3D printing body parts youtube
Creating body parts with 3D printing
Skip to content
menu
curiousFollow
- Home
- browse videos
- Creating body parts with 3D printing
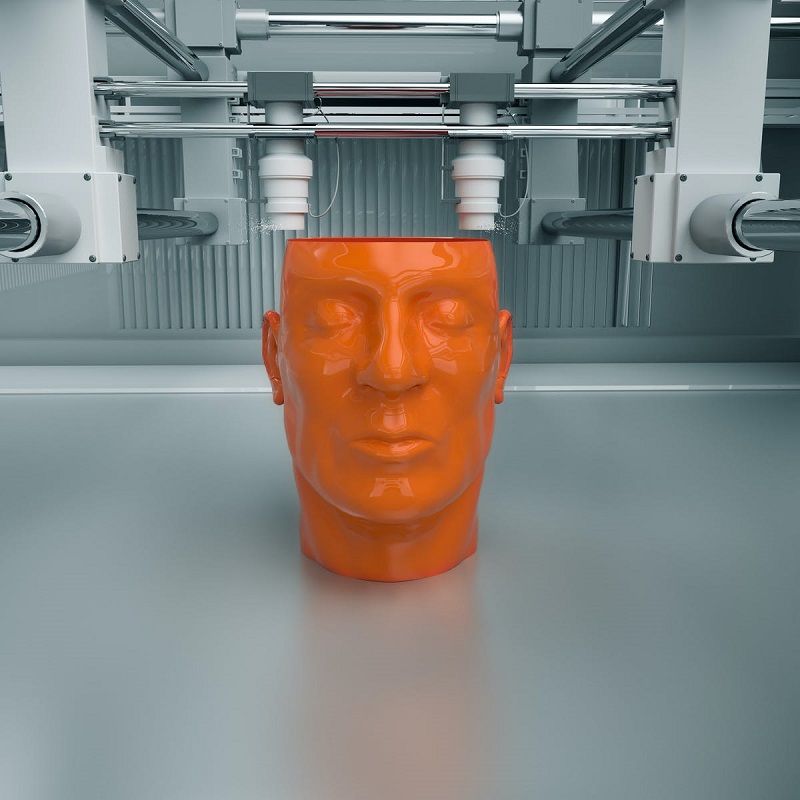
Lawrence Bonassar, Ph.D., Associate Professor of Biomedical Engineering, describes a cutting-edge process he has developed in which he uses a 3D Printer and "ink" composed of living cells to create body parts such as ears.
Video source: Cornell University / YouTube.
View Transcriptarrow
DR LAWRENCE BONASSAR, Ph.D., Associate Professor Biomedical Engineering, Cornell University: I'm Dr Bonassar, and my lab makes ears.
The invention that we've discovered is a way to print living cells in a material that can be used to reconstruct tissues in the body. My laboratory's interested in regenerating cartilage wherever it's found in the body.
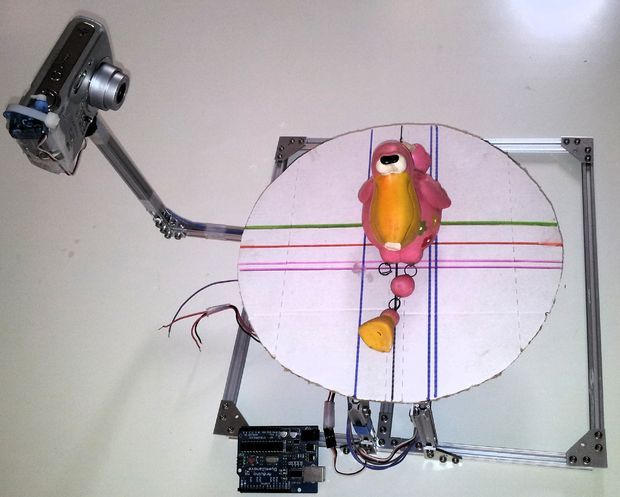
The process starts with a scan of an ear. We sit someone down in a chair, and we have a camera that spins around their head, and takes a 3D image of their head. Then you can very precisely map out the topology of the ear.
The next kind of key step is developing the ink for this printer. This ink is actually a living ink. It contains living cells. It's alive when we put it into the printer, it's alive when it comes out of the printer.
The real power of the printing technique is that it can be used to make geometries that you just can't make with any other technique. You can make parts with holes in them, we can layer and cover and put different cells next to each other to create, really, the complex organs that make up our bodies. And after 2 months in an incubator, the tissue fills in and looks white, just like real cartilage.
The implants that we're making are not rubber or plastic. They are alive. They grow inside the body or out. And this has a whole host of advantages over conventional technology. The body accepts these materials like it's part of the body, because it is.
They are alive. They grow inside the body or out. And this has a whole host of advantages over conventional technology. The body accepts these materials like it's part of the body, because it is.
Our long-term goals are to change the way that clinicians practice, to give them next-generation of implants that will be more successful, more like real tissue that will last in the body for decades.
1:51 People & medicine
All videos arrow
Global efforts to beat hepatitis B
Video: Global efforts to beat hepatitis B
Personal mission to improve stroke outcomes
Video: Personal mission to improve stroke outcomes
Tackling asbestos beyond borders
Video: Tackling asbestos beyond borders
Back to top
3D printing of body parts is coming fast – but regulations are not ready
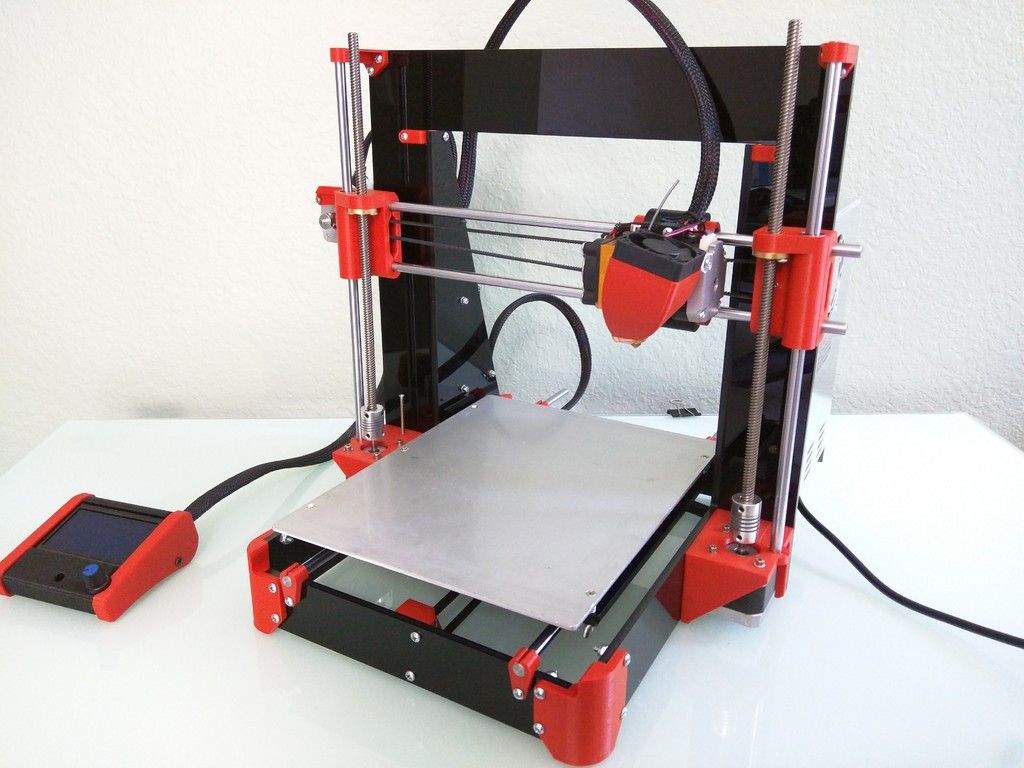
In the last few years, the use of 3D printing has exploded in medicine. Engineers and medical professionals now routinely 3D print prosthetic hands and surgical tools. But 3D printing has only just begun to transform the field.
Engineers and medical professionals now routinely 3D print prosthetic hands and surgical tools. But 3D printing has only just begun to transform the field.
Today, a quickly emerging set of technologies known as bioprinting is poised to push the boundaries further. Bioprinting uses 3D printers and techniques to fabricate the three-dimensional structures of biological materials, from cells to biochemicals, through precise layer-by-layer positioning. The ultimate goal is to replicate functioning tissue and material, such as organs, which can then be transplanted into human beings.
We have been mapping the adoption of 3D printing technologies in the field of health care, and particularly bioprinting, in a collaboration between the law schools of Bournemouth University in the United Kingdom and Saint Louis University in the United States. While the future looks promising from a technical and scientific perspective, it’s far from clear how bioprinting and its products will be regulated. Such uncertainty can be problematic for manufacturers and patients alike, and could prevent bioprinting from living up to its promise.
Such uncertainty can be problematic for manufacturers and patients alike, and could prevent bioprinting from living up to its promise.
From 3D printing to bioprinting
Bioprinting has its origins in 3D printing. Generally, 3D printing refers to all technologies that use a process of joining materials, usually layer upon layer, to make objects from data described in a digital 3D model. Though the technology initially had limited applications, it is now a widely recognized manufacturing system that is used across a broad range of industrial sectors. Companies are now 3D printing car parts, education tools like frog dissection kits and even 3D-printed houses. Both the United States Air Force and British Airways are developing ways of 3D printing airplane parts.
The NIH in the U.S. has a program to develop bioprinted tissue that’s similar to human tissue to speed up drug screening. Paige Derr and Kristy Derr, National Center for Advancing Translational SciencesIn medicine, doctors and researchers use 3D printing for several purposes. It can be used to generate accurate replicas of a patient’s body part. In reconstructive and plastic surgeries, implants can be specifically customized for patients using “biomodels” made possible by special software tools. Human heart valves, for instance, are now being 3D printed through several different processes although none have been transplanted into people yet. And there have been significant advances in 3D print methods in areas like dentistry over the past few years.
It can be used to generate accurate replicas of a patient’s body part. In reconstructive and plastic surgeries, implants can be specifically customized for patients using “biomodels” made possible by special software tools. Human heart valves, for instance, are now being 3D printed through several different processes although none have been transplanted into people yet. And there have been significant advances in 3D print methods in areas like dentistry over the past few years.
Bioprinting’s rapid emergence is built on recent advances in 3D printing techniques to engineer different types of products involving biological components, including human tissue and, more recently, vaccines.
While bioprinting is not entirely a new field because it is derived from general 3D printing principles, it is a novel concept for legal and regulatory purposes. And that is where the field could get tripped up if regulators cannot decide how to approach it.
State of the art in bioprinting
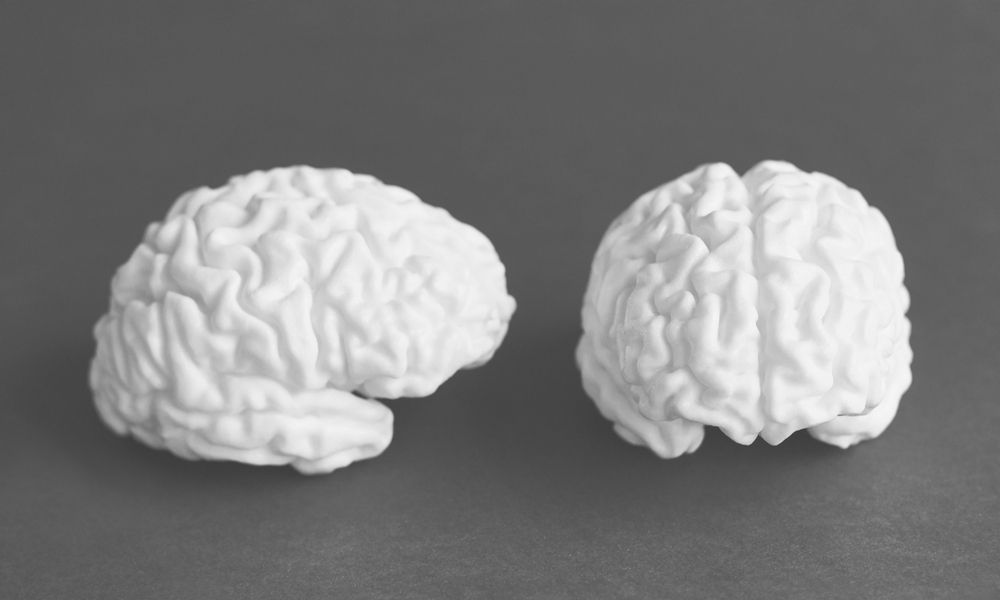
Scientists are still far from accomplishing 3D-printed organs because it’s incredibly difficult to connect printed structures to the vascular systems that carry life-sustaining blood and lymph throughout our bodies. But they have been successful in printing nonvascularized tissue like certain types of cartilage. They have also been able to produce ceramic and metal scaffolds that support bone tissue by using different types of bioprintable materials, such as gels and certain nanomaterials. A number of promising animal studies, some involving cardiac tissue, blood vessels and skin, suggest that the field is getting closer to its ultimate goal of transplantable organs.
But they have been successful in printing nonvascularized tissue like certain types of cartilage. They have also been able to produce ceramic and metal scaffolds that support bone tissue by using different types of bioprintable materials, such as gels and certain nanomaterials. A number of promising animal studies, some involving cardiac tissue, blood vessels and skin, suggest that the field is getting closer to its ultimate goal of transplantable organs.
We expect that advancements in bioprinting will increase at a steady pace, even with current technological limitations, potentially improving the lives of many patients. In 2019 alone, several research teams reported a number of breakthroughs. Bioengineers at Rice and Washington Universities, for example, used hydrogels to successfully print the first series of complex vascular networks. Scientists at Tel Aviv University managed to produce the first 3D-printed heart. It included “cells, blood vessels, ventricles and chambers” and used cells and biological materials from a human patient. In the United Kingdom, a team from Swansea University developed a bioprinting process to create an artificial bone matrix, using durable, regenerative biomaterial.
It included “cells, blood vessels, ventricles and chambers” and used cells and biological materials from a human patient. In the United Kingdom, a team from Swansea University developed a bioprinting process to create an artificial bone matrix, using durable, regenerative biomaterial.
‘Cloneprinting’
Though the future looks promising from a technical and scientific perspective, current regulations around bioprinting pose some hurdles. From a conceptual point of view, it is hard to determine what bioprinting effectively is.
Consider the case of a 3D-printed heart: Is it best described as an organ or a product? Or should regulators look at it more like a medical device?
Regulators have a number of questions to answer. To begin with, they need to decide whether bioprinting should be regulated under new or existing frameworks, and if the latter, which ones. For instance, should they apply regulations for biologics, a class of complex pharmaceuticals that includes treatments for cancer and rheumatoid arthritis, because biologic materials are involved, as is the case with 3D-printed vaccines? Or should there be a regulatory framework for medical devices better suited to the task of customizing 3D-printed products like splints for newborns suffering from life-threatening medical conditions?
In Europe and the U. S., scholars and commentators have questioned whether bioprinted materials should enjoy patent protection because of the moral issues they raise. An analogy can be drawn from the famed Dolly the sheep over 20 years ago. In this case, it was held by the U.S. Court of Appeals for the Federal Circuit that cloned sheep cannot be patented because they were identical copies of naturally occurring sheep. This is a clear example of the parallels that exist between cloning and bioprinting. Some people speculate in the future there will be ‘cloneprinting,’ which has the potential for reviving extinct species or solving the organ transplant shortage.
S., scholars and commentators have questioned whether bioprinted materials should enjoy patent protection because of the moral issues they raise. An analogy can be drawn from the famed Dolly the sheep over 20 years ago. In this case, it was held by the U.S. Court of Appeals for the Federal Circuit that cloned sheep cannot be patented because they were identical copies of naturally occurring sheep. This is a clear example of the parallels that exist between cloning and bioprinting. Some people speculate in the future there will be ‘cloneprinting,’ which has the potential for reviving extinct species or solving the organ transplant shortage.
Dolly the sheep’s example illustrates the court’s reluctance to traverse this path. Therefore, if, at some point in the future, bioprinters or indeed cloneprinters can be used to replicate not simply organs but also human beings using cloning technologies, a patent application of this nature could potentially fail, based on the current law. A study funded by the European Commission, led by Bournemouth University and due for completion in early 2020 aims to provide legal guidance on the various intellectual property and regulatory issues surrounding such issues, among others.
On the other hand, if European regulators classify the product of bioprinting as a medical device, there will be at least some degree of legal clarity, as a regulatory regime for medical devices has long been in place. In the United States, the FDA has issued guidance on 3D-printed medical devices, but not on the specifics of bioprinting. More important, such guidance is not binding and only represents the thinking of a particular agency at a point in time.
Cloudy regulatory outlook
Those are not the only uncertainties that are racking the field. Consider the recent progress surrounding 3D-printed organs, particularly the example of a 3D-printed heart. If a functioning 3D-printed heart becomes available, which body of law should apply beyond the realm of FDA regulations? In the United States, should the National Organ Transplant Act, which was written with human organs in mind, apply? Or do we need to amend the law, or even create a separate set of rules for 3D-printed organs?
We have no doubt that 3D printing in general, and bioprinting specifically, will advance rapidly in the coming years.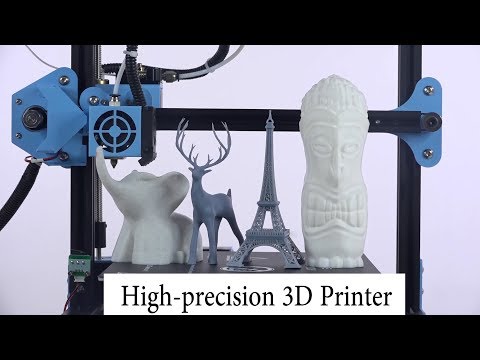 Policymakers should be paying closer attention to the field to ensure that its progress does not outstrip their capacity to safely and effectively regulate it. If they succeed, it could usher in a new era in medicine that could improve the lives of countless patients.
Policymakers should be paying closer attention to the field to ensure that its progress does not outstrip their capacity to safely and effectively regulate it. If they succeed, it could usher in a new era in medicine that could improve the lives of countless patients.
[ You’re smart and curious about the world. So are The Conversation’s authors and editors. You can get our highlights each weekend. ]
all about printing organs on a 3D printer
Printing organs on a 3D printer or bioprinting is a promising technology for growing healthy and living organs to replace damaged or missing ones. In addition to a 3D printer, bioprinting requires a model of an organ, patient cell material, and an environment where the organ will remain until implantation.
Printed organs are better than prostheses and transplanted body parts. Their capabilities are identical to native ones and they are not rejected by the immune system if they are created from the patient's DNA. Bioprinting will reduce the time to obtain the desired organ and save the lives of patients who need an immediate transplant.
Bioprinting will reduce the time to obtain the desired organ and save the lives of patients who need an immediate transplant.
Printing organs on a 3D printer has already been successfully tested on animals. Scientists at Northwestern University implanted artificial ovaries in sterilized mice and they gave birth to healthy mice. In the Chinese company Sichuan Revotek, rhesus monkeys have been implanted with blood vessels grown from the material of the same monkeys.
From human body parts, only internal tissues and skin are printed so far. Reduced but working copies of ears and noses are created. The first printing of human organs is expected by 2030.
How bioprinting works
Research groups or companies are developing different bioprinting concepts:
- Wireframe. The growth of living cells on an inorganic base, which disappears with the development of natural connections between cells. The main difficulty is to find a material that is as elastic or rigid as the organ being replaced.
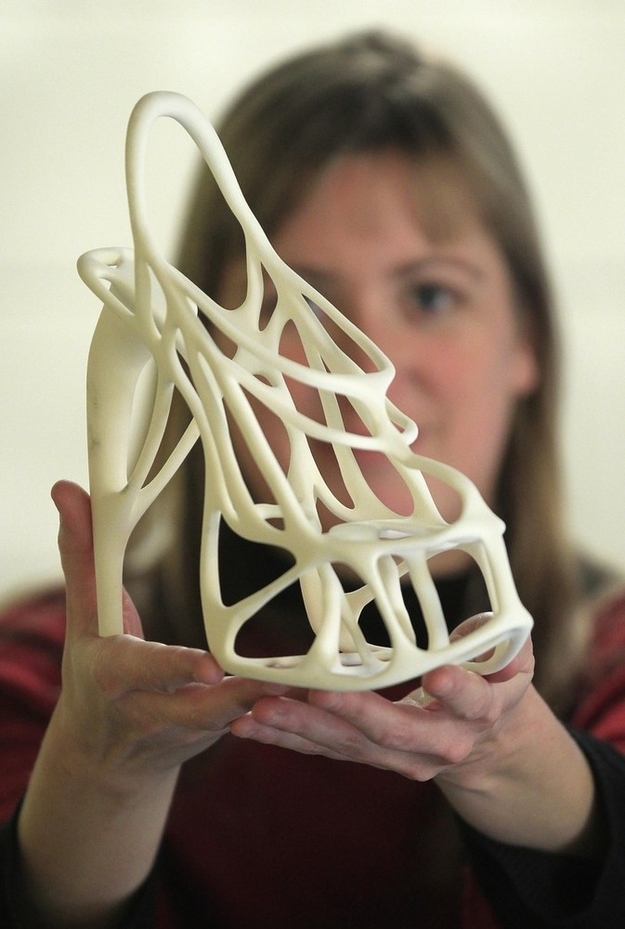 It must degrade quickly so as not to interfere with the strengthening of the extracellular matrix and dissolve without leaving toxic compounds. Hydrogel, titanium, gelatin, synthetic and biopolymers are suitable for wireframe printing.
It must degrade quickly so as not to interfere with the strengthening of the extracellular matrix and dissolve without leaving toxic compounds. Hydrogel, titanium, gelatin, synthetic and biopolymers are suitable for wireframe printing.
- Frameless. Application of prepared cells on a hydrogel base. While the cells are in the printer, they are cooled and are in thin hydrogel spheroids. When printing, the temperature rises to 36.6°C, the spheroids scatter, and the cells gradually form their own natural framework - the cellular matrix. This printing is less common than wireframe printing - it appeared later and is more difficult to reproduce.
- Mimicry. The technology of the future, involves the creation of complete copies of organs at once. For it, bioprinting is being developed at the molecular level and in-depth studies of the nature of cells are being carried out.
Methods for 3D printing of organs
Inkjet.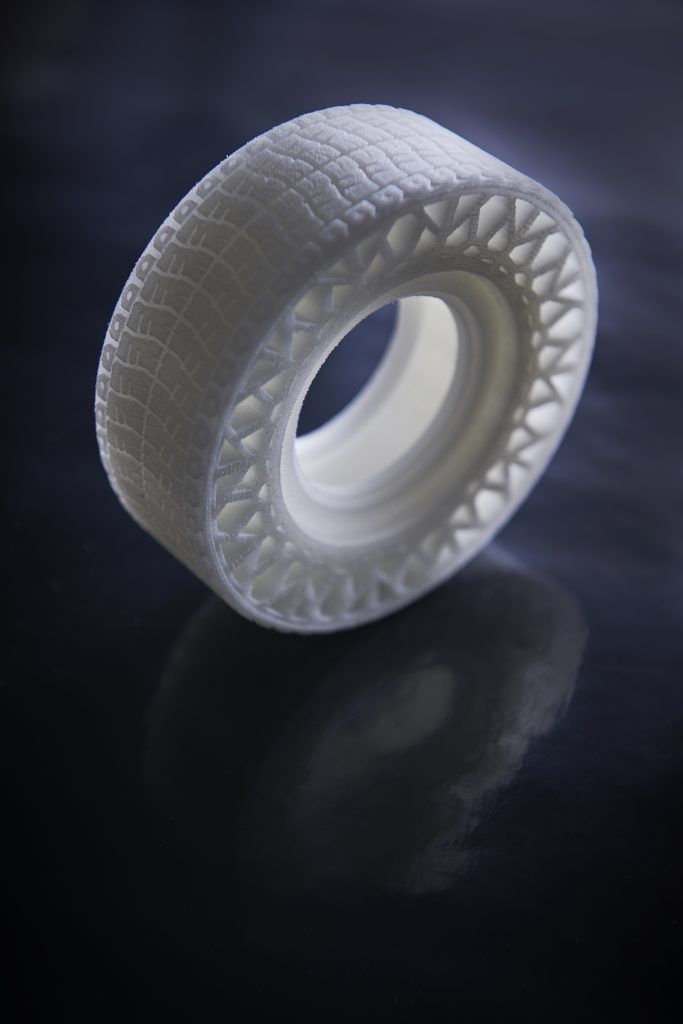 The first devices for bioprinting were inkjet, conventional printers also use this method. They store biological material in cartridges that are sprayed onto a hydrogel substrate like paint on paper. Disadvantages - inaccurate droplet ejection and blockage of the spray nozzle with possible death of cellular material. Inkjet printing of organs on a printer is not suitable for viscous materials because they are not atomized. The scope is limited to the restoration of bone, cartilage, muscles and skin. Advantages - low cost and mass reproducibility.
The first devices for bioprinting were inkjet, conventional printers also use this method. They store biological material in cartridges that are sprayed onto a hydrogel substrate like paint on paper. Disadvantages - inaccurate droplet ejection and blockage of the spray nozzle with possible death of cellular material. Inkjet printing of organs on a printer is not suitable for viscous materials because they are not atomized. The scope is limited to the restoration of bone, cartilage, muscles and skin. Advantages - low cost and mass reproducibility.
Microextrusion. This method is used in inorganic 3D printing. For printing, a pneumatic supply of material is used in a movable extruder head, which stacks the cells. The more heads, the more accurate and faster the printer. Disadvantages - the denser the cells fit, the less they survive. With a comparable stacking density, more cells die from microextrusion printing than from inkjet printing. Advantages - suitable for 3D printing of high-density organs, fine-tuning of the material supply due to pressure regulation.
Laser. Common in industry but used in bioprinting. A laser is used to heat glass with a liquid cell substrate. At the beam concentration point, excess pressure is created, which pushes the cells to the desired area of the substrate. A reflective element is placed between the beam and the glass with biomaterial, which reduces the power of the beam. Disadvantages - increased metal content in the cells from the evaporation of the reflective element. Price. Advantages - controlled up to individual cells, laying of biomaterial.
Who offers 3D printing of organs
Bioprinting companies that offer 3D printing of organs or sell bioprinters:
- Organovo - San Diego, USA. Prints and sells liver tissue " exVive3D" to pharmaceutical companies. In 2009, Organovo, together with the Austrian Invetech, launched the first mass-produced bioprinter, Novogen.
- BioBots is a startup that presented a cheap commercial bioprinter at TechCrunch 2013.
 Today, the Biobot 1 model is available for purchase, Biobot 2 is still in development, but already presented on the company's website.
Today, the Biobot 1 model is available for purchase, Biobot 2 is still in development, but already presented on the company's website. - 3D Bioprinting Solutions - Russia , Moscow. Focused on frameless printing, has developed its FABION 3D printer and is working on its own organoprinting technology
- Cyfuse Biomedical - Tokyo, Japan. They developed the Regenovo bioprinter, which was used to print skin and successfully grew 2-mm vessels.
How much does a 3D bioprinter cost
The average cost of a bioprinter is a quarter of a million dollars, but budget models are available for up to $10,000. Most printers available for purchase are extrusion type and work with frame printing.
- 3D Bioplotter - $200,000 Envision TEC, Germany.
- Novogen MMX - $250.00. Organovo, USA.
- Biobot 1 - $10,000. Biobots, USA.
- 3DDiscovery - $200,000. RegenHU & Biofactory, Switzerland.

- BioAssemblyBot - $160,000 Advanced Solutions, The Netherlands.
Supporting a patient with life support devices costs about $75,000 per year. In 10 years, the patient will spend $1 million. The printer costs $200,000 and the operation costs about the same. Considering how much it costs to print organs, the operation using 3D bioprinting is reduced by 50%.
The Future of Bioprinting
3D bioprinting has gone from concept to working and commercially successful technology. So far, the main clients of bioprinting companies are large pharmaceutical corporations. They speed up drug testing by testing them directly on printed human tissues.
Expensive bioprinters won't be in city clinics in 5 years, but some patients are already recovering thanks to 3D printing. The jaw of an 83-year-old woman from Belgium was struck by osteomyelitis. The restoration was more expensive and would have taken longer than the removal of the diseased jaw and the implantation of a printed new one.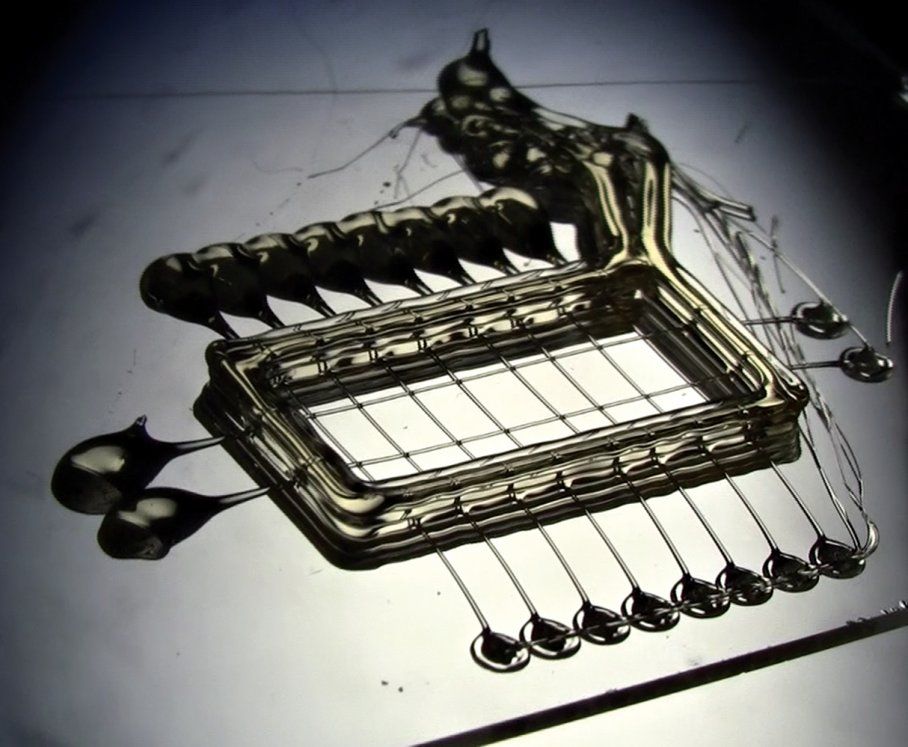 A team of doctors led by Professor Jules Poukan performed the operation and the woman was able to speak immediately after the operation. The development of bioprinting will lead to medical practices where it is easier to remove an injured limb and grow a new one than to treat injuries that are now treated without amputation.
A team of doctors led by Professor Jules Poukan performed the operation and the woman was able to speak immediately after the operation. The development of bioprinting will lead to medical practices where it is easier to remove an injured limb and grow a new one than to treat injuries that are now treated without amputation.
Medicine of the distant future minimizes mechanical intervention in the body. The scalpel will remain in the past - a swarm of nanorobots will print organs immediately inside the body. In 2018, a full-fledged printing of a human organ on a printer is planned - the kidneys. Then the bronchi, arteries and heart will be printed. But even clinical trials on humans are about 10 years away, and mass 3D printing of human organs and body parts will come even later.
In addition to doctors, bioprinting is attractive to cosmetologists and plastic surgeons. The desire to remain young and beautiful, and not the treatment of rare and complex diseases, will make 3D printing of human organs mass. Perhaps the people of the future will change organs and appearance as easily as smartphones.
Perhaps the people of the future will change organs and appearance as easily as smartphones.
3D technology in medicine | 3d modeling in medicine: using a 3d printer to print implants
The article will discuss how 3D printing has gone beyond education and science. Even today, 3D technologies are able to help doctors save human lives: we talk about all the areas of application of 3D printing in medicine in our review.
Prospects for the development of 3D printing in medicine
Medicine was one of the first industries that decided to use the potential of 3D printers for practical purposes. Moving from simple to complex, leading physicians have been looking for ways to introduce additive printing into medical practice.
The creators of 3D printers also did not stand still, developing materials ideal for printing dental implants, prostheses, prototypes of human organs, and even found a way to print with biological material.
Fun fact: The first implant was printed in 2012 by the LayerWise Corporation. At the same time, doctors performed the world's first operation to implant a titanium lower jaw, which was printed on a 3D printer.
Nowadays, 3D printing is used in almost all branches of medicine: dentistry, prosthetics, eye surgery and microsurgery, gynecology and many others.
Medical 3D modeling
Medical 3D modeling allows you to create 3D models. The technology has found application in aesthetic dentistry, oncology, otolaryngology and other fields.
Additively printed 3D models coupled with computed tomography have become one of the indispensable advances in the medical field. Three-dimensional images of diseased organs are transformed into a high-quality image, and then converted into 3D models.
Modeling makes it possible to prepare for the operation with the highest quality and to study the features of the disease.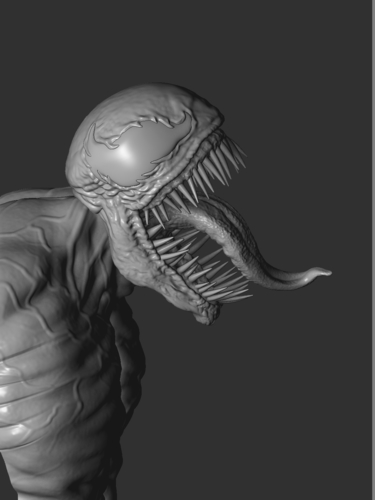 For example, when preparing for an operation to remove a tumor, doctors carefully study the size, shape, and outline of the neoplasm in three dimensions in order to understand what tactics to choose during the operation.
For example, when preparing for an operation to remove a tumor, doctors carefully study the size, shape, and outline of the neoplasm in three dimensions in order to understand what tactics to choose during the operation.
Preparation for operations using 3D modeling is carried out according to the following algorithm:
- scanning of the desired organ/tumor;
- creation of a three-dimensional image by the program;
- prototype printing;
- model study;
- choice of treatment or operation.
Thus, modern 3D printers help doctors to properly prepare for the operation. Of course, the technology is also used in other areas of medicine, but we decided to focus on oncology in order to demonstrate how invaluable help 3D printers can provide in saving lives.
Technologies for growing organs and tissues
Modern technologies have made it possible to carry out three-dimensional printing of cells, biocompatible materials and their auxiliary components in order to further create fully functional living tissues based on them.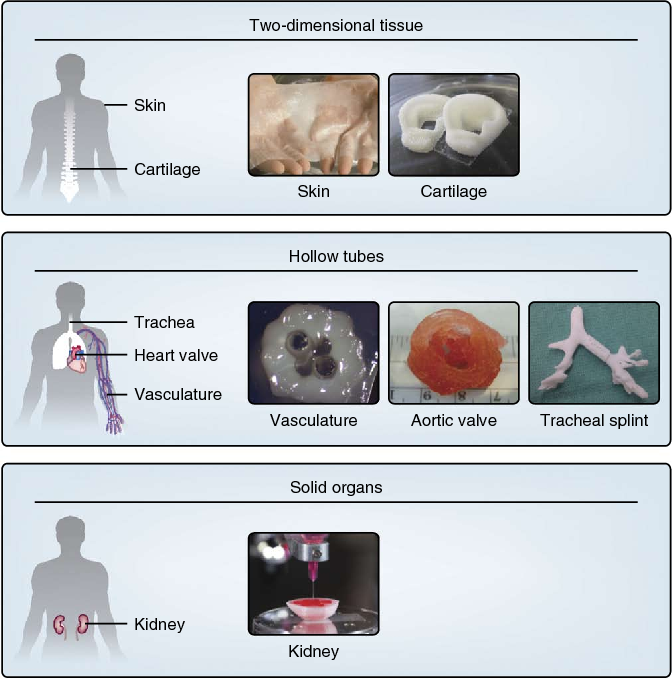 The technology is called 3D bioprinting, which has found its application in regenerative medicine and has significantly simplified and reduced the cost of transplantation of vital tissues and organs.
The technology is called 3D bioprinting, which has found its application in regenerative medicine and has significantly simplified and reduced the cost of transplantation of vital tissues and organs.
Bioengineer Thomas Boland at Clemson University in South Carolina (USA) independently modified Lexmark and HP printers to try to print human DNA fragments. The study showed that the size of DNA cells is similar to the size of a drop of standard ink and is about 10 microns. Further experiments showed that 90% of cells remain viable during the bioprinting process. In 2003, the scientist patented bioprinting, the first successful printing occurred in 2006.
The first successful experiment in 3D printing of human organs took place in 2006. Scientists at the Wake Forest Institute for Regenerative Medicine designed and printed seven bladders for patient volunteers.
Scientists-bioengineers took patient stem cells as a basis, with the help of which future organs were printed. Donor tissue samples stored in a special sealed chamber were applied by an extruder over a 3D model of the bladder, heated to the natural temperature of the human body.
Donor tissue samples stored in a special sealed chamber were applied by an extruder over a 3D model of the bladder, heated to the natural temperature of the human body.
Results: Eight weeks later, during intensive growth, the cells began to divide and recreate the bladder.
Depending on the selected 3D printer, the donor material is dosed from the dispenser. This approach is used to print soft tissues with low cell density. For example, when printing pieces of skin or soft cartilage. The method of layer-by-layer fusing is used for printing bone implants.
Seal of human hearts
A group of scientists from the ETH Zurich Switzerland in 2017 made the world's first 3D printed heart, very small: its prototype weighs only 390 grams and withstands about three thousand contractions, but it is created from human fat cells and connective tissue. The breakthrough of physicians is that before them, synthetic substances were used to create human hearts.
Scientists from Switzerland have been able to develop a prototype of the heart, which will be as similar as possible to the human organ. The heart consists of two ventricles, which are separated by a special chamber that replaces the heart muscle. The air pump deflates and inflates the chamber, allowing fluid to be pumped through the heart.
The heart consists of two ventricles, which are separated by a special chamber that replaces the heart muscle. The air pump deflates and inflates the chamber, allowing fluid to be pumped through the heart.
The cornea was first printed on a 3D printer. The material is called bioink. Using the simplest 3D bioprinter in the university's arsenal, doctors have successfully printed forms that are as similar as possible to human corneas. Printing took about 10 minutes.
Stem cells printed with bioink began to grow, transforming into a human cornea. Swiss bioengineers have been able to demonstrate that they can print corneas that fit the unique dimensions of the human cornea. The characteristics of the printed tissue were taken from the real cornea. The researchers scanned the patient's eye and were then able to print a cornea that perfectly matched the size and shape.
3D printed middle ear for hearing restoration
In 2017 Radiological Society of North America, Dr. Jeffrey Hirsch at the University of Maryland in Baltimore, USA. The CT scan images were converted into 3D printed prostheses. With their help, surgeons placed four different-sized implants in human ears.
Jeffrey Hirsch at the University of Maryland in Baltimore, USA. The CT scan images were converted into 3D printed prostheses. With their help, surgeons placed four different-sized implants in human ears.
As part of the experiment, four surgeons alternately injected prototypes into four different human middle ears. The fact that all doctors were able to perfectly match the printed prosthesis to the temporal bone is amazing: with a conventional middle ear prosthesis, the chances of a successful operation are reduced to 1: 1296.
Orthopedic corsets
2014, Stanford University, USA 3D Systems, James Policy, Robert Jensen - created a unique exoskeleton.
Doctors tested a 3D printed corset on 22 patients treated at Auckland Children's Hospital. It turned out that the corset not only perfectly corrects scoliosis, but also likes little patients. In addition, in 2014, 3D Systems again made a splash by demonstrating a unique exoskeleton. With his help, the paralyzed girl was able to get to her feet.
In dentistry
1990, 2012, Align Technology, Layer Wise, USA
The first attempts to introduce additive technologies into dentistry were crowned with relative success. With the help of the first 3D printers, scientists were able to print mouthguards for teeth. It took scientists about 20 years to make the first dental implant. In 2012, a titanium mandible made using a 3D dental printer was implanted for the first time.
Nowadays, 3D technologies have become an integral part of dentistry: dentures, orthodontic models, correction plates and veneers are printed using 3D printers.
Mobile Infection Detector Print
A group of American engineers and scientists, USA, 2017.
Scientists have developed a unique complex for diagnosing infectious diseases. As a mobile detector, a simple cell phone is used, in which a diagnostic chip is implanted.
The Mobile Infection Detector is indispensable in resource-constrained settings. In addition, the system allows for personalized treatment of the infected and timely monitoring of the epidemiological situation. The time for obtaining results is similar to the time for conducting such tests under standard laboratory conditions.
In addition, the system allows for personalized treatment of the infected and timely monitoring of the epidemiological situation. The time for obtaining results is similar to the time for conducting such tests under standard laboratory conditions.
Seal of the ovaries
Scientists at Northwestern University Chicago, USA, 2017.
Doctors and scientists have developed a unique artificial ovary that allows a woman to fully restore her reproductive function.
In this study, a 3D-printed ovary prosthesis was implanted in a sterile laboratory mouse. Subsequently, mice were born who not only survived, but were able to produce offspring. It is not yet clear whether it will be possible to replace such an ovary in a woman, since human follicles grow much faster.
Skull
Doctors from Chung-Ang University, South Korea, 2016.
Doctors were able to print a three-dimensional model of the skull and implant it in a person. The operation helped to save a human life: a part of the patient's skull was removed due to cerebral edema.
Scientists have printed a piece of the skull from pure titanium. This material is recognized as one of the best in the creation of implants. The metal has a low probability of rejection by the body.
3D printed surgical instruments invented
Research team, Walter Reed Medical Center, 2006-2014.
Scientists have invented 3D printed surgical instruments that are still widely used in medicine and the educational process of medical students: 3D anatomical prototypes, visual teaching aids, prostheses.
Medicines
Pharmaceutical company Aprecia Pharmaceuticals, USA, 2015.
The first 3D printed drug was Spritam. A few years later, the British biotechnology corporation FabRx appeared in London, introducing 3D printing in the manufacture of pharmaceuticals. Not too many examples came out, since there are only a few companies using additive technologies in pharmacology.
Individual sensors
Scientists at Washington University in St. Louis USA, 2016.
Louis USA, 2016.
Scientists used scanned copies of the hearts of experimental animals to then print 3D prototypes, around which movable and flexible individual silicone sensors were placed.
3D volume sensors can be removed from a printed prototype and attached to the human heart. Such sensors can monitor the work of the heart muscle in order to prevent heart attacks, strokes and other dangerous diseases. And although so far individual sensors are used only outside, scientists do not deny the possibility of introducing them directly into the human body.
Spain starts printing ventilators on 3D printers
Leitat Technological Center laboratory, Spain, 2020.
Invented an inexpensive ventilator that can be 3D printed.
The 3D printed ventilator is almost ready for mass production. The price of the device is about €500. Scientists plan that soon they will be able to get approval from the government and set up production, providing the country with the necessary amount of equipment.
HP Inc. began 3D printing medical products to combat coronavirus
HP Corporation, USA, 2020.
As part of the fight against the coronavirus pandemic, HP Inc. launched the production of 3D parts for ventilators and other equipment, as well as essential goods for both ordinary citizens and medical institutions. The corporation called on the help of its partners around the world to set up and optimize the mass production of essential goods as quickly as possible.
Products have already been successfully tested. The company produces the following groups of products: protective masks, face shields, mask holders, disposable earplugs, respirators, devices for safe window opening.
Medical masks in Russia began to be printed on a 3D printer
Temporum, Russia, 2020.
Temporum has developed its own mask printing technology. Products are created using reliable FDM technology: the model is built up in layers from a pre-melted filament. The company uses PETG as the plastic. This is the safest material from which excellent reusable masks are obtained. The user only needs to change the internal filter in a timely manner.
The company uses PETG as the plastic. This is the safest material from which excellent reusable masks are obtained. The user only needs to change the internal filter in a timely manner.
Results: 3D printed reusable masks are much more profitable than their disposable counterparts. Considering the fact that the company recommends using regular cotton pads instead of filters, buying such a mask becomes very profitable. Temporum is reportedly already in talks to mass-produce printed masks.
Hospitals in Italy began purchasing 3D printed devices
Hospitals in northern Italy, 2020
When hospitals in Northern Italy experienced a severe shortage of spare parts for resuscitators during the coronavirus pandemic, Massimo Temporelli, founder of FabLab, offered his help to hospitals left without the necessary equipment. The company provided medical institutions with cheap but high-quality breathing tubes for intensive care units. FabLab came to the aid of Isinnova, which brought a 3D printer directly to the hospital. A few hours later, the doctors received the necessary spare parts.
A few hours later, the doctors received the necessary spare parts.
As a result, about 10 patients in an Italian hospital survived thanks to a device for which a valve was printed on a 3D printer. If the companies did not come to the aid of doctors, the resuscitation system would have to be turned off, which would lead to the inevitable death of patients. Other Italian companies have not stood aside: hospitals are already using 3D parts for ventilators, made using the technology of powder sintering under the action of a polymer laser.
Creation of 3D models of organs before surgeries in Dubai
Dubai Health Authority, DHA.
In October 2016, major medical institutions in Dubai purchased 3D printers. With the help of devices, doctors planned to create the most accurate prototypes of patients' organs. Thanks to the new technology, surgeons have been able to study diseased organs before surgery, increasing the efficiency and accuracy of surgical intervention. What's more, most of Dubai's hospitals are already equipped with additive printing equipment for teeth, bone prostheses and human organ models, which doctors need in preparation for operations.
What's more, most of Dubai's hospitals are already equipped with additive printing equipment for teeth, bone prostheses and human organ models, which doctors need in preparation for operations.
It is expected that by 2030 the vast majority of medical institutions in Dubai will be equipped with 3D printers. Doctors note that three-dimensional technologies have significantly simplified the process of preparing for operations and minimized the likelihood of medical errors.
Liver
Scientists from the University of Kyushu, Japan, 2017.
Japanese scientists were able to 3D print a biotransplantation tissue of the liver, which was successfully transplanted into the body of a rat. Doctors are sure that soon they will be able to print organs for people.
Scientists conducted a unique experiment, creating a "scalable" liver tissue. To create it, they needed to connect hundreds of hepatic-renal spheroids, a 3D printer helped them in this. A system for fixing liver tissue using needle arrays helped researchers ensure proper circulation of blood and oxygen through the liver, successfully avoiding organ ischemia.