3D print medicine
3D printing of drugs can revolutionise personalised medicine
February 4, 2021
By GlobalData Healthcare
3D printers can be installed in pharmacies, hospitals, clinics, and remote locations, enabling on-demand production of drugs. Credit: Adul10 / Shutterstock.As the pharmaceutical industry moves away from mass production towards a more personalised model, 3D printing of drugs have the potential to revolutionise the market. The main benefit of using 3D printing technology for personalised pharmaceuticals is the ability to produce small batches with carefully tailored dosages, shapes, sizes, and release characteristics. It also allows flavours to be incorporated into a pill without the need of a film coating, entirely masking the taste of chemical compounds. 3D printers can be installed in pharmacies, hospitals, clinics, and remote locations, enabling on-demand production of drugs, particularly those with poor stability or that have cold chain storage requirements. For pharmaceutical companies, 3D printing can significantly reduce costs, waste, and environmental burden as printers only deposit the exact amount of raw materials required.
Aprecia Pharmaceuticals’ Spritam (levetiracetam), an anti-epileptic drug, is the first and only 3D-printed pharmaceutical. It received the Food and Drug Administration (FDA) approval in 2015 and is made using Aprecia’s proprietary ZipDose technology. The orodispersible tablet achieves full disintegration within seconds when in contact with liquid. Additionally, very high doses are achievable (up to 1,000mg), which are not typically possible through conventional methods. ZipDose technology uses a drop-on-solid printing technique where droplets of a liquid binding agent are deposited by a print nozzle onto a free pharmaceutical powder bed, unifying the free-form powder where it lands. The bed is then lowered to allow for another layer of free-form powder to be added. Further droplets are introduced, adding height to the nascent pill, while the surrounding, unbound powder particles act as a support structure to prevent the collapse of the highly porous pill structure.
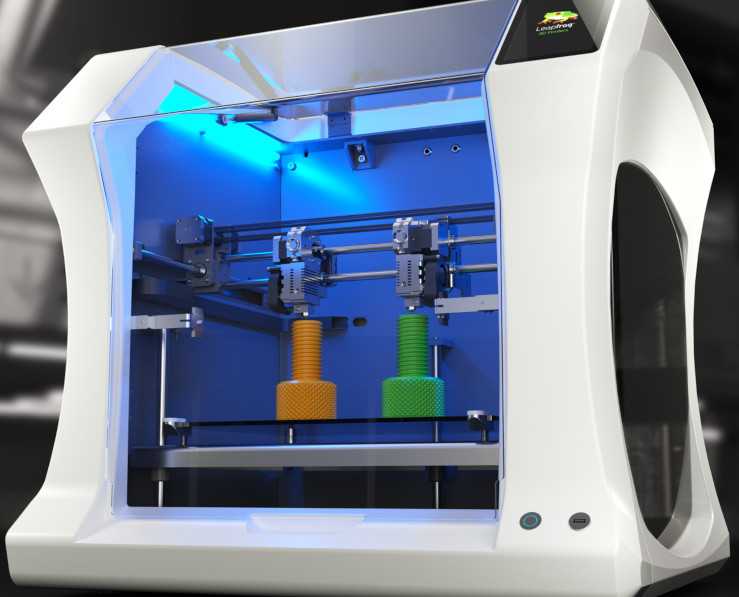
In April 2020, UK-based FabRx launched the first commercially available 3D printer for personalised drug manufacturing. M3DIMAKER is an extrusion-based printer that allows the print nozzle to be changed to accommodate different dosage requirements. Alongside the established extrusion-based fusion deposition modelling printing, whereby the printer melts the pharmaceutical mixture and excipients through a nozzle onto the build plate, the M3DIMAKER also uses a different extrusion-based method developed by FabRx: direct powder extrusion (DPE). Similar to Aprecia’s ZipDose technology, DPE deposits a powdered pharmaceutical agent onto a print bed through a nozzle aided by a single extruder. Both methods enable the manufacture of multiple-drug combination pills and sustained or delayed-release tablets.
To date, large biopharmaceutical companies have shown minimal activity in this area. In February 2020, Merck KGaA announced a collaboration with AMCM for the development and production of 3D printed pharmaceuticals for clinical trials and, later, for clinical manufacturing. The stated goal of the partnership is to develop drugs using powder bed fusion, whereby a laser melts and fuses powder together layer by layer. Merck and AMCM expect this to make the manufacturing of tablets both faster and cheaper due to the avoidance of reformulations. GlaxoSmithKline has also shown interest in 3D printing of drugs, partnering with The University of Nottingham on a study that used nozzle printing and ultraviolet curing to produce 3D printed ropinirole tablets to treat Parkinson’s disease.
The stated goal of the partnership is to develop drugs using powder bed fusion, whereby a laser melts and fuses powder together layer by layer. Merck and AMCM expect this to make the manufacturing of tablets both faster and cheaper due to the avoidance of reformulations. GlaxoSmithKline has also shown interest in 3D printing of drugs, partnering with The University of Nottingham on a study that used nozzle printing and ultraviolet curing to produce 3D printed ropinirole tablets to treat Parkinson’s disease.
The traditional one-size-fits-all model of drug development is inefficient and costly. Pharma companies need to adopt new technologies such as 3D printing to make more personalised treatments, improve R&D efficiencies, reduce costs, and minimise waste. This will not only lead to more streamlined and cost-effective supply chains, it will also improve sustainability, which has been touted as one of the most important trends across industries for 2021 and beyond.
3D printing in the medical field: four major applications revolutionising the industry
August 7, 2018updated 21 Jul 2022 8:14am
3D printing has many functions in a variety of industries, however, in the medical field it has four main applications.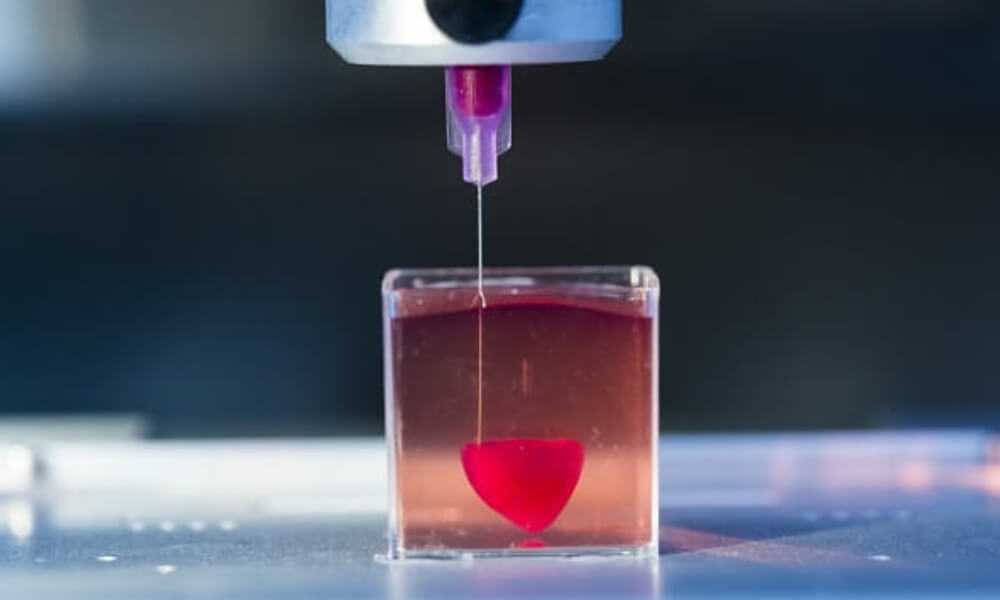 Allie Nawrat found out how this technology could be used to replace human organ transplants, speed up surgical procedures, produce cheaper versions of required surgical tools, and improve the lives of those reliant on prosthetic limbs.
Allie Nawrat found out how this technology could be used to replace human organ transplants, speed up surgical procedures, produce cheaper versions of required surgical tools, and improve the lives of those reliant on prosthetic limbs.
By Allie Nawrat
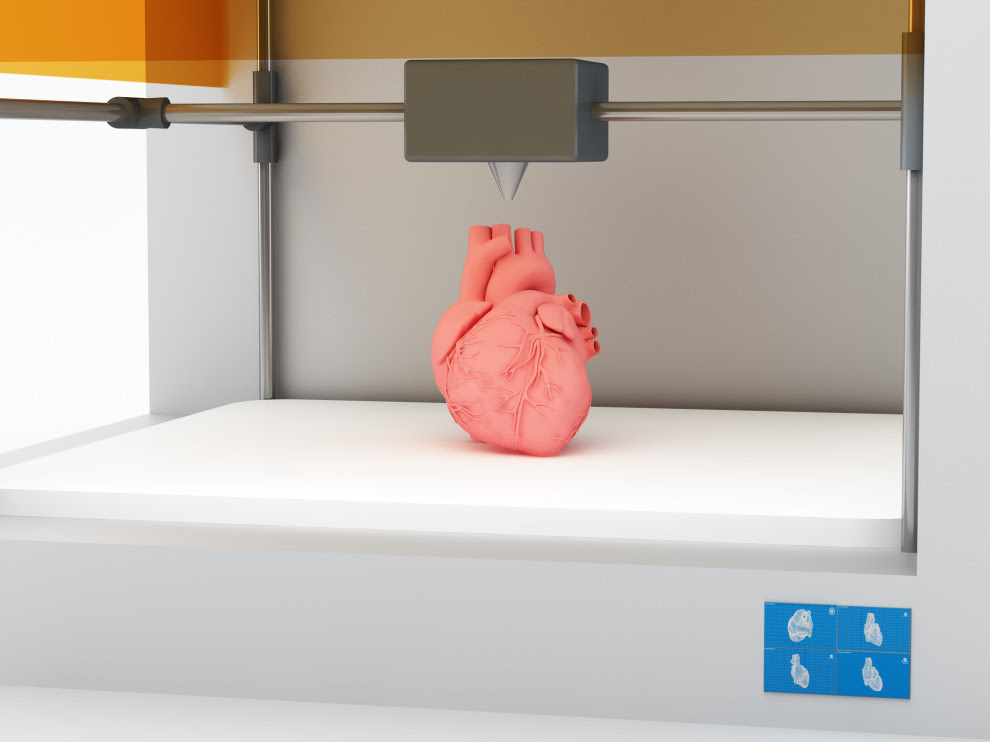
3D printed organoid. Credit: Shutterstock.Additive manufacturing, otherwise known as 3D printing, was first developed in the 1980s. It involves taking a digital model or blueprint of the subject that is then printed in successive layers of an appropriate material to create a new version of the subject.
The technique has been applied to (and utilised by) many different industries, including medical technology. Often medical imaging techniques, such as X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI) scans and ultrasounds are used to produce the original digital model, which is subsequently fed into the 3D printer.
It has been forecast that 3D printing in the medical field will be worth $3.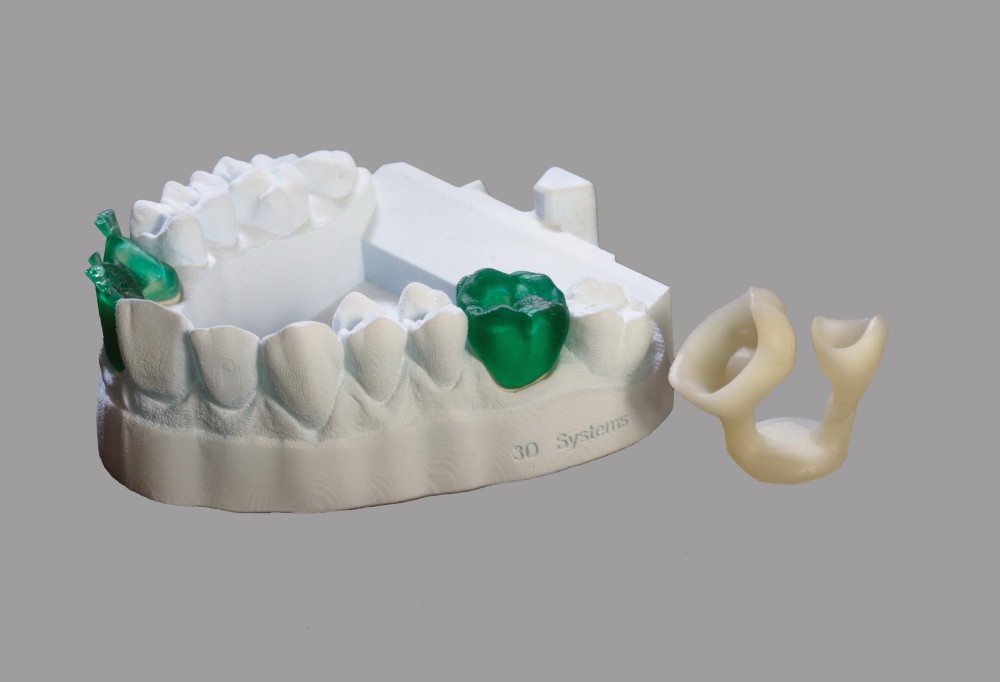 5bn by 2025, compared to $713.3m in 2016. The industry’s compound annual growth rate is supposed to reach 17.7% between 2017 and 2025.
5bn by 2025, compared to $713.3m in 2016. The industry’s compound annual growth rate is supposed to reach 17.7% between 2017 and 2025.
There are four core uses of 3D printing in the medical field that are associated with recent innovations: creating tissues and organoids, surgical tools, patient-specific surgical models and custom-made prosthetics.
Bioprinting tissues and organoids
One of the many types of 3D printing that is used in the medical device field is bioprinting. Rather than printing using plastic or metal, bioprinters use a computer-guided pipette to layer living cells, referred to as bio-ink, on top of one another to create artificial living tissue in a laboratory.
These tissue constructs or organoids can be used for medical research as they mimic organs on a miniature scale. They are also being trialled as cheaper alternatives to human organ transplants.
US-based medical laboratory and research company Organovo is experimenting with printing liver and intestinal tissue to help with the studying of organs in vitro, as well as with drug development for certain diseases. In May 2018, the company presented pre-clinical data for the functionality of its liver tissue in a programme for type 1 tyrosinemia, a condition that impedes the body’s ability to metabolise the amino acid tyrosine due to the deficiency of an enzyme.
In May 2018, the company presented pre-clinical data for the functionality of its liver tissue in a programme for type 1 tyrosinemia, a condition that impedes the body’s ability to metabolise the amino acid tyrosine due to the deficiency of an enzyme.
The Wake Forest Institute in North Carolina, US, adopted a similar approach by developing a 3D brain organoid with potential applications in drug discovery and disease modelling. The university announced in May 2018 that it’s organoids have a fully cell-based, functional blood brain barrier that mimics normal human anatomy. It has also been working on 3D printing skin grafts that can be applied directly to burn victims.
Surgery preparation assisted by the use of 3D printed models
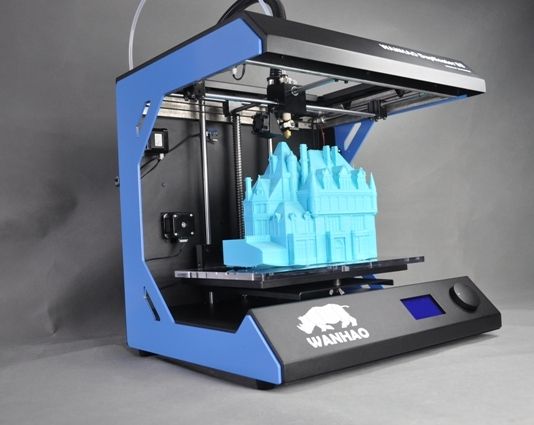
Another application of 3D printing in the medical field is creating patient-specific organ replicas that surgeons can be use to practice on before performing complicated operations. This technique has been proven to speed up procedures and minimise trauma for patients.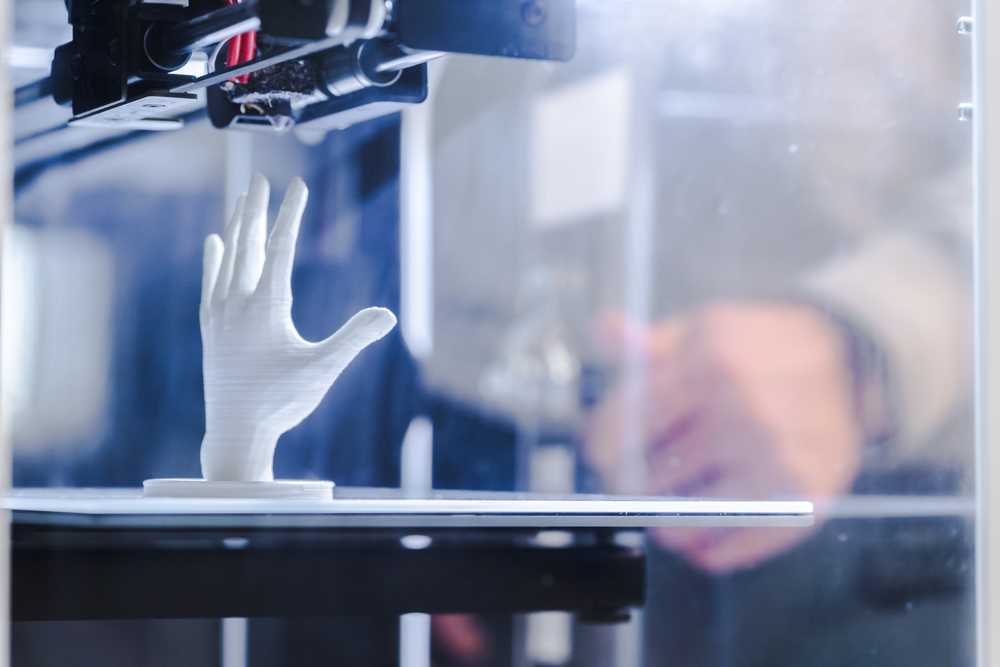
This type of procedure has been performed successfully in surgeries ranging from a full-face transplant to spinal procedures and is beginning to become routine practice.
“3D printing has been used to create patient-specific organ replicas that surgeons can be use to practice on before performing complicated operations.”
In Dubai, where hospitals have a mandate to use 3D printing liberally, doctors successfully operated on a patient who had suffered a cerebral aneurysm in four veins, using a 3D printed model of her arteries to map out how to safely navigate the blood vessels.
In January 2018, surgeons in Belfast successfully practiced for a kidney transplant for a 22-year-old woman using a 3D printed model of her donor’s kidney. The transplant was fraught with complications as her father, who was her donor, had an incompatible blood group and his kidney was discovered to have a potentially cancerous cyst. Using the 3D printed replica of his kidney, surgeons were able to assess the size and placement of the tumour and cyst.
3D printing of surgical instruments
Sterile surgical instruments, such as forceps, hemostats, scalpel handles and clamps, can be produced using 3D printers.
Not only does 3D printing produce sterile tools, some are based on the ancient Japanese practice of origami, meaning they are precise and can be made very small. These instruments can be used to operate on tiny areas without causing unnecessary extra damage to the patient.
One of the main benefits of using 3D printing rather than traditional manufacturing methods to produce surgical instruments is the production costs are significantly lower.
Custom-made prosthetics using 3D printing
3D printing in the medical field can be used to produce prosthetic limbs that are customised to suit and fit the wearer. It is common for amputees to wait weeks or months to receive prosthetics through the traditional route; however, 3D printing significantly speeds up the process, as well as creating much cheaper products that offer patients the same functionality as traditionally manufactured prosthetics.
The lower price point of these products makes them particularly applicable for use with children, who quickly outgrow their prosthetic limbs.
“3D printing can be used to produce prosthetic limbs that are customised.”
3D printing also allows the patient to design a prosthetic that corresponds directly to their needs. For example, Body Labs has created a system that allows patients to model their prosthetic on their own limbs through scanning in order to create a more natural fit and appearance. Plus, researchers at the Massachusetts Institute of Technology have sought to design more comfortable prosthetic sockets.
How 3D printing is used in domestic medicine: successful examples and developments
How do additive technologies help doctors and hospitals work? For what areas are 3D printing technologies used in our country? Consider the example of successful cases of their use in Russian medicine.
The use of 3D printing in world practice
For the first time, additive technologies in medicine were officially used in 1999, when employees of the American Wake Forest Institute of Regenerative Medicine implanted an organ made using computed tomography and a 3D printer into a human.
Now 3D printing in medicine is a rather extensive list of directions and possibilities. Among them are:
- creation of implants;
- bone print;
- modeling of human internal organs;
- creation of medical instruments for doctors.
3D printing in medicine makes it possible to model and create dental implants, prostheses, and organ prototypes with high accuracy. Also, 3D printing helps already working specialists and doctors to study and improve their skills more effectively, practice and make accurate plans for surgical operations.
With the advent of new, more and more advanced printing devices and the expansion of the list of materials, additive technologies in medicine are developing more and more rapidly. The most active 3D printing is used in the USA.
For example, in 2019, a 3D-printed finger bone was transplanted to a Florida patient for the first time. And University of Kentucky radiology and cardiology professor Michael Winkler has created a 3D printed model of the heart that doctors can work with. Such organ prototypes help surgeons plan operations more accurately and increase the chances of a patient's quick recovery.
Such organ prototypes help surgeons plan operations more accurately and increase the chances of a patient's quick recovery.
How are medical
3D technologies developing in Russia?
There are a number of successful companies in Russia that produce devices and materials for 3D printing, develop additive technologies in various industries (among them are PICASO 3D, Imprinta, Anisoprint, Tsvetnoy Mir, and many others). Domestic medicine has also achieved considerable success in terms of the use of 3D technologies.
For example, back in 2016 in Nizhny Novgorod, specialists from the Federal State Budgetary Institution “PFMIC” of the Ministry of Health of Russia performed two successful surgical interventions, during which they implanted prostheses for the hip joints printed on a 3D printer.
Since 2015, the hospital at the St. Petersburg State Pediatric Medical University has been carrying out heart surgeries, which are planned on 3D-printed organ prototypes. An important characteristic of such objects is that they are modeled taking into account all the anatomical features of a person and help surgeons perform the necessary procedures more quickly and accurately. In the treatment of heart defects, this reduces the time of the operation and reduces the risk of complications.
An important characteristic of such objects is that they are modeled taking into account all the anatomical features of a person and help surgeons perform the necessary procedures more quickly and accurately. In the treatment of heart defects, this reduces the time of the operation and reduces the risk of complications.
More information about how additive technologies are used in modern Russian medicine can be found in the report of Roman Gorbatov, head of the PIMU Laboratory of Additive Technologies, who will speak at the seventh 3D Print Expo on October 4th.
Russian "bone cement"
for the treatment of fractures
Scientists from around the world are working on the invention of the optimal material for 3D printing of bones. So, researchers from the US Northwestern University in 2016 came up with an elastic and at the same time durable material for this. Russian specialists have developed a fabric that can become an alternative to titanium implants.
Researchers from the National Research Nuclear University have created a material that is biocompatible with the human body for printing bones. It is based on the composition of animal bones, so it is not rejected when implanted. The material is quite plastic, but quickly hardens, and then gradually dissolves: the body manages to heal the damage quickly and without side inflammatory processes.
It is based on the composition of animal bones, so it is not rejected when implanted. The material is quite plastic, but quickly hardens, and then gradually dissolves: the body manages to heal the damage quickly and without side inflammatory processes.
This significantly speeds up the treatment process, reduces the risk of complications and eliminates the need for a second operation, as with titanium implants, which must be removed after a while.
This technology is implemented as follows: biocement is loaded into a 3D printer, and the damaged bone is scanned. Based on the information received, a three-dimensional model of the fragment to be printed is designed. The implant is made according to an exact design from bone cement loaded into the printer, and the material solidifies right during manufacturing, becoming strong and hard.
Prospects for 3D printing
technologies in Russian medicine
Rusatom – Additive Technologies, which is the main industry integrator uniting several enterprises, specializes in the development of the additive business in Russia.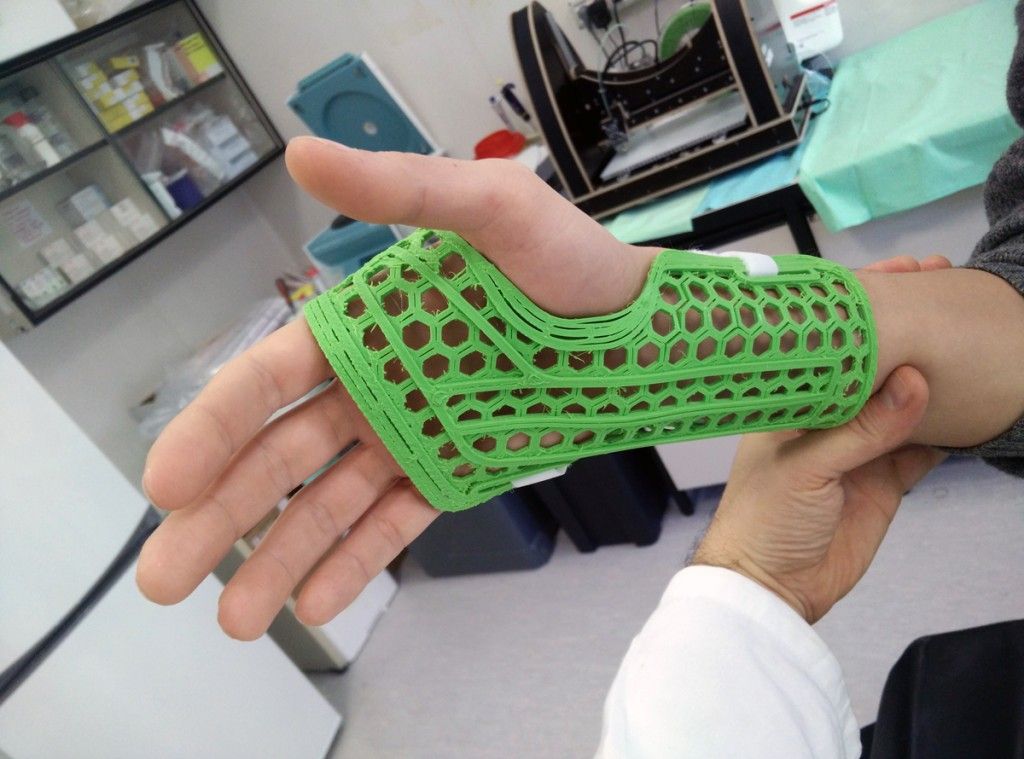 In 2020, RusAT plans to start producing 3D printed medical implants. Aleksey Dub, CEO of the company, claims that, in addition, the corresponding software will be created.
In 2020, RusAT plans to start producing 3D printed medical implants. Aleksey Dub, CEO of the company, claims that, in addition, the corresponding software will be created.
The project is currently being developed at the State Scientific Center of the Russian Federation TsNIITMASH, one of the institutes of Rosatom. The final product is an SLM printer with a three-axis optical system that will print objects using metal powder smelting technology. According to representatives of Rosatom, the printed products are anatomically accurate and ready to use. It is important that the objects are tested in the relevant authorities and are officially suitable for use.
With this SLM printing device, medical professionals can quickly create individual implants for any person (based on the data of his tomography and other studies). The cost of a Russian printer will be an order of magnitude lower than foreign counterparts.
Productivity of the device from Rusatom - Additive Technologies is 5-50 cm³ per hour. This speed will help provide patients with the necessary implants as soon as possible, which will speed up treatment and help serve more people in a certain period of time.
This speed will help provide patients with the necessary implants as soon as possible, which will speed up treatment and help serve more people in a certain period of time.
Alexey Dub, General Director of RusAT, will open the 3D Print Expo 2019 lecture hall with an introductory speech, and will also become a participant in the round table "CAE for additive technologies: a market for solutions for the future."
Click here for more information on who will be speaking at the event ►►►
5 innovative uses for 3D printing in medicine
Personalized and precise solutions in the medical field are becoming increasingly popular. New tools and advanced technologies bring doctors closer to patients by providing treatments and devices that meet the needs of each individual.
The expansion of 3D printing technologies in healthcare has made a huge contribution to improving the quality of medical services. With new tools and treatment approaches developed using 3D printing, patients feel that their treatment becomes more comfortable and personal. For physicians, the new technology available allows them to better analyze complex cases and provides new tools that can ultimately raise standards of care.
For physicians, the new technology available allows them to better analyze complex cases and provides new tools that can ultimately raise standards of care.
Later in this article, you'll learn about five areas, from models for surgical planning to vascular systems and bioreactors, in which 3D printing is used in healthcare, and why many healthcare professionals see great potential in this technology.
In today's medical practice, 3D printed anatomical models based on patient body scans are becoming more indispensable tools, as they provide more personalized and accurate treatment. As cases become more complex and standard case times become more important, visual and tactile anatomical models are helping surgeons to better understand their task, communicate more effectively, and communicate with patients more easily.
Medical professionals, hospitals and research institutes around the world use 3D printed anatomical models as a reference tool for preoperative planning, intraoperative imaging, and for sizing medical instruments or presetting equipment for both standard and very complex procedures, which is reflected in hundreds of scientific publications.
3D printing makes 3D printing affordable and easy to create customized patient anatomical models based on CT and MRI data. The peer-reviewed scientific literature demonstrates that they help clinicians better prepare for surgery, resulting in significant cost and time savings. At the same time, patient satisfaction is also increased through reduced anxiety and reduced recovery time.
Physicians can use individual patient anatomical models to explain the procedure to the patient, making it easier to obtain patient consent and reduce patient anxiety.
Preparation for surgery using preoperative models can also affect the effectiveness of the treatment. The experience of Dr. Michael Ames confirms this. After obtaining bone replications from the young patient's forearm, Dr. Ames realized that the injury was different from what he expected.
Based on this information, Dr. Ames chose a new soft tissue procedure that was much less invasive, reduced downtime, and resulted in much less scarring. Using imprinted bone replication, Dr. Ames explained the procedure to the young patient and his parents and obtained their consent.
Using imprinted bone replication, Dr. Ames explained the procedure to the young patient and his parents and obtained their consent.
Physicians can use patient-specific surgical models to explain the procedure beforehand, improving patient consent and lowering anxiety.
Result? The operation lasted less than 30 minutes instead of the originally planned three hours. With this reduction in operating time, the hospital avoided a cost of about $5,500 and the patient recovered faster.
According to Dr. Alexis Dang, Orthopedic Surgeon at UC San Francisco and Veterans Affairs Medical Center San Francisco: “All of our full-time orthopedic surgeons and almost all of our full-time surgeons part-time, used 3D printed models to treat patients at a Veterans Medical Center in San Francisco. We could all see that 3D printing improves the efficiency of our work.”
The advent of new biocompatible medical polymers for 3D printing has opened up opportunities for the development of new surgical instruments and techniques to further improve clinical operating procedures.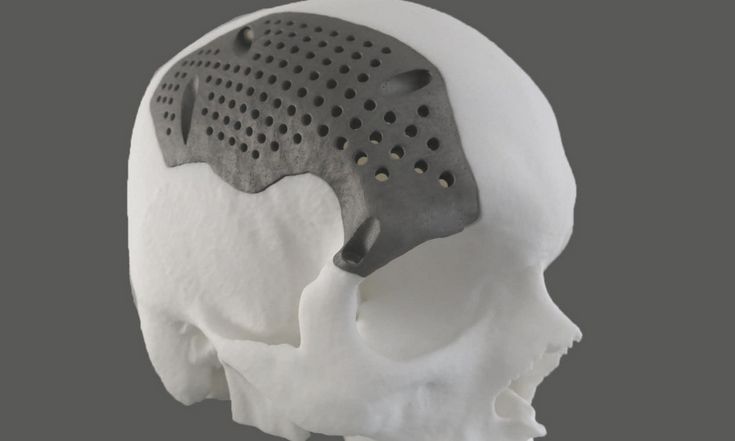 These include sterilizable trays, contoured surgical guides, and implant models that can be used to determine the size of an implant prior to surgery, helping surgeons reduce time and improve accuracy in complex procedures.
These include sterilizable trays, contoured surgical guides, and implant models that can be used to determine the size of an implant prior to surgery, helping surgeons reduce time and improve accuracy in complex procedures.
Anatomical hand model with elastic resin skin for 3D printing.
Todd Goldstein, PhD, lecturer at the Feinstein Institute for Medical Research, is unequivocal about the importance of 3D printing technology to the work of his department. He estimates that if Northwell used 3D-printed models 10-15% of the time, it could save $1,750,000 a year.
“Whether it's prototyping medical devices, complex anatomical models for our children's hospital, designing training systems, or making surgical templates for dental clinics, [3D printing technology] has increased our capabilities and reduced our costs in a variety of areas. In doing so, we were able to produce instruments for treating patients that would be almost impossible to recreate without our sought-after stereolithography 3D printer,” says Goldstein.
3D printing has become virtually synonymous with rapid prototyping. The ease of use and low cost of 3D printing in-house has also revolutionized product development, with many medical instrument manufacturers adapting the technology to produce entirely new medical devices and surgical instruments.
Over 90 percent of the top 50 medical device companies use 3D printing to create accurate medical device prototypes and fixtures and fittings to simplify testing.
According to Alex Drew, Principal Mechanical Engineer at DJO Surgical, an international medical device supplier, “Before DJO Surgical purchased [Formlabs' 3D printer], we printed nearly all of our prototypes outsourced. Today we are working with four Formlabs printers and are very pleased with the results. The speed of 3D printing has doubled, the cost has been reduced by 70%, and the level of detail allows you to effectively coordinate designs with orthopedic surgeons.
Medical companies such as Coalesce are using 3D printing to create accurate medical device prototypes.
3D printing helps speed up the design process by iterating complex designs in days instead of weeks. When Coalesce was tasked with building an inhaler device that could digitally evaluate an asthma patient's inspiratory flow profile, outsourcing would result in a significant increase in production time for each prototype. Before sending the project files to a third party company for the physical implementation of the project, they would have to be carefully developed and carried through various iterations.
Instead, desktop stereolithographic 3D printing allowed Coalesce to handle the entire prototyping process in-house. The prototypes were suitable for use in clinical trials and looked just like the finished product. Moreover, when the company demonstrated the device, its customers mistook the prototype for the final product.
Overall, the introduction of in-house manufacturing resulted in an exceptional reduction in prototyping time by 80–90%. In addition, the models took only eight hours to print and were finished and painted in a matter of days, while outsourcing the same process would take a week or two.
Hundreds of thousands of people lose limbs every year, but only a fraction of them have the ability to restore limb function with a prosthesis.
Conventional dentures are only available in a few sizes, so patients must adjust to what fits best. On the other hand, custom bionic prostheses that mimic the movements and grips of a real limb based on the impulses of the surviving limb muscles are so expensive that they can only be used by patients living in developed countries with the best medical insurance. In the case of children's prostheses, the situation is aggravated even more. Children grow up and inevitably outgrow their prostheses, which, as a result, require costly modifications.
The difficulty lies in the lack of manufacturing processes that would allow for individual orders at an affordable price. But increasingly, prosthetists are looking to reduce these high financial barriers to rehabilitation with the flexible design capabilities of 3D printing.
Initiatives like e-NABLE allow people around the world to learn about the possibilities of 3D printed prostheses. They are driving an independent movement in the prosthesis industry by offering information and free open source projects so that patients can get a custom-designed prosthesis for as little as $50.
They are driving an independent movement in the prosthesis industry by offering information and free open source projects so that patients can get a custom-designed prosthesis for as little as $50.
Other inventors like Lyman Connor go even further. With only a small fleet of four desktop 3D printers, Lyman was able to fabricate and customize his first mass-produced prostheses. His ultimate goal? Create a customizable fully bionic arm that will cost incomparably less than similar prostheses that retail for tens of thousands of dollars.
Researchers at the Massachusetts Institute of Technology have also found that 3D printing is the best method for making more comfortable prosthetic sockets.
In addition, the low cost of manufacturing these prostheses, as well as the freedom that comes with being able to design custom designs, speak for themselves. 3D printed prostheses have a lead time of just two weeks, and then they can be tried and serviced at a much lower cost than traditional counterparts.
As costs continue to fall and material properties improve, the role of 3D printing in healthcare will no doubt become more important.
The same high financial barriers that are seen in prosthetics are common in orthoses and insoles. Like many other patient-specific medical devices, custom-made orthoses are often not available due to their high cost and take weeks or months to manufacture. 3D printing solves this problem.
Confirmation is the example of Matei and his son Nick. Nick was born in 2011. Complications during preterm birth led to the fact that he developed cerebral palsy, a pathology that affects nearly twenty million people worldwide. Matei was delighted with how determined his son was to overcome the limitations of his illness, but he was faced with a choice between a standard, off-the-shelf orthosis that would be uncomfortable for his son, or an expensive custom solution that would take weeks or months to manufacture and ship. , and from which the child would quickly grow.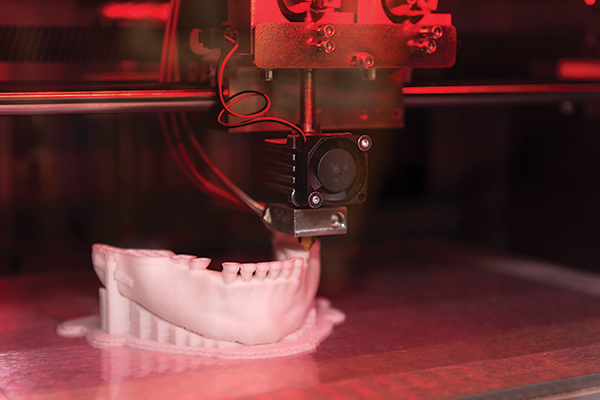
He decided to take matters into his own hands and began to look for new ways to achieve his goal. Thanks to the opportunities provided by digital technologies, in particular 3D scanning and 3D printing, Matei and Nika's physiotherapists were able to develop a completely new innovative workflow for the manufacture of ankle orthoses through experiments.
The resulting 3D-printed, custom-fit orthosis that provides support, comfort, and motion correction helped Nick take his first steps on his own. This non-standard orthopedic device reproduced the functionality of the highest-class orthopedic products, at the same time it cost many times less and did not require any additional settings.
Professionals around the world are using 3D printing as a new method of manufacturing customized insoles and orthoses for patients and clients, as well as a range of other physiotherapy tools. In the past, undergoing a course of physiotherapy with the use of individual physiotherapy instruments carried many difficulties. Often there was a situation when patients had to wait a long time for a finished product, which at the same time did not provide proper comfort. 3D printing is step by step changing this status quo. Data confirms that 3D printed insoles and orthoses offer a more precise fit and lead to better therapeutic outcomes, which means greater comfort and benefit for patients.
Often there was a situation when patients had to wait a long time for a finished product, which at the same time did not provide proper comfort. 3D printing is step by step changing this status quo. Data confirms that 3D printed insoles and orthoses offer a more precise fit and lead to better therapeutic outcomes, which means greater comfort and benefit for patients.
The usual treatments for patients with severe organ damage today are autografts, transplantation of tissue from one area of the body to another, or transplantation of a donor organ. Researchers in bioprinting and tissue engineering hope to expand this list soon with on-demand fabrication of tissues, blood vessels, and organs.
3D bioprinting is an additive manufacturing process that uses materials known as bioink (a combination of living cells and a compatible substrate) to create tissue-like structures that can be used in medicine. Tissue engineering combines new technologies, including bioprinting, which make it possible to grow replacement tissues and organs in the laboratory for use in the treatment of injuries and diseases.
Using high-precision 3D printing, researchers such as Dr. Sam Pashne-Tala from the University of Sheffield are breaking new ground in tissue engineering.
In order to direct cell growth to form the necessary tissue, Dr. Pashne-Tala grows living cells on a laboratory scaffold that provides a template of the required shape, size and geometry. For example, to create a blood vessel for a patient with cardiovascular disease, a tubular structure is needed. The cells will multiply and cover the scaffold, taking on its shape. Then the scaffold is gradually destroyed, and the living cells take the form of the target tissue, which is cultured in a bioreactor - a chamber that contains the cultured tissue and can reproduce the internal environment of the body so that the cultured tissue acquires the mechanical and biological characteristics of organic tissue.
3D printed bioreactor chamber with tissue engineered aorta miniature inside. The tissue is cultured in a bioreactor to acquire the mechanical and biological characteristics of the organic tissue.
3D printed bioreactor chamber with tissue engineered aorta miniature inside. The tissue is cultured in a bioreactor to acquire the mechanical and biological characteristics of the organic tissue.
This will allow scientists to design patient-specific vascular grafts, expand surgical care, and provide a unique platform for testing new vascular medical devices for people suffering from cardiovascular disease, which is currently the leading cause of death worldwide. The ultimate goal is to create blood vessels that are ready for implantation in patients. Since tissue engineering uses cells taken from a patient in need of treatment, this eliminates the possibility of rejection by the immune system, which is the main problem of modern transplantation.
3D printing has proven its ability to solve the problems that exist in the production of synthetic blood vessels, in particular, the difficulty of recreating the required accuracy of the shape, size and geometry of the vessel. The ability of printed solutions to clearly reflect the specific characteristics of patients was a step forward.
The ability of printed solutions to clearly reflect the specific characteristics of patients was a step forward.
According to Dr. Pashne-Tal: “[Creating blood vessels using 3D printing] makes it possible to expand the possibilities of surgical care and even create designs of blood vessels for a specific patient. Without the existence of high-precision affordable 3D printing, the creation of such forms would not be possible.”
We are witnessing significant advances in the development of biological materials that can be used in 3D printers. Scientists are developing new hydrogel materials that have the same consistency as organ tissues present in the human brain and lungs, which can be used in a range of 3D printing processes. Scientists hope that they will be able to implant them into the body as a "scaffold" for cell growth.
Although bioprinting of fully functional internal organs such as the heart, kidneys and liver still looks futuristic, hybrid 3D printing at very high speed opens up more and more new horizons.
It is expected that sooner or later the creation of biological matter on laboratory printers will lead to the generation of new, fully functional 3D printed organs. In April 2019, scientists at Tel Aviv University 3D-printed the first heart using biological tissue from a patient. A tiny copy was created using the patient's own biological tissues, which made it possible to fully match the immunological, cellular, biochemical and anatomical profile of the patient.
“At this stage, the heart we printed is small, about the size of a rabbit heart, but normal-sized human hearts require the same technology,” says Prof. Tal Dvir.
The first 3D bioprinted heart created at Tel Aviv University.
Precise and affordable 3D printing processes, such as desktop stereolithography, are democratizing access to technology, enabling healthcare professionals to develop new clinical solutions and quickly produce medical devices with individual characteristics, and doctors around the world to offer new types of therapy.