Dr. Anthony Atala Explains the Frontiers of Bioprinting for Regenerative Medicine at Wake Forest - 3DPrint.com
Anthony Atala is a pediatric surgeon, urologist and directs the Wake Forest Institute for Regenerative Medicine (WFIRM) in North Carolina. Together with 400 colleagues and in a work that spans more than three decades, he has successfully implanted in human patients a variety of tissues regenerated from the patient’s own cells. Dr. Atala talked to 3DPrint.com about ways to translate the science of regenerative medicine into clinical therapy and the importance of adopting new technologies, as well as some of the challenges.
Dr. Anthony Atala in the Regenerative medicine laboratories, Wake Forest Institute for Regenerative Medicine (WFIRM).
“Back in the 90’s we created by hand, even without using the printer, bladders, skin, cartilage, urethra, muscle and vaginal organs, and later implanted them successfully in patients. The printer automated what we were already doing and scaled it up making some of the processes easier.
Still, the technology has its own challenges. With hand made constructs you have more control as you are creating the tissue, but with the printed structure everything has to be built in before it is created, so that you have to have the whole plan and information ready to go once you push that ‘start’ button,” suggested Dr. Atala, who earned his medical degree from the University of Louisville School of Medicine and went onto complete a fellowship at Harvard Medical School, before joining Wake Forest Baptist in 2006 as the founding director of the Wake Forest Institute for Regenerative Medicine and chair of the Department of Urology.
The WFIRM is working to grow tissues and organs and develop healing cell therapies for more than 40 different areas of the body, from kidney and trachea to cartilage and skin. Dr. Atala and his team of scientists have been first in the world to implant lab-grown tissues and organs into patients. Starting in 1990 with most of their research and implanting the first structures at the end of that decade, using a 3D printer to build a synthetic scaffold of a human bladder, which they then coated with cells taken from their patients. New research at WFIRM shows innovative wound healing through the use of a bedside 3D skin printer.
New research at WFIRM shows innovative wound healing through the use of a bedside 3D skin printer.
Specialist Young-Joon Seol at WFIRM demonstrates bioprinting muscle tissue with The Integrated Tissue Organ Printing System.
“Today, we continue to develop replacement tissues and organs, and are also working to speed up the availability of these treatments to patients. The ultimate goal is to create tissues for patients. Part of that is taking a very small piece of the patients tissue from the organ that we are trying to reconstruct, like muscle or blood vessels, only to expand the cells outside of the body and then use them to create the organ or structure along with a scaffold or a hydrogel which is the glue that holds the cells together. We have been doing this for quite some time with patients and 16 years ago we realized that we needed to scale up the technology and automate it to work with thousands of patients at a time, so we started thinking about 3D printers, and began using the typical desktop inkjet printer which was modified in-house to print cells into a 3D shape,” continued Dr.
Atala, who also directs the Armed Forces Institute of Regenerative Medicine, with federally funded projects underway in engineering blood vessels, developing treatments to heal wounds and engineering replacement tissues for devastating pelvic injuries.
The living cells were placed in the wells of the ink cartridge and the printer was programmed to print them in a certain order. The printer is now part of the permanent collection of the National Museum of Health and Medicine. According to Dr. Atala, all the printers at the WFIRM continue to be built in-house specifically to create tissues, so that they are highly specialized and able to create cells without damaging the tissue as it gets printed. Inside the institute, more than 400 scientists in the fields of biomedical and chemical engineering, cell and molecular biology, biochemistry, pharmacology, physiology, materials science, nanotechnology, genomics, proteomics, surgery and medicine work to try to develop some of the most advanced functional organs for their patients.
A bladder scaffold being seeded with cells at WFIRM.
Dr. Atala claims that “we have to really understand cells to do this work. To get to where we are now, we studied and looked at cell biology during most of the first 10 years of our work. It is critical for us to understand how to harvest cells, keep them alive, how to grow them into large quantities, as well as making sure they retain their normal functions. The cells are alive and we need to keep them that way, giving them nutrition and keeping them in the same conditions as those they had in the human body – including a temperature of 37 degrees centigrades and 95% oxygen. We place them in incubators that offer the same conditions as the human body, later we artificially feed the cells with nutrients and when we create the tissues we feed them as well. We can only leave them outside of the body for a short period of time, between seven to ten days, depending on the organ.”
Completed ear and jaw bone structure in cell culture medium.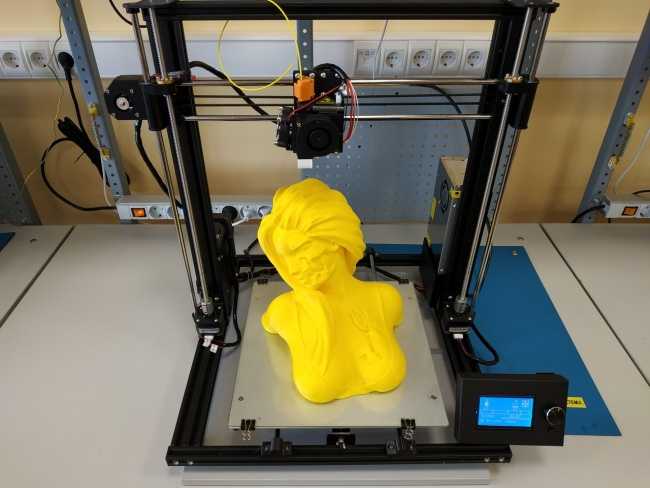
At WFRIM they are focusing on personalized medicine, whereby the scientists use the sample tissue from the patient they are treating, grow it and implant it back to avoid rejection. Dr. Atala claims that “these technologies get tested extensively before they are implanted into a patient,” and that “it could take years or even decades of research and investigation before going from the experimental phase to the actual trial in humans.”
“Our goal for the coming decade is to keep implanting tissues in patients, however, the most important thing for us is that we temper peoples expectations because these tissues come out very slowly and they come out one at a time, so we don’t give false hopes and provide the technology to patients who really need them. Working with over 40 different tissues and organs, means that about 10 applications of this technologies are already in patients. The research we have done helps us categorize tissues under order of complexity, so we know that flat structures (like skin) are the least complex; tubular structures (such as blood vessels) have the second level of complexity, and hollow non-tubular organs, including the bladder or stomach, have the third level of complexity because the architecture of the cells are manifold.
Finally, the most complex organs are solid ones, like the heart, the liver and kidneys, which require more cells per centimeter,” implied the expert 3D bioprinting scientist.
The 3D printer at the Wake Forest Institute for Regenerative Medicine seeds different types of cells onto various scaffolds including ear cartilage.
With the goal to cure, rather than merely treat, disease, in the early 2000s Dr. Atala successfully led a project to grow a human bladder using bioprinting and transplanted it to a young patient suffering from spina bifida, a condition which can cause bladder problems. The patient’s case was an early example of what tissue engineering can accomplish, but advances in bioprinting are making such cases more common and now the lead investigator at Wake Forest’s institute has also set his eyes on bioprinting kidneys – one of the organs most in demand. And although he claims that the science is progressing in the right direction, it is still a long way from printing completely functional organs for transplant in humans.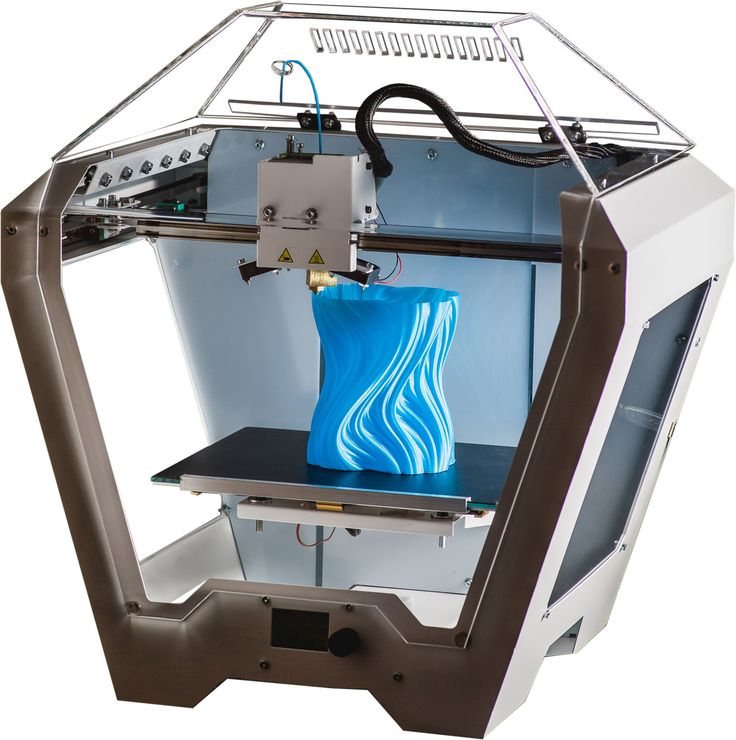 Dr. Atala began working way back when the tissues were engineered by hand and as the research advanced, he noticed the higher needs for better solutions.
Dr. Atala began working way back when the tissues were engineered by hand and as the research advanced, he noticed the higher needs for better solutions.
“We are still looking for better ways to what we do today, and that will never change, because we will always want to improve the process of tissue engineering,” Dr. Atala said.
There are a lot of technologies benefiting the area of regenerative medicine, including nanotechnology and gene editing.
“As science advances, we can benefit from leading research in other areas and help each other out,” Dr. Atala said. “The pace has picked up, because we know so much more than we did 30 years ago, we have more knowledge that allows us to be more precise in our strategies. This does not mean that we are progressing faster but the information that we get, allows us to be more precise in how we target our solutions.”
Dr. Atala and his team understand firsthand how to treat and care for patients, which is why the WFIRM is so good at advancing regenerative medicine.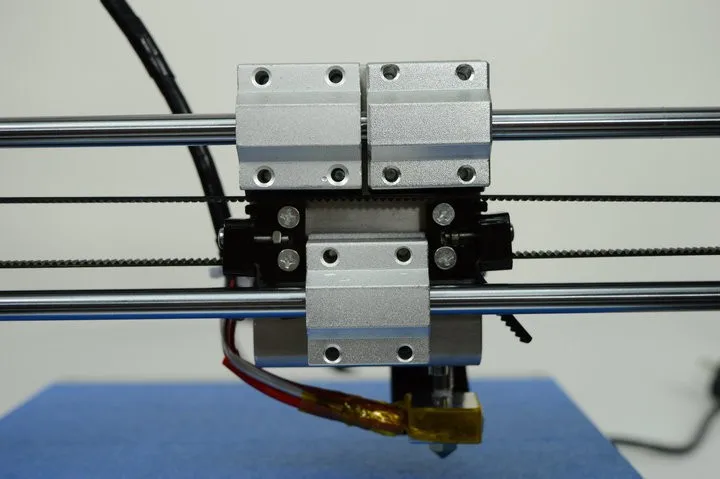 Dr. Atala knows how important it is for a patient’s health to implant a tissue harvested from the person’s own cells, and looks forward to the next disruptive technologies that will lead regenerative medicine into further advances for better health solutions. One thing is for sure, demand for WFIRM’s technology will most likely be soaring in the next few years.
Dr. Atala knows how important it is for a patient’s health to implant a tissue harvested from the person’s own cells, and looks forward to the next disruptive technologies that will lead regenerative medicine into further advances for better health solutions. One thing is for sure, demand for WFIRM’s technology will most likely be soaring in the next few years.
[Images: WFIRM]
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
Tagged with: 3d bioprinting • 3d bioprinting 3d print tissue • 3d printing interview • Dr. Anthony Atala • regenerative medicine • tissue engineering • Wake Forest Institute for Regenerative Medicine • WFIRM
Please enable JavaScript to view the comments powered by Disqus.
Three‐Dimensional Bioprinting in Regenerative Medicine: Reality, Hype, and Future
Regenerative medicine aims to repair or restore function to tissues and organs. The field has seen major advances recently even if serious challenges still remain, stemming primarily from the inherent complexity of the human body. The organs in our body are results of millions of years of evolution in the course of which nature experimented until it “got it right.” This experimentation was not without victims: many of the shapes and forms that appeared eventually were eliminated by natural selection, favoring those with the most relevant function and compatible intricate structure. As a consequence, present day tissues and organs are all complex, and their complexity varies depending on the cell type and organization, architecture, and function. Flat tissues (e.g., skin) are the least complex, tubular structures (e.g., blood vessels) more complex, hollow nontubular organs (e.g., bladder) even more complex, and solid organs (e.g., liver or heart) the most complex.
The field has seen major advances recently even if serious challenges still remain, stemming primarily from the inherent complexity of the human body. The organs in our body are results of millions of years of evolution in the course of which nature experimented until it “got it right.” This experimentation was not without victims: many of the shapes and forms that appeared eventually were eliminated by natural selection, favoring those with the most relevant function and compatible intricate structure. As a consequence, present day tissues and organs are all complex, and their complexity varies depending on the cell type and organization, architecture, and function. Flat tissues (e.g., skin) are the least complex, tubular structures (e.g., blood vessels) more complex, hollow nontubular organs (e.g., bladder) even more complex, and solid organs (e.g., liver or heart) the most complex.
Just three decades ago, most human cell types could not be grown and expanded outside the body, human stem cells had not yet been identified, and technologies such as cloning had not yet been developed.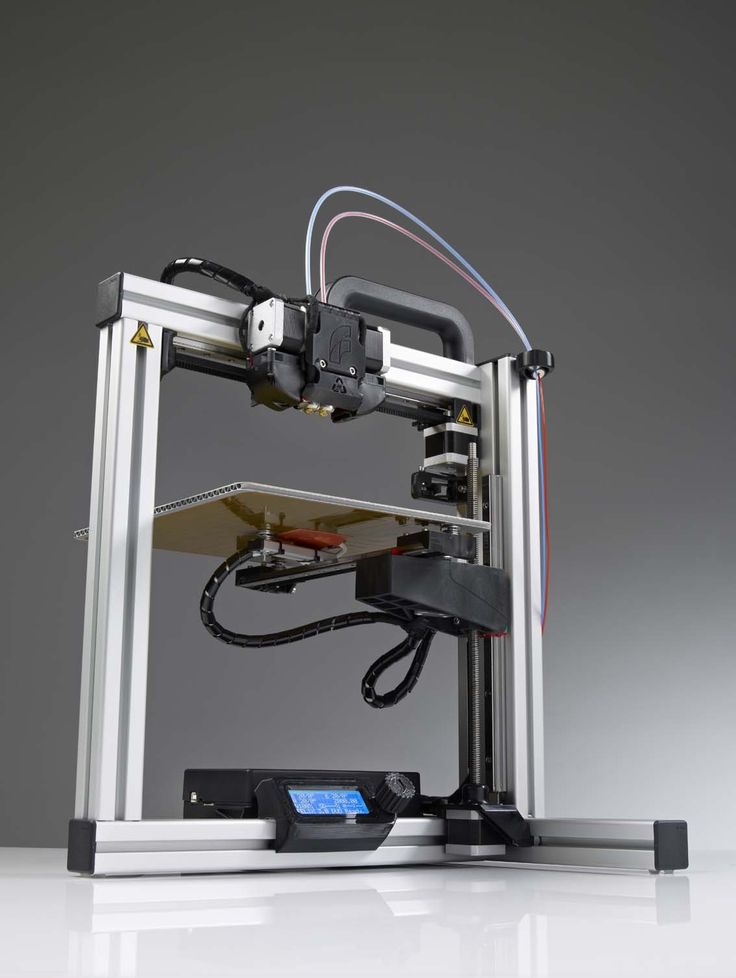 Today, with advances in cell and molecular biology, most types of cells can be grown in vitro, multiple types of human stem cells have been established and organs have been engineered in the laboratory. Engineered organs such as skin, urethra, blood vessel, bladder, and vagina have been implanted in patients in limited numbers in clinical trials. Several tissue‐engineered products are advancing through the regulatory pathway so they can be eventually commercialized and disseminated widely. However, most of the engineered tissues now in the more advanced stages of the regulatory pathway were made by hand.
Today, with advances in cell and molecular biology, most types of cells can be grown in vitro, multiple types of human stem cells have been established and organs have been engineered in the laboratory. Engineered organs such as skin, urethra, blood vessel, bladder, and vagina have been implanted in patients in limited numbers in clinical trials. Several tissue‐engineered products are advancing through the regulatory pathway so they can be eventually commercialized and disseminated widely. However, most of the engineered tissues now in the more advanced stages of the regulatory pathway were made by hand.
The engineering of a living tissue and its fabrication by hand require several steps, each with its own hurdles. The undertaking starts with the sourcing of the seed population of cells. For this, typically, a tissue biopsy is performed. The resulting cells then have to be grown and expanded in vitro. This may sound easy. However, reliably obtaining cells with similar release criteria that will perform with the expected level of function requires extensive knowledge of cell and molecular biology. Harvesting and cell expansion techniques, culture media protocols, growth factor additives, environmental conditions, and sterility are just a few of the many details necessary to have the right cells as a starting material. Furthermore, an adult liver for example contains approximately 100 billion cells, and is composed of multiple cell types, including hepatocytes, stellate cells, and Kupffer cells. In order to create such an organ, the various cells need to be expanded at the same time, to large numbers and thus divided many times outside of the body. Extreme care needs to be exercised to make sure that the resulting cells do not become transformed and remain functional consistent with their intended use.
Harvesting and cell expansion techniques, culture media protocols, growth factor additives, environmental conditions, and sterility are just a few of the many details necessary to have the right cells as a starting material. Furthermore, an adult liver for example contains approximately 100 billion cells, and is composed of multiple cell types, including hepatocytes, stellate cells, and Kupffer cells. In order to create such an organ, the various cells need to be expanded at the same time, to large numbers and thus divided many times outside of the body. Extreme care needs to be exercised to make sure that the resulting cells do not become transformed and remain functional consistent with their intended use.
Equally complex are the biomaterials that are necessary to make normal tissues. They need to have the right properties to support cells in vitro but also characteristics to make them biocompatible and suitable for impantation into the patient. Finally, adding the cells to the biomaterials with the interactions necessary to have the right environment for tissue formation in bioreactors and incubators adds yet another level of complexity to the process.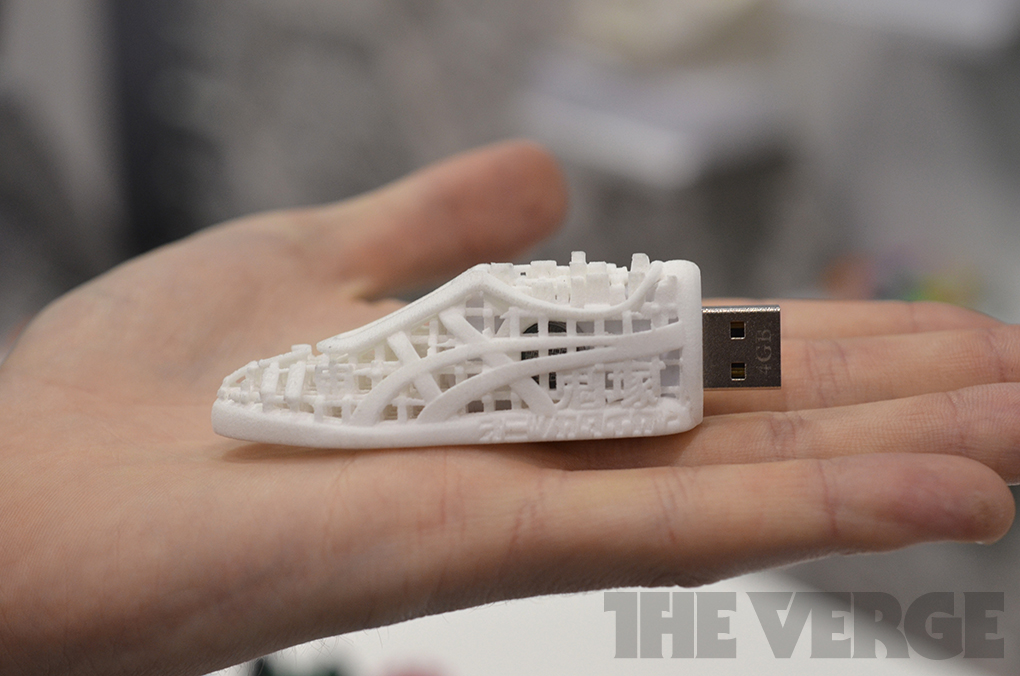
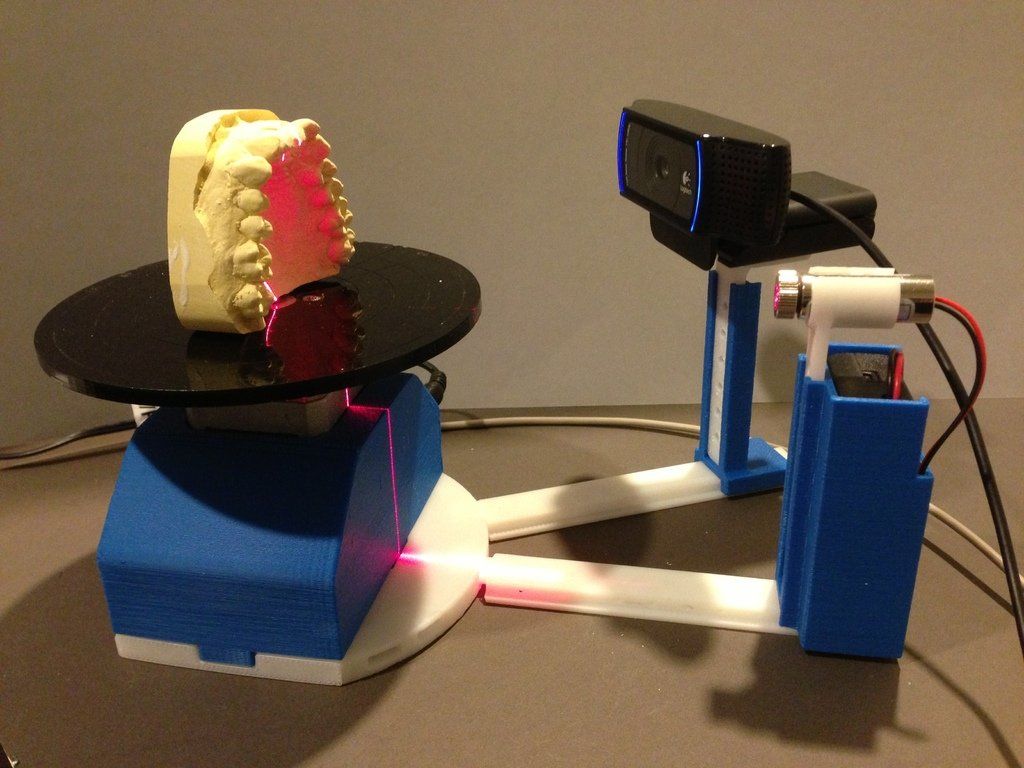
In parallel to the development of regenerative medicine, the field of three‐dimensional (3D) printing has also advanced. Three‐dimensional printing has been used in the manufacturing industry for decades. It was first applied to make plastic samples to be used as prototypes for more complex parts that would typically be later mass produced. This was a laborious and costly process. The printers initially were cumbersome and expensive pieces of machinery, some with a cost of more than a million dollars, and technically difficult to operate. Technological advances have led to the current state‐of‐the‐art printers that are being used to manufacture a wide range of products, from complex tools to automotive parts and entire buildings. The design and operation of 3D printers have been markedly simplified. Desktop 3D printers can now be used even by children and are being sold in toy stores at a low cost, some for less than $100.
Three‐dimensional printing, now also a major component of additive manufacturing, led to the more recent advent of bioprinting, the specific application of the technology in the life sciences and medicine.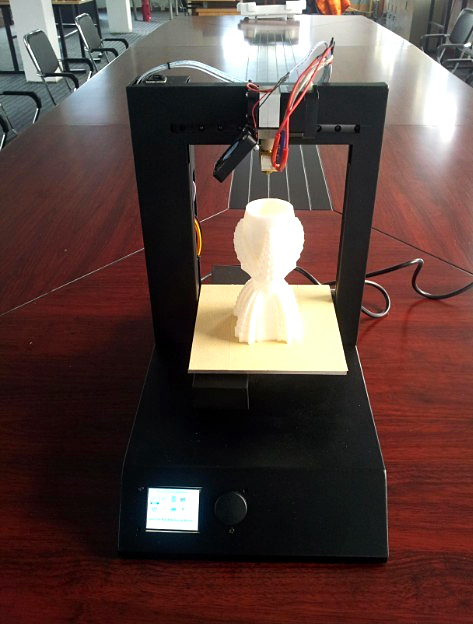 Just like 3D printing can assemble different inorganic materials together into actual products, the process of bioprinting can assemble cells, proteins, and hydrogels into living structures. Although scientists in regenerative medicine initially had been constructing tissues manually to bring the technologies of the field to patients, it soon became obvious that the process needed to be automated, as the by‐hand approach was arduous, time‐consuming, technically demanding, and expensive. Bioprinting had the potential to offer several advantages, such as reproducibility, precision, automation, scalability, and lower costs; features that could eventually allow the delivery of tissues on demand.
Just like 3D printing can assemble different inorganic materials together into actual products, the process of bioprinting can assemble cells, proteins, and hydrogels into living structures. Although scientists in regenerative medicine initially had been constructing tissues manually to bring the technologies of the field to patients, it soon became obvious that the process needed to be automated, as the by‐hand approach was arduous, time‐consuming, technically demanding, and expensive. Bioprinting had the potential to offer several advantages, such as reproducibility, precision, automation, scalability, and lower costs; features that could eventually allow the delivery of tissues on demand.
The modern era of bioprinting commenced in the early years of the 21st century with the appearance of the inkjet bioprinter. Progress since has been remarkable, as can be judged by the steadily increasing number of publications and professional meetings devoted to the topic or by the number of Google‐search entries on the subject. Inkjet bioprinting was soon followed by other specialized formulations of the process (i.e., extrusion, acoustic, laser, and liquid bioprinting). With the appearance of commercial entities, the field has matured beyond basic academic research.
Inkjet bioprinting was soon followed by other specialized formulations of the process (i.e., extrusion, acoustic, laser, and liquid bioprinting). With the appearance of commercial entities, the field has matured beyond basic academic research.
Unfortunately, as with any new technology, a number of forward‐looking statements were made and erroneously interpreted as the then prevailing reality. By the time the general public became aware of bioprinting, 3D printing with inanimate materials had already produced a myriad of useful products expeditiously. Thus, many could expect that bioprinting, being a specific application of the more general technology, would deliver equally versatile and easy‐to‐manufacture living biological products; the field of 3D bioprinting quickly captured the public's imagination. Just like toys could be printed with the push of a button, many thought, tissues and organs would be printed in a similar manner. However, nothing could have been further from the truth.
The fabrication of tissues by hand is complex, but the conversion of the technology to 3D bioprinting compounds the complexity. The printing of biological products implies a number of challenges specific to living matter. For example, whereas printing nonliving matter results in a useful product as soon as printing is complete, this is not the case when cells are involved. Bioprinters deliver bioink units, the analogues of the inorganic ink drops. These delicate structures, prepared in advance, are composed of cells and cell‐supporting materials. The latter are typically some sort of biocompatible hydrogel, a novel material, specifically developed for the cell types to be printed and playing the role of a temporary extracellular matrix during printing. The cells within the bioink units have to survive the process of going through fine nozzles. This imposes stringent requirements on the biomechanical and architectural properties of the bioink units. The discrete bioink units need to self‐assemble into useful biological constructs postprinting. This process, referred to as maturation, is governed by biology and requires time. During maturation the printed construct must be maintained in bioreactors that provide the environment to keep it alive. Numerous conditions and parameters need to be fine‐tuned to eventually produce a tissue or organ that has the needed compositional integrity, 3D organization, and adequate properties for the desired function and implantation into the patient. If the correct conditions for maturation (e.g., temperature) are not provided, no useful product emerges. In short, 3D bioprinting is intricate and multifaceted.
This process, referred to as maturation, is governed by biology and requires time. During maturation the printed construct must be maintained in bioreactors that provide the environment to keep it alive. Numerous conditions and parameters need to be fine‐tuned to eventually produce a tissue or organ that has the needed compositional integrity, 3D organization, and adequate properties for the desired function and implantation into the patient. If the correct conditions for maturation (e.g., temperature) are not provided, no useful product emerges. In short, 3D bioprinting is intricate and multifaceted.
The above discussion may suggest that we might in vain hope for the anticipated benefits to be delivered by bioprinting in regenerative medicine, replacement organs, and other domains. This, however, is not necessarily the case; it all depends on one's realistic expectations. In our view, bioprinting will bring about innovation in several areas, some already under way.
As bioprinting allows for the construction of anatomically and physiologically accurate 3D biological structures, it is poised to advance the drug development process. Tissue models, such as liver or cardiac organoids fabricated with human cells may precede animal trials to test for efficacy and toxicity. Bioprinted tissues can be interconnected (e.g., liver, heart, kidney, etc.) to test drugs on a body‐on‐a‐chip model before the start of human clinical trials. With improvement of such models, eventually animal trials can be reduced and, many of us hope, perhaps even eliminated. On the therapeutic side, bioprinting will likely follow the same sequence as with hand‐made organs, achieving clinical success first with the least complex tissues, such as skin, that are already being delivered, even if not yet shelf‐ready.
Tissue models, such as liver or cardiac organoids fabricated with human cells may precede animal trials to test for efficacy and toxicity. Bioprinted tissues can be interconnected (e.g., liver, heart, kidney, etc.) to test drugs on a body‐on‐a‐chip model before the start of human clinical trials. With improvement of such models, eventually animal trials can be reduced and, many of us hope, perhaps even eliminated. On the therapeutic side, bioprinting will likely follow the same sequence as with hand‐made organs, achieving clinical success first with the least complex tissues, such as skin, that are already being delivered, even if not yet shelf‐ready.
In the more distant future, with further progress in large‐scale cell culture, bioprocess engineering, and genetic strategies, it is possible that we will be able to design specific printable living structures that are not even conceivable today. Tissues printed with gene‐edited cells from the diseased patient to achieve a normal endpoint or combination of extended bioprinted tissue units functionally interconnected similarly to that in the human body are examples that could lead to unforeseen progress in regenerative medicine.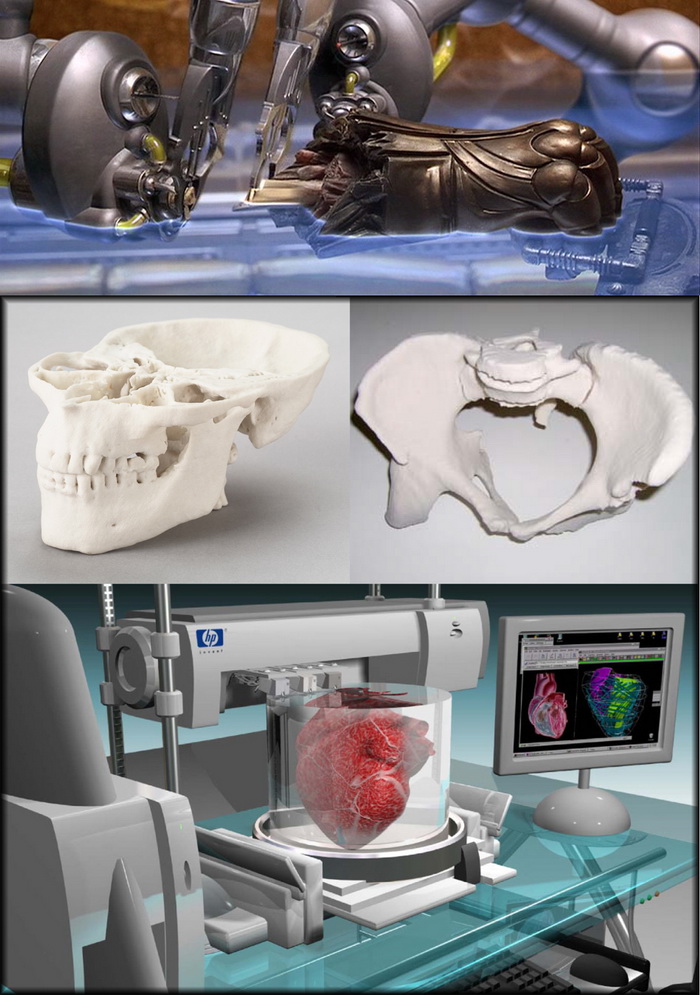 Bioprinting offers many promising opportunities. However, patience and perseverance are needed to realize the full potential of the technology.
Bioprinting offers many promising opportunities. However, patience and perseverance are needed to realize the full potential of the technology.
Disclosure of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
•
Dr. Atala is the Editor‐in‐Chief of Stem Cells Translational Medicine and Director of the Wake Forest Institute for Regenerative Medicine, and the W. Boyce Professor and Chair of Urology at Wake Forest University. Dr. Atala is a practicing surgeon and a researcher in the area of regenerative medicine. His work focuses on growing human cells, tissues and organs. Dr. Atala heads a team of over 450 physicians and researchers. Over twelve applications of technologies developed in Dr. Atala's laboratory have been used clinically.
•
Dr. Forgacs is a physicist turned tissue engineer turned innovator and entrepreneur. He received his physics training at the Eötvös Loránd University, Budapest, Hungary. His academic affiliations include the George Vineyard Chair in Biophysics at the University of Missouri‐Columbia and the Chanderna‐Stirkey Chair in Theoretical Physics at Clarkson University, where he also served as the Director of the Shipley Innovation Center. He is the scientific founder of Organovo, Inc., Modern Meadow, Inc., and Fork & Goode, Inc., and serves as the Chief Scientific Officer of the latter. He is a pioneer in methods of building living structures, in particular by bioprinting. The technologies he has developed have been applied to drug development and testing and the engineering of biomaterials of animal origin, such as leather in an environmentally friendly and ethically conscious manner. Dr. Forgacs has been recognized by numerous awards. In particular, he is a member of the National Academy of Innovators and was named as one of the “100 most innovative people in business in 2010” by FastCompany.
His academic affiliations include the George Vineyard Chair in Biophysics at the University of Missouri‐Columbia and the Chanderna‐Stirkey Chair in Theoretical Physics at Clarkson University, where he also served as the Director of the Shipley Innovation Center. He is the scientific founder of Organovo, Inc., Modern Meadow, Inc., and Fork & Goode, Inc., and serves as the Chief Scientific Officer of the latter. He is a pioneer in methods of building living structures, in particular by bioprinting. The technologies he has developed have been applied to drug development and testing and the engineering of biomaterials of animal origin, such as leather in an environmentally friendly and ethically conscious manner. Dr. Forgacs has been recognized by numerous awards. In particular, he is a member of the National Academy of Innovators and was named as one of the “100 most innovative people in business in 2010” by FastCompany.
Anthony Atala, bioengineer on 3D printing of organs, stem cells and micro hearts
One way is to 3D print new organs from the recipient's own cells.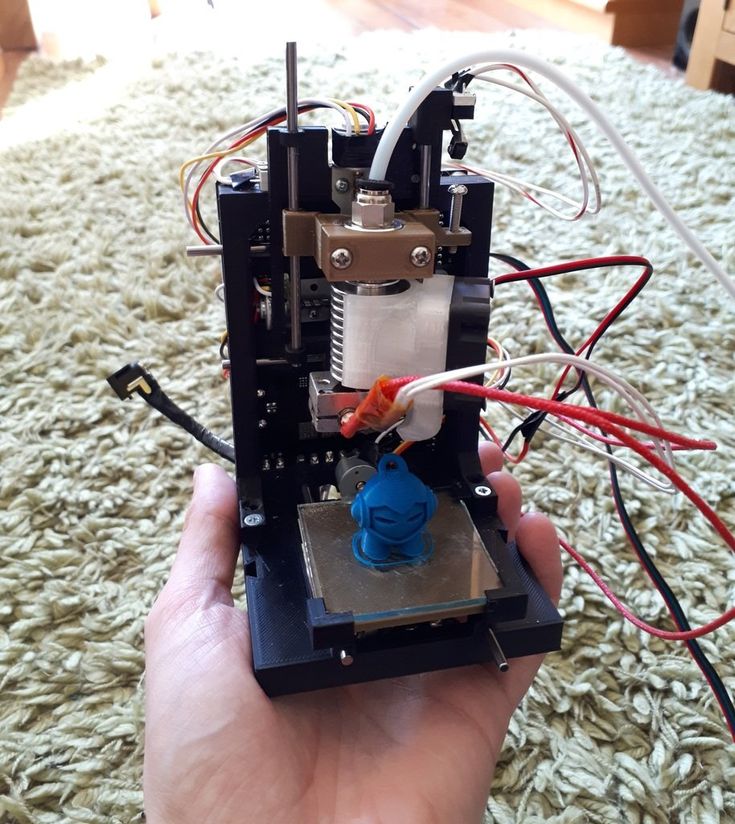 But despite the success - doctors are already transplanting printed skin and blood vessels, there are still problems in the technology. Entire organs with a circulatory system are overly complex, and sometimes patients require an organ they don't have (such as a kidney) or is severely genetically damaged. In this case, scientists are trying to use stem cells. Hi-Tech visited the Healthy Moscow Assembly and recorded a speech by Anthony Atala, director of the Wake Forest Institute of Regenerative Medicine, about the future of transplantation, the search for a new type of stem cells, and testing drugs on microorganism.
But despite the success - doctors are already transplanting printed skin and blood vessels, there are still problems in the technology. Entire organs with a circulatory system are overly complex, and sometimes patients require an organ they don't have (such as a kidney) or is severely genetically damaged. In this case, scientists are trying to use stem cells. Hi-Tech visited the Healthy Moscow Assembly and recorded a speech by Anthony Atala, director of the Wake Forest Institute of Regenerative Medicine, about the future of transplantation, the search for a new type of stem cells, and testing drugs on microorganism.
Start regeneration
The world's first successful organ transplant occurred in 1954 when surgeon Joe Murray implanted a kidney into a patient. Thanks to this, many people were subsequently saved. But as before, these organs are not enough, and, in addition, there is a reaction of rejection of the transplant. Therefore, we are seeing a huge shortage of organs: over the past 10 years, the number of patients who need transplants has doubled, while the number of procedures itself has increased by less than 1%.
An average of 100,800 organ transplants are performed worldwide every year. The most common transplants are kidneys (69,400 operations), liver (20,200), heart (5,400), lungs (2,400) and pancreas (2,400). Donation can be related and posthumous, when the desired organ is taken from a corpse. At the same time, in Russia, for example, the average waiting time for a donor kidney is 1.5-2 years. The Sklifosovsky Research Institute performs about 200 surgeries annually, while there are approximately 500 people on the waiting list.
Nature created cells in such a way that they always know what to do. They have the ability to regenerate, every cell has that potential. Skin cells are renewed every two weeks, intestinal cells within two weeks, and brain cells every ten years. The problem is that we do not regenerate tissue when disease, scar or injury occurs. At this point, regeneration stops and this is where regenerative medicine can help. We take very small muscle tissues from the patient, then process these cells and place them in the area where the damaged muscle is located. This can also be applied to patients with burns: in this case, we take a small sample of the patient's skin, then process the cells and simply spray them on the damaged areas. Moreover, if the patient is injured, it is necessary to first treat him, get rid of the infection and wait for time so that he himself is ready for treatment.
This can also be applied to patients with burns: in this case, we take a small sample of the patient's skin, then process the cells and simply spray them on the damaged areas. Moreover, if the patient is injured, it is necessary to first treat him, get rid of the infection and wait for time so that he himself is ready for treatment.
Grow a new organ
Instead of cells, you can use the so-called substrate - a kind of building frame. Its materials are very similar to those of seams. They dissolve in a few months, are safe for humans and cells. We take a small tissue sample from the patient, then process these cells outside of the body, culture them, use a scaffold to make them tubular, and implant that into the patient. The whole process takes approximately 30 days. The same applies to blood vessels. We put these cells on the material, then we train this organ. When the compressions become what we need, the vessels are implanted in people. The most complex organ is a solid organ with blood circulation, like the heart, kidney and liver, because there are different types of tissues, and they all have a lot of blood vessels.
Simple fabrics are easiest to grow. In clinical practice, the method of skin regeneration with the help of special hydrogels or cells of the patient himself is already being used.
Gordana Vunjak-Novakovic at Columbia University grew a fragment of a skull bone by seeding the frame with stem cells.
At Johns Hopkins University, doctors removed a tumor-affected ear and part of the skull from a patient. Taking cartilage tissue from the chest, vessels and skin, they grew a new ear on her arm, and then transplanted the artificial organ into place.
Successful experiments on the cultivation and transplantation of blood vessels took place at the universities of Gothenburg (Sweden) and Rice (USA). There are also examples of growing muscles, blood cells, bone marrow and teeth.
As far as the cultivation of complex organs is concerned, experiments are still carried out mainly on animals. However, there are also examples of successful transplants of artificially grown organs in humans. Anthony Atala has been performing surgeries to implant a bladder grown from patient cells for several years. In 2008, the Italian surgeon Paolo Macchiarini transplanted a trachea grown on the basis of a donor scaffold. True, a few years later, Macchiarini found himself at the center of a scandal - six of his patients died, and, according to scientific reports, he embellished his achievements. Published in May 2015, the results of an independent examination conducted by the chief surgeon of Uppsala University, Bengt Gerdin, confirmed that Macchiarini falsified the results of his research and committed scientific fraud.
Anthony Atala has been performing surgeries to implant a bladder grown from patient cells for several years. In 2008, the Italian surgeon Paolo Macchiarini transplanted a trachea grown on the basis of a donor scaffold. True, a few years later, Macchiarini found himself at the center of a scandal - six of his patients died, and, according to scientific reports, he embellished his achievements. Published in May 2015, the results of an independent examination conducted by the chief surgeon of Uppsala University, Bengt Gerdin, confirmed that Macchiarini falsified the results of his research and committed scientific fraud.
Advanced Cell Technology in 2002 grew a miniature cow kidney 5 cm long using cloning technology, taking cells from the ear of an animal. The kidney was implanted next to the main organs, and it began to successfully produce urine.
There is also a positive experience of growing and transplanting livers in laboratory rats (University of Massachusetts) and lungs in pigs (University of Texas).
The vessels of transplanted organs are very small. We already started this work 30 years ago, but we did not have the technology. They began to think about how to take the organs of people who died and use them again. The liver was removed from the deceased patient and, as it were, washed from the inside. Two weeks later, the liver still looked like a liver, but there were no cells inside. However, we were able to preserve the vascular tree, such a skeleton of the liver. Then they took the patient's cells, grew them, and placed them on this skeleton. We create tissue from the patient's body and thus treat him. Therefore, there is no immune response at all. This is a very big plus of regenerative medicine.
Even from a very bad organ, we can get good cells with the help of a biopsy. But we cannot do this with genetic diseases, because the defect will be in the entire tissue. There are other technologies here - we take cells from this patient, correct the defects, heal these cells, as it were, and then work on the same strategy. So far, unfortunately, this is experimental, but there is still hope that genetic diseases can also be treated.
So far, unfortunately, this is experimental, but there is still hope that genetic diseases can also be treated.
We make sure to follow the life of our patients for at least 5-8 years after transplantation. We must make sure that everything will be fine, only then it will be possible to say that this technology has worked and the transplanted organs are functioning normally.
Organ printing and drug testing
You can print a miniature heart and it will start contracting in two hours. Six years ago, we started using 3D printing because it was necessary to scale these technologies - before that, we did everything by hand. But the organs obtained with the help of printing did not have such integrity to be implanted into the body. Then we began to develop more specific printers that could create human tissue. And they worked on it for 14 years.
The first experiments in bioprinting were carried out on conventional household 3D printers, which were upgraded in the field. In 2000, Thomas Boland set up Lexmark and HP machines so that they could print DNA fragments, and in 2003 he patented the technology.
In 2000, Thomas Boland set up Lexmark and HP machines so that they could print DNA fragments, and in 2003 he patented the technology.
Several companies are now involved in organ printing. Bioengineers at Organovo have developed a technology that allows them to print liver tissue. They also printed kidneys that last for two weeks. So far, such organs are used only for testing medical products, but the creators do not exclude that they will soon begin developing equipment for printing donor organs.
Russian bioengineers from 3D Bioprinting Solutions developed the FABION 3D printer and conducted a successful experiment to print the thyroid gland and transplant it into an experimental mouse.
Fripp Designs printers, developed at the University of Sheffield, print prosthetic eyes. The same team is developing 3D printing technologies for noses, ears and chins.
Part of the equipment is produced for customers' own needs and is not intended for sale (FABION, Organovo's NovoGen MMX).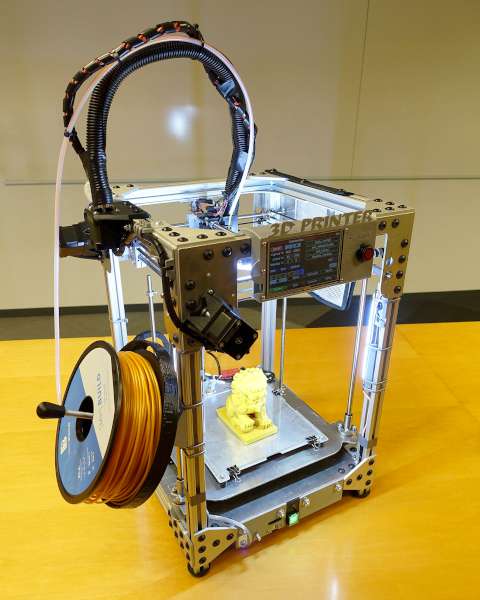 Prices for commercial bioprinters start from $10,000 (BioBots) and €5,000 (CELLINK Inkredible) to $200,000 and up (EnvisionTEC's 3D Bioplotter, RegenHU's 3DDiscovery).
Prices for commercial bioprinters start from $10,000 (BioBots) and €5,000 (CELLINK Inkredible) to $200,000 and up (EnvisionTEC's 3D Bioplotter, RegenHU's 3DDiscovery).
There are five interesting criteria for a 3D printer to print organs. Firstly, they have very small nozzles, they can reach up to 2 microns - this is 2% of the diameter of a human hair. Secondly, this printer gives us precision, we can lay out cells where they are actually needed. The third is bio-ink, a liquid that passes through the nozzle. And then when it becomes gelatin, it already functions like normal tissue. The next criterion is microchannels, they provide nutrition to the central part of the cells. In fact, these are blood substitutes. And finally, software that allows you to have a three-dimensional image. In this way, we understand what is happening in the body and create the structure necessary for a given organ. To do this, we take digital data from X-rays and use them in such a way as to create a structure for this particular defect in a particular patient.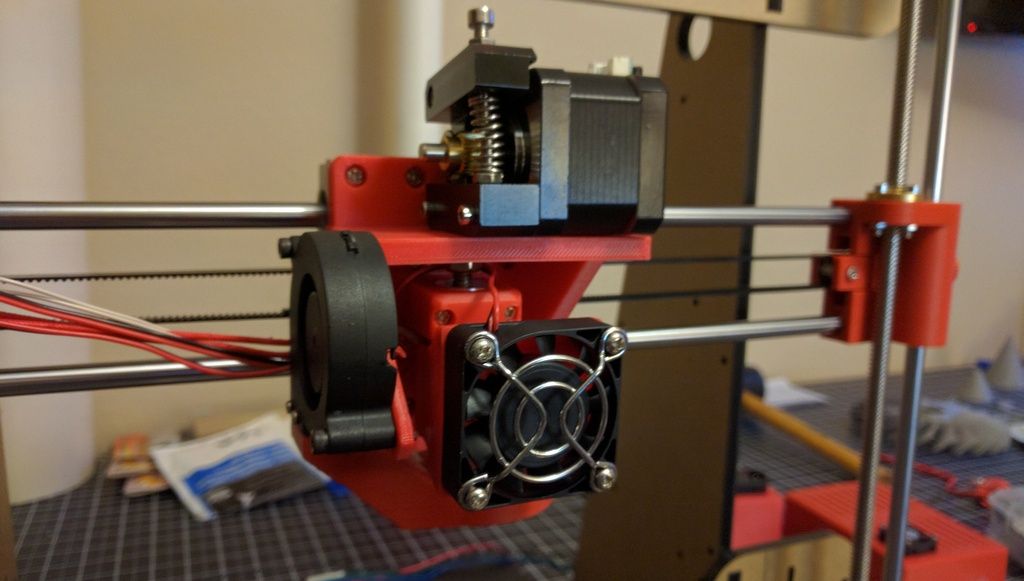
We have two certified systems for printing human organs. They are approved by the FDA (Food and Drug Administration in the USA - "Hitech"). For the past six years, we've been using the printer to create what's called a body-on-a-chip program. Now it is at the development stage, because it is necessary to ensure the viability of these organs, but in general we can make miniature lungs, heart, blood vessels and connect this entire system on chips. We can also create miniature organs the size of a pinhead and see how these organs react to drugs. For example, if a drug speeds up the heart rate, it will speed up the heart rate in our miniature heart. In this way, side effects of drugs that are not detected by other tests can be detected.
Avoid side effects
Printed miniature organs can be used to test drugs. For example, the drug Hismanal, which has been on the market for 11 years around the world. This antipsychotic has also been used as an antihistamine.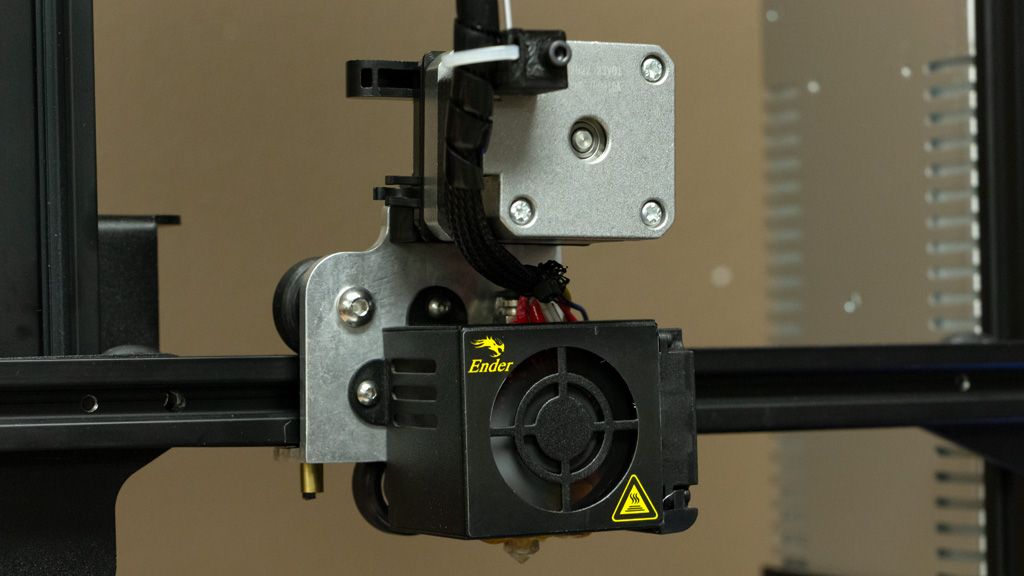 After some time of its use, it became clear that many patients experience side effects associated with disruption of the heart. When the drug was tested on a cell, there were no problems; when it was tested on animals, there were no problems. When the clinical studies of the first, second and third stages were carried out, nothing happened. We took this drug, used it on our organs on chips, and after a week it became clear that this drug is toxic to the heart.
After some time of its use, it became clear that many patients experience side effects associated with disruption of the heart. When the drug was tested on a cell, there were no problems; when it was tested on animals, there were no problems. When the clinical studies of the first, second and third stages were carried out, nothing happened. We took this drug, used it on our organs on chips, and after a week it became clear that this drug is toxic to the heart.
This is due to the fact that everyone reacts differently to drugs, everyone is genetically different, and the same drug will be processed differently. Everyone has a different diet, different living conditions, different health problems. This acts as a hindrance to understanding what the drug actually does to the organs. And if we remove all these interferences and look directly at how the drug acts on the organs, we can immediately detect toxicity.
Today we are developing a system that we call "body on a chip".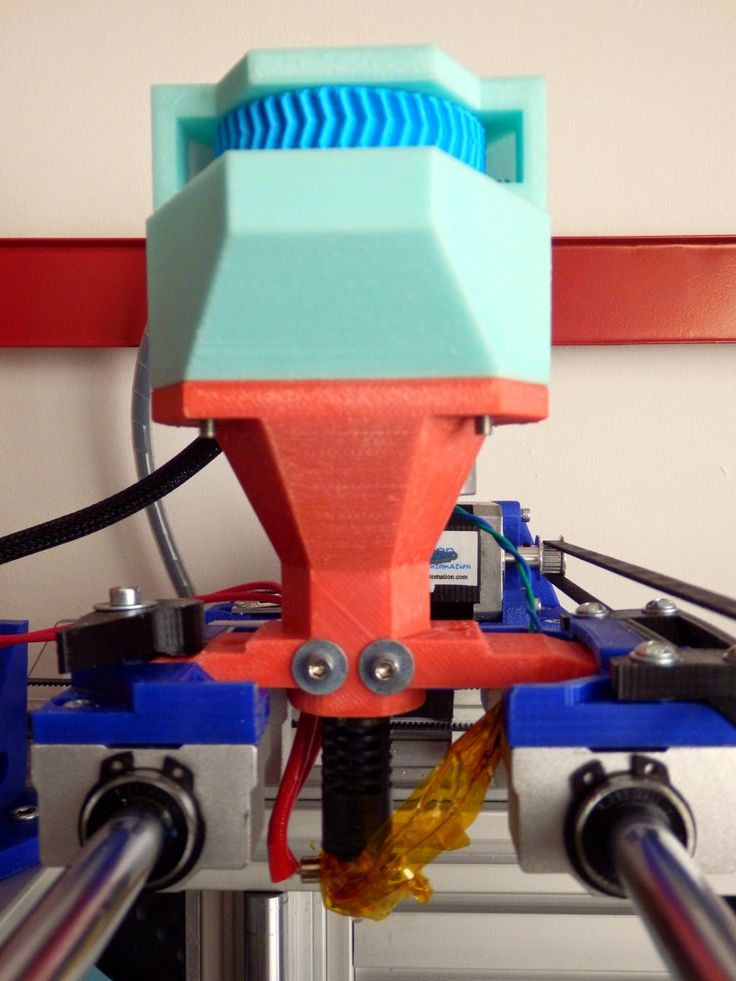 In particular, it will help reduce the toxicity of drugs - for example, to work with cancer patients. We can take a small cancer cell and grow it, and then test chemotherapy on a chip before giving it to a patient. We had a patient with melanoma, he was on chemotherapy for six months, a lot of money was spent, and the tumor only grew. We tested a drug that was not considered, and the patient began to receive it. Two weeks later, the patient for the first time said that his condition was improving, and the doctor noted that the tumor was decreasing. Thus, it is very useful to test a drug before giving it to a patient.
In particular, it will help reduce the toxicity of drugs - for example, to work with cancer patients. We can take a small cancer cell and grow it, and then test chemotherapy on a chip before giving it to a patient. We had a patient with melanoma, he was on chemotherapy for six months, a lot of money was spent, and the tumor only grew. We tested a drug that was not considered, and the patient began to receive it. Two weeks later, the patient for the first time said that his condition was improving, and the doctor noted that the tumor was decreasing. Thus, it is very useful to test a drug before giving it to a patient.
Stem cells: creating something that does not exist
When it comes to growing an organ that a patient has never had or has lost, stem cells can be used. Usually, in order to grow a kidney, we take a kidney cell, in order to grow a urethra, we take urethra cells. But in the case of stem cells, we can take one that can become a lung cell, a kidney cell, or a blood vessel cell. There are two main types of stem cells. One of them is human embryonic. They are very powerful, grow and can turn into anything, but they can also form tumors, so it is very difficult to use them. On the other hand, if we talk about these cells in an adult, they can be fat or bone marrow cells, they will not form tumors, but they do not grow as well.
There are two main types of stem cells. One of them is human embryonic. They are very powerful, grow and can turn into anything, but they can also form tumors, so it is very difficult to use them. On the other hand, if we talk about these cells in an adult, they can be fat or bone marrow cells, they will not form tumors, but they do not grow as well.
The term "stem cell" was first used by the German scientist Valentin Haaker at the end of the 19th century. In 1909, the Russian scientist Alexander Maksimov suggested that there are cells in the body that remain unchanged, but at the right time they can change the program and turn into cells of a different type.
This theory was confirmed in the 60s of the last century. Americans James Till and Ernest McCulloch irradiated mice with a lethal dose of radiation, and then transplanted them with a healthy individual's blood stem cell. It turned out that in this way it is possible to restore blood and save mice from death. From 19For 64 years, this method has been used in the treatment of blood cancer: patients first destroy their own blood cells, and then transplant healthy stem cells from a donor. The efficiency of this method reaches 70–80%.
From 19For 64 years, this method has been used in the treatment of blood cancer: patients first destroy their own blood cells, and then transplant healthy stem cells from a donor. The efficiency of this method reaches 70–80%.
In 1981, Martin Evans and Matthew Kaufman, along with Gale Martin, isolated embryonic stem cells from mouse embryos. These cells could exist for an indefinitely long time outside the body without changing their properties, and if they got into certain conditions, for example, back into the body, they could turn into tissues.
In 1999, Science magazine ranked the discovery of stem cells as one of the three greatest discoveries in biology, following the deciphering of DNA and the Human Genome Program.
It has long been believed that once a stem cell has turned into a tissue cell, it is impossible to make it a stem cell again. However, in 2006, the Japanese Shinya Yamanaka discovered a way to turn somatic cells back into stem cells. For this, he received the Nobel Prize in 2012.
About 17 years ago we started looking for an alternative source of stem cells. It has been suggested that there is another type of stem cell present in the amniotic fluid and in the placenta that surrounds the baby in the uterus. And we found these very powerful stem cells. They will not form tumors and can develop into the three main categories of tissue that make up our body. These cells can be rapidly grown to sufficient numbers. In this way, we avoid all the limitations of bone marrow cells and other cell types. They are now the subject of a number of clinical studies and are not yet widely used.
I don't want you to think that all the problems are already solved, and you can just take and print organs on the printer. It will take decades for these technologies to develop. It is very difficult and it takes a long time for us to be able to develop the very recipe that will allow technologies to work optimally. In addition, these are expensive technologies, they will be difficult to replicate, but we can definitely say that they have potential. And for us, this is the promise of regenerative medicine - to improve the lives of patients.
And for us, this is the promise of regenerative medicine - to improve the lives of patients.
Source
3D printing of organs, Wake Forest Anthony Atala, bioengineer, transplantology, bioprinting, DNA printing, Organovo, 3D printing of liver tissue, 3D Bioprinting Solutions, FABION, 3D printing of the thyroid gland, 3D printing of noses, ears, chins , BioBots, CELLINK Ink
Printing organs: how ears, skin and noses are made with a 3D printer
- Natalka Pisnya
- BBC Russian Service, USA
Image copyright, Masela family archive
Photo caption,Luc Masela with his parents one month after the artificial bladder transplant. year 2001.
Luc Masela, now 27, is an athlete with a degree in economics, works for a large exhibition company, travels a lot and recently met, in his words, "the most beautiful girl in the world.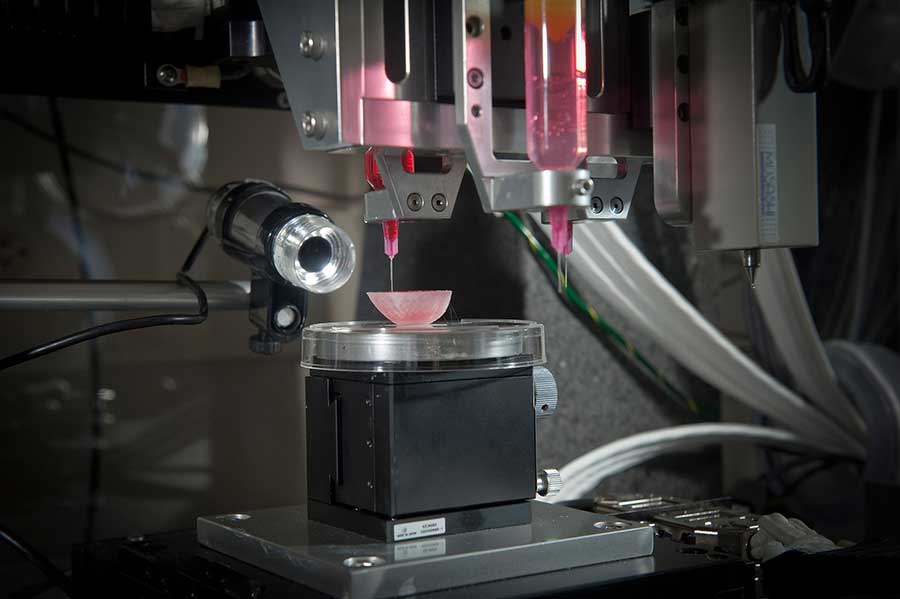 " Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
" Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
Luke was born with spina bifida - and although he was able to walk, his bladder was severely damaged. By the age of 10, he almost did not leave hospitals: due to improper functioning of the bladder, fluid began to return to the boy's kidneys, doctors diagnosed an irreversible pathology of the organ.
You need JavaScript enabled or a different browser to view this content
Video caption,"3D printed" organs are here
Doctors offered the family two solutions: lifelong dialysis or the creation of a new bladder from a segment of the intestine. This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
The urologist in charge of the boy suggested that Masela's family take part in an experimental program to grow a new bladder from his own cells. Then, in 2001, it sounded like science fiction: only nine people took part in the program before Luke. Despite this, his family agreed.
Then, in 2001, it sounded like science fiction: only nine people took part in the program before Luke. Despite this, his family agreed.
"The essence of the operation was reduced to two stages: first, a piece of bladder tissue was taken from me, and over the next two months, cells were grown in the laboratory in order to grow a new healthy bladder from them," says Luke.
Photo copyright, Masela family archive
Photo caption,Luc Masela, 17 years after the artificial bladder transplant
Next was the transplant operation, which, according to him, lasted 16 hours. “I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
The operation was performed by Dr. Anthony Atala, Pediatric Regenerative Surgeon.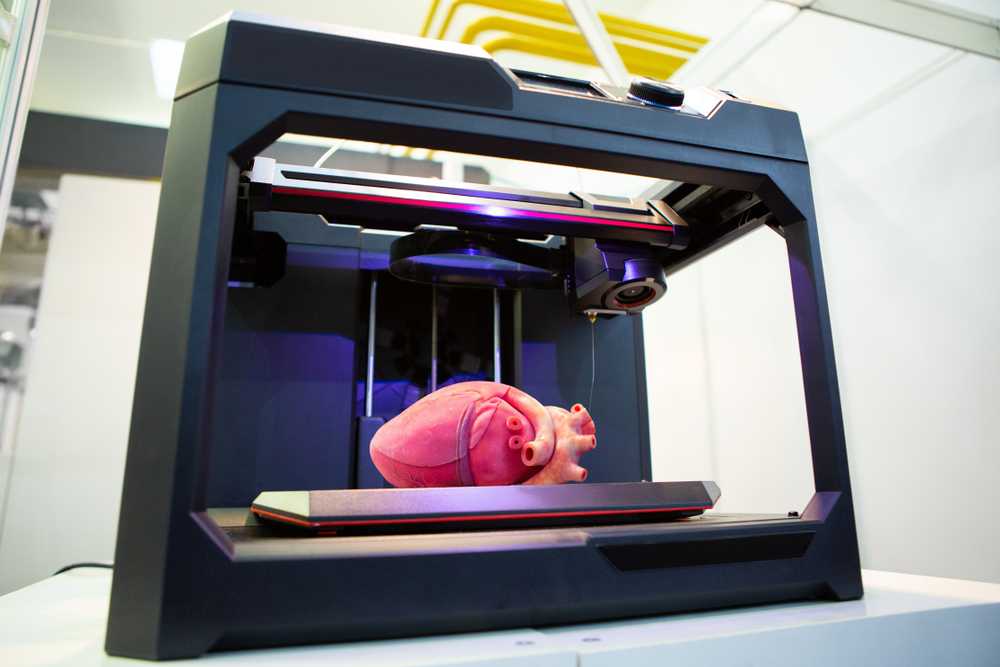 In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like a normal organ, taking root thanks to Luke’s own cells.
In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like a normal organ, taking root thanks to Luke’s own cells.
- An animal capable of regrowing its head
- The birth of a chimera: why do scientists need a human-animal hybrid?
- Swedish company 3D prints body parts
Luke and Dr. Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.
The professor took charge of the Wake Forest Institute of Regenerative Medicine in North Carolina in those 10 years, but he never forgot about Luke: his bladder was one of the most challenging and most successful projects in his early practice.
By 2018, Atala won the Christopher Columbus Prize for "work on a discovery that will have a significant impact on society"; The Times and Scientific American magazines at various times named him "Physician of the Year", he was also recognized as "one of the 50 scientists on the planet who in the next 10 years will change the way we live and work."
How to print a new face
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
In the mid-2000s, Atala's team turned their attention to an ordinary household 3D printer and wrote special software for it, later specialized machines were created for the laboratory. Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
One of the team's latest achievements is ears and noses grown outside the human body.
The main customer and sponsor of Atala's developments is the US Department of Defense, and many of the patients are military victims of military operations.
It works like this: first, a CT scan of the ear or nose is done. One of Atala's assistants, Joshua Corpus, jokes that at this stage, people often ask to "improve" the shape of the nose if they thought theirs was too wide or hooked, and the ears if they were too wide.
After that, a special computer code is written, and the printing of the basis of the organs begins.
For this, a bioresorbable polymer, polycaprolactam, is used. At the same time flexible and durable, in the human body it disintegrates within four years.
After printing, the layers of polycaprolactam resemble lace; after transplantation, their place will be taken by a person's own cartilage tissue in a few years.
Polycaprolactam is then saturated with a gel created from the patient's cells, cooled to -18 degrees Celsius - so the cells, according to scientists, are not damaged, they are "alive and happy."
Image caption,Printing a test kidney sample on a bioprinter
In order for the polymer and gel structure to take shape and become something more durable, ultraviolet light is used in the laboratory - it does not damage cells.
The future implant is printed for 4-5 hours, then it is finally formed and inserted under the epidermis.
Skin can also be grown: children affected by fires were the first to take part in the early trials of Atala - after the "printing" of the skin, scientists observed the patients for several more years. The new skin did not crack, did not burst, and grew with the children.
The most difficult work, according to the scientist, is facial wounds: it is not enough just to stretch the skin, you need to accurately calculate the geometry, align swelling, bone structure, and understand how a person will look after that.
In addition to the skin and ears, Atala can "print" the bones of the jaws, grow blood vessels and cells of some organs - the liver, kidneys, lungs.
This technology is especially appreciated by oncologists: on the basis of patient cells, it is possible to recreate the body's response to various types of chemotherapy and observe the reaction to a particular type of treatment in the laboratory, and not on a living person.
But the liver, kidneys, lungs and heart are still being tested. Atala says he raised them in miniature, but creating organs from various tissues to real size requires a lot of additional research.
But, according to him, cells were grown in the laboratory and a vagina was created for a girl who was born several years ago with a congenital deformity of the genital organs - several years have passed since the transplant.
Image caption,Bioprinted polycaprolactam ear implant base
Atala smiles and adds that his team is also working on a working penis. This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
Among others, Igor Vasyutin, a Russian post-graduate student of the First Moscow State Medical University (MGMU) named after Sechenov, is working on this under laboratory conditions. He is a cell biologist, Atala's right hand.
Vasyutin has been in the USA for about a year - he came on an exchange. He is ready to talk about the behavior of stem cells for hours, but becomes less verbose when it comes to Russian science.
Vasyutin's alma mater has not reached mass regeneration of human organs and is still training on animals: local scientists "printed" a mouse thyroid gland on a 3D printer.
They, however, also study human organs. According to the head of the Institute of Regenerative Medicine at MSMU Denis Butnar, several years ago the Institute recreated a special engineering design of the buccal mucosa.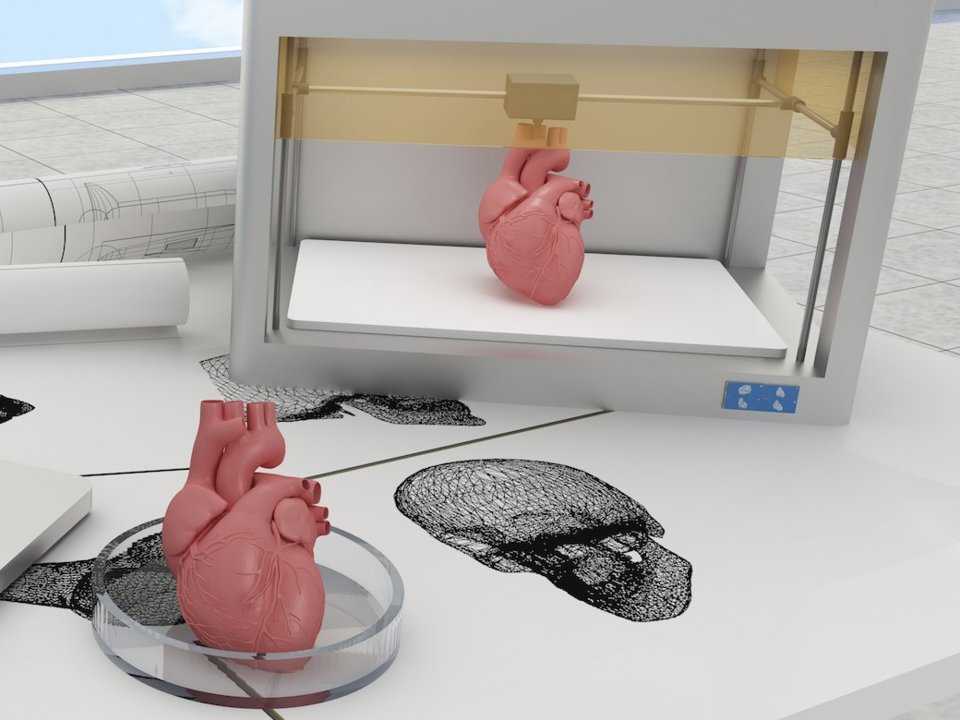 She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
Test specimen of an ear implant under ultraviolet light
In Russia, however, over the past few years, the Italian surgeon-transplantologist Paolo Macchiarini has been practicing - the man who was the first in history to perform a synthetic organ transplant operation - a plastic tube that replaced the patient trachea.
- Paolo Macchiarini: the rise and fall of the famous surgeon
However, seven of his nine patients died, and the breathing tubes implanted in the remaining two subsequently had to be replaced with donor ones.
Several criminal cases were brought against him, including on charges of pressure on patients and fraud, and the leading doctors of the world called Macchiarini's operations "ethical Chernobyl".
Will printed organs replace donors?
At the zenith of his career, Macchiarini argued that a new perspective is opening up for humanity: you can "print" any human organ on a printer, create an engineering structure from it, enriched with the patient's stem cells, and get the perfect prosthesis.
Be that as it may, complex human organs - the liver, kidneys, heart, lungs - have not yet been able to grow any regenerative surgeon.
Bioprinting of the so-called simple organs, however, is already available in the US, Sweden, Spain and Israel - at the level of clinical trials and special programs.
The American government is actively investing in such programs - in addition to Wake Forest, cooperating with the Pentagon, the Massachusetts Institute of Technology also receives significant amounts to recreate the work of the liver, heart and lungs.
Image caption,Skin application test on a burnt wound
According to Professor Jorge Raquela, a gastroenterologist at the Mayo Clinic Research Center, "Bioprinting is one of the most exciting branches of modern medicine, it has huge potential, and the turning point of the most important discoveries is already close."
Meanwhile, Pete Basillier, head of R&D at analytics firm Gartner, insists technology is advancing much faster than understanding the implications of 3D printing.
Such developments, according to Basilière, even if created with the best of intentions, give rise to a set of questions: what will happen when "improved" organs are created, the basis of which will not only be human cells - will they have "superpowers"? Will a regulatory body be created to monitor their production? Who will check the quality of these organs?
More than 150,000 Americans are on the waiting list for organ transplants every year, according to a report from the US National Library of Medicine. Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
- A 3D printer helped a cyclist who lost his jaw
- Genetically modified pigs - human organ donors?
- The world's first child who received both hands transplanted plays baseball
Most Americans are potential donors: upon obtaining a driver's license, they voluntarily answer the question of whether they agree to donate their organs in the event of a car accident or other dangerous incident .