3D printed human body parts
3D Printers Can Already Create Human Body Parts
Do you feel like you are living in a sci-fi version of the future? Because you probably should.
A close up view of the skin bioprinter nozzle.WFIRM
In recent years, updates in 3D printing technologies have allowed medical researchers to print things that were not possible to make using the previous version of this technology, including food, medicine, and even body parts.
In 2018, doctors from the Ontario Veterinary College 3D printed a custom titanium plate for a dog that had lost part of its skull after cancer surgery.
Source: University of Guelph“By performing these procedures in our animal patients, we can provide valuable information that can be used to show the value and safety of these implants for humans”, said veterinary surgical oncologist Michelle Oblak at the time. “These implants are the next big leap in personalized medicine that allows for every element of an individual’s medical care to be specifically tailored to their particular needs. ”
And not just for animal patients.
What is 3D bioprinting?
3D bioprinting is the utilization of 3D printing technologies to fabricate body parts. Bioprinters work in a similar way to 3D printers. However, instead of depositing materials such as plastic or ceramic, they deposit layers of biomaterial, including living cells, to build complex structures like blood vessels or skin tissue.
The required cells are taken from a patient and then cultivated. These cells are usually combined with a carrier material or scaffold. This carrier is usually a type of biopolymer gel, which acts as a 3D molecular scaffold and provides protection for the cells during the printing process. Cells attach to the gel, which is sturdy enough to allow printing and flexible enough to allow the flow and diffusion of nutrients and the movement of cells. This combination of encapsulated cells and biopolymer gels is the bio-ink used by biomedical engineers to create 3D-printed, tissue-like structures.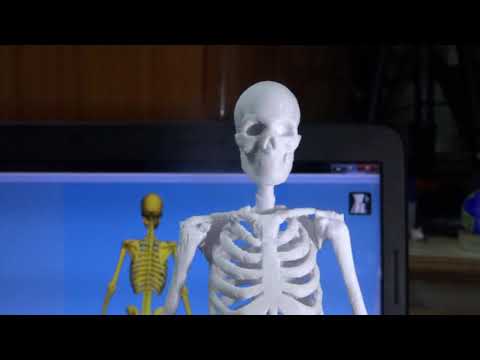
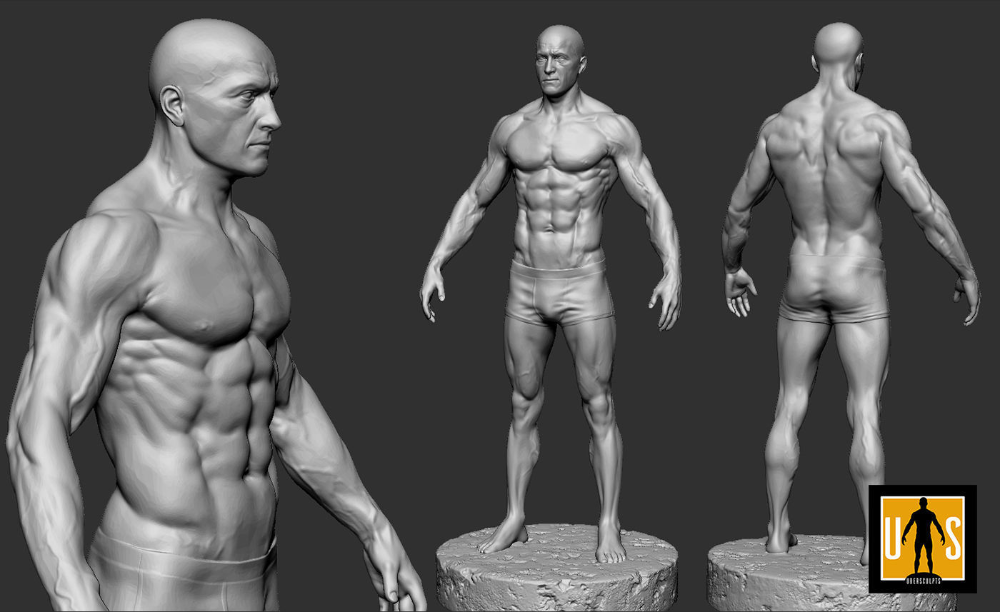
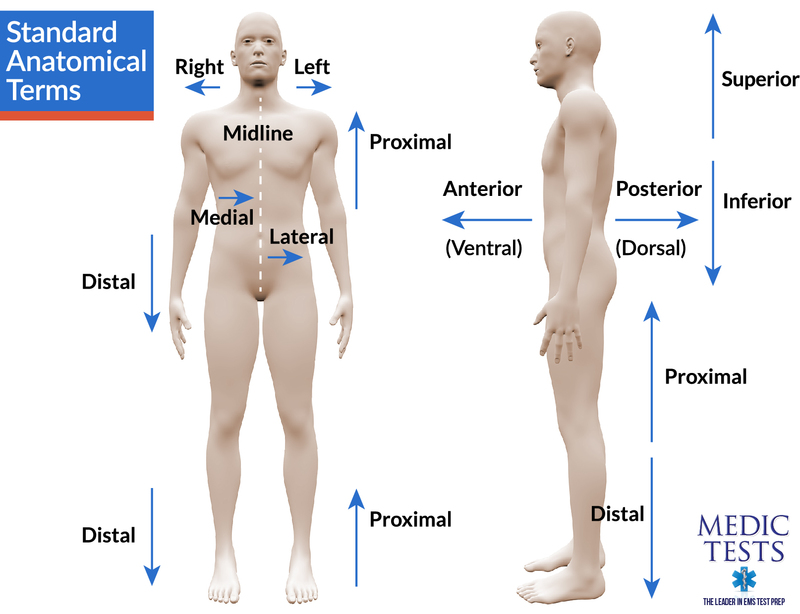
Detailed computer designs and models are first made, often based on scans such as magnetic resonance imaging or computerized tomography taken directly from a patient. Precision printer heads then deposit cells and bio-inks exactly where they are needed and, over the course of several hours, an organic object is built up using a large number of very thin layers.
A research fellow, Dr. Young Joon Seol, works on a project to print experimental muscle tissue for reconstructive surgery. Source: Army Medicine/FlickrThe cells are kept alive using liquefied nutrients and oxygen during the whole process.
In the post-printing stage, the structures may be crosslinked with UV light or ionic solutions to make them more stable. Cells are chemically and mechanically stimulated to control the remodeling and growth of tissues. Then, the 3D printed product is put into an incubator to allow the cells to grow.
When it’s ready, the structure must be used as soon as possible, unless the 3D bioprinting is combined with cryopreservative techniques — something that researchers from Brigham and Women's Hospital and Harvard Medical School achieved last year.
Most Popular
The work, published on December 21st, showed how the team was able to 3D print tissues onto a cold plate at -4°F (-20ºC), after which they were preserved in a freezer at -320.8°F (-196ºC). The tissues, researchers said, can then be thawed within minutes for immediate use.
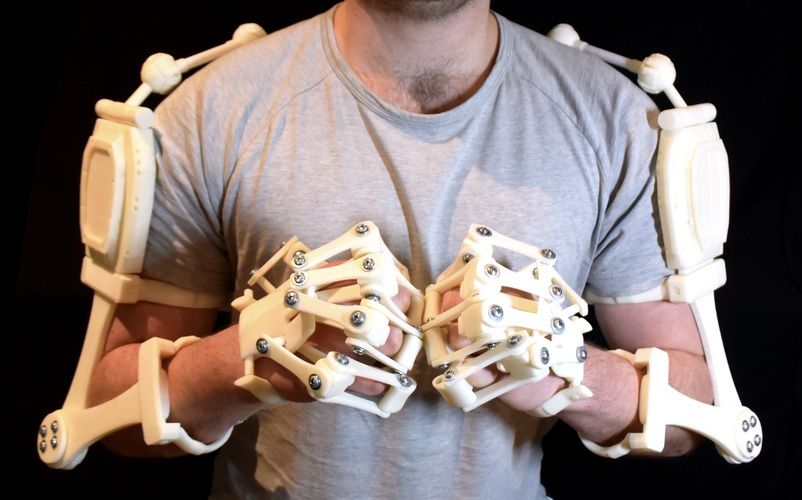
Tendons and ligaments
In 2018, biomedical engineers from the University of Utah developed a method for 3D printing ligaments and tendons. The method involves first taking stem cells from the patient and printing them on a layer of hydrogel to form a tendon or ligament. This is allowed to grow in vitro in a culture before being implanted. However, the process was very complex, because connective tissue is made up of different cells in complex patterns. The team first needed to develop a special printer head that could lay down human cells in the highly controlled manner they require.
To do this, the team partnered with Utah-based company Carterra, Inc., to develop a specialized printhead that would let them lay down cells in complex patterns.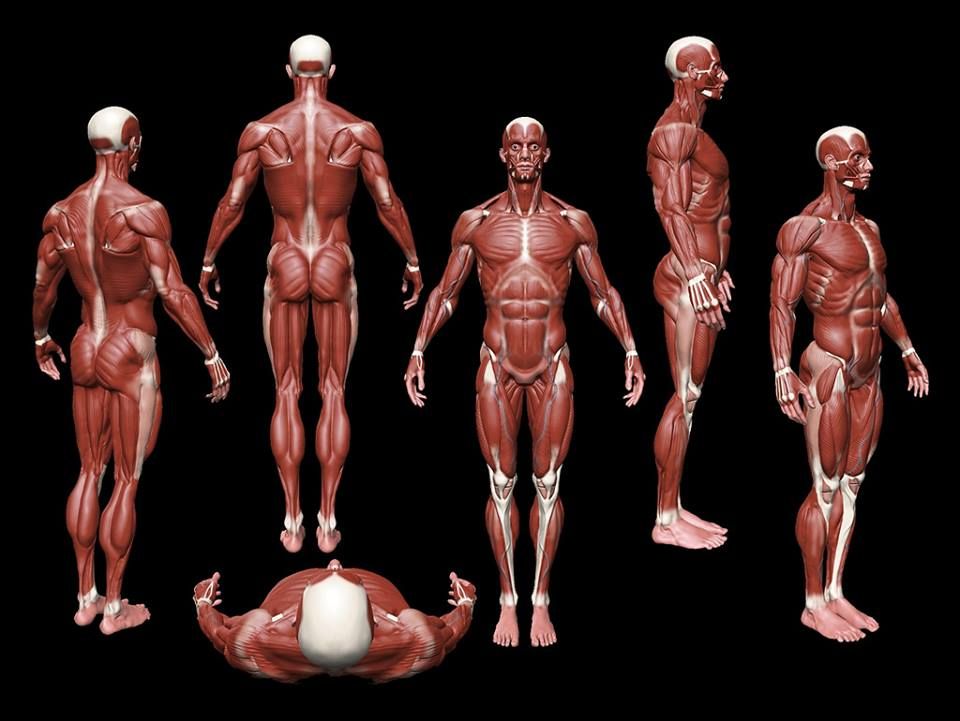 The printhead was then attached to a 3D printer normally used to print antibodies for cancer treatment.
The printhead was then attached to a 3D printer normally used to print antibodies for cancer treatment.
With this technique, the scientists managed to 3D print stem cells taken from a patient’s body fat onto a layer of hydrogel. This hydrogel facilitates cell growth in vitro in a culture, forming either a ligament or tendon in the process.
The new tissue is then implanted in the damaged area of the patient’s body, eliminating the need for additional tissue replacement procedures.
Replacement tissues for those needing it are often harvested from elsewhere on a patient's body or from a cadaver. However, tissue from cadavers runs a high risk of being rejected by the surrounding tissues or of being of poor quality and ineffective.
Instead, tissues created from the patient’s own cells can reduce the complications involved with a transplant and speed up the healing process.
Skin bioprinting and wound healing
3D bioprinting could also help us say goodbye to skin grafts in the near future, as doctors could be able to 3D print new skin for each patient.
Skin grafting is the transplantation of healthy skin from an animal, a human donor, or the patient’s own body to another part of his or her body where the skin is badly damaged. The procedure is commonly used to treat severe wounds, burns, ulcers, and infections, or after the removal of skin cancers.
Source: Scientific Animations/Wikimedia CommonsBut the technique involves several risks, from hemorrhages and loss of sensitivity to infections, scarring, and rejection.
This is why scientists from Wake Forest Institute for Regenerative Medicine (WFIRM) are working on a mobile bedside skin bioprinting system that could let doctors print bi-layered skin directly on the patient’s wound.
“The unique aspect of this technology is the mobility of the system and the ability to provide on-site management of extensive wounds by scanning and measuring them in order to deposit the cells directly where they are needed to create skin,” said Sean Murphy, Ph. D., a WFIRM assistant professor who was the lead author of the paper.
D., a WFIRM assistant professor who was the lead author of the paper.
To do this, the scientists isolated certain skin cells from a biopsy of healthy tissue and grew them in culture. After that, they combined the cells with a hydrogel and put them into the bioprinter. The device printed the cells onto the damaged area following the data extracted from the wound’s scan through a software.
Again, because the cells are taken from the patient’s own body, there is a much lower risk of rejection.
Meanwhile, in Dublin, scientists from the RCSI University of Medicine and Health Sciences developed a hydrogel scaffold with natural platelet-rich plasma (PRP) that has promising regenerative properties. The compound can be used as a bio-ink to accelerate the wound healing process in 3D printed tissues.
“Existing literature suggests that while the PRP already present in our blood helps to heal wounds, scarring can still occur,” said RCSI Professor Fergal O’Brien. “By 3D printing PRP into a biomaterial scaffold, we can increase the formation of blood vessels while also avoiding the formation of scars, leading to more successful wound healing.”
“By 3D printing PRP into a biomaterial scaffold, we can increase the formation of blood vessels while also avoiding the formation of scars, leading to more successful wound healing.”
Blood vessels
Perhaps the ultimate goal of 3D bioprinting is to assemble functional organs and solve the problem of organ transplantation.
Currently, there are more than 100,000 people waiting for an organ on the U.S. national transplant waiting list. Roughly 17 of them die each day because they don’t receive the organ they need. This is largely due to the lack of donors. Although around 60% of Americans are signed up as donors, organ donation is only possible in 3 out of every 1,000 deaths.
3D bioprinting of organs could save a lot of lives, but scientists struggle to create the vascular structures needed to create viable printed organs. All organs, including 3D-printed ones, need an effective, continuous blood supply to prevent the death of the cells and the tissues.
In October 2021, a team of researchers at Israel's Technion Institute of Technology managed to 3D print blood vessel structures to add a blood supply to tissue implants.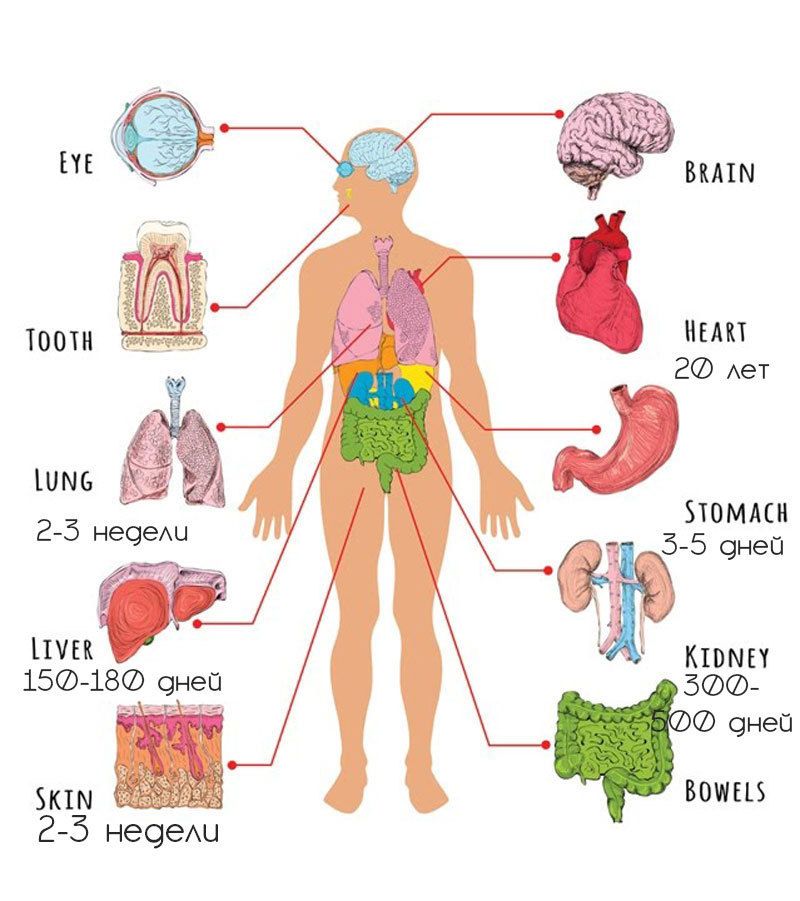
These structures grew spontaneously after the team implanted endothelial cells from the inner layer of blood vessels in the body in a polymeric collagen scaffold.
However, these are only microvessels that can be used to improve in vitro tissue development — they wouldn’t be able to, “feed” a whole organ, and so far, they don’t allow the integration of lab-grown tissues into the patient’s vascular system.
This study shows that there’s still a long way to go until we can actually 3D print organs on demand. But who knows which techniques can scientists develop to solve this issue in the future?
For You
science
The company, Takachar, turns 'waste' biomass into profitable items. In doing so, it aims to broaden smallholder farmers' livelihood.
Sade Agard | 10/4/2022
scienceThe Moon keeps drifting away from Earth. Will it ever leave?
Will it ever leave?
Paul Ratner| 10/29/2022
innovationSCOPE: This quantum dot spectrometer can hasten Uranus and Neptune orbital missions
Deena Theresa| 9/27/2022
More Stories
innovation
A company's nuclear fusion rockets could help us escape the Solar System in our lifetime
Chris Young| 12/1/2022
science
In a first, researchers discovered a rare mineral that comes directly from Earth's lower mantle
Sade Agard| 11/28/2022
innovation
Space cement is here: How it could be used to build houses on Mars and the Moon
Deena Theresa| 9/16/2022
3D Printed Organs: The Top Viable Projects
Published on April 7, 2020 by Carlota V.
Bioprinting is a method that enables cellular structures to be made from bioinks loaded with stem cells. Layer by layer, the biomaterial is deposited to create skin, tissue or even an organ.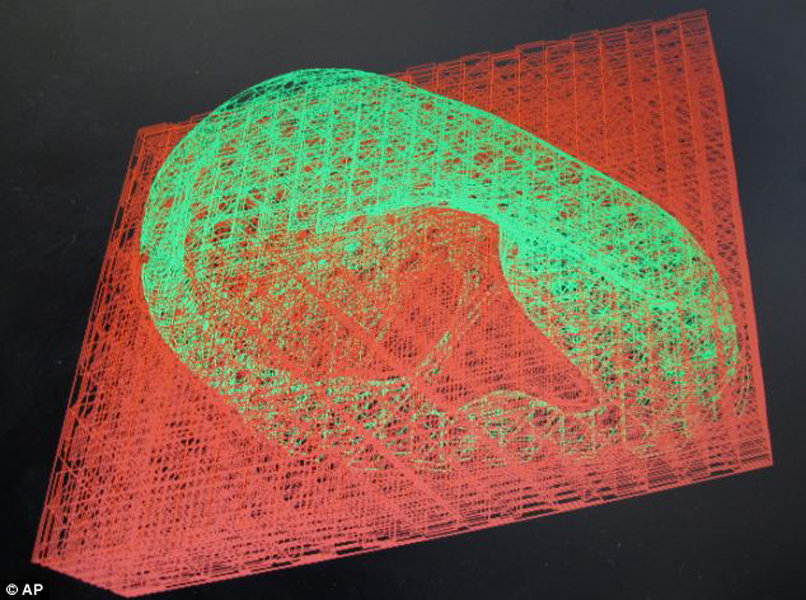 Bioprinting projects are growing, and each new project is one-step closer to being a fully functional and viable solution. Laboratories and research centers are bioprinting human livers, kidneys and hearts. The objective is to make them suitable for transplantation, and viable long-term solutions. In fact, this method could allow to cope with the lack of organ donors, and to better study and understand certain diseases. There is still progress to be made but we wanted to present the main bioprinting projects in the listing below, including 3D printed organs and other human body parts!
Bioprinting projects are growing, and each new project is one-step closer to being a fully functional and viable solution. Laboratories and research centers are bioprinting human livers, kidneys and hearts. The objective is to make them suitable for transplantation, and viable long-term solutions. In fact, this method could allow to cope with the lack of organ donors, and to better study and understand certain diseases. There is still progress to be made but we wanted to present the main bioprinting projects in the listing below, including 3D printed organs and other human body parts!
A Bioprinted Heart Made Out of Cells
Last April, a team of Israeli researchers presented a bioprinted heart the size of a cherry. This 3D printed organ consisted of cells, blood vessels, ventricles and chambers: a first for the industry. The researchers developed a hydrogel from the patient’s own fat tissue, reducing the risk of rejection once implanted. The printing process would have taken only 3 to 4 hours.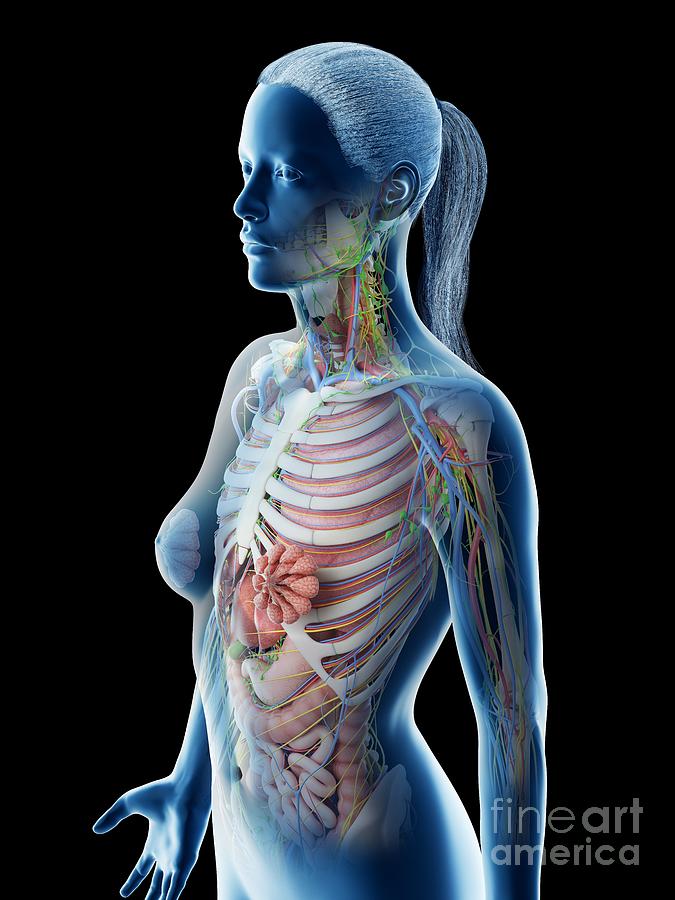 The heart is no bigger than a rabbit’s heart, but it’s an encouraging start. Note also the results obtained by BIOLIFE4D: the American company has succeeded in bioprinting a miniature human heart with ventricles and cavities.
The heart is no bigger than a rabbit’s heart, but it’s an encouraging start. Note also the results obtained by BIOLIFE4D: the American company has succeeded in bioprinting a miniature human heart with ventricles and cavities.
Bioprinting a Kidney, a 3D Printed Organ Made From Stem Cells
In 2011, Professor Anthony Atala, Director of the Wake Forest Institute for Regenerative Medicine, presented a 3D bioprinted kidney for the first time. Within seven hours, his team was able to design this 3D printed organ from stem cells. The kidney could not live for very long, but the project was full of promise. Since then, the printing work has continued. At Harvard, for example, researchers have succeeded in bioprinting a 3D model of a vascularized proximal tubule to better understand the structure and function of the kidney.
Bioprinted Corneas to Help Prevent Blindness
The World Health Organisation estimates that 10 million people worldwide require surgery to prevent corneal blindness, and 4.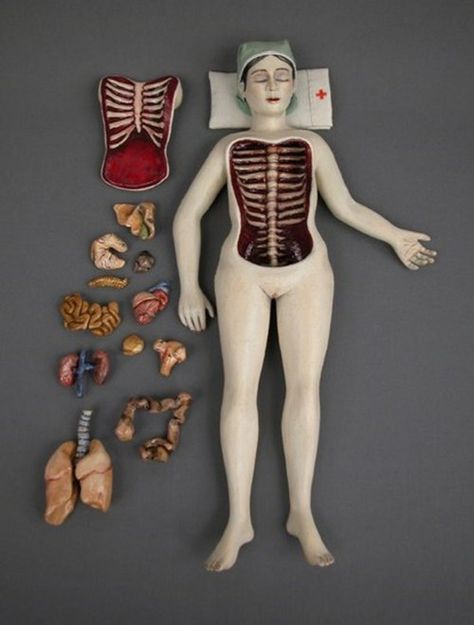 9 million already suffer from complete blindness due to corneal scarring. In 2019, researchers from the University of Newcastle developed a 3D printed artificial cornea for the first time that could be transplanted for people in need. After studying and gathering data from a volunteer’s eye, the researchers were able to design a 3D model of the cornea. One of the most challenging aspects was using the right materials to hold the concave shape of the cornea as well as finding an ink thin enough to squirt through a 3D bioprinter’s nozzle. Using only one healthy human cornea they were able to 3D print 50 artificial ones; a breakthrough advancement in ophthalmology.
9 million already suffer from complete blindness due to corneal scarring. In 2019, researchers from the University of Newcastle developed a 3D printed artificial cornea for the first time that could be transplanted for people in need. After studying and gathering data from a volunteer’s eye, the researchers were able to design a 3D model of the cornea. One of the most challenging aspects was using the right materials to hold the concave shape of the cornea as well as finding an ink thin enough to squirt through a 3D bioprinter’s nozzle. Using only one healthy human cornea they were able to 3D print 50 artificial ones; a breakthrough advancement in ophthalmology.
Bioprinted Ovaries Advanced 3D Printed Reproductive Organs
In May 2017, researchers from Northwestern University were developing a solution for women with fertility issues. Back then, they had succeeded in implanting a bioprinted ovary in a sterile mouse. Two years later, the researchers made some very promising progress. They were able to map the location of structural proteins in a pig ovary, allowing them to create a bioink to bioprint functional ovaries for human use. Additionally, the team explained that their methodology could be used to identify other types of proteins that could facilitate the creation of bioinks for other 3D printed organs!
They were able to map the location of structural proteins in a pig ovary, allowing them to create a bioink to bioprint functional ovaries for human use. Additionally, the team explained that their methodology could be used to identify other types of proteins that could facilitate the creation of bioinks for other 3D printed organs!
Bioprinting a Mini Liver in Only 90 Days
Researchers at the University of São Paulo in Brazil have succeeded in creating miniature versions of a human liver from blood cells. The process took only 90 days, from the collection of the patient’s blood to the production of the tissue. These liver organoids, developed using 3D bioprinting technologies, integrate the functionalities of the 3D printed organ in question. These include the production of vital proteins, the storage of vitamins and the secretion of bile. To create the liver tissue, the team used the Inkredible bioprinter, marketed by the manufacturer CELLINK, one of the most recognized in the industry.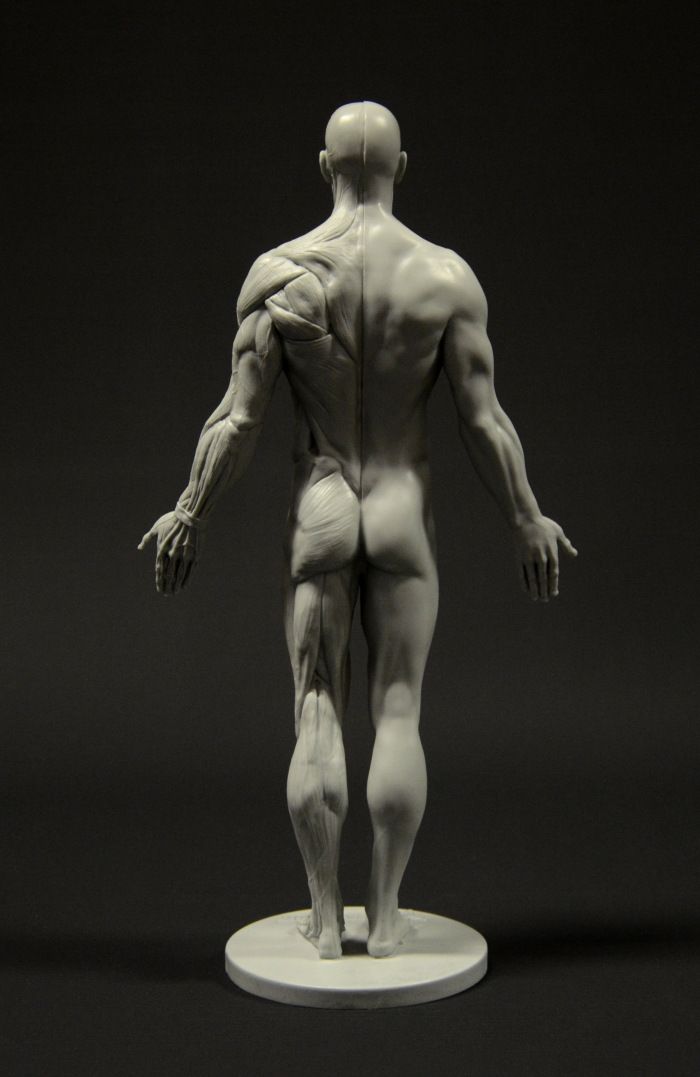
A Bioprinted Ear Project Helps a Young Girl Regain Hearing
This bioprinting project was made possible through a collaboration between Queensland University of Technology (QUT) and Maia Van Mulligan, to help her regain her hearing. The HearSay Foundation, also involved in the recovery of the little girl, states that the 3D printed ear is fully functional and will allow Maia to hear again. The ear implant was created using the patient’s cartilage cells, reducing the risk of rejection once implanted. In addition, this type of custom-made bioprinting solution is actually less-expensive than other alternatives.
Bioprinting a Pancreas: One of the Most Difficult 3D Printed Organs
A team of scientists from the “Foundation for Research and Development of Science” has set itself the goal of developing a functional 3D printed pancreas by 2020, which will help diabetic patients avoid having to inject insulin and minimize the risk of related secondary complications, which often lead to death.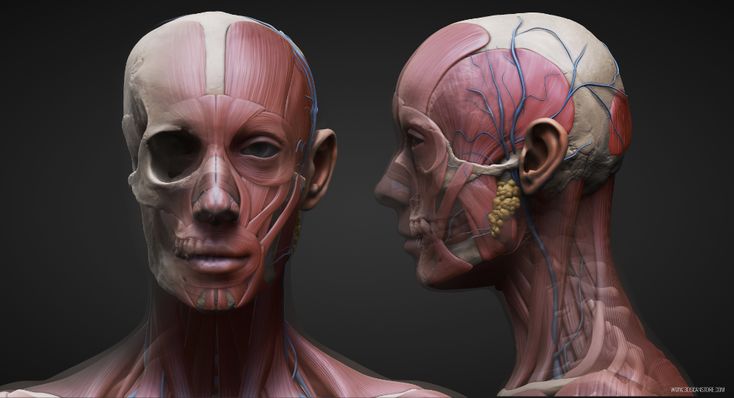 For the bioprinting, a biopsy of the patient, and stem cell harvest is first performed. The cells are then converted into cells capable of producing insulin and glucagon. These are then used as bioink to print the pancreas.
For the bioprinting, a biopsy of the patient, and stem cell harvest is first performed. The cells are then converted into cells capable of producing insulin and glucagon. These are then used as bioink to print the pancreas.
Bioprinted Skin, the Body’s Largest Organ
The market for bioprinted skin is growing steadily: according to BBC Research, the market will grow from 24.7 billion dollars in 2018 to 109.9 billion dollars in 2023. The startup company Poietis has developed 4D printed skin, which in the future could be transplanted for victims of burns or skin diseases. A software called Cytocentric CAD has been developed specifically for the printing process, which is designed to meet the challenge of imitating the body’s own tissue. This is 4D printing, as tissue components are precisely arranged in space and are also subject to the action of self-organization processes of the cells. By taking self-organizing processes into account, it is possible to create highly complex tissue structures that are very close to those of the human body.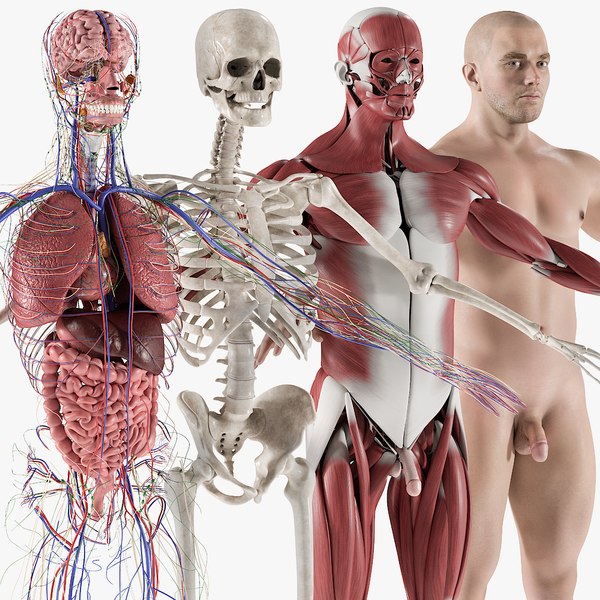 The 4D printed skin is clinically tested in a collaboration with the Assistance Publique – Hôpitaux de Marseille. Poietis’ long-term goal is “to place a bio-printer in every hospital to enable the production of personalized tissues and improve the waiting time of patients waiting for transplants,” says Dr. Fabien Guillemot, founder of Poietis.
The 4D printed skin is clinically tested in a collaboration with the Assistance Publique – Hôpitaux de Marseille. Poietis’ long-term goal is “to place a bio-printer in every hospital to enable the production of personalized tissues and improve the waiting time of patients waiting for transplants,” says Dr. Fabien Guillemot, founder of Poietis.
What do you think of these bioprinting projects? Let us know in a comment below or on our Facebook and Twitter pages! Find even more videos like the one below on our Youtube channel!
Body parts that can already be printed on a 3D printer Including in medicine. Presumably, with the help of this equipment, the problem of donation will be finally resolved. After all, almost any part of the body or organ can simply be printed. And no matter how fantastic it may sound, scientists have already achieved amazing results in this direction.
Pinna
At least 1 in 12,500 newborns is born with microtia, a condition that can lead to hearing problems due to abnormal or missing pinna. In this case, surgical intervention is attempted, or a complete replacement of the shell may be required. Up to this point, artificial implants were used, which were often rejected by the body.
But using a 3D printer, it is already possible to create an auricle from living cells. The organ is first modeled in SolidWorks CAD software (and it is not difficult to create an exact copy of the other ear using 3D scanning), and then printed using a special high-density gel consisting of cells taken from bovine cartilage - they require about 25 million. Collagen (protein, providing strength and elasticity of the fabric) is “extracted” from rat tails. After the "printing" procedure, about 3 months of incubation period is required.
Being completely natural, this auricle is more readily accepted by the body.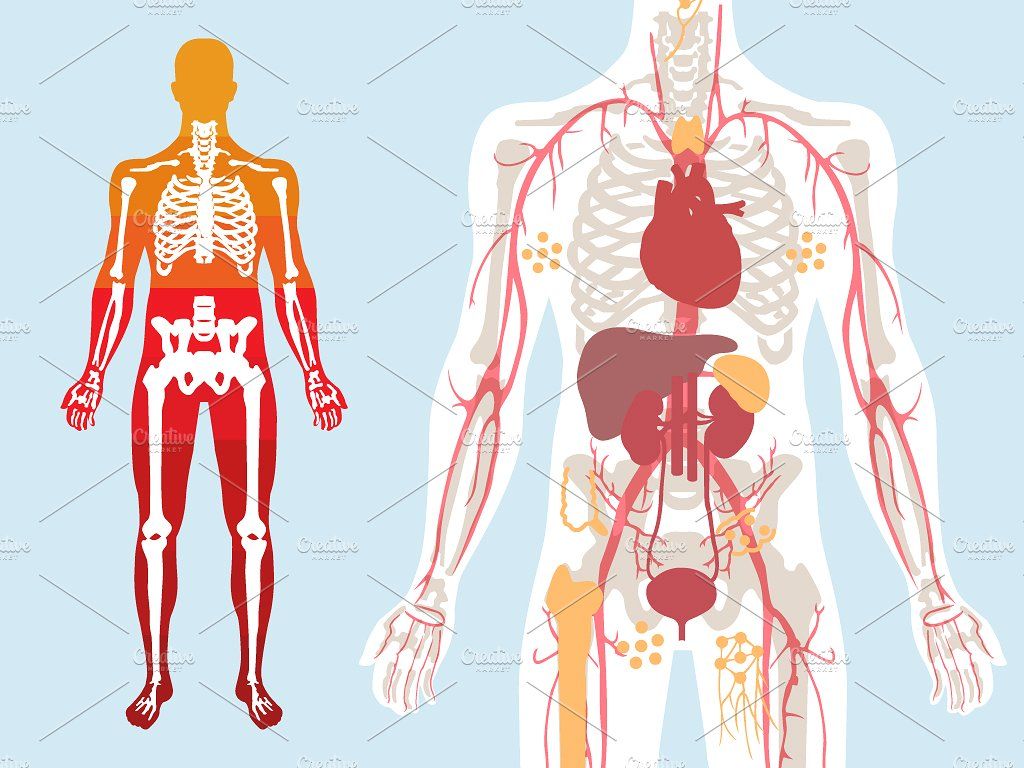 The chance of rejection is much lower. The technique was developed by scientists from Cornell University.
The chance of rejection is much lower. The technique was developed by scientists from Cornell University.
By the way, ears can be printed not only for the treatment of diseases or injuries. So, scientists from Princeton University are creating special ears that can pick up radio signals. It is assumed that such additions will be very useful for various electronics for the time being, and in the future they will be able to expand human capabilities.
Kidneys
As you know, with a sick heart or stomach, a person can live more or less normally for many years. Sick kidneys usually mean a significant reduction in life expectancy. However, it is sometimes extremely difficult or simply impossible to make a “replacement” due to the lack of a suitable donor. And the possibility of "conveyor" production of kidneys would save the lives of tens of thousands of people around the world.
Scientists from the Wake Forest Institute for Regenerative Medicine are currently working on 3D printing of kidneys. To create a new organ, cells are taken directly from the organs of the patient. That is, the chance that his body will more readily accept an implant that will not differ much from the replaced one increases significantly.
To create a new organ, cells are taken directly from the organs of the patient. That is, the chance that his body will more readily accept an implant that will not differ much from the replaced one increases significantly.
Unfortunately, this is only a project so far, but with very bright prospects. It is likely that in the very near future, scientists will learn how to create kidneys for "any requests."
Blood vessels
Teams of scientists from the University of Pennsylvania and the Massachusetts Institute of Technology are currently working on making printed blood vessels. For work, a printer developed by the RepRap project and software specially created for such purposes is used.
Future vessels are based on sugar, mold fungi and special polymers obtained from corn. Moreover, sugar is needed only for shaping, then it is washed out with water.
However, the obtained vessels cannot yet be used in the human body. But we are talking only about the development of the principles themselves. But the ability to create blood vessels that are indistinguishable from real ones is an important step towards creating any human organs using 3D printers.
But the ability to create blood vessels that are indistinguishable from real ones is an important step towards creating any human organs using 3D printers.
Leather
Scientists from the Wake Forest Institute of Regenerative Medicine, already mentioned above, are also developing a technique where the skin will not be transplanted from other parts of the victim's body or from a donor, but printed directly on the affected area.
"Print" is preceded by a preliminary scan and mapping of the patient's wound. When creating the skin, various proteins and enzymes will be used, such as fibrinogen, collagen, thrombin, etc., each of which is then involved in the process of creating cells.
The ultimate goal is to create a compact 3D printer that can be used in disaster areas or in war.
Bones
Every year, thousands of people suffer complex bone fractures that are very difficult to repair using traditional methods.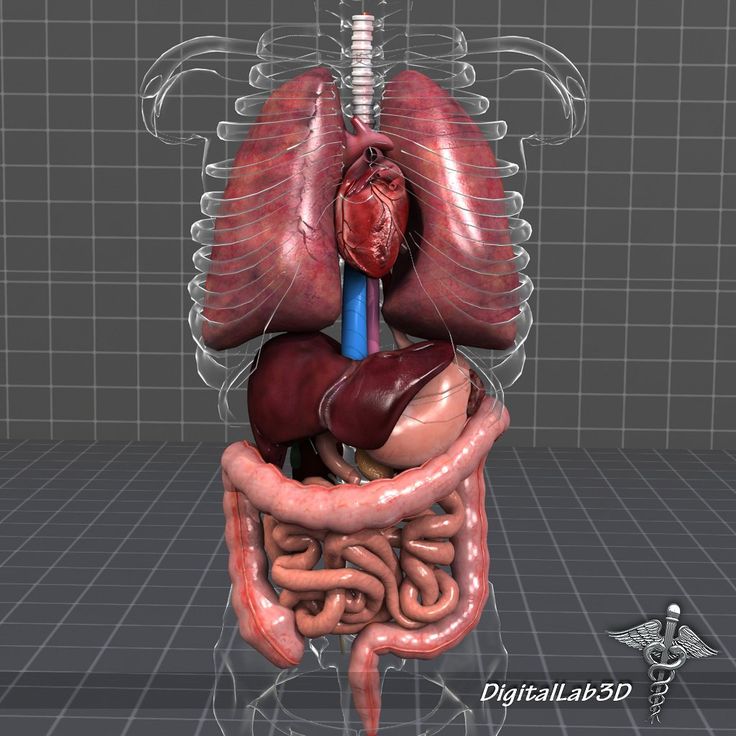 The technique, on which scientists from the University of Washington are currently working, is good because it will allow you to create replacements for any bones in the human body.
The technique, on which scientists from the University of Washington are currently working, is good because it will allow you to create replacements for any bones in the human body.
It was decided to use a special ceramic powder to create grafts. After printing is completed, the finished bone is subjected to heat treatment - heated to 2282 degrees for 120 minutes. The finished product is similar in its properties to human bone and can be used in the body.
In this case, the printing process is not too complicated. This technology is already actively used in the creation of some parts of electric motors. Thus, it is the printing of bones that looks like the most complete technology, the mass application of which is quite possible in the very near future.
By the way, this is not the first attempt to use 3D printers to print bone tissue. The same tireless researchers from the Wake Forest Institute for Regenerative Medicine are also working on the technology to create cartilage to treat various bone injuries.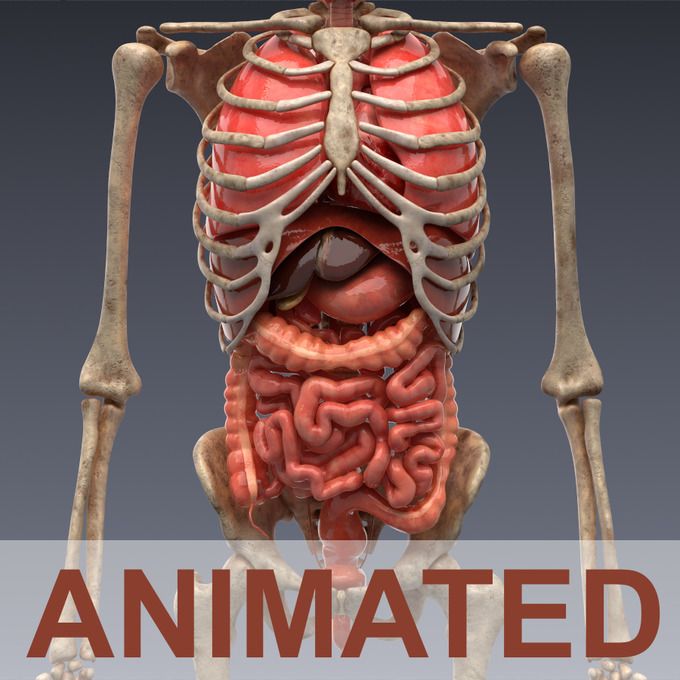
Total
All technologies described above are under laboratory testing and are not used by doctors in everyday practice. However, the very fact of their appearance gives hope for healing to millions of people. The ideas of a complete restoration of the body no longer look like something fantastic, this is a matter of the future, and it is quite possible that it will be in the near future.
Printing organs: how ears, skin and noses are made with a 3D printer
- Natalka Pisnya
- BBC Russian Service, USA
Sign up for our ”Context” newsletter: it will help you understand the events.
Photo copyright, Masela family archive
Photo caption,Luc Masela with his parents one month after the artificial bladder transplant. year 2001.
Luc Masela, now 27, is an athlete with a degree in economics, works for a large exhibition company, travels a lot and recently met, in his words, "the most beautiful girl in the world. " Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
" Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
Luke was born with spina bifida - and although he was able to walk, his bladder was severely damaged. By the age of 10, he almost did not leave hospitals: due to improper functioning of the bladder, fluid began to return to the boy's kidneys, doctors diagnosed an irreversible pathology of the organ.
You need JavaScript enabled or a different browser to view this content
Video caption,"3D printed" organs are here
Doctors offered the family two solutions: lifelong dialysis or the creation of a new bladder from a segment of the intestine. This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
The urologist in charge of the boy suggested that Masela's family take part in an experimental program to grow a new bladder from his own cells. Then, in 2001, it sounded like science fiction: only nine people took part in the program itself before Luke. Despite this, his family agreed.
Then, in 2001, it sounded like science fiction: only nine people took part in the program itself before Luke. Despite this, his family agreed.
"The essence of the operation was reduced to two stages: first, a piece of bladder tissue was taken from me, and over the next two months, cells were grown in the laboratory in order to grow a new healthy bladder from them," says Luke.
Photo copyright, Masela family archive
Photo caption,Luc Masela, 17 years after the artificial bladder transplant
Next was the transplant operation, which, according to him, lasted 16 hours. “I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
The operation was performed by Dr. Anthony Atala, Pediatric Regenerative Surgeon.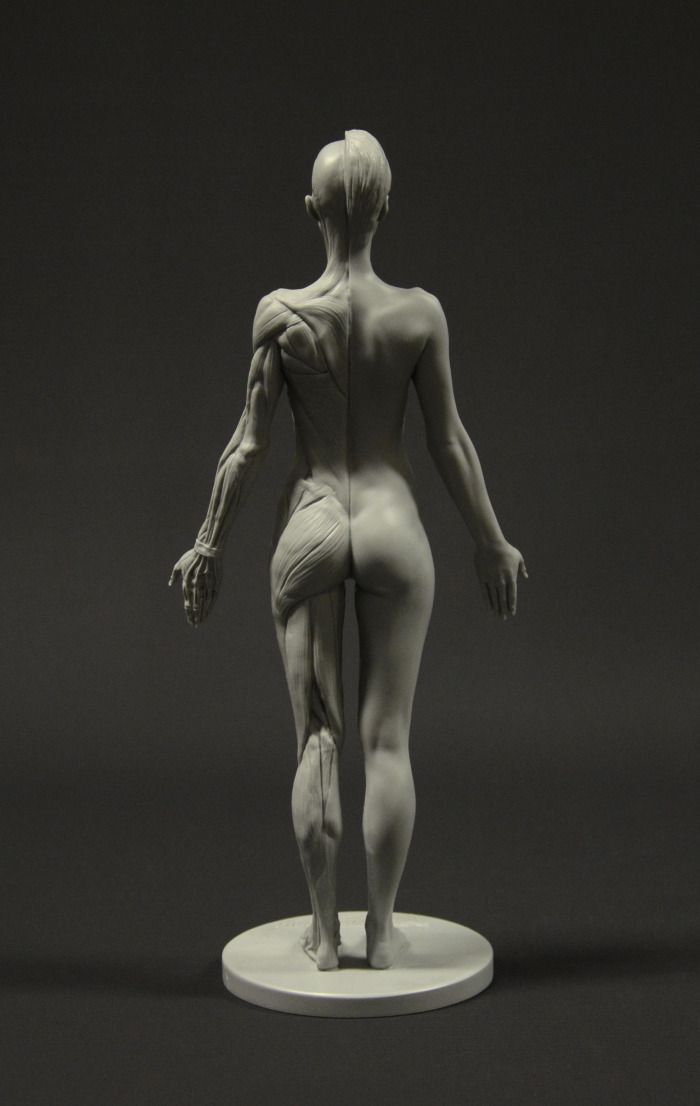 In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like an ordinary organ, taking root thanks to Luke’s own cells.
In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like an ordinary organ, taking root thanks to Luke’s own cells.
- An animal capable of regrowing its head
- The birth of a chimera: why do scientists need a human-animal hybrid?
- Swedish company 3D prints body parts
Luke and Dr. Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.
The professor took charge of the Wake Forest Institute of Regenerative Medicine in North Carolina in those 10 years, but he never forgot about Luke: his bladder was one of the most challenging and most successful projects in his early practice.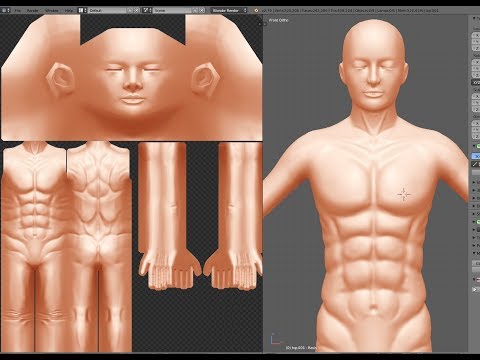
By 2018, Atala won the Christopher Columbus Award for "work on a discovery that will have a significant impact on society"; The Times and Scientific American magazines at various times named him "Physician of the Year", he was also recognized as "one of the 50 scientists on the planet who in the next 10 years will change the way we live and work."
How to print a new face
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it is important and what will happen next.
episodes
The End of the Story Podcast
In the mid-2000s, Atala's team turned their attention to an ordinary household 3D printer and wrote special software for it, later specialized machines were created for the laboratory.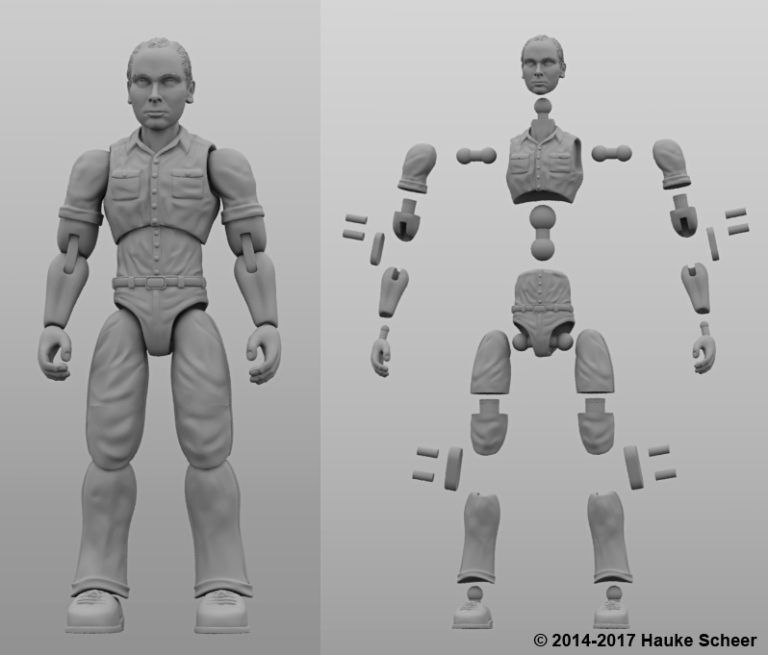 Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
One of the team's latest achievements is ears and noses grown outside the human body.
The main customer and sponsor of Atala's developments is the US Department of Defense, and many of the patients are military victims of military operations.
It works like this: first, a CT scan of the ear or nose is done. One of Atala's assistants, Joshua Corpus, jokes that at this stage, people often ask to "improve" the shape of the nose if they thought theirs was too wide or hooked, and the ears if they were too wide.
After that, a special computer code is written, and the printing of the basis of the organs begins.
For this, a bioabsorbable polymer, polycaprolactam, is used. Both flexible and strong at the same time, it disintegrates in the human body within four years.
After printing, the layers of polycaprolactam resemble lace, their place after transplantation in a few years will be taken by the person's own cartilage tissues.
Polycaprolactam is then saturated with a gel created from the patient's cells, cooled to -18 degrees Celsius - so the cells, according to scientists, are not damaged, they are "alive and happy."
Image caption,Printing a test kidney sample on a bioprinter
In order for the polymer and gel structure to take shape and become something more durable, ultraviolet light is used in the laboratory - it does not damage cells.
The future implant is printed for 4-5 hours, then it is finally formed and inserted under the epidermis.
Skin can also be grown: children affected by fires were the first to take part in the early trials of Atala - after the "printing" of the skin, scientists observed the patients for several more years. The new skin did not crack, did not burst, and grew with the children.
The most difficult work, according to the scientist, is facial wounds: it is not enough just to stretch the skin, you need to accurately calculate the geometry, align swelling, bone structure, and understand how a person will look after that.
In addition to the skin and ears, Atala can "print" the bones of the jaws, grow blood vessels and cells of some organs - the liver, kidneys, lungs.
This technology is especially appreciated by oncologists: on the basis of patient cells, it is possible to recreate the body's response to various types of chemotherapy and observe the reaction to a particular type of treatment in the laboratory, and not on a living person.
But the liver, kidneys, lungs and heart are still being tested. Atala says he raised them in miniature, but creating organs from various tissues to real size requires a lot of additional research.
But, according to him, cells were grown in the laboratory and a vagina was created for a girl who was born several years ago with a congenital deformity of the genital organs - several years have passed since the transplant.
Image caption,Bioprinted polycaprolactam ear implant base
Atala smiles and adds that his team is also working on a working penis. This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
Among others, Igor Vasyutin, a Russian post-graduate student of the First Moscow State Medical University (MSMU) named after Sechenov, is working on this under laboratory conditions. He is a cell biologist, Atala's right hand.
Vasyutin has been in the USA for about a year - he came on an exchange. He is ready to talk about the behavior of stem cells for hours, but becomes less verbose when it comes to Russian science.
Vasyutin's alma mater has not reached mass regeneration of human organs and is still training on animals: local scientists "printed" a mouse thyroid gland on a 3D printer.
Research on human organs, however, is also being done there. According to the head of the Institute of Regenerative Medicine at MSMU Denis Butnar, several years ago the Institute recreated a special engineering design of the buccal mucosa. She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
A test sample of an ear implant exposed to ultraviolet light
In Russia, however, over the past few years, the Italian surgeon-transplantologist Paolo Macchiarini has been practicing, the man who was the first in history to perform an operation on transplanting a synthetic organ - a plastic tube that replaced the patient trachea.
- Paolo Macchiarini: the rise and fall of the famous surgeon
However, seven of his nine patients died, and the breathing tubes implanted in the remaining two subsequently had to be replaced with donor ones.
Several criminal cases were brought against him, including on charges of pressure on patients and fraud, and the world's leading doctors called Macchiarini's operations "ethical Chernobyl."
Will printed organs replace donors?
At the zenith of his career, Macchiarini argued that a new perspective is opening up for humanity: you can "print" any human organ on a printer, create an engineering structure from it, enriched with the patient's stem cells, and get the perfect prosthesis.
Be that as it may, complex human organs - the liver, kidneys, heart, lungs - have not yet been able to grow any regenerative surgeon.
Bioprinting of the so-called simple organs, however, is already available in the US, Sweden, Spain and Israel - at the level of clinical trials and special programs.
The US government is actively investing in such programs - in addition to Wake Forest, cooperating with the Pentagon, the Massachusetts Institute of Technology also receives significant amounts to recreate the work of the liver, heart and lungs.
Image caption,Skin application test on a burnt wound
According to Professor Jorge Raquela, a gastroenterologist at the Mayo Clinic Research Center, "Bioprinting is one of the most exciting branches of modern medicine, it has huge potential, and the turning point of the most important discoveries is already close."
Meanwhile, Pete Basillier, head of R&D at analytics firm Gartner, insists technology is advancing much faster than understanding the implications of 3D printing.
Such developments, according to Basilière, even if created with the best of intentions, give rise to a set of questions: what will happen when "improved" organs are created, the basis of which will not only be human cells - will they have "superpowers"? Will a regulatory body be created to monitor their production? Who will check the quality of these organs?
More than 150,000 Americans are on the waiting list for organ transplants each year, according to a report from the US National Library of Medicine. Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
- A 3D printer helped a cyclist who lost his jaw
- Genetically modified pigs - human organ donors?
- The world's first child who received both hands transplanted plays baseball
Most Americans are potential donors: upon obtaining a driver's license, they voluntarily answer the question of whether they agree to donate their organs in the event of a car accident or other dangerous incident .