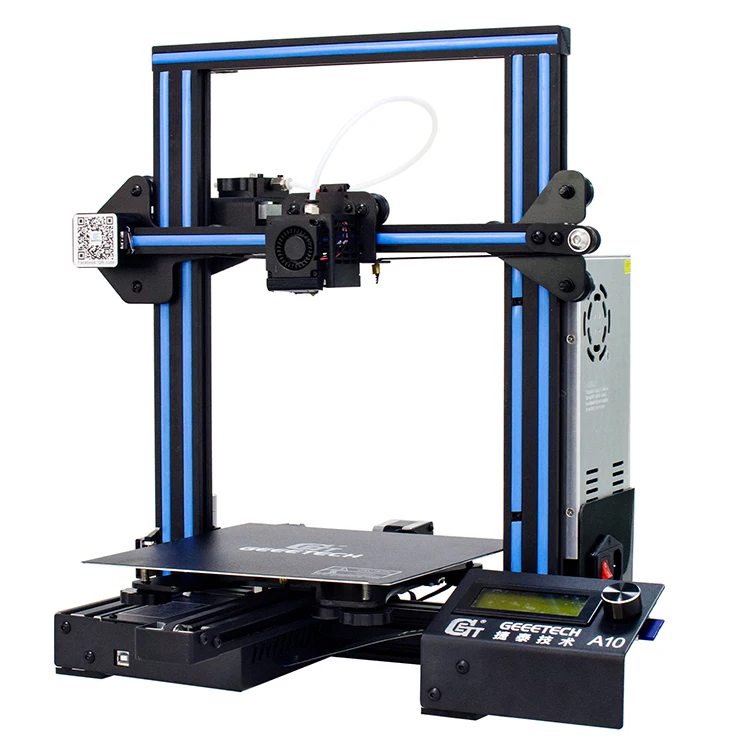
Biofab 4500 3d printer
The first 3D-printed human stem cells
- By John Hewitt on February 6, 2013 at 9:47 am
This site may earn affiliate commissions from the links on this page. Terms of use.
The shortage of transplantable organs has spawned a fascinating science and market. A liver, for example, is often split among two recipients, while for a cystic fibrosis patient in need of two lungs, it is technically preferable to just swap out both the heart and lungs as a combo unit. The extra heart can then be domino donated to a third party. Bioprinting complete organs en masse is a tough proposition because the identity expressed by each component cell must be individually programmed. Then the cells need to be knitted together in a developmentally sound fashion. Researchers in Scotland, land of Dolly, the first cloned mammal, have recently demonstrated the ability to print human embryonic stem cells. Stem cells, of course, are known for a unique feature — they can program themselves.
It was announced at the end of last year, that Autodesk, the makers of CAD software like AutoCAD, would be partnering with a new startup by the name of Organovo to make 3D organ printing a reality. While it is encouraging to see engineering tools rigorously applied to the life sciences, it should be recognized that printing something that looks like an organ does not mean it will actually be an organ. In the short term at least, the main goal of the startup is to produce some tissues which may be able to serve as a testbed for pharmaceuticals. The new stem cell study, published this week in the journal Biofabrication, looks to create tissues pregnant with real organ-producing power, and may prove to be just what the doctor ordered.
So, in 20 years, will replacement organs be printed, grown, or built?
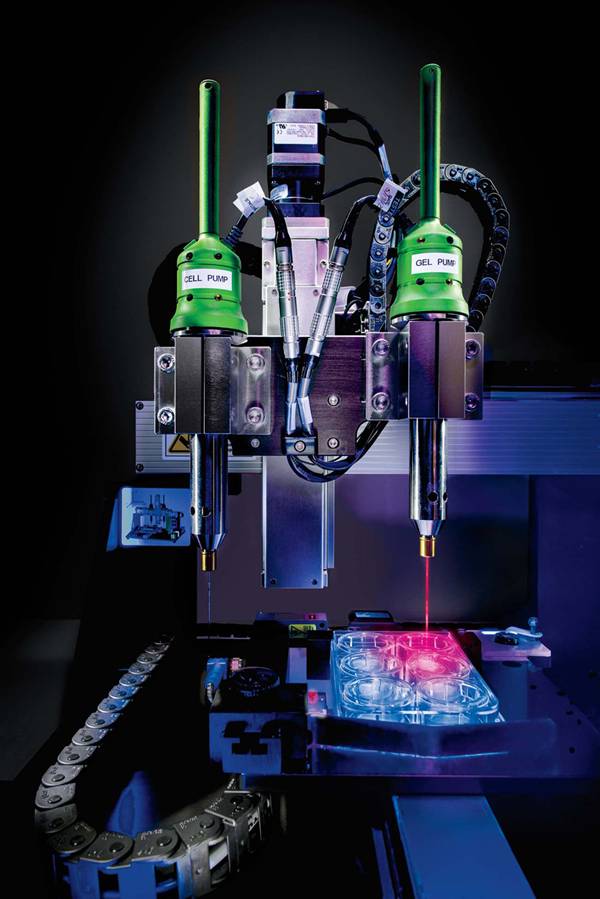
While stem cells from a mouse have been printed before, human stem cells have proven to be a bit more fragile and generally more difficult to work with. Part of the problem is due to subtle differences in the required cellular nutrient environments (think about some dogs getting pancreatitis from eating bacon), and part is also due to the fact that researchers are simply more familiar with the mouse cells.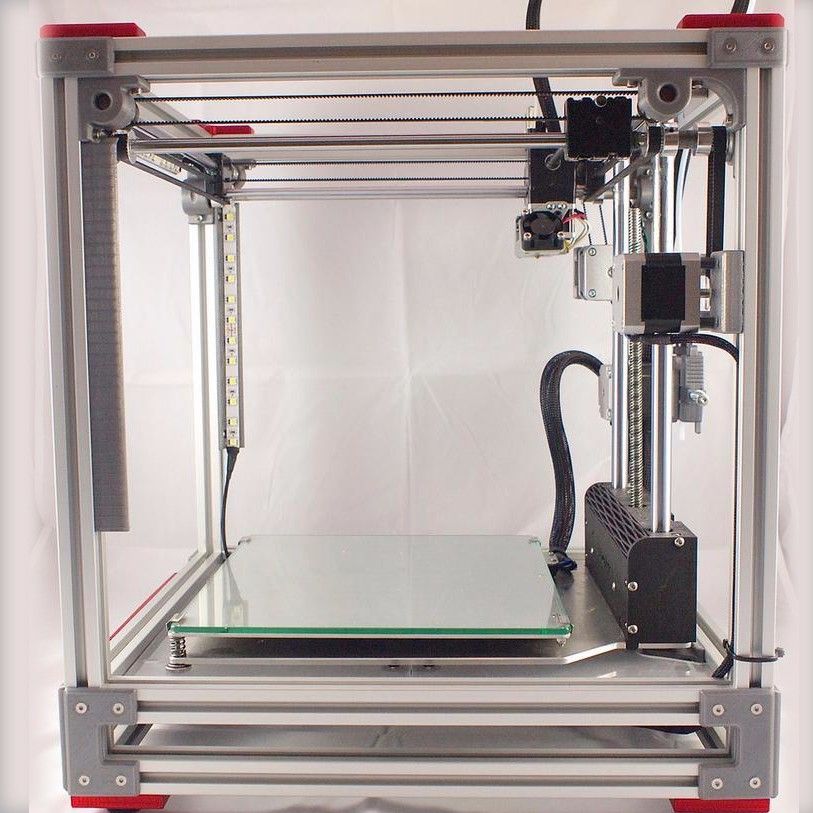 For the specific needs of the Scotland researchers, commercial 3D printers were far too crude, so they built their own by modifying a precision CNC machine that was capable of micron step resolution. Using dual extrusion heads to deliver cells and media, they could deposit cells with just right amount of personal space to make them feel at home and comfortable.
For the specific needs of the Scotland researchers, commercial 3D printers were far too crude, so they built their own by modifying a precision CNC machine that was capable of micron step resolution. Using dual extrusion heads to deliver cells and media, they could deposit cells with just right amount of personal space to make them feel at home and comfortable.
By fine manipulation of the dispensing aperture, extrusion pressure, and viscosity of the bioink, the researchers could print spheroids of cells that varied between five and 140 cells. When a bank of spheroids was complete, they were inverted and the cells could coalesce at the bottom under the influence of gravity. One new technique that would be of great benefit here would be to feed the cells a few ferrite beads and position them instead with maglev manipulation.
Before getting too carried away, there are many important checks that need to be run to make sure the stem cells retain pluripotence after having been traumatically birthed through the extruder.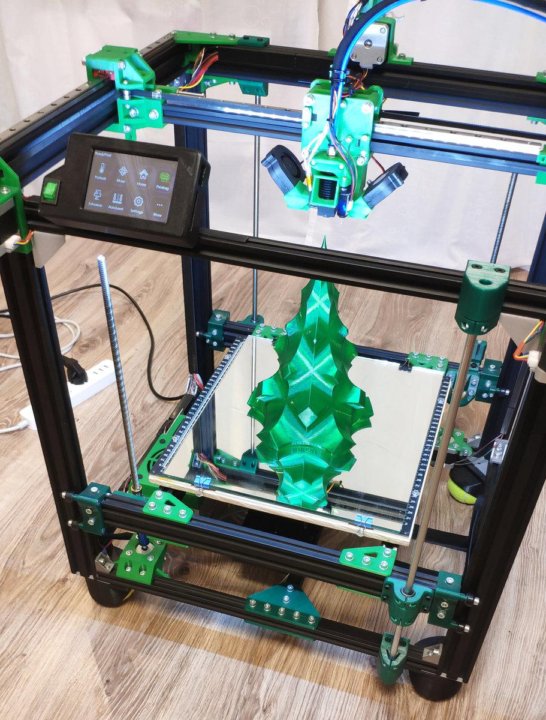 In other words, they may still be alive, but if they have lost the ability to turn into any kind of cell, organs are not going to happen. The researchers did a partial check on this, finding that the cells continued to manufacture a particular control protein that helps keep them in a youthful state. The real test will be how the cells respond when they must compete for oxygen and fuel in a proto-organ matrix that more closely mimics conditions in the body.
In other words, they may still be alive, but if they have lost the ability to turn into any kind of cell, organs are not going to happen. The researchers did a partial check on this, finding that the cells continued to manufacture a particular control protein that helps keep them in a youthful state. The real test will be how the cells respond when they must compete for oxygen and fuel in a proto-organ matrix that more closely mimics conditions in the body.
All too often with cancers, several organs have been infiltrated by tumors but the organs themselves are still functional. When the cancer doesn’t respond to drugs anymore, and traditional surgery is impossible because the critical vasculature has become so gnarled with disease and previous radiation treatments, the patient has typically reached the end of the line. The inevitable merging of 3D print systems with surgical robots will enable in situ repairs that surgeons would never even dream about doing by hand in the span of a single shift, extending the life of these patients.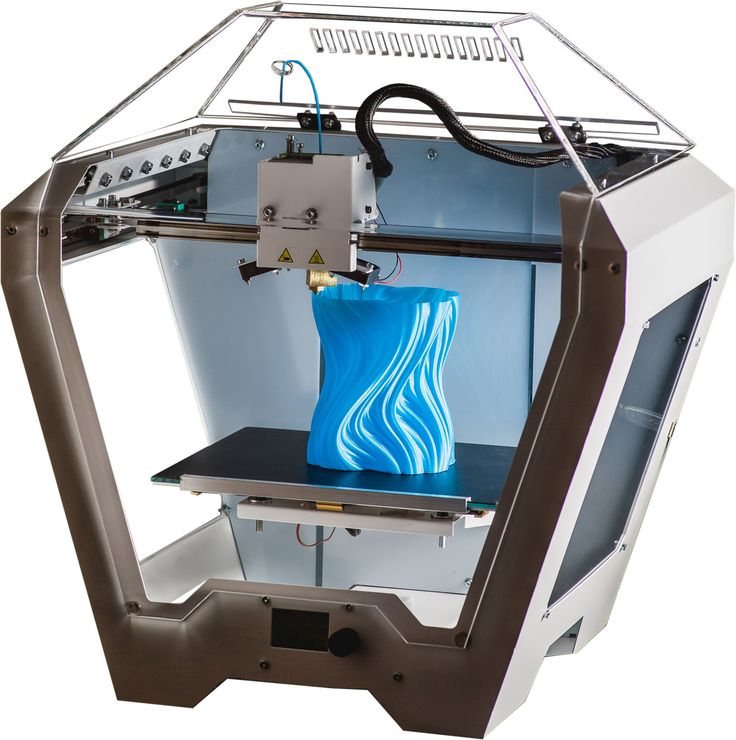 At the extreme, we can imagine an ingenious solution to the cell identity programming problem — the organ is printed inside the patient from a real prototype that is first deconstructed by enzyme, then reconstituted cell-by-cell with the proper local and connections. This is the technology of the future that so many in hospitals wait for today.
At the extreme, we can imagine an ingenious solution to the cell identity programming problem — the organ is printed inside the patient from a real prototype that is first deconstructed by enzyme, then reconstituted cell-by-cell with the proper local and connections. This is the technology of the future that so many in hospitals wait for today.
Now read: The first open-source 3D-printed gun
Research paper: doi:10.1088/1758-5082/5/1/015013 – “Development of a valve-based cell printer for the formation of human embryonic stem cell spheroid aggregates”
Tagged In
This site may earn affiliate commissions from the links on this page. Terms of use.
ExtremeTech Newsletter
Subscribe Today to get the latest ExtremeTech news delivered right to your inbox.
This newsletter may contain advertising, deals, or affiliate links. Subscribing to a newsletter indicates your consent to our Terms of Use and Privacy Policy. You may unsubscribe from the newsletter at any time.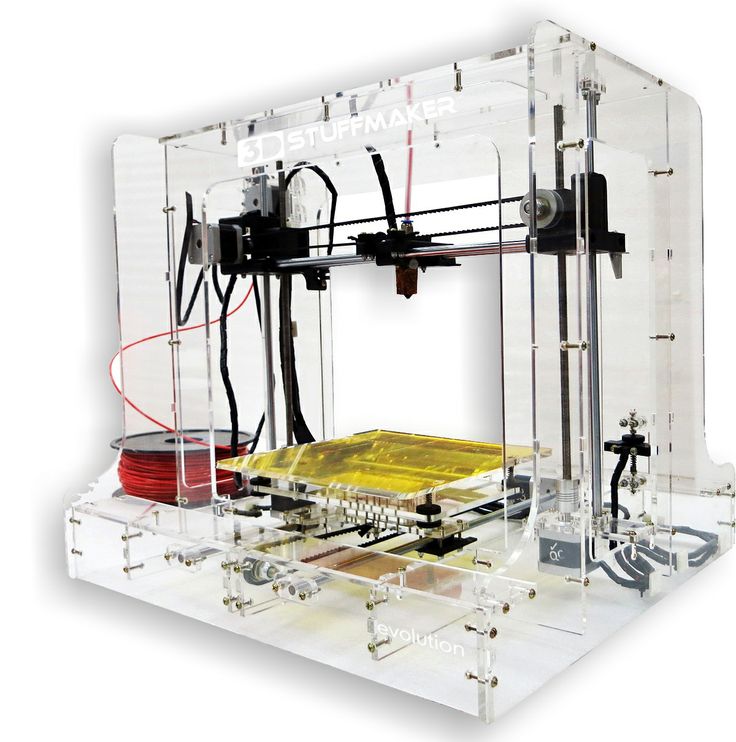
More articles
T&R Biofab gains patent for lucrative heart disease-treating technology
0Shares
Korean 3D bioprinting specialist T&R Biofab has patented a way of creating human tissues that could one day be used to develop a heart disease treatment which doesn’t put patients through open surgery.
Utilizing T&R Biofab’s process, scientists have already proven it possible to create 100-micrometer cardiac spheroids, capable of regenerating damaged tissues upon transplantation. While the technology remains at a pre-clinical stage, the firm’s patent approval in Japan could now be significant, in that the only developer of something similar in the country, has reportedly licensed it out for $600 million.
Imaging showing cardiac fibrosis taking place in spheroid samples after 8 weeks. Image via T&R Biofab.Regenerative cardiac therapy
According to CDC heart disease data, cardiac illnesses are the leading cause of death in men and women across most racial and ethnic groups in the US. As such, the development of robust cardiac therapies is a matter of life and death for many Americans. Yet, despite the urgency surrounding the issue, the T&R Biofab scientists behind its spheroid research say that current treatments are “unrealistic.”
As such, the development of robust cardiac therapies is a matter of life and death for many Americans. Yet, despite the urgency surrounding the issue, the T&R Biofab scientists behind its spheroid research say that current treatments are “unrealistic.”
Due to the “limitations and drawbacks” associated with transplantation, as well as the installation of pumps into the ventricles of patients’ hearts, the scientists have therefore identified cell-based regenerative treatments as an alternative.
Generally speaking, such methods involve using cardiomyocytes (the cells that make a heart contract) derived from human pluripotent stem cells to develop transplantable tissues, with the likes of Matricelf taking a similar path towards creating 3D bioprinted neural implants last year.
In the field of cardiac 3D bioprinting research, scientists also continue to make rapid advances, and a team at Harvard University recently found they were able to produce functional multi-layered heart tissues. However, as the T&R Biofab researchers point out in their spheroid paper, the heterogeneity of stem cells remains an issue that makes them extremely difficult to store and use long-term.
However, as the T&R Biofab researchers point out in their spheroid paper, the heterogeneity of stem cells remains an issue that makes them extremely difficult to store and use long-term.
“Major issues, including the heterogeneity of human pluripotent stem cells, may cause tumorigenicity and arrhythmia, and affect their long-term storage, causing their poor survival, retention, and engraftment in-vivo following implantation into diseased hearts,” said the T&R Biofab-led team in their paper. “These issues must be resolved before pursuing clinical application.”
The scientists’ approach to creating cell aggregates. Image via T&R Biofab.Improving cardiac tissue viability
One of the early breakthroughs in the scientists’ research was their discovery that cluster of differentiation 71 (CD71) surface proteins are key to creating tissues formed of homogenous stem cells. While generally used inside the human body for delivering iron, the researchers found that CD71 also plays an important role in the heart, and when added to tissues, it can trigger microfibrillar cell growth.
Having come up with a way of improving cell viability, the team then turned to developing a means of better preserving tissues during storage, something that could be key to their future clinical usage. To achieve this, the team came up with the idea of cardiac spheroids, essentially groups of human pluripotent stem cells, which, when packed together, are capable of surviving for longer periods.
As a means of testing the long-term viability of these structures, the scientists later created prototypes before freezing them with liquid nitrogen. When defrosted six months later, it was discovered each of the spheroids was uniform in size, and that 80% of the tissues’ cells were still viable. Over shorter 7-day trials, samples also lasted demonstrably longer than single-cells or larger aggregate clusters.
Once they’d proven the efficacy of their overall approach, the last stage of the team’s study saw them test their spheroids, by implanting them into rats entering cardiac arrest.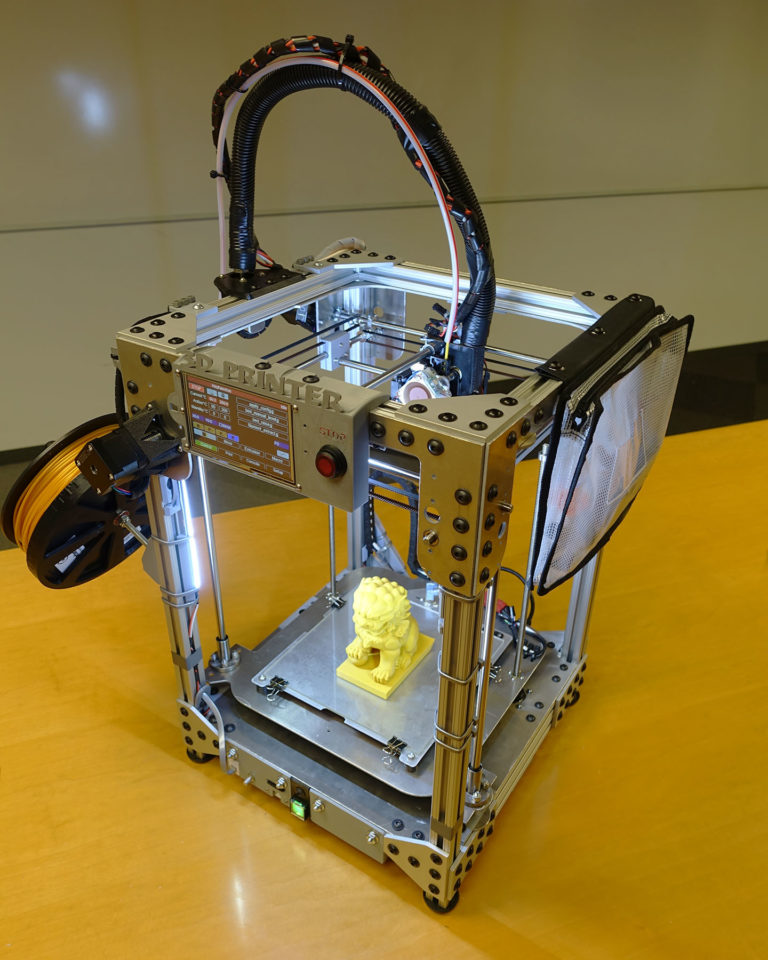 Those treated with the scientists’ tissues were found to exhibit higher levels of cardiac function than those treated with regular stem cells, and following removal, the spheroids ultimately showed excellent engraftment and stability.
Those treated with the scientists’ tissues were found to exhibit higher levels of cardiac function than those treated with regular stem cells, and following removal, the spheroids ultimately showed excellent engraftment and stability.
“The approach described in this study is simple and effective for the production of readily available human pluripotent stem cells in clinical settings,” the scientists concluded in their paper. “The microcardiac spheroids established in this study can be preserved and stored; they exhibit superior viability under hypoxic conditions and in-vivo. [However], despite several meaningful results, future studies examining more sophisticated implantation methods, such as the 27G NOGA catheter system and applicability to large animals, are considered limitations of this study.”
T&R Biofab has previously managed to implant liver tissues into animal test subjects. Photo via T&R Biofab.Although viable 3D bioprinted soft tissue transplants remain a long way from reality, the technology continues to make progress in lab settings. T&R Biofab itself found that it was able to implant 3D bioprinted liver tissues into animal test subjects last year, in a project that saw its scientists replicate the ‘lobules’ of the human liver.
T&R Biofab itself found that it was able to implant 3D bioprinted liver tissues into animal test subjects last year, in a project that saw its scientists replicate the ‘lobules’ of the human liver.
More recently, researchers at the University of California, Berkeley have also uncovered a way of ensuring the viability of 3D bioprinted structures by freezing them. The team’s novel approach to ‘3D Cryoprinting’ allows for the cross-linking of cells layer-by-layer, in a way that yields self-supporting structures with potential in regenerative medicine R&D.
The research behind T&R Biofab’s microcardiac spheroids technology is detailed in the paper titled “Effect and application of cryopreserved three-dimensional microcardiac spheroids in myocardial infarction therapy.”
The study was co-authored by Soon-Jung Park, Hyeok Kim, Sunghun Lee, Jongsoo Kim,Taek-Hee Jung, Seong Woo Choi, Bong-Woo Park, Sun-Woong Kang, David A. Elliott, Edouard G. Stanley ,Andrew G. Elefanty, Kiwon Ban, Hun-Jun Park and Sung-Hwan Moon.
Elefanty, Kiwon Ban, Hun-Jun Park and Sung-Hwan Moon.
As you’d expect from such a large team, they hailed from multiple organizations, including T&R Biofab’s Research Institute, the Catholic University of Korea, the City University of Hong Kong, Konkuk University, Seoul National University, the Korean Institute of Toxicology, and Monash University.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
For a deeper dive into additive manufacturing, you can now subscribe to our Youtube channel, featuring discussion, debriefs, and shots of 3D printing in-action.
Are you looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows cardiac fibrosis occurring in spheroid samples after 8 weeks. Image via T&R Biofab.
Image via T&R Biofab.
Tags Catholic University of Korea CDC City University of Hong Kong Harvard University Konkuk University Korean Institute of Toxicology Matricelf Monash University Seoul National University T&R Biofab University of California Berkeley
Paul Hanaphy
Paul is a history and journalism graduate with a passion for finding the latest scoop in technology news.
ProJet 4500:
Full Color Plastic 3D Printer TheProJet 4500 is currently the world's only full color 3D printer capable of printing with plastic. It is able to create parts with excellent surface quality, ready to use flexible and durable colored products. The ProJet 4500 is highly productive and has an intuitive control console.
ProJet 4500 Benefits
- Capable of producing durable full color plastic models straight from the build chamber without any post-processing.
- A unique feature of the 3D printer is the ability to print in different colors up to a million shades, and each pixel of the model can have its own color, which gives designers and designers a wide scope for creativity.
- High print speed.
- Media Savings: ProJet 4500 does not use support materials, model material can be reused for printing.
- Combination of ergonomics and reliability: The ProJet 4500 fits perfectly in a typical office, it does not require special conditions and is easy to operate.
- Eco-Friendly: This 3D printer does not require a water connection or the use of any chemicals.
Applications
The capabilities of the ProJet 4500 are used in a wide variety of applications. It is actively used by professionals in various industries, wherever it is necessary to obtain high-quality color products in a short time.
ProJet 4500 Applications:
- design;
- architecture and construction;
- fashion industry;
- production of souvenirs;
- advertising production and marketing communications;
- development of consumer goods;
- health care.
The manufacturer can always be sure of the quality of the printed models. The ProJet 4500 creates durable, full color plastic products.
The ProJet 4500 creates durable, full color plastic products.
Printing technology
The ProJet 4500 creates models using CJP technology, which uses two components in its work: the base material of construction and the binder. The build material is spread across the chamber in a thin layer, then the inkjet printheads apply a coloring binder in accordance with a predetermined geometry, which causes the material to harden. The working platform is lowered with each layer applied until the model is completely built.
Using the VisiJet C4 Spectrum material, the ProJet 4500 3D printer allows you to quickly create prototypes that match the original model, transfer its critical characteristics, as well as receive custom-made finished products with high resolution.
Materials
The ProJet 4500 is the first 3D printer in its class to produce full color plastic products using color inkjet technology. The 3D printer uses VisiJet C4 Spectrum acrylate-based heat-curable materials and has a pixel-by-pixel coloring feature that allows you to produce strong, flexible plastic products and paint them in almost one million unique user-selectable colors. If necessary, a simple additional processing can enhance the brightness of the colors.
The 3D printer uses VisiJet C4 Spectrum acrylate-based heat-curable materials and has a pixel-by-pixel coloring feature that allows you to produce strong, flexible plastic products and paint them in almost one million unique user-selectable colors. If necessary, a simple additional processing can enhance the brightness of the colors.
VisiJet C4 Spectrum is a plastic material with excellent flexibility and strength for long-term testing of concepts, prototypes, and final products. The material is ideal for manufacturers in a wide range of applications requiring wear resistant parts. From homewares and toys to healthcare, science and design accessories.
ProJet 4500 or ProJet 660Pro: Which Should You Choose?
In the 3D hardware market, you can often find machines with similar features. For example, the specifications of the ProJet 4500 3D printer are very similar to the ProJet 660Pro. Which of these 3D printers is best for your needs?
The main difference between these two printers is the materials they use: the 660Pro is a gypsum-based powder, while the 4500 is a resin compound (plastic).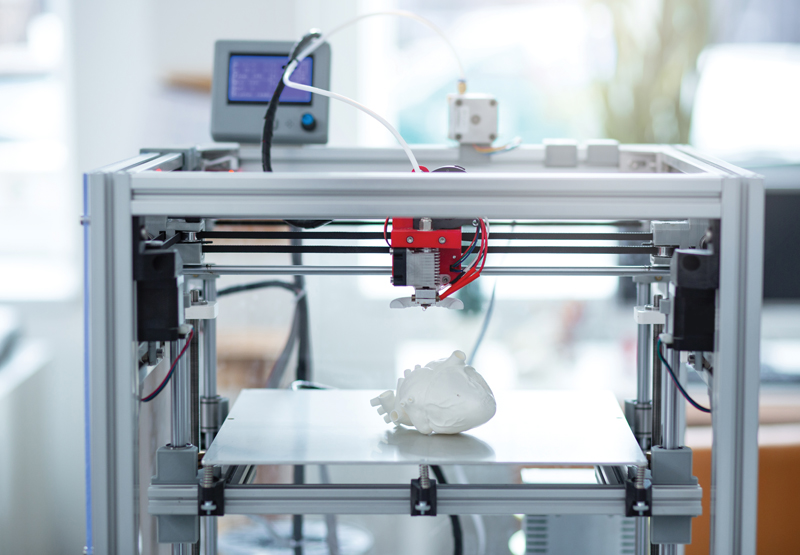 Due to the strength of the modeling plastic, the ProJet 4500 is able to print products that are more durable than those made on the plaster 660Pro. However, the detailing of plaster prototypes is better, and the heat resistance is higher, which allows you to create molds with the ProJet 660Pro.
Due to the strength of the modeling plastic, the ProJet 4500 is able to print products that are more durable than those made on the plaster 660Pro. However, the detailing of plaster prototypes is better, and the heat resistance is higher, which allows you to create molds with the ProJet 660Pro.
Increased product strength gives the ProJet 4500 a wider range of applications than models built on the 660Pro. Given the quality of the surfaces, the ProJet 4500 3D printer is more versatile and finds application in many areas of manufacturing and design.
Some businesses are successfully using both models of these 3D printers. According to Steve Corey (Objex Unlimited), the ProJet 4500 is the perfect complement to the 660:
“With the ProJet 4500, we can complete any model that would be too complex for the Projet 660Pro. It allows you to create products that are more durable, with thin walls and geometry that is not always available to gypsum.”
Corey also notes that the 4500 is more reliable and does an excellent job of printing thin-walled complex structures for mechanical and architectural needs.
Digging into the internals of the ProJet 4500 3D printer, Steve also commented on the manufacturability of the printhead: “The printer runs with little to no downtime, and the head wears out for a long time, avoiding costly costs.”
Bioprinter - ciclomenstrual.info
Bioprinter (bioprinter, rarely: organic printer) is a special form of 3D printer, which is controlled by a computer using tissue engineering techniques, to produce regular structures (so-called bioarrays) or tissue from pre-grown single cells. Later, the technology will make it possible to produce whole organs. Bioprinters can be used in medicine (individual organs), in synthetic biology (artificial life forms), and in the food industry (artificial meat). According to the manufacturer, bioprinters are at a very advanced stage of development. Companies that use the Bioprinter (as of 2013) are Organovo and Modern Meadow. Both have the same founders. Organovo has plans to introduce bioprinters in medicine. Initially, artificial blood vessels for vascular surgery must be created. Modern Meadow, on the other hand, would like to use them in the food industry. According to their own statements, they want to produce synthetic meat instead of factory farming. This process is commonly referred to as "bioprinting".
Contents
- 1 How it works
- 2 Medical use
- 3 synthetic biology
- 4 food industry
- 5 Modern bioprinters
- 6 web links
- 7 individual proofs
functionality
The bioprinter works similarly to a 3D printer based on the FDM process. The extruder builds a mold from a material, in this case not a thermoplastic material such as ABS, but a polymer gel, such as alginate-based B., with living cells embedded in it. The Organovos Bioprinter uses another promising technology to apply droplets, each containing between 10,000 and 30,000 individual cells. Later, they must, stimulated by appropriate growth factors, organize themselves into functional tissue structures.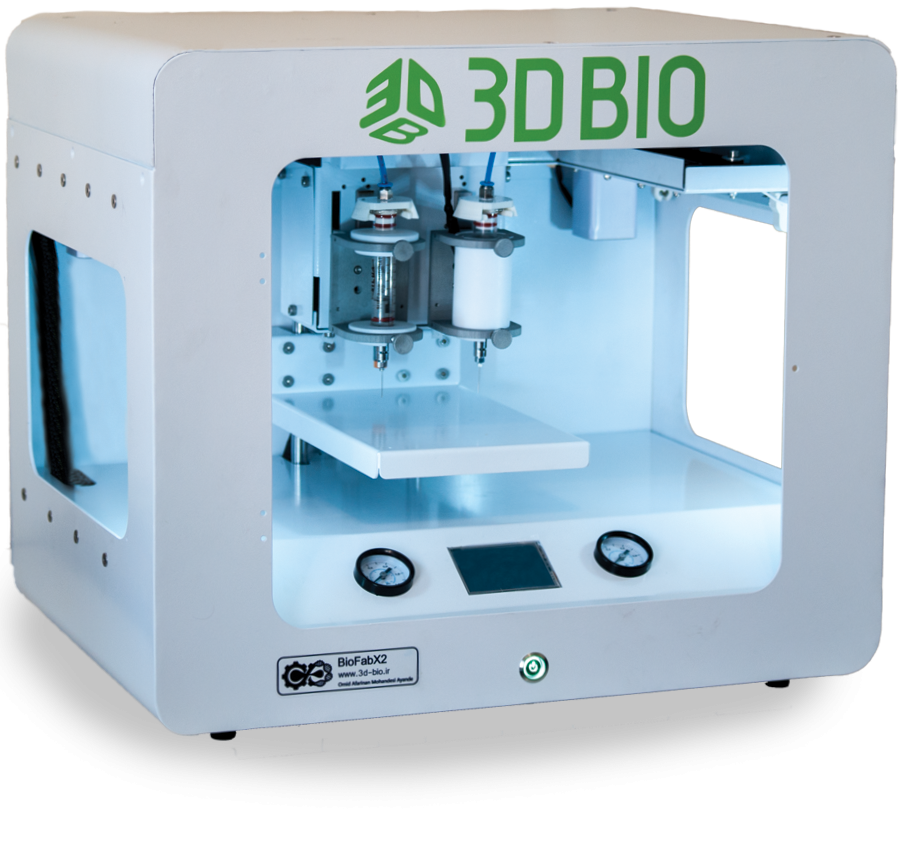
Bioprinters have special components such as temperature control that are very important for proper printing.
Today, this technology allows printing of simply structured tissues such as muscles, cartilage, skin, parts of the liver and parts of the kidneys. They are mainly for drug testing.
Medical use
Bioprinters (in experimental area) have been used for medical purposes since 2000. To date, it is impossible to experimentally print organs consisting of several types of tissues. Some research is more focused on creating relatively large aggregations of cells through a printing process, which are then supposed to "mature" into organs through biological self-organization. For example, a serious problem is the creation of a functioning system of blood vessels.
However, it seems likely that bioprinters, or organs created with them, could eventually replace donor organs. One of the advantages of bioprinter organs is that they are precisely adapted to the intended body.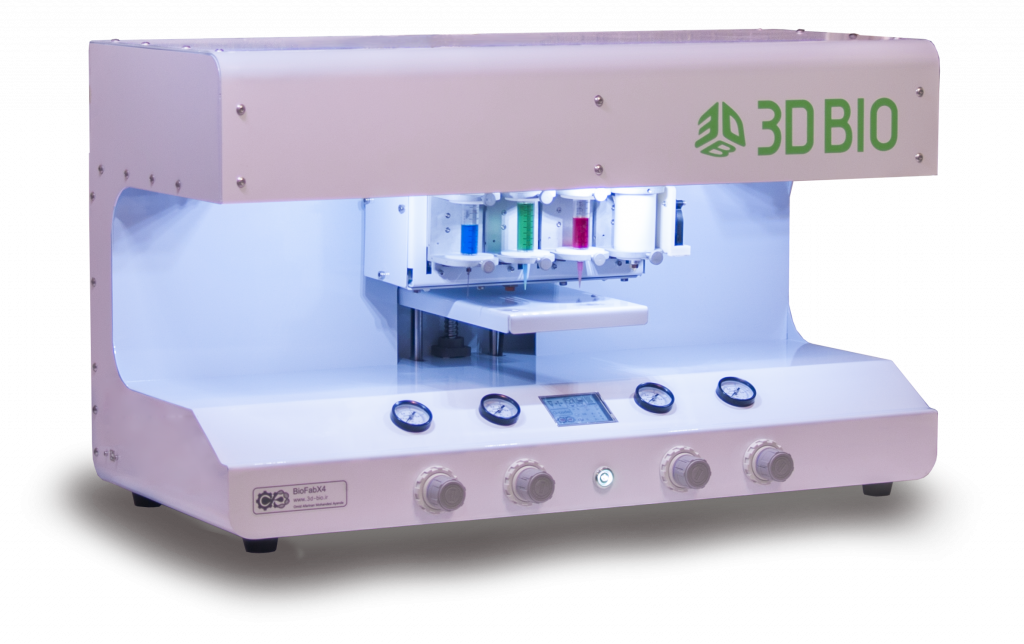 In the case of donor organs, one has to wait until an organ is available that fits as best as possible. However, it is usually unlikely that a donor organ will be available at all. The “printing time” of an artificial organ, which lasts several hours, can become a barrier in case of acute accidental injuries. Grafts printed on a conventional 3D printer and made of metal or plastic do not count towards bioprinting because no cells are used. Smaller bone parts or calcium phosphate dentures are already being produced through the 3D printing process. However, for the manufacture of bones, material from specially bred cattle is usually used.
In the case of donor organs, one has to wait until an organ is available that fits as best as possible. However, it is usually unlikely that a donor organ will be available at all. The “printing time” of an artificial organ, which lasts several hours, can become a barrier in case of acute accidental injuries. Grafts printed on a conventional 3D printer and made of metal or plastic do not count towards bioprinting because no cells are used. Smaller bone parts or calcium phosphate dentures are already being produced through the 3D printing process. However, for the manufacture of bones, material from specially bred cattle is usually used.
Synthetic biology
In synthetic biology, bioprinters can be used to print new life forms. The result of synthetic biology, which caused a sensation among the public, was the "jellyfish", an artificial "jellyfish" made from rat muscle cells and silicone capable of swimming. However, this was not only created by the bioprinter.
food industry
Also, food such as meat can be used in bulk to produce the Bioprinter. Modern Meadow says it has already printed delicious meat that was produced with less effort than breeding and slaughtering. The company wants to end the carnage. Currently, there is no "printed" meat for sale, although this is already possible in terms of taste and health. Professor Stampfl from the Institute of Materials Science and Technology at the Vienna University of Technology estimated the cost of a printed piece of meat in 2013 to be at least 50,000 euros.
Modern Meadow says it has already printed delicious meat that was produced with less effort than breeding and slaughtering. The company wants to end the carnage. Currently, there is no "printed" meat for sale, although this is already possible in terms of taste and health. Professor Stampfl from the Institute of Materials Science and Technology at the Vienna University of Technology estimated the cost of a printed piece of meat in 2013 to be at least 50,000 euros.
A satire of such a food industry was presented in the 1976 film Chest or Legs, in which Louis de Funes played a leading role and secretly invaded a factory in which, for example, chickens were artificially created.
Current bioprinter
Currently the only commercial bioprinter is offered by Organovo, which also invests in research: NovoGen MMX. The price is available only on request. In addition, bioprinter development methods based on commercially available inkjet printers are being tested. Theoretically, any "normal" 3D printer can become a bioprinter by replacing plastic with cells. The BioFab 4000 (later also the BioFab 4500) is often shown in animation but does not actually exist, only the function needs to be illustrated. The same goes for the bioprinter, on which the Hewlett-Packard logo can be seen. Probably, it was shown there, since many printers are associated with the market leader Hewlett-Packard. In fact, Hewlett-Packard does not offer any bioprinters and currently has no plans to (as of 2013).
The BioFab 4000 (later also the BioFab 4500) is often shown in animation but does not actually exist, only the function needs to be illustrated. The same goes for the bioprinter, on which the Hewlett-Packard logo can be seen. Probably, it was shown there, since many printers are associated with the market leader Hewlett-Packard. In fact, Hewlett-Packard does not offer any bioprinters and currently has no plans to (as of 2013).
web links
- Official website of Organovo
- Modern Meadow official website
- Several reports of bioprinting on the Golem, including a flint jellyfish and a modern grassland
Individual evidence
- ↑ a b "Bioprinting technology promises to create complex skin models." Retrieved 6 March 2019.
- ↑ Vladimir Mironov, Richard P. Visconti, Vladimir Kasyanov, Gabor Forgax, Christopher J. Drake, Roger R. Marwald (2009Richard P. Visconti, Vladimir Kasyanov, Carmine Gentile1, Jing Zhang, Roger R.

Learn more