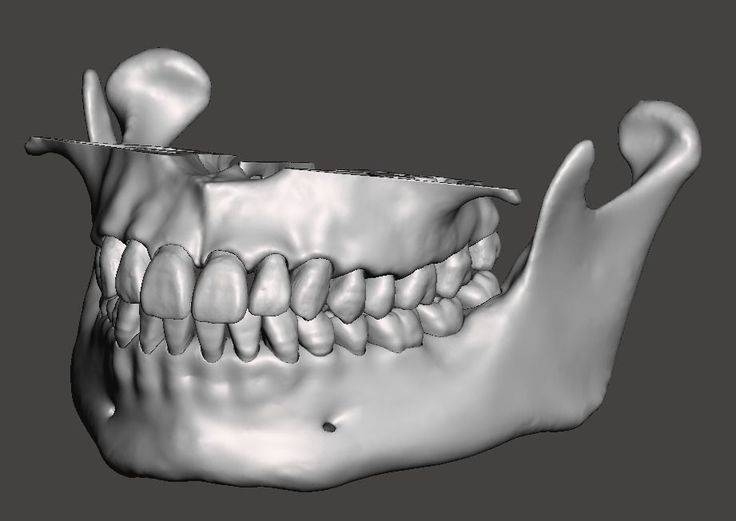
3D printed mandible
3D-printed titanium implant with pre-mounted dental implants for mandible reconstruction: a case report | Maxillofacial Plastic and Reconstructive Surgery
- Case report
- Open Access
- Published:
- Jung-Hyun Park1,
- Michidgerel Odkhuu2,
- Sura Cho3,
- Jingwen Li4,
- Bo-Young Park5 &
- …
- Jin-Woo Kim ORCID: orcid.org/0000-0002-1672-57303
Maxillofacial Plastic and Reconstructive Surgery volume 42, Article number: 28 (2020) Cite this article
-
5328 Accesses
-
19 Citations
-
Metrics details
Abstract
Background
This clinical case presented a novel method of segmental mandible reconstruction using 3D-printed titanium implant with pre-mounted dental implants that was planned to rehabilitate occlusion.
Case presentation
A 53-year-old male who suffered osteoradionecrosis due to the radiation after squamous cell carcinoma resection. The 3D-printed titanium implant with pre-mounted dental implant fixtures was simulated and fabricated with selective laser melting method. The implant was successfully inserted, and the discontinuous mandible defect was rehabilitated without postoperative infection or foreign body reaction during follow-ups, until a year.
Conclusions
The 3D-printed titanium implant would be the one of the suitable treatment modalities for mandible reconstruction considering all the aspect of mandibular functions.
Background
Reconstruction of mandibular defect resulting from segmental mandibulectomy is one of many challenges faced by oral surgeons [1]. Segmental defect of the mandible, whatever the cause—benign tumor, malignant tumor, osteomyelitis, or osteoradionecrosis—impacts both facial esthetics and oral functions such as mastication, swallowing, and speaking. Many reconstruction modalities have been reported to achieve optimal functional and aesthetic results. Conventional modalities for mandibular reconstruction include reconstruction plate, microvascular fibula free flap, iliac bone graft, costochondral rib bone graft, and alloplastic prosthesis [2]. When the segmental defect is large, microvascular free flap has been the golden standard of mandibular reconstruction. It allows dental implant installation, enabling the recovery of mandibular function as well as mandibular shape and aesthetics. Autogenous graft, however, has its disadvantages such as donor site morbidity, extended operation time, and potential graft failure due to tissue necrosis [2].
Many reconstruction modalities have been reported to achieve optimal functional and aesthetic results. Conventional modalities for mandibular reconstruction include reconstruction plate, microvascular fibula free flap, iliac bone graft, costochondral rib bone graft, and alloplastic prosthesis [2]. When the segmental defect is large, microvascular free flap has been the golden standard of mandibular reconstruction. It allows dental implant installation, enabling the recovery of mandibular function as well as mandibular shape and aesthetics. Autogenous graft, however, has its disadvantages such as donor site morbidity, extended operation time, and potential graft failure due to tissue necrosis [2].
Recent development in three-dimensional (3D) printing technology enabled fabrication of customized prosthesis. 3D-printed titanium implant has successfully been used for the reconstruction of facial bone defect including the mandible. The advantage of 3D-printed titanium implant is that it can be designed according to the defect size and morphology [3]. Customized titanium implants can be fitted accurately in the defective site without interference [4]. It allows for reduced operating time and also recovers the original contour of the mandible and facial symmetry. Even so, 3D-printed titanium implant has its limitations regarding oral function in occlusal rehabilitation.
Customized titanium implants can be fitted accurately in the defective site without interference [4]. It allows for reduced operating time and also recovers the original contour of the mandible and facial symmetry. Even so, 3D-printed titanium implant has its limitations regarding oral function in occlusal rehabilitation.
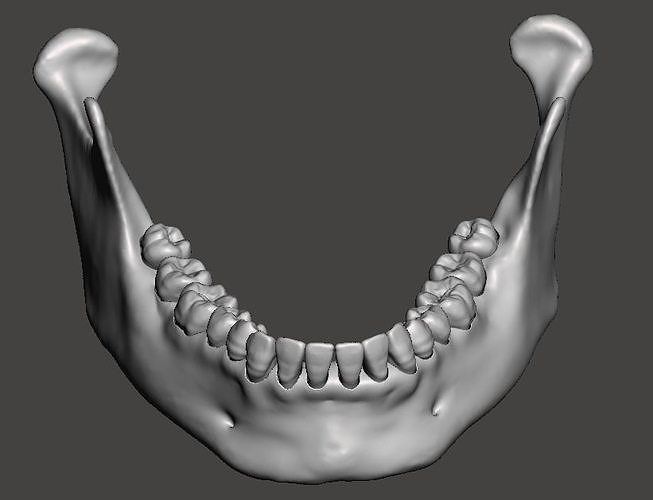
The purpose of mandibular reconstruction is not only to re-establish the morphology of the lower third of the face but also to restore the patient’s oral function such as mastication and pronunciation [5]. This clinical case presents a novel method of mandible reconstruction using 3D-printed custom titanium implant in a patient who suffered from osteoradionecrosis due to radiation after squamous cell carcinoma resection. To rehabilitate dentition, we installed dental implants into the 3D-printed titanium mandibular implant. To the best of our knowledge, this is the first report on 3D-printed titanium implant with pre-mounted dental implants, attempting to overcome the limitations of dental implant-less titanium implant in dental rehabilitation.
Case presentation
A 53-year-male was presented to Ewha Womans University Mokdong Hospital, diagnosed with squamous cell carcinoma of attached gingiva in the left mandible. After whole body examination including magnetic resonance images and positron emission tomography scan, metastasis to neck lymph node was confirmed, and the patient was staged cT4N1M0 by American Joint Committee on Cancer Cancer Staging. Wide excision and marginal mandibulectomy of the left mandible preserving the inferior border of the mandible as well as modified radical neck dissection were performed. For reinforcement, reconstruction plate was applied. Intraoral defect was closed with an anterolateral thigh flap. The permanent biopsy revealed tumor invasion to the inferior alveolar nerve; thus, postoperative radiation therapy with total dose of 60 Gy was performed 2 months after operation. After radiation therapy, the patient showed extra oral skin fistula on the left mandible. The fistula was closed using thoracodorsal artery perforator flap.
At the 1-year follow-up, the patient presented discomfort from changes in occlusion. Destructive bony change of the left mandibular body and pathologic fracture was observed in the panoramic radiograph and computed tomography (Fig. 1). Along with increased uptake on bone scintigraphy, the patient was diagnosed with osteoradionecrosis (ORN), and segmental mandibulectomy with reconstruction was planned for treatment. The patient was informed of the treatment options including autogenous microvascular free flap and 3D-printed titanium mandibular implant. The patient preferred a single surgical site to avoid donor site morbidity. Thus, customized 3D titanium implant, rather than the conventional fibula reconstruction, was selected for mandible reconstruction.
Fig. 1Pathologic fracture of the left mandibular body was observed in the panoramic radiograph
Full size image
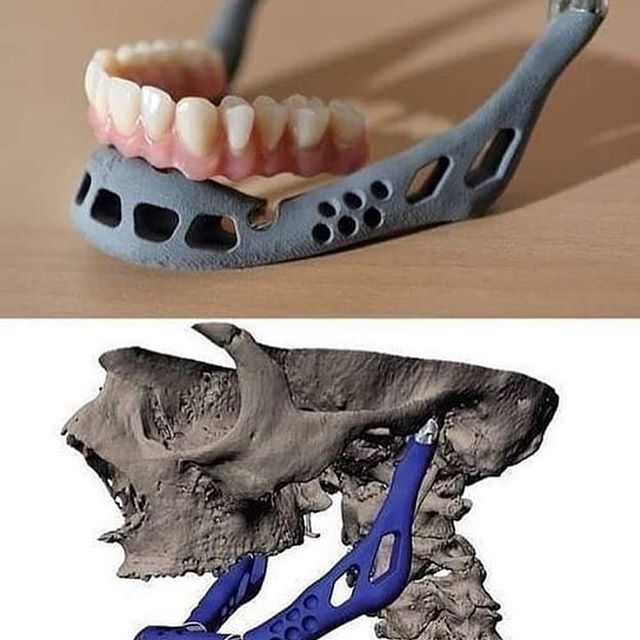
Pre-surgical simulation based on CT data was performed using image processing software (Mimics, Materialise, Belgium). The resection margin was carefully planned in accordance to the ORN lesion. Since the left proximal segment was rotated anterosuperiorly due to fracture, the segment was repositioned on the simulation using contralateral condylar position as the reference. The mandibular implant was designed to restore the original mandibular shape. Resection guide and titanium mandibular implant were fabricated using a 3D printer with selective laser melting (SLM) method (Fig. 2). All surface except bone contact surface of the titanium mandibular implant was polished. Bone contact surface was maintained rough to enhance osseointegration. Seven bicortical screw holes were designed on each ends of the implant for fixation. A portion of titanium implant distant from the dental implant insertion site was hollowed to decrease weight. For future dental rehabilitation, 3 dental implant fixtures (Dio implant, Busan, Republic of Korea) were installed in the titanium mandibular implant using conventional dental implant drilling system before the operation (Fig.
The resection margin was carefully planned in accordance to the ORN lesion. Since the left proximal segment was rotated anterosuperiorly due to fracture, the segment was repositioned on the simulation using contralateral condylar position as the reference. The mandibular implant was designed to restore the original mandibular shape. Resection guide and titanium mandibular implant were fabricated using a 3D printer with selective laser melting (SLM) method (Fig. 2). All surface except bone contact surface of the titanium mandibular implant was polished. Bone contact surface was maintained rough to enhance osseointegration. Seven bicortical screw holes were designed on each ends of the implant for fixation. A portion of titanium implant distant from the dental implant insertion site was hollowed to decrease weight. For future dental rehabilitation, 3 dental implant fixtures (Dio implant, Busan, Republic of Korea) were installed in the titanium mandibular implant using conventional dental implant drilling system before the operation (Fig. 3). A titanium implant with only the female part of the fixture screw was first designed, but current SLM printing technology was unable to precisely reproduce the spiral thread of the small screw. Thus, we solely printed the titanium implant and manually installed the conventional dental implant to the titanium implant before surgery.
3). A titanium implant with only the female part of the fixture screw was first designed, but current SLM printing technology was unable to precisely reproduce the spiral thread of the small screw. Thus, we solely printed the titanium implant and manually installed the conventional dental implant to the titanium implant before surgery.
3D-printed resection guide and titanium mandibular implant
Full size image
Fig. 3Dental implant fixtures were installed in the titanium mandibular implant
Full size image
Under general anesthesia, skin incision on the left neck was made through the existing scar. Pre-existing reconstruction plate and screws were removed, and the affected mandible was resected using 3D printed resection guides. Resection guides were well fitted on the mandible body according to the virtual plan. Subsequently, the titanium implant was inserted to the resected area and fixed using bicortical screws on the remaining mandible (Fig. 4). The dental implant was completely submerged inside the oral mucosa, and its exposure was planned in the subsequent second surgery. Recovery was uneventful, and the patient was discharged on the seventh day after surgery. At the 1-year follow-up after the operation, there were no evidences of postoperative infection or foreign body reaction. Pre-mounted implants were exposed during the second surgery for abutment placement, but the peri-implant mucosal healing was unfavorable; thus, the wound was closed, and implant exposure was re-planned for the future. The surgical protocol is available at https://www.youtube.com/watch?v=rd7FkbESRpA.
4). The dental implant was completely submerged inside the oral mucosa, and its exposure was planned in the subsequent second surgery. Recovery was uneventful, and the patient was discharged on the seventh day after surgery. At the 1-year follow-up after the operation, there were no evidences of postoperative infection or foreign body reaction. Pre-mounted implants were exposed during the second surgery for abutment placement, but the peri-implant mucosal healing was unfavorable; thus, the wound was closed, and implant exposure was re-planned for the future. The surgical protocol is available at https://www.youtube.com/watch?v=rd7FkbESRpA.
Titanium implant was inserted to the resected area of left mandible
Full size image
Discussion
This clinical case presents a novel method of mandible reconstruction using 3D-printed titanium implant with pre-mounted dental implants to improve mandibular function. Recent application of 3D printing technology to medicine allows precise patient-specific preoperative design of implants. Surgeons are able to design the implant in ways to restore the original features, and greater implant stability is expected with an accurate fit in the defective site without interference [6]. 3D printing has many advantages over traditional methods such as its ability to fabricate complex structures, its improved customization, and its time efficiency.
Surgeons are able to design the implant in ways to restore the original features, and greater implant stability is expected with an accurate fit in the defective site without interference [6]. 3D printing has many advantages over traditional methods such as its ability to fabricate complex structures, its improved customization, and its time efficiency.
3D-printed titanium implant has been used in various fields of facial reconstruction including the mandible for its mechanical strength that can support mandibular movement [6,7,8]. Unlike other facial compartments, reconstruction of the maxilla or mandible requires careful consideration of dental rehabilitation. Mastication and pronunciation are important functions of the mandible that can be restored with dental rehabilitation. The most widely used method for dental rehabilitation is the installation of dental implants to the vital bone for osseointegration. However, the use of titanium implant for occlusal rehabilitation is limited in that dental implants cannot be installed to the implant body itself.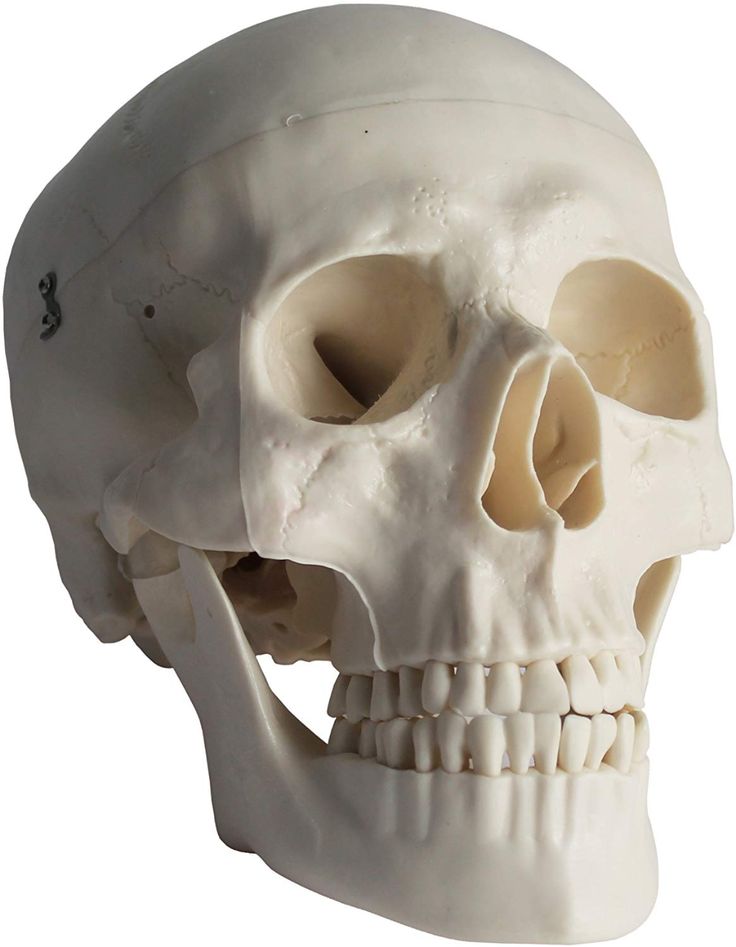
There are several ways to install fixed prosthesis on titanium implants, one of which is via the abutment designed as part of the titanium implant [9]. Lee et al. reported the use of titanium mandibular implant with 2 abutment projections to rehabilitate occlusion [9]. Another possible way to install fixed prosthesis is by installing the conventional dental implant to the titanium implant as illustrated in this report. Because the exposure of titanium mandibular implant immediately leads to infection of the implant and eventual failure, dental implant insertion was done before the reconstruction surgery to avoid immediate exposure to the oral cavity. The concept of submerged dental implant procedure was applied. This aimed to allow initial healing period for osseointegration to the titanium mandible and promote barrier formation of soft tissue surrounding the titanium mandible including the periosteum. After this period, the dental implants were exposed to the oral cavity, and procedures for permanent prosthesis installation were carried out by the conventional method.
One of main goals of mandibular reconstruction is to restore the patient’s oral function such as mastication, swallowing, and pronunciation. The use of vascularized bone flap technique has been the golden standard for mandibular reconstruction treatment because it allows dental implant installation, promoting occlusal rehabilitation. Previously reported limitation of titanium implant was its inability for implant insertion [9], but in this report, 3D-printed titanium mandible implant was efficiently used in mandibular reconstruction with pre-mounted dental implant for occlusal rehabilitation. To avoid the risk of infection, the concept of submerged dental implant was applied. Although the soft tissues surrounding the titanium implant needs to be closely monitored after exposing the dental implant in the second surgery for any risk of infection, this case presents the possibility of conventional dental implant installation into titanium implant, which will play an important role in the rehabilitation of masticatory function for mandibular reconstruction.
Conclusions
This case demonstrated the possibility of conventional dental implant installation into titanium implant for occlusal rehabilitation using the concept of submerged dental implant. 3D-printed titanium implant can be a suitable treatment modality for mandible reconstruction considering all aspects of mandibular functions.
Availability of data and materials
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.
Abbreviations
- 3D:
-
Three-dimensional
- ORN:
-
Osteoradionecrosis
- SLM:
-
Selective laser melting
References
Cordeiro PG, Disa JJ, Hidalgo DA, Hu QY (1999) Reconstruction of the mandible with osseous free flaps: a 10-year experience with 150 consecutive patients.
 Plastic and reconstructive surgery 104:1314–1320
Plastic and reconstructive surgery 104:1314–1320Article Google Scholar
Jo YY, Kim SG, Kim MK, Shin SH, Ahn J, Seok H (2018) Mandibular reconstruction using a customized three-dimensional titanium implant applied on the lingual surface of the mandible. J Craniofac Surg 29:415–419
Article Google Scholar
Wilde F, Hanken H, Probst F, Schramm A, Heiland M, Cornelius CP (2015) Multicenter study on the use of patient-specific CAD/CAM reconstruction plates for mandibular reconstruction. Int J Comput Assist Radiol Surg 10:2035–2051
Article Google Scholar
Probst FA, Metzger M, Ehrenfeld M, Cornelius CP (2016) Computer-assisted designed and manufactured procedures facilitate the lingual application of mandible reconstruction plates. J Oral Maxillofac Surg 74:1879–1895
Article Google Scholar
Kumar BP, Venkatesh V, Kumar KJ, Yadav BY, Mohan SR (2016) Mandibular reconstruction: overview. J Maxillofacial Oral Surg 15:425–441
Article Google Scholar
Xue R, Lai Q, Sun S et al (2019) Application of three-dimensional printing technology for improved orbital-maxillary-zygomatic reconstruction. J Craniofac Surg 30:e127–ee31
Article Google Scholar
Qassemyar Q, Assouly N, Madar Y, Temam S, Kolb F (2018) Total nasal reconstruction with 3D custom made porous titanium prosthesis and free thoracodorsal artery perforator flap: a case report. Microsurgery 38:567–571
Article Google Scholar
Jansen J, Schreurs R, Dubois L, Maal TJJ, Gooris PJJ, Becking AG (2018) The advantages of advanced computer-assisted diagnostics and three-dimensional preoperative planning on implant position in orbital reconstruction.
 J Cranio-Maxillofacial Surg 46:715–721
J Cranio-Maxillofacial Surg 46:715–721Article Google Scholar
Lee U-L, Kwon J-S, Woo S-H, Choi Y-J (2016) Simultaneous bimaxillary surgery and mandibular reconstruction with a 3-dimensional printed titanium implant fabricated by electron beam melting: a preliminary mechanical testing of the printed mandible. J Oral Maxillofacial Surg 74:1501 e1-. e15
Google Scholar
Download references
Acknowledgements
None
Funding
This work was supported by the Technology Innovation Program (Development of craniofacial prosthesis using 3D printing additive manufacturing technology, P0008799) funded by the Ministry of Trade, Industry and Energy (MI, Korea).
Author information
Authors and Affiliations
Department of Oral and Maxillofacial Surgery, Ewha Womans University Medical Center, Seoul, Korea
Jung-Hyun Park
Graduate School of Clinical Dentistry, Ewha Womans University, Seoul, Korea
Michidgerel Odkhuu
Department of Oral and Maxillofacial Surgery, School of Medicine, Ewha Womans University, Anyangcheon-ro 1071, Yangcheon-gu, Seoul, 07985, Korea
Sura Cho & Jin-Woo Kim
Graduate School of Clinical Dentistry, Ewha Womans University, Seoul, Korea
Jingwen Li
Department of Plastic Surgery, School of Medicine, Ewha Womans University, Seoul, Korea
Bo-Young Park
Authors
- Jung-Hyun Park
View author publications
You can also search for this author in PubMed Google Scholar
- Michidgerel Odkhuu
View author publications
You can also search for this author in PubMed Google Scholar
- Sura Cho
View author publications
You can also search for this author in PubMed Google Scholar
- Jingwen Li
View author publications
You can also search for this author in PubMed Google Scholar
- Bo-Young Park
View author publications
You can also search for this author in PubMed Google Scholar
- Jin-Woo Kim
View author publications
You can also search for this author in PubMed Google Scholar
Contributions
JHP and MO obtained data and wrote the manuscript.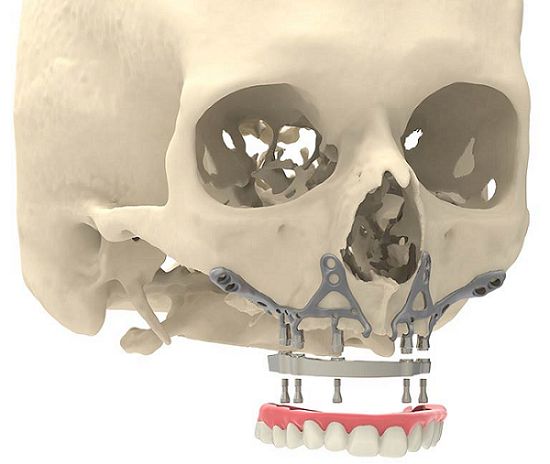 SC and JWK reviewed and revised the manuscript. JWK participated in the design of this study and manuscript revision. All authors read and approved the final manuscript.
SC and JWK reviewed and revised the manuscript. JWK participated in the design of this study and manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jin-Woo Kim.
Ethics declarations
Ethics approval and consent to participate
This study followed the Declaration of Helsinki (2000) on medical protocol and ethics and was approved by the Institutional Review Board of Ewha Medical Center, Seoul, Republic of Korea (IRB No. 2019-06-014).
Consent for publication
This manuscript does not contain any individual person’s identifier (including individual details, images, or videos).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4. 0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Patient-Specific 3D-Printed Miniplates for Free Flap Fixation at the Mandible: A Feasibility Study
Introduction
Fibula free flap (FFF) reconstruction is the treatment of choice for segmental mandibular defects.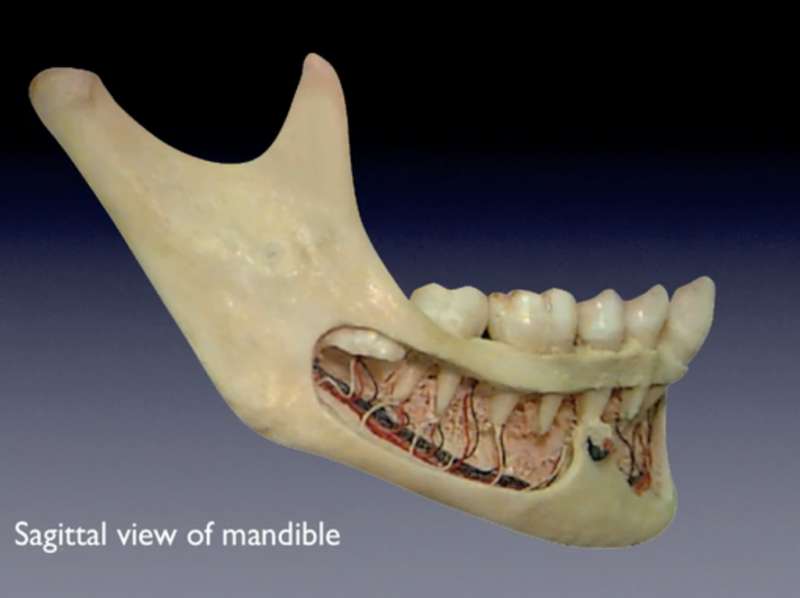 Either load-bearing (locking) reconstruction plates with bi-cortical screws or load-sharing miniplates with mono-cortical non-locking screws are used for flap fixation. Following the introduction of computer-generated models in the early 1990s (1), virtual planning was first described for mandible reconstruction in 2005 (2). The combination of the computer-aided design/computer aided manufacturing (CAD/CAM) workflow with milled and, later, selective laser-melted patient-specific reconstruction plates revolutionized mandible reconstruction with free flaps (3). The main advantages of patient-specific 3D-printed plates are high surgical precision, efficiency, and decreased surgery time (4, 5). Higher mechanical integrity due to differences in plate design, increased bone-plate contact area, and most importantly a lack of predetermined breaking points from manual bending were also demonstrated recently (6, 7). Today, a backward-planned, fully guided CAD/CAM procedure is the state of the art, with a good aesthetic and functional outcome (Figure 1).
Either load-bearing (locking) reconstruction plates with bi-cortical screws or load-sharing miniplates with mono-cortical non-locking screws are used for flap fixation. Following the introduction of computer-generated models in the early 1990s (1), virtual planning was first described for mandible reconstruction in 2005 (2). The combination of the computer-aided design/computer aided manufacturing (CAD/CAM) workflow with milled and, later, selective laser-melted patient-specific reconstruction plates revolutionized mandible reconstruction with free flaps (3). The main advantages of patient-specific 3D-printed plates are high surgical precision, efficiency, and decreased surgery time (4, 5). Higher mechanical integrity due to differences in plate design, increased bone-plate contact area, and most importantly a lack of predetermined breaking points from manual bending were also demonstrated recently (6, 7). Today, a backward-planned, fully guided CAD/CAM procedure is the state of the art, with a good aesthetic and functional outcome (Figure 1).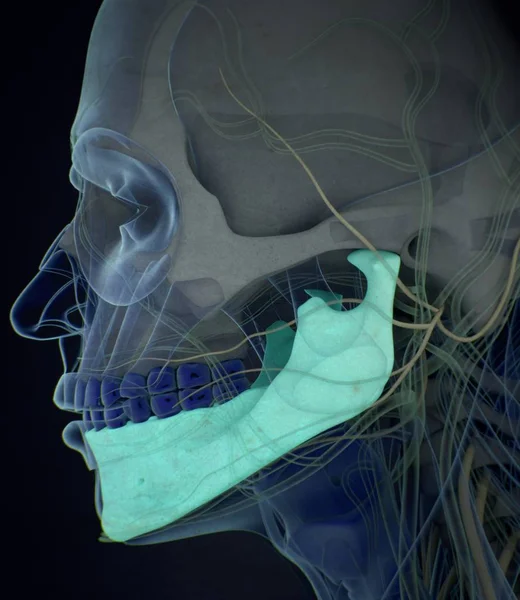
Figure 1. Demonstration of the CAD/CAM-workflow: Cutting and drilling guides placed at the mandible defect (orange) and the fibula segments (green and blue). Guides include holes for temporary guide fixation as well as permanent holes for miniplates fixation. Bottom left: Visualization of the dentition of the upper jaw (violet) and dental setup of the lower dentition (pink) for planning of the dental implant insertion. Osteotomy lines 1, 2, and 3 are also shown. Final reconstruction results with patient-specific 3D-printed miniplates are demonstrated in the bottom right corner. Created with BioRender.com.
However, plate-related complications are still common when using patient-specific reconstruction plates and do not only occur in patients with relevant risk factors like radiotherapy or multi-segmental defects (7–9). Complications also include soft tissue complications and pseudarthrosis, which are frequently observed within the first postoperative year (7). In comparison to low-profile miniplates, 2.0–3.0 mm reconstruction plates increase local compression on the surrounding tissues, which potentially favors the onset of plate exposure. Their increased stiffness reduces intersegmental movements between flap segments and between the fibula and mandible to a critically low range (10). This is unfavorable and may increase risk for pseudarthrosis, since certain amounts of micromovement and microstrain are essential for sufficient bone healing (11, 12).
In comparison to low-profile miniplates, 2.0–3.0 mm reconstruction plates increase local compression on the surrounding tissues, which potentially favors the onset of plate exposure. Their increased stiffness reduces intersegmental movements between flap segments and between the fibula and mandible to a critically low range (10). This is unfavorable and may increase risk for pseudarthrosis, since certain amounts of micromovement and microstrain are essential for sufficient bone healing (11, 12).
In contrast, load-sharing miniplates transmit applied loads through both the plate and the bone, which stimulates bone healing under frictional contact between the bone segments (13). From a mechanobiological point of view, the use of miniplates is therefore beneficial. Additionally, plate removal due to plate-related complications or in the course of preparing the patient for dental implantation and, later, prosthetic rehabilitation (14) is easier with miniplates and reduces the risk of damaging the vascular pedicle or marginal mandibular branch of the facial nerve (15). The use of conventional miniplates for free flap fixation has been described several times (16, 17). However, complications also occur with conventional miniplates (18), and plate fractures are registered more frequently (8). This is due to pre-determined breaking points during manual bending with forceps and potential poor anatomical reduction of the (joint-carrying) segments, setting the fixation under unfavorable pre-stress (19).
The use of conventional miniplates for free flap fixation has been described several times (16, 17). However, complications also occur with conventional miniplates (18), and plate fractures are registered more frequently (8). This is due to pre-determined breaking points during manual bending with forceps and potential poor anatomical reduction of the (joint-carrying) segments, setting the fixation under unfavorable pre-stress (19).
Considering the well-known advantages of the CAD/CAM workflow and patient-specific plates in general (efficiency, handling, no predetermined breaking points) together with the advantages of miniplates (mechanobiology, plate removal, soft tissue management), it was hypothesized that the combination of both worlds could significantly improve the clinical outcome after mandible reconstruction with free flaps. Accordingly, this feasibility study aimed to be the first to evaluate patient-specific 3D-printed miniplates for free flap fixation.
Materials and Methods
Ethical approval was obtained by the local ethics committee (EA2/138/18). The cases represent the first clinical use of patient-specific 3D-printed miniplates for mandible reconstruction. The inclusion period was between July and November 2019. Only patients planned for segmental mandibular resection due to malignant or benign tumors or osteoradionecrosis and primary reconstruction with a mono- or dual-segmental fibula free flap were included. A minimum clinical and radiological postoperative follow-up period of 6 months was required. Follow-up analysis was performed until December 2020. Multisegmented fibula free flaps (>2 segments) and bruxism were exclusion criteria.
The cases represent the first clinical use of patient-specific 3D-printed miniplates for mandible reconstruction. The inclusion period was between July and November 2019. Only patients planned for segmental mandibular resection due to malignant or benign tumors or osteoradionecrosis and primary reconstruction with a mono- or dual-segmental fibula free flap were included. A minimum clinical and radiological postoperative follow-up period of 6 months was required. Follow-up analysis was performed until December 2020. Multisegmented fibula free flaps (>2 segments) and bruxism were exclusion criteria.
The CAD/CAM planning procedure followed previously reported workflow (20): All patients underwent preoperative CT/cone beam CT (CBCT) scans of the mandible and CT angiography of the lower extremities to check the perfusion status and to provide 3D data for virtual planning. In patients with malignancies, the treatment protocol was defined after staging completion in an interdisciplinary tumor conference.
Tomographic imaging data of both the donor and recipient sites were uploaded to cloud-based software (IPS Gate, KLS Martin Group, Mühlheim, Germany). Resection margins were defined according to the radiological and clinical findings by a senior consultant of the Department of Oral and Maxillofacial Surgery, Charité – University Medicine, Berlin (Germany). Flap reconstruction and the design of cutting and drilling guides and plates were virtually performed in web meetings with engineers from the manufacturer and a senior consultant (KLS Martin Group, Mühlheim, Germany). The plate thickness was 1.0 mm, the screw diameter was 2.0 mm, and the screw length was 7.0 mm. As with patient-specific 3D-printed reconstruction plates, a linear plate design was chosen to increase fatigue strength between the plate holes. Each intersegmental gap was bridged with two 4-hole miniplates on the vestibular side. The placement of the 3D-printed miniplates was in accordance with the biomechanical tension lines in fracture treatment. The design of some plates was modified to preserve the function of the mental nerve. Cutting and drilling guides were 3D printed. 3D-printed miniplates were manufactured by a laser-melting procedure.
The design of some plates was modified to preserve the function of the mental nerve. Cutting and drilling guides were 3D printed. 3D-printed miniplates were manufactured by a laser-melting procedure.
In patient 7, a combined approach with anterior miniplates and a posterior reconstruction plate was performed. This was because a previous fibula free flap had been transplanted and needed surgical revision and a second FFF due to osteoradionecrosis. A posterior reconstruction plate was chosen due to the small dimensions of the previous flap.
Resection, flap harvesting, and reconstruction with miniplates were performed in a 2-team approach by senior consultants. Flap harvesting was performed using the lateral approach. A piezoelectric bone-cutting device was used for all osteotomies after guide fixation (Piezosurgery, Mectron, Cologne, Germany). Monocortical 2.0 mm non-locking screws with a length of 7.0 mm were used for plate fixation. Prolene 8.0 single-button sutures were used for both arterial and venous anastomosis. Alternatively, a coupler system was used for venous anastomosis. Intraoral wound closure was performed with Vicryl 3-0. Subcutaneous Fraxiparin® 0.3 mL was administered twice a day for 1 week. Initial nutrition was ensured with a nasogastric tube. A protective tracheostomy was performed in all patients until postoperative swelling was reduced and patients were able to swallow. Flap perfusion was controlled closely during the first 7 days. After discharge, outpatient controls with intra- and extraoral examination were performed on a regular basis postoperatively, including at least 1 CT or CBCT control. In clinical examinations particular attention was paid to soft tissue complications, material failure, or osseous complications.
Alternatively, a coupler system was used for venous anastomosis. Intraoral wound closure was performed with Vicryl 3-0. Subcutaneous Fraxiparin® 0.3 mL was administered twice a day for 1 week. Initial nutrition was ensured with a nasogastric tube. A protective tracheostomy was performed in all patients until postoperative swelling was reduced and patients were able to swallow. Flap perfusion was controlled closely during the first 7 days. After discharge, outpatient controls with intra- and extraoral examination were performed on a regular basis postoperatively, including at least 1 CT or CBCT control. In clinical examinations particular attention was paid to soft tissue complications, material failure, or osseous complications.
3D Accuracy
Accuracy measurements were performed by a single independent investigator (CS) with the 3D GOM software (GOM, Braunschweig, Germany). After semi-automatic alignment of the CAD/CAM planning and the postoperative scan, which was based on the non-operated side of the mandible, the quality of fitting was determined as the mean deviation of 4 reproducible points at the contralateral ascending ramus by calculating the vector magnitude (Figure 2; green marks). The vector magnitude was also used for all other values in the precision analysis. For further analysis of accuracy measurements, care was taken to select points in the reconstruction region that could be reliably identified in all images, undisturbed by metal imaging artifacts. The deviation (planning vs. postoperative scan) of the medial and distal basal contact points at the transition of the transplant to the local bone were measured to evaluate accuracy. In addition, the most caudal point of the ipsilateral incisura semilunaris was measured to reflect the positioning of the ipsilateral ascending ramus (Figure 2; red marks). The mean of all three values (mesial gap, distal gap, ipsilateral incisura semilunaris) was determined. By subtracting the quality of fitting the corrected mean deviation was calculated. This resulted in a value demonstrating the absolute deviation (21).
The vector magnitude was also used for all other values in the precision analysis. For further analysis of accuracy measurements, care was taken to select points in the reconstruction region that could be reliably identified in all images, undisturbed by metal imaging artifacts. The deviation (planning vs. postoperative scan) of the medial and distal basal contact points at the transition of the transplant to the local bone were measured to evaluate accuracy. In addition, the most caudal point of the ipsilateral incisura semilunaris was measured to reflect the positioning of the ipsilateral ascending ramus (Figure 2; red marks). The mean of all three values (mesial gap, distal gap, ipsilateral incisura semilunaris) was determined. By subtracting the quality of fitting the corrected mean deviation was calculated. This resulted in a value demonstrating the absolute deviation (21).
Figure 2. Green marks: measurement points at the contralateral ascending ramus to evaluate the quality of fitting; red marks: measurement points at the base of the mandible at the connection of the original bone to the FFF and the most inferior point of the ipsilateral incisura semilunaris.
All data were included in a database (Microsoft Excel, Microsoft Corporation, Redmond, USA). Descriptive statistics were performed using Microsoft Excel.
Osseous Union
The degree of osseous consolidation was determined by 2 independent observers based on postoperative sectional imaging (CT or CBCT). For each osteotomy line, the highest degree of osseous consolidation was classified according to the axial view as previously published by Yla-Kotola et al. (22). Non-union was classified as a lack of apposition of the bone segments on every section of the mandible. Partial-union was determined as incomplete bone fusion in every section of the mandible. And complete union was valued as good bone fusion of the osteotomized sections of the fibula and the neomandible. This led to 2 values in single-segment reconstructions and 3 values in 2-segment transplants. Osteotomy 1 always represented the osteotomy line at the angle of the mandible (ipsilateral posterior), osteotomy 2 the ipsilateral anterior, and osteotomy 3 the contralateral osteotomy. In patient 7, the posterior gap was not quantified, as it was bridged with a reconstruction plate.
In patient 7, the posterior gap was not quantified, as it was bridged with a reconstruction plate.
Results
Eight patients (3 men and 5 women, mean age 63 ± 19 years; range 18–83 years) underwent mandible reconstruction with a fibula free flap and patient-specific 3D-printed miniplates between July and November 2019. Table 1 illustrates the patient characteristics. Certain pre-existing diseases considered were diabetes (n = 2), osteoporosis (n = 0), and vascular diseases (n = 1). Seven patients were treated due to primary oral squamous cell carcinoma (87.5%). One patient required a second fibula flap owing to osteoradionecrosis (ORN) after recent fibula reconstruction due to the resection of an Ewing‘s osteosarcoma (12.5%). Four patients received a mono-segmental and 4 patients a dual-segmental fibula flap. The mean flap length was 63 mm (SD ± 12 mm). Intraoral wound closure was performed with tibialis posterior muscle (n = 2), posterior septum (n = 2), or a skin island (n = 4). Screw insertion and plate fixation following pre-drilling with cutting and drilling guides was unproblematic, without the need for additional drilling due to imperfect fitting. Four patients (50%) received adjuvant radio(chemo)therapy. In this study, no revisional surgery was necessary, and no flap was either partially or completely lost. Radiological follow-up was performed 10 ± 2 months after surgery. Concerning patients with squamous cell carcinoma as initial diagnosis, there were no locoregional recurrences or distant metastases noted within the follow-up. Seven patients presented a clinically uneventful course regarding infections, wound healing disorders, plate exposure, and material failure. In patient 2, a late-onset infection with fistula in the canine region was registered after 4 months. Surgical exploration revealed partial screw loosening but complete osseous union of the former anterior intersegmental gap. Early plate removal in this region was therefore performed during the same procedure.
Screw insertion and plate fixation following pre-drilling with cutting and drilling guides was unproblematic, without the need for additional drilling due to imperfect fitting. Four patients (50%) received adjuvant radio(chemo)therapy. In this study, no revisional surgery was necessary, and no flap was either partially or completely lost. Radiological follow-up was performed 10 ± 2 months after surgery. Concerning patients with squamous cell carcinoma as initial diagnosis, there were no locoregional recurrences or distant metastases noted within the follow-up. Seven patients presented a clinically uneventful course regarding infections, wound healing disorders, plate exposure, and material failure. In patient 2, a late-onset infection with fistula in the canine region was registered after 4 months. Surgical exploration revealed partial screw loosening but complete osseous union of the former anterior intersegmental gap. Early plate removal in this region was therefore performed during the same procedure. In patient 7, all miniplates were removed as early as 7 months after surgery, as complete osseous union was detected in a postoperative CBCT, and the patient had advocated for short-term dental rehabilitation. Prosthetic rehabilitation was completed 13 months after reconstructive surgery in this patient, with an excellent functional and aesthetic result (Figure 3).
In patient 7, all miniplates were removed as early as 7 months after surgery, as complete osseous union was detected in a postoperative CBCT, and the patient had advocated for short-term dental rehabilitation. Prosthetic rehabilitation was completed 13 months after reconstructive surgery in this patient, with an excellent functional and aesthetic result (Figure 3).
Table 1. Patient characteristics; SCC, squamous cell carcinoma; ORN, osteonecrosis/late-onset flap loss; R(C)T, radio(chemo)therapy.
Figure 3. (A) control after placement of dental implants into the first CAD/CAM FFF with reconstruction plate, (B) partial loss of the FFF and partial removal of the reconstruction plate with re-osteosynthesis, (C) control after mandible reconstruction with the second CAD/CAM FFF with miniplates and small reconstruction plate, (D) control after intraoral removal of the miniplates and simultaneous dental implant insertion, (E) intraoperative site of (C), (F) intraoperative site of (D), (G) dental rehabilitation with implant supported fixed prosthesis (H) clinical impression 14 months postoperatively.
Precision analysis revealed that the planning could be superimposed with the postoperative imaging with high accuracy (Table 2). The values for quality of fitting were between 0.19 mm and 1.53 mm (mean value 0.7 mm). The planned reconstruction was achieved with a heterogeneous deviation between 0.82 mm and 9.72 mm. The corrected mean deviation over all marks and patients was 3.64 mm (SD ± 1.18 mm). Mean deviations in 2-segment reconstructions were found to be only slightly higher than in 1-segment reconstructions (3.84 mm vs. 3.44 mm). In the radiological assessment of intersegmental regions, only 1 gap was classified as a partial union, while all other gaps were defined as complete osseous unions (Table 3).
Table 2. Precision Analysis.
Table 3. Qualitative analysis of osseous union (1 = non-union, 2 = partial-union, 3 = union).
Discussion
Plate-related complications after mandible reconstruction with free flaps are common, and neither conventional and patient-specific reconstruction plates nor conventional miniplates can be considered as ideal fixation systems given the specific needs of patients undergoing this procedure. We conducted a study to examine the feasibility of newly designed patient-specific 3D-printed miniplates.
We conducted a study to examine the feasibility of newly designed patient-specific 3D-printed miniplates.
The precise implementation of preoperative planning represents the greatest advantage of the CAD/CAM technology. Accuracy plays a prominent role in the reconstruction of the lower jaw, as it directly influences the restoration or maintenance of the occlusion and the pitch of the temporomandibular joints, and thus function and aesthetics. In this study, the preoperative VSP (virtual surgical planning) was compared to the postoperative result. With a corrected mean deviation of 3.64 mm over all marks and patients, a high level of accuracy was achieved with 3D-printed miniplates. Comparison of accuracy measurements is difficult, since a wide range of measurement techniques has been described for VSP mandible reconstruction (23–31), and the results also depend on the defect. In a systematic review, van Baar et al. identified several reasons that postoperative results never fully match virtual plans, including image acquisition, segmentation, 3D printing, surgery, and evaluation (26). Among 42 studies, they found deviations ranging from 0 to 12.5 mm, demonstrating that computer assisted mandible reconstruction is superior to conventional plating techniques, with 2.81–6.35 mm greater deviations of the condyle in the conventional plating group. The results of the current study are at the upper end of this scale. Its high accuracy is further underlined by the fact that no malocclusion was found in any of the patients. Comparison of our study with the review by van Baar et al. needs to be performed cautiously due to different analyzation method and software.
Among 42 studies, they found deviations ranging from 0 to 12.5 mm, demonstrating that computer assisted mandible reconstruction is superior to conventional plating techniques, with 2.81–6.35 mm greater deviations of the condyle in the conventional plating group. The results of the current study are at the upper end of this scale. Its high accuracy is further underlined by the fact that no malocclusion was found in any of the patients. Comparison of our study with the review by van Baar et al. needs to be performed cautiously due to different analyzation method and software.
The high precision achieved by the CAD/CAM technology may positively affect development of pseudarthrosis. Several factors influence bone healing, both in general and after free flap reconstruction of the mandible. Bone healing will not occur when bone segments are mal-positioned and no adequate contact area exists. Osseous union at the osteotomy site after free flap reconstruction is indicative of successful flap surgery with high precision (32).:background_color(FFFFFF):format(jpeg)/images/article/en/mandibular-foramen/7YaI0UXzmSfT6NqOTkMb5A_d2DFbcWqOqSTAXfJrVg3Mg_Foramen_mandibulae_01.png) There is no standardized procedure for evaluating the ossification in the osteotomy gap (22, 32–34). This is even more challenging because there is no radiological definition of a “healed” fracture (35). The inevitable superimposition of artifacts due to the adjacent osteosynthesis significantly impairs quantitative assessment.
There is no standardized procedure for evaluating the ossification in the osteotomy gap (22, 32–34). This is even more challenging because there is no radiological definition of a “healed” fracture (35). The inevitable superimposition of artifacts due to the adjacent osteosynthesis significantly impairs quantitative assessment.
However, as far as can be concluded from the non-quantitative analysis with 8 patients, the high rate of full osseous unions in this pilot study must be outlined. Recently, it was demonstrated that partial osseous union and pseudarthrosis occur much more frequently under fixation with conventional and especially rigid patient-specific 3D-printed reconstruction plates (7, 16, 17, 34). There is a lack of prospective randomized controlled studies comparing load-bearing rigid and load-sharing miniplate fixation for mandible reconstruction, but non-union with miniplates seems less frequent (17, 36, 37). While previous and adjuvant radiotherapy, chemotherapy, and the number of segments were recently seen to be associated with impaired bone healing, differences between fixation techniques may be explained by fundamentally different biomechanical principles. The load distribution in a load-sharing osteosynthesis can lead to improved bone consolidation if the bone fragments are well-adapted. Stress shielding, as provoked by stiff reconstruction plates, is a well-known cause of a lack of consolidation due to insufficient stimulation in the osteotomy gaps (11, 12, 17, 38, 39). This is in accordance with recent findings from in vitro biomechanical analyses (6, 10), which revealed that miniplate fixation allows for more intersegmental micromovements than conventional and patient-specific 3D-printed reconstruction plates. However, in vivo evidence for this hypothesis in the context of mandible and free flap mandibular reconstruction is still missing.
The load distribution in a load-sharing osteosynthesis can lead to improved bone consolidation if the bone fragments are well-adapted. Stress shielding, as provoked by stiff reconstruction plates, is a well-known cause of a lack of consolidation due to insufficient stimulation in the osteotomy gaps (11, 12, 17, 38, 39). This is in accordance with recent findings from in vitro biomechanical analyses (6, 10), which revealed that miniplate fixation allows for more intersegmental micromovements than conventional and patient-specific 3D-printed reconstruction plates. However, in vivo evidence for this hypothesis in the context of mandible and free flap mandibular reconstruction is still missing.
Within the scope of this investigation, only 1 patient suffered a soft tissue complication, namely plate-related infection. Remarkably, no plate exposure occurred. Others found plate extrusion rates of 6–14% with miniplates, 8–24% with reconstruction plates, and 29% for CAD/CAM locking reconstruction plates (7, 16, 17). Despite this, however, no study has reported a significant difference between fixation techniques. Also from this study no general statement concerning possibly lower complication rates can be made—the patient number is too small and follow-up is too short. In terms of feasibility of patient-specific 3D-printed miniplates it can be concluded that osteosynthesis using these type of plates seems to be reliable.
Despite this, however, no study has reported a significant difference between fixation techniques. Also from this study no general statement concerning possibly lower complication rates can be made—the patient number is too small and follow-up is too short. In terms of feasibility of patient-specific 3D-printed miniplates it can be concluded that osteosynthesis using these type of plates seems to be reliable.
Regarding soft tissue management and the further clinical course, the possibility to remove miniplates at a later stage via an intraoral approach when they have been inserted using wide exposure for segmental resection from an extraoral position represents another important advantage of miniplate fixation. The complete removal of reconstruction plates, if necessary, is usually only feasible via a laborious submandibular approach. In contrast, an intraoral approach, potentially combining plate removal with dental implant insertion, enables a rapid and less stressful procedure and can be conducted in an outpatient setting.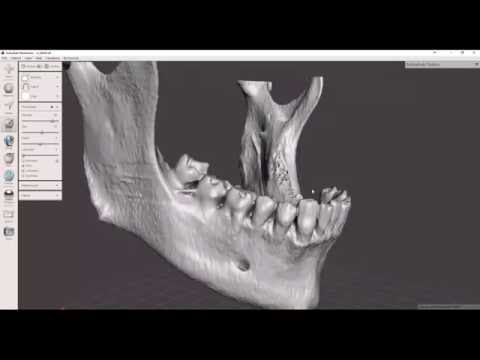 Another, so far hardly discussed, factor is the lack of compatibility of a reconstruction plate with dental rehabilitation. In patient 7, the reconstruction plate from prior mandible reconstruction was the limiting factor for both the implant position and peri-implant soft tissue management (Figure 3A). Before this patient received the second flap with miniplates, there was a local infection and, consequently, loss of the implant-bearing part of the fibula due to poor soft tissue management over the residual part of the reconstruction plate (Figure 3B). Certainly, backward-planning including positioning of dental implants is possible before surgery (40), but reconstruction plates often impede reliable soft tissue management for dental implants (20).
Another, so far hardly discussed, factor is the lack of compatibility of a reconstruction plate with dental rehabilitation. In patient 7, the reconstruction plate from prior mandible reconstruction was the limiting factor for both the implant position and peri-implant soft tissue management (Figure 3A). Before this patient received the second flap with miniplates, there was a local infection and, consequently, loss of the implant-bearing part of the fibula due to poor soft tissue management over the residual part of the reconstruction plate (Figure 3B). Certainly, backward-planning including positioning of dental implants is possible before surgery (40), but reconstruction plates often impede reliable soft tissue management for dental implants (20).
As for the CAD/CAM workflow in general (41), shifting treatment time from the operating room to the preoperative VSP is another advantage of flap fixation with patient-specific miniplates. In comparison to 3D-printed reconstruction plates we do not see a disadvantage concerning time consumption with 3D-printed miniplates due to the possibility to adapt miniplates to the fibula bone in a two team approach before isolating the fibula free flap from the leg.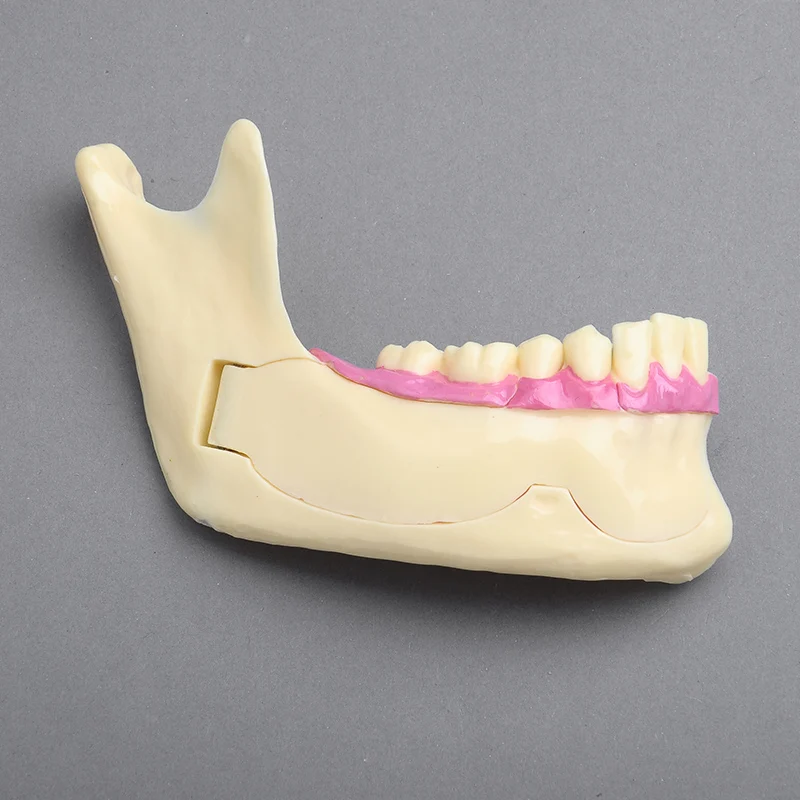 In comparison to conventional miniplates the advantage of the CAD/CAM workflow is even more important than with reconstruction plates, considering the more complex intraoperative plate bending required for sufficient anatomical repositioning.
In comparison to conventional miniplates the advantage of the CAD/CAM workflow is even more important than with reconstruction plates, considering the more complex intraoperative plate bending required for sufficient anatomical repositioning.
The limitations of this study include the small number of patients, the non-quantitative analysis of bone healing, the observational (feasibility) study design, and the lack of a control group. Our strict exclusion criteria (more than 2 segments of fibula graft and bruxism) due to reasons of safety also limit the meaningfulness to patients with more complex situations. Accordingly, neither a clear-cut recommendation to use patient-specific 3D-printed miniplates instead of patient-specific reconstruction plates nor an evidence-based demonstration of the superiority of such miniplates over conventional fixation plates can be provided. Yet, the results from this study are encouraging.
In summary, fibula free flap fixation with patient-specific 3D-printed miniplates is technically feasible, can be conducted with high accuracy, and is associated with minimal plate-related complication rates and a good chance of bone healing in the osteotomy gaps (Table 4). Following this pilot, prospective randomized controlled trials comparing the clinical outcomes and complication rates of a) conventional versus patient-specific miniplates and b) patient-specific mini- and reconstruction plates are necessary.
Following this pilot, prospective randomized controlled trials comparing the clinical outcomes and complication rates of a) conventional versus patient-specific miniplates and b) patient-specific mini- and reconstruction plates are necessary.
Table 4. Advantages of 3D-printed miniplates.
Data Availability Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Charité - Universitätsmedizin Berlin. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
KK and CR: conceived and designed the analysis, performed the analysis, and drafted this manuscript.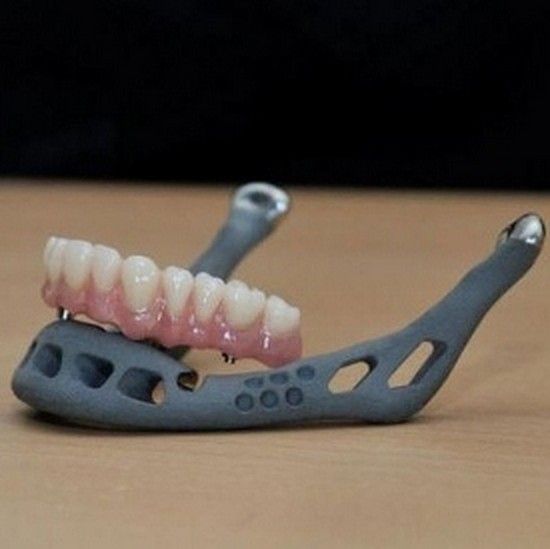 CS: collected the data, performed the analysis, and drafted this manuscript. SK and CD: collected the data and drafted this manuscript. TE, SN, and TF: drafted this manuscript. MH and BB-B: conceived and designed the analysis and drafted this manuscript. All authors contributed to the article and approved the submitted version.
CS: collected the data, performed the analysis, and drafted this manuscript. SK and CD: collected the data and drafted this manuscript. TE, SN, and TF: drafted this manuscript. MH and BB-B: conceived and designed the analysis and drafted this manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
MH received speaker remuneration by Karl Leibinger Medizintechnik GmbH and Co KG. CR received research funding for other projects by Karl Leibinger Medizintechnik GmbH and Co KG.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rose EH, Norris MS, Rosen JM. Application of high-tech three-dimensional imaging and computer-generated models in complex facial reconstructions with vascularized bone grafts. Plast Reconstr Surg. (1993) 91:252–64. doi: 10.1097/00006534-199302000-00007
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Eckardt A, Swennen GR. Virtual planning of composite mandibular reconstruction with free fibula bone graft. J Craniofac Surg. (2005) 16:1137–40. doi: 10.1097/01.scs.0000186306.32042.96
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Yang WF, Choi WS, Leung YY, Curtin JP, Du RY, Zhang CY, et al. Three-dimensional printing of patient-specific surgical plates in head and neck reconstruction: a prospective pilot study. Oral Oncol. (2018) 78:31–6. doi: 10.1016/j.oraloncology.2018.01.005
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Wilde F, Cornelius CP, Schramm A. Computer-assisted mandibular reconstruction using a patient-specific reconstruction plate fabricated with computer-aided design and manufacturing techniques. Craniomaxillofac Trauma Reconstr. (2014) 7:158–66. doi: 10.1055/s-0034-1371356
Craniomaxillofac Trauma Reconstr. (2014) 7:158–66. doi: 10.1055/s-0034-1371356
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Yang WF, Choi WS, Wong MC, Powcharoen W, Zhu WY, Tsoi JK, et al. Three-dimensionally printed patient-specific surgical plates increase accuracy of oncologic head and neck reconstruction versus conventional surgical plates: a comparative study. Ann Surg Oncol. (2021) 28:363–75. doi: 10.1245/s10434-020-08732-y
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Rendenbach C, Sellenschloh K, Gerbig L, Morlock MM, Beck-Broichsitter B, Smeets R, et al. CAD-CAM plates versus conventional fixation plates for primary mandibular reconstruction: a biomechanical in vitro analysis. J Craniomaxillofac Surg. (2017) 45:1878–83. doi: 10.1016/j.jcms.2017.08.024
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Rendenbach C, Steffen C, Hanken H, Schluermann K, Henningsen A, Beck-Broichsitter B, et al.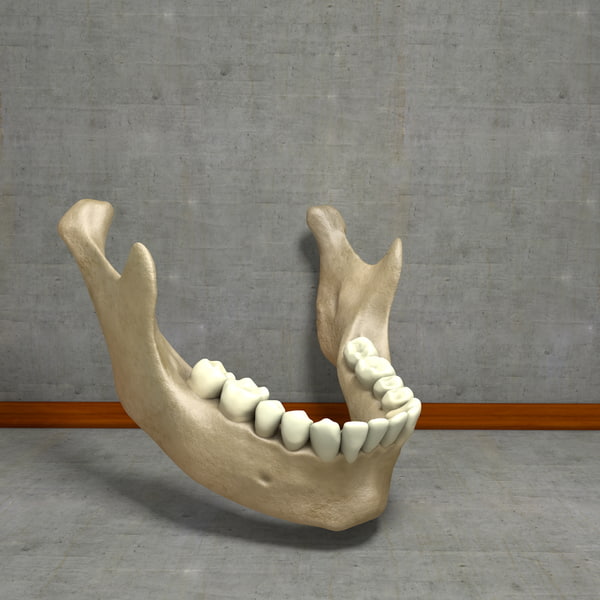 Complication rates and clinical outcomes of osseous free flaps: a retrospective comparison of CAD/CAM versus conventional fixation in 128 patients. Int J Oral Maxillofac Surg. (2019) 48:1156–62. doi: 10.1016/j.ijom.2019.01.029
Complication rates and clinical outcomes of osseous free flaps: a retrospective comparison of CAD/CAM versus conventional fixation in 128 patients. Int J Oral Maxillofac Surg. (2019) 48:1156–62. doi: 10.1016/j.ijom.2019.01.029
PubMed Abstract | CrossRef Full Text | Google Scholar
8. Brown JS, Lowe D, Kanatas A, Schache A. Mandibular reconstruction with vascularised bone flaps: a systematic review over 25 years. Br J Oral Maxillofac Surg. (2017) 55:113–26. doi: 10.1016/j.bjoms.2016.12.010
PubMed Abstract | CrossRef Full Text | Google Scholar
9. Claes L. [Mechanobiology of fracture healing part 1: principles]. Unfallchirurg. (2017) 120:14–22. doi: 10.1007/s00113-016-0280-3
PubMed Abstract | CrossRef Full Text | Google Scholar
10. Steffen C, Sellenschloh K, Polster V, Heyland M, Vollmer M, Morlock MM, et al. Biomechanical comparison of polylactide-based versus titanium miniplates in mandible reconstruction in vitro. J Stomatol Oral Maxillofac Surg. (2019) 121:377–82. doi: 10.1016/j.jormas.2019.12.001
(2019) 121:377–82. doi: 10.1016/j.jormas.2019.12.001
PubMed Abstract | CrossRef Full Text | Google Scholar
11. Frost HM. Vital biomechanics: proposed general concepts for skeletal adaptations to mechanical usage. Calcif Tissue Int. (1988) 42:145–56. doi: 10.1007/BF02556327
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Bartnikowski N, Claes LE, Koval L, Glatt V, Bindl R, Steck R, et al. Modulation of fixation stiffness from flexible to stiff in a rat model of bone healing. Acta Orthop. (2017) 88:217–22. doi: 10.1080/17453674.2016.1256940
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Claes L. [Mechanobiology of fracture healing part 2: Relevance for internal fixation of fractures]. Unfallchirurg. (2017) 120:23–31. doi: 10.1007/s00113-016-0281-2
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Wood CB, Shinn JR, Amin SN, Rohde SL, Sinard RJ. Risk of plate removal in free flap reconstruction of the mandible. Oral Oncol. (2018) 83:91–5. doi: 10.1016/j.oraloncology.2018.06.008
Oral Oncol. (2018) 83:91–5. doi: 10.1016/j.oraloncology.2018.06.008
PubMed Abstract | CrossRef Full Text | Google Scholar
15. Haubner F, Ohmann E, Pohl F, Strutz J, Gassner HG. Wound healing after radiation therapy: review of the literature. Radiat Oncol. (2012) 7:162. doi: 10.1186/1748-717X-7-162
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Shaw RJ, Kanatas AN, Lowe D, Brown JS, Rogers SN, Vaughan ED. Comparison of miniplates and reconstruction plates in mandibular reconstruction. Head Neck. (2004) 26:456–63. doi: 10.1002/hed.10343
PubMed Abstract | CrossRef Full Text | Google Scholar
17. Robey AB, Spann ML, Mcauliff TM, Meza JL, Hollins RR, Johnson PJ. Comparison of miniplates and reconstruction plates in fibular flap reconstruction of the mandible. Plastic Reconstr Surg. (2008) 122:1733–8. doi: 10.1097/PRS.0b013e31818a9ac5
PubMed Abstract | CrossRef Full Text | Google Scholar
18. Zhang ZL, Wang S, Sun CF, Xu ZF. Miniplates versus reconstruction plates in vascularized osteocutaneous flap reconstruction of the mandible. J Craniofac Surg. (2019) 30:e119–25. doi: 10.1097/SCS.0000000000005020
Miniplates versus reconstruction plates in vascularized osteocutaneous flap reconstruction of the mandible. J Craniofac Surg. (2019) 30:e119–25. doi: 10.1097/SCS.0000000000005020
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Kang SH, Lee S, Nam W. Condyle dislocation following mandibular reconstruction using a fibula free flap: complication cases. Maxillofacial Plastic Reconstr Surg. (2019) 41:14. doi: 10.1186/s40902-019-0197-1
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Kreutzer K, Steffen C, Nahles S, Koerdt S, Heiland M, Rendenbach C, et al. Removal of patient-specific reconstruction plates after mandible reconstruction with a fibula free flap: is the plate the problem? Int J Oral Maxillofac Surg. (2021) 51:182–90. doi: 10.1016/j.ijom.2021.04.003
PubMed Abstract | CrossRef Full Text | Google Scholar
21. Yang WF, Choi WS, Zhu WY, Zhang CY, Li DTS, Tsoi JKH, et al. Spatial deviations of the temporomandibular joint after oncological mandibular reconstruction. Int J Oral Maxillofac Surg. (2022) 51:44–53. doi: 10.1016/j.ijom.2021.02.033
Int J Oral Maxillofac Surg. (2022) 51:44–53. doi: 10.1016/j.ijom.2021.02.033
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Yla-Kotola TM, Bartlett E, Goldstein DP, Armstrong K, Gilbert RW, Hofer SO. Union and bone resorption of free fibular flaps in mandibular reconstruction. J Reconstr Microsurg. (2013) 29:427–32. doi: 10.1055/s-0033-1343953
PubMed Abstract | CrossRef Full Text | Google Scholar
23. Metzler P, Geiger EJ, Alcon A, Ma X, Steinbacher DM. Three-dimensional virtual surgery accuracy for free fibula mandibular reconstruction: planned versus actual results. J Oral Maxillofac Surg. (2014) 72:2601–12. doi: 10.1016/j.joms.2014.07.024
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Ciocca L, Marchetti C, Mazzoni S, Baldissara P, Gatto MR, Cipriani R, et al. Accuracy of fibular sectioning and insertion into a rapid-prototyped bone plate, for mandibular reconstruction using CAD-CAM technology. J Craniomaxillofac Surg.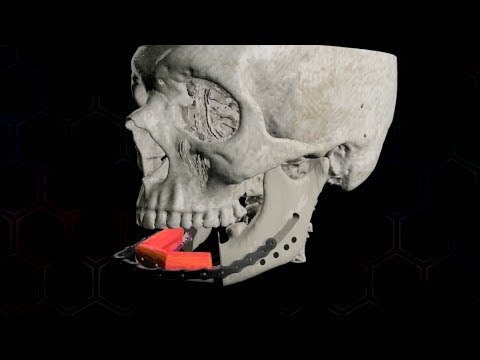 (2015) 43:28–33. doi: 10.1016/j.jcms.2014.10.005
(2015) 43:28–33. doi: 10.1016/j.jcms.2014.10.005
PubMed Abstract | CrossRef Full Text | Google Scholar
25. Mascha F, Winter K, Pietzka S, Heufelder M, Schramm A, Wilde F. Accuracy of computer-assisted mandibular reconstructions using patient-specific implants in combination with CAD/CAM fabricated transfer keys. J Craniomaxillofac Surg. (2017) 45:1884–97. doi: 10.1016/j.jcms.2017.08.028
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Van Baar GJC, Forouzanfar T, Liberton N, Winters HAH, Leusink FKJ. Accuracy of computer-assisted surgery in mandibular reconstruction: a systematic review. Oral Oncol. (2018) 84:52–60. doi: 10.1016/j.oraloncology.2018.07.004
PubMed Abstract | CrossRef Full Text | Google Scholar
27. Ong HS, Liu JN, Ahmed A, Qu XZ, Wan K, Xie DP, et al. Improved accuracy of hemimandibular reconstructions involving the condyle by utilizing hydroformed reconstruction plates rather than hand-bent stock plates. Head Neck.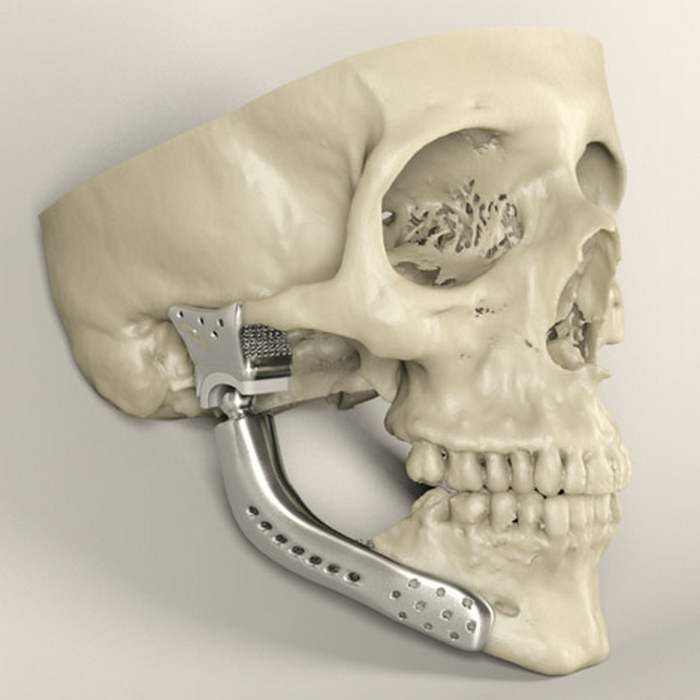 (2019) 41:3168–76. doi: 10.1002/hed.25809
(2019) 41:3168–76. doi: 10.1002/hed.25809
PubMed Abstract | CrossRef Full Text | Google Scholar
28. Wu TF, Liu JY, Li YS, Liu B. Matching locating holes in multiple plates to record bone position for accurate reconstruction after segmental mandibulectomy. Int J Oral Maxillofac Surg. (2019) 48:1516–9. doi: 10.1016/j.ijom.2019.04.013
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Bartier S, Mazzaschi O, Benichou L, Sauvaget E. Computer-assisted versus traditional technique in fibular free-flap mandibular reconstruction: a CT symmetry study. Eur Ann Otorhinolaryngol Head Neck Dis. (2020) 138:23–27. doi: 10.1016/j.anorl.2020.06.011
PubMed Abstract | CrossRef Full Text | Google Scholar
30. Pucci R, Weyh A, Smotherman C, Valentini V, Bunnell A, Fernandes R. Accuracy of virtual planned surgery versus conventional free-hand surgery for reconstruction of the mandible with osteocutaneous free flaps. Int J Oral Maxillofac Surg. (2020) 49:1153–61. doi: 10.1016/j.ijom.2020.02.018
(2020) 49:1153–61. doi: 10.1016/j.ijom.2020.02.018
PubMed Abstract | CrossRef Full Text | Google Scholar
31. Sweed AH, Bolzoni AR, Kadubiec A, Beltramini GA, Cherchi A, Baj A. Factors influencing CAD/CAM accuracy in fibula free flap mandibular reconstruction. Acta Otorhinolaryngol Ital. (2020) 40:138–43. doi: 10.14639/0392-100X-N0400
PubMed Abstract | CrossRef Full Text | Google Scholar
32. Hashemi S, Oda M, Onoue K, Basa K, Rubin SJ, Sakai O, et al. Determining the optimal osteotomy distance with the fibula free flap in mandibular reconstruction. Am J Otolaryngol. (2020) 41:102436. doi: 10.1016/j.amjoto.2020.102436
PubMed Abstract | CrossRef Full Text | Google Scholar
33. Trignano E, Fallico N, Faenza M, Rubino C, Chen HC. Free fibular flap with periosteal excess for mandibular reconstruction. Microsurgery. (2013) 33:527–533. doi: 10.1002/micr.22159
PubMed Abstract | CrossRef Full Text | Google Scholar
34. Akashi M, Hashikawa K, Kakei Y, Sakakibara A, Hasegawa T, Minamikawa T, et al. Sequential evaluation for bone union of transferred fibula flaps in reconstructed mandibles: panoramic X-ray versus computed tomography. Int J Oral Maxillofac Surg. (2015) 44:942–7. doi: 10.1016/j.ijom.2015.04.014
Sequential evaluation for bone union of transferred fibula flaps in reconstructed mandibles: panoramic X-ray versus computed tomography. Int J Oral Maxillofac Surg. (2015) 44:942–7. doi: 10.1016/j.ijom.2015.04.014
PubMed Abstract | CrossRef Full Text | Google Scholar
35. Vannabouathong C, Sprague S, Bhandari M. Guidelines for fracture healing assessments in clinical trials. Part I: definitions and endpoint committees. Injury. (2011) 42:314–16. doi: 10.1016/j.injury.2010.11.048
PubMed Abstract | CrossRef Full Text | Google Scholar
36. Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. (1989) 84:71–9. doi: 10.1097/00006534-198907000-00014
PubMed Abstract | CrossRef Full Text | Google Scholar
37. Hidalgo DA. Titanium miniplate fixation in free flap mandible reconstruction. Ann Plast Surg. (1989) 23:498–507. doi: 10.1097/00000637-198912000-00005
PubMed Abstract | CrossRef Full Text | Google Scholar
38. Kennady MC, Tucker MR, Lester GE, Buckley MJ. Stress shielding effect of rigid internal fixation plates on mandibular bone grafts. A photon absorption densitometry and quantitative computerized tomographic evaluation. Int J Oral Maxillofac Surg. (1989) 18:307–10. doi: 10.1016/S0901-5027(89)80101-8
Kennady MC, Tucker MR, Lester GE, Buckley MJ. Stress shielding effect of rigid internal fixation plates on mandibular bone grafts. A photon absorption densitometry and quantitative computerized tomographic evaluation. Int J Oral Maxillofac Surg. (1989) 18:307–10. doi: 10.1016/S0901-5027(89)80101-8
PubMed Abstract | CrossRef Full Text | Google Scholar
39. Strackee SD, Kroon FH, Bos KE. Fixation methods in mandibular reconstruction using fibula grafts: a comparative study into the relative strength of three different types of osteosynthesis. Head Neck. (2001) 23:1–7. doi: 10.1002/1097-0347(200101)23:1<1::AID-HED1>3.0.CO;2-2
PubMed Abstract | CrossRef Full Text | Google Scholar
40. Zhu WY, Su YX, Pow EHN, Yang WF, Qin L, Choi WS. “Three-in-one” patient-specific surgical guides for simultaneous dental implants in fibula flap jaw reconstruction: a prospective case series. Clin Implant Dent Relat Res. (2021) 23:43–53. doi: 10.1111/cid.12954
PubMed Abstract | CrossRef Full Text | Google Scholar
41. Toto JM, Chang EI, Agag R, Devarajan K, Patel SA, Topham NS. Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck. (2015) 37:1660–64. doi: 10.1002/hed.23815
Toto JM, Chang EI, Agag R, Devarajan K, Patel SA, Topham NS. Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck. (2015) 37:1660–64. doi: 10.1002/hed.23815
PubMed Abstract | CrossRef Full Text | Google Scholar
STL file mandible・3D printer design download・Cults
Best 3D Printer Files in the Miscellaneous Category
SpaceX Dragon 2 Crew Capsule
3.71 €
Double helix challenge
Free
Headphone Holder
Free
Spray can holder for 2" / 52mm cans
Free
Customizable Tri Glide
Free
NFL NBA 3D MODULAR LOGO / LETTERING
50 €
CelticMandolinIncenseHolder
Free
Deactivated
Bestsellers in Miscellaneous category
Christmas stitch
1. 25 €
25 €
Ciberpunk 2077 Rebecca Guts Pistol
4 € -25% 3 €
ItsLitho "Pure" personalized lithophane Christmas ball
1,90 €
Charizard - pokemon with flexible articulation (seal in place, without supports)
3 €
WORLD CHAMPIONSHIP OF SPACE
5.39 €
Christmas Park
4.61 €
Christmas house
6.91 €
T-800 Terminator Moving Skull
15€ -25% 11. 25 €
25 €
Targaryen Crown - Viserys - Dragon House
€11.67 -twenty% 9.34 €
RS-X-Bow "Government - 1911" style
6,25 €
Adderini - 3D printed repeating slingbow / crossbow pistol
6.25 €
4th planet Fighting pre-Olympic god
12 €
Giarados - articulated sea serpent
1,50 €
Key holder for middle finger
1 €
MATI
4.83 €
Ghost Boom x10
1.99 €
Do you want to support Cults?
Do you like Cults and want to help us continue our journey on our own ? Please note that we are a small team of 3 people, so supporting us in maintaining activities and creating future developments is very easy. Here are 4 solutions available to everyone:
Here are 4 solutions available to everyone:
-
AD: Disable your AdBlock banner blocker and click on our banner ads.
-
AFFILIATION: Shop online with our affiliate links here Amazon.
-
DONATIONS: If you want, you can donate via PayPal here.
-
* INVITE FRIENDS: * Invite your friends, discover the platform and great 3D files shared by the community!
Top Jaw・Cults
3D PrintersSnapmaker 2.0 swivel jaw extension
1.95 €
3D printed grill model
25 €
Vice jaw // STL file
€1.10 -25% 0.83€
Human jaw with teeth (scale 1:1)
Free
Spinosaurus skull
38. 08 €
08 €
Mask ideal for Halloween, Day of the Dead events
6,50 €
Krampus mask with movable jaw
7.32 €
Temporary parts of caries imprinted on resin 1.1 2.1
5 €
Candy dispenser with skulls
5.08 €
Deadbird
€10.89
Halloween faces
Free
Thermoformable skull mask.
€0.90
4-jaw chuck
3 €
Magnetic vice
1 €
Benchy's epic story
Free
Phone stand "Fangs"
Free
TUNE GUARD HOLDER - PRINT IN SITE
Free
Complete skeleton of a Brachiosaurus / Giraffatitan
31. 25 €
25 €
Brachiosaurus / giraffatitan skull
6.25 €
TPU soft vice 75 mm
1 €
Articulated skull mask
4.88 €
Animal lower jaw
Free
zirconia crowns parts 2.1 and 2.3
30 €
cat jaw mask
0,80 €
Soft jaws gearbox V2
12.20 €
human jaw teeth
5,50 €
Upper jaw
3 €
Serpent head
6.47 €
Complete skeleton of the dinosaur Dilophosaurus
31. 25 €
25 €
part 11
5 €
Star Wars Hasbro 2010 ATAT Interchangeable Jaw Pistols
4.87 €
TRANSPARENT ALIGNERS Pac A. 21 dental model or setting UPPER AND LOWER MAXILLARY "READY FOR 3D PRINTER" - AREA3D- PATIENT A. FULL DENTURE
€59.84
LATERAL JAILS - UPPER AND LOWER "3D ready" - AREA3D - Patient A. FULL DENTURE
5.98 €
Yondu skull - movable jaw
1.25 €
ANATOMICAL CROWN 16
5 €
BOTH MAXILLARS - SUPERIOR and INFERIOR intraoral scan (IOS) - AREA3D - Patient A. full bite
5.83 €
SUPERIOR MAXILLARY according to intraoral scanning - AREA3D - patient A.