Cnn 3d printing organs
3D-printed organs: The future of transplantation
CNN —
What if doctors could just print a kidney, using cells from the patient, instead of having to find a donor match and hope the patient’s body doesn’t reject the transplanted kidney?
The soonest that could happen is in a decade, thanks to 3D organ bioprinting, said Jennifer Lewis, a professor at Harvard University’s Wyss Institute for Biologically Inspired Engineering. Organ bioprinting is the use of 3D-printing technologies to assemble multiple cell types, growth factors and biomaterials in a layer-by-layer fashion to produce bioartificial organs that ideally imitate their natural counterparts, according to a 2019 study.
This type of regenerative medicine is in the development stage, and the driving force behind this innovation is “real human need,” Lewis said.
In the United States, there are 106,075 men, women and children on the national organ transplant waiting list as of June 10, according to the Health Resources & Services Administration. However, living donors provide only around 6,000 organs per year on average, and there are about 8,000 deceased donors annually who each provide 3.5 organs on average.
47-year-old Steve Verze is to become the first man in the world to be fitted with a 3D printed eye, according to Moorfields Eye Hospital.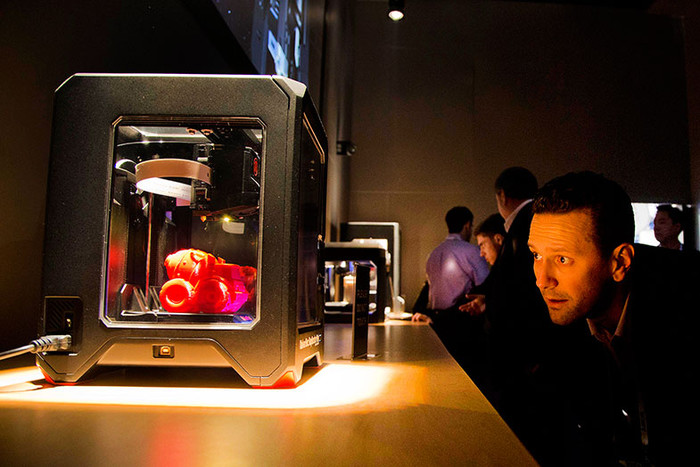 He tried the eye for size earlier this month, as photographed here.
He tried the eye for size earlier this month, as photographed here.
British man given 3D printed eye in world first, hospital says
The cause of this discrepancy is “a combination of people who undergo catastrophic health events, but their organs aren’t high enough quality to donate, or they’re not on the organ donor list to begin with, and the fact that it’s actually very difficult to find a good match” so the patient’s body doesn’t reject the transplanted organ, Lewis said.
And even though living donors are an option, “to do surgery on someone who doesn’t need it” is a big risk, said Dr. Anthony Atala, director of the Wake Forest Institute for Regenerative Medicine. “So, living related donors are usually not the preferred way to go because then you’re taking an organ away from somebody else who may need it, especially now as we age longer.”
Anthony Atala, director of the Wake Forest Institute for Regenerative Medicine. “So, living related donors are usually not the preferred way to go because then you’re taking an organ away from somebody else who may need it, especially now as we age longer.”
Atala and his colleagues were responsible for growing human bladders in a lab by hand in 2006, and implanting a complicated internal organ into people for the first time – saving the lives of three children in whom they implanted the bladders.
A bladder scaffold is seeded with cells at the Wake Forest Institute for Regenerative Medicine.
Courtesy Wake Forest Institute for Regenerative Medicine Every day, 17 people die waiting for an organ transplant, according to the Health Resources & Services Administration. And every nine minutes, another person is added to the waitlist, the agency says. More than 90% of the people on the transplant list in 2021 needed a kidney.
And every nine minutes, another person is added to the waitlist, the agency says. More than 90% of the people on the transplant list in 2021 needed a kidney.
“About a million people worldwide are in need of a kidney. So they have end-stage renal failure, and they have to go on dialysis,” Lewis said. “Once you go on dialysis, you have essentially five years to live, and every year, your mortality rate increases by 15%. Dialysis is very hard on your body. So this is really motivating to take on this grand challenge of printing organs.”
“Anti-hypertensive pills are not scarce. Everybody who needs them can get them,” Martine Rothblatt, CEO and chairman of United Therapeutics, said at the Life Itself conference, a health and wellness event presented in partnership with CNN.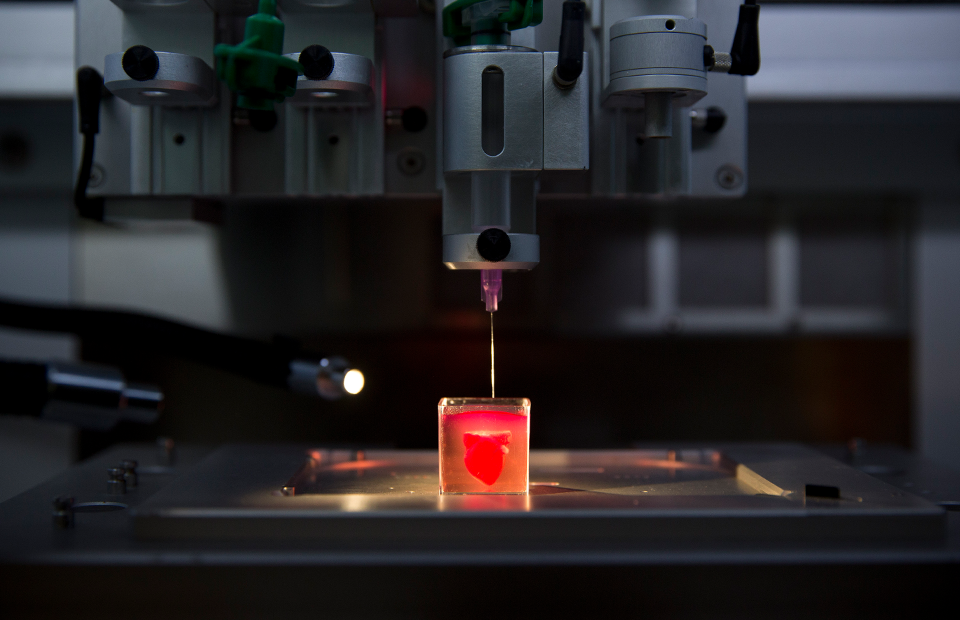 United Therapeutics is one of the conference’s sponsors.
United Therapeutics is one of the conference’s sponsors.
“There is no practical reason why anybody who needs a kidney – or a lung, a heart, a liver – should not be able to get one,” she added. “We’re using technology to solve this problem.”
To begin the process of bioprinting an organ, doctors typically start with a patient’s own cells. They take a small needle biopsy of an organ or do a minimally invasive surgical procedure that removes a small piece of tissue, “less than half the size of a postage stamp,” Atala said. “By taking this small piece of tissue, we are able to tease cells apart (and) we grow and expand the cells outside the body.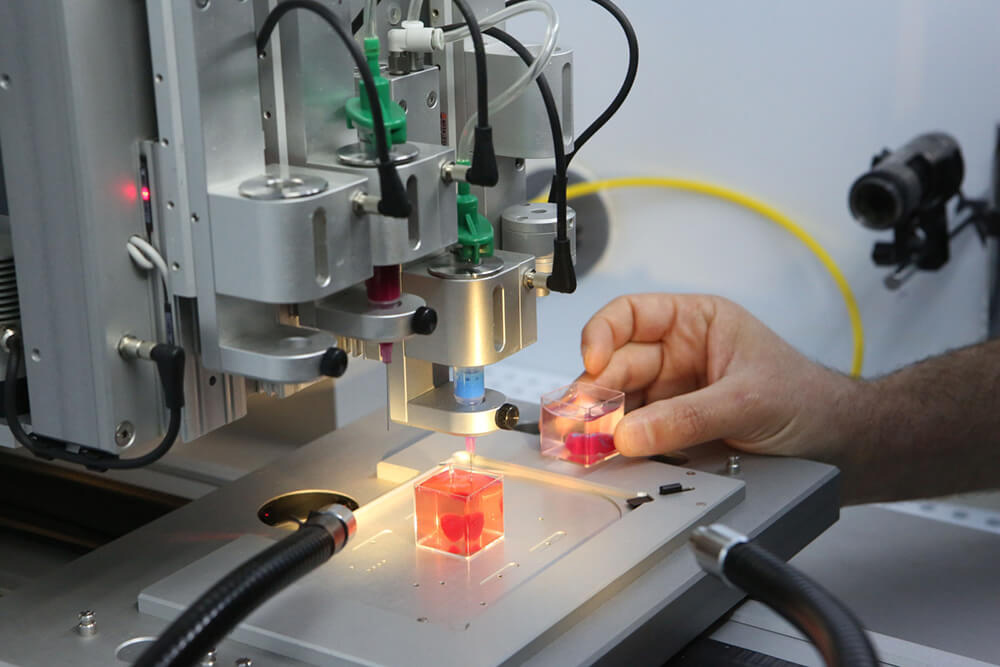 ”
”
This growth happens inside a sterile incubator or bioreactor, a pressurized stainless steel vessel that helps the cells stay fed with nutrients – called “media” – the doctors feed them every 24 hours, since cells have their own metabolism, Lewis said. Each cell type has a different media, and the incubator or bioreactor acts as an oven-like device mimicking the internal temperature and oxygenation of the human body, Atala said.
“Then we mix it with this gel, which is like a glue,” Atala said. “Every organ in your body has the cells and the glue that holds it together. Basically, that’s also called ‘extracellular matrix.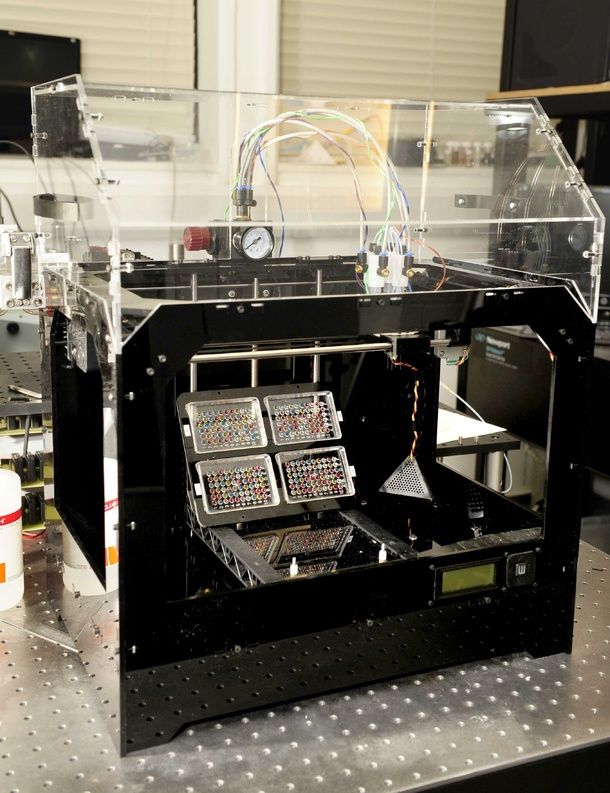 ’ ”
’ ”
Richard Roth with Samira Jafari
Courtesy Samira JafariLiving organ donations save lives. This is how you become a donor
This glue is Atala’s nickname for bioink, a printable mixture of living cells, water-rich molecules called hydrogels, and the media and growth factors that help the cells continue to proliferate and differentiate, Lewis said. The hydrogels mimic the human body’s extracellular matrix, which contains substances including proteins, collagen and hyaluronic acid.
The non-cell sample portion of the glue can be made in a lab, and “is going to have the same properties of the tissue you’re trying to replace,” Atala said.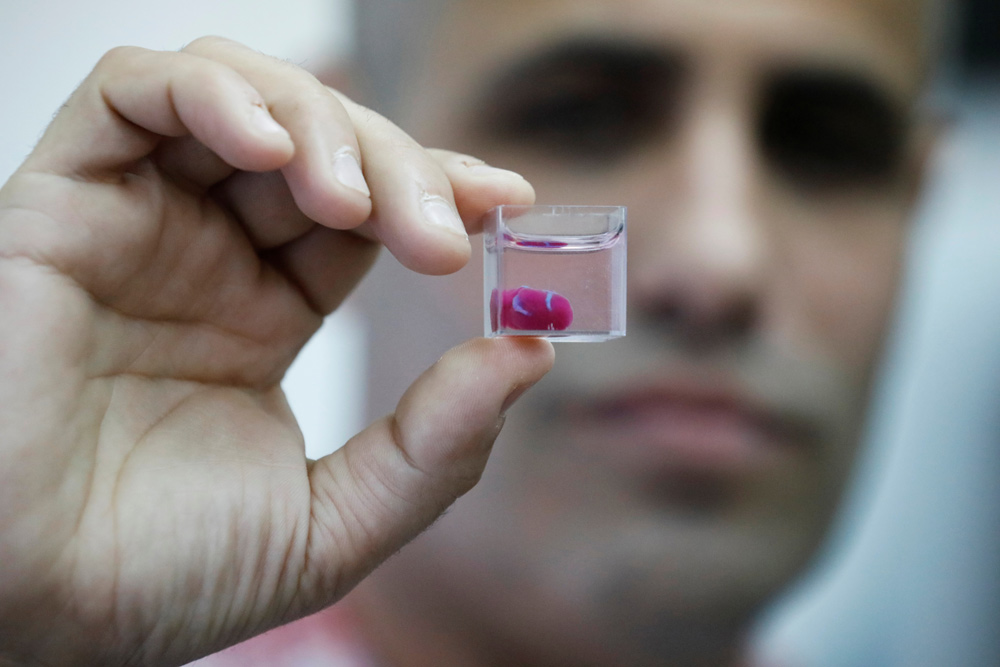
The biomaterials used typically have to be nontoxic, biodegradable and biocompatible to avoid a negative immune response, Lewis said. Collagen and gelatin are two of the most common biomaterials used for bioprinting tissues or organs.
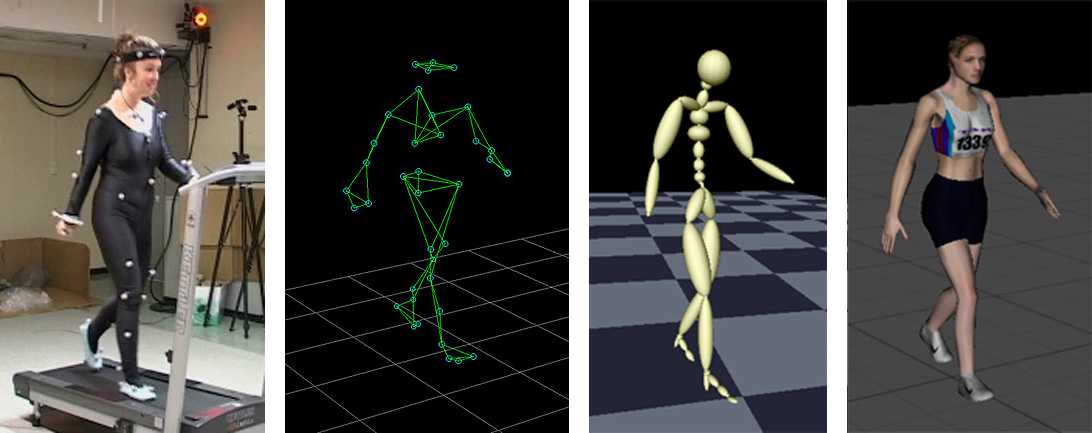
From there, doctors load each bioink – depending on how many cell types they’re wanting to print – into a printing chamber, “using a printhead and nozzle to extrude an ink and build the material up layer by layer,” Lewis said. Creating tissue with personalized properties is enabled by printers being programmed with a patient’s imaging data from X-rays or scans, Atala said.
“With a color printer you have several different cartridges, and each cartridge is printing a different color, and you come up with your (final) color,” Atala added. Bioprinting is the same; you’re just using cells instead of traditional inks.
How long the printing process takes depends on several factors, including the organ or tissue being printed, the fineness of the resolution and the number of printheads needed, Lewis said. But it typically lasts a few to several hours. The time from the biopsy to the implantation is about four to six weeks, Atala said.
A 3D printer seeds different types of cells onto a kidney scaffold at the Wake Forest Institute for Regenerative Medicine.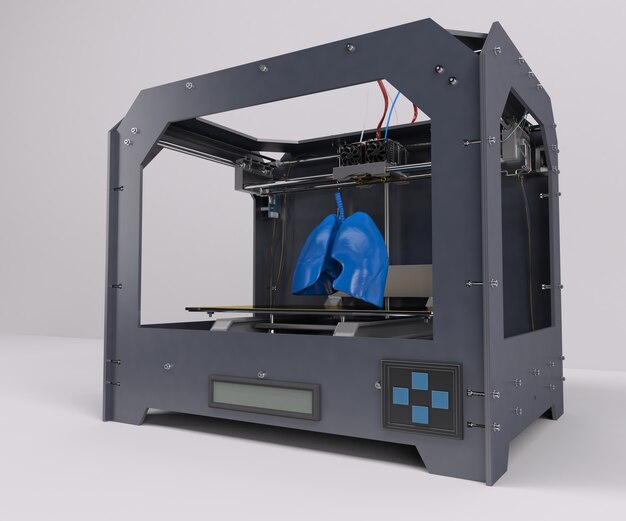
The ultimate challenge is “getting the organs to actually function as they should,” so accomplishing that “is the holy grail,” Lewis said.
“Just like if you were to harvest an organ from a donor, you have to immediately get that organ into a bioreactor and start perfusing it or the cells die,” she added. To perfuse an organ is to supply it with fluid, usually blood or a blood substitute, by circulating it through blood vessels or other channels.
Depending on the organ’s complexity, there is sometimes a need to mature the tissue further in a bioreactor or further drive connections, Lewis said. “There’s just a number of plumbing issues and challenges that have to be done in order to make that printed organ actually function like a human organ would in vivo (meaning in the body). And honestly, this has not been fully solved yet.”
“There’s just a number of plumbing issues and challenges that have to be done in order to make that printed organ actually function like a human organ would in vivo (meaning in the body). And honestly, this has not been fully solved yet.”
Once a bioprinted organ is implanted into a patient, it will naturally degrade over time – which is OK since that’s how it’s designed to work.
“You’re probably wondering, ‘Well, then what happens to the tissue? Will it fall apart?’ Actually, no,” Atala said. “These glues dissolve, and the cells sense that the bridge is giving way; they sense that they don’t have a firm footing anymore. So cells do what they do in your very own body, which is to create their own bridge and create their own glue.”
So cells do what they do in your very own body, which is to create their own bridge and create their own glue.”
Atala and Lewis are conservative in their estimates about the number of years remaining before fully functioning bioprinted organs can be implanted into humans.
“The field’s moving fast, but I mean, I think we’re talking about a decade plus, even with all of the tremendous progress that’s been made,” Lewis said.
“I learned so many years ago never to predict because you’ll always be wrong,” Atala said.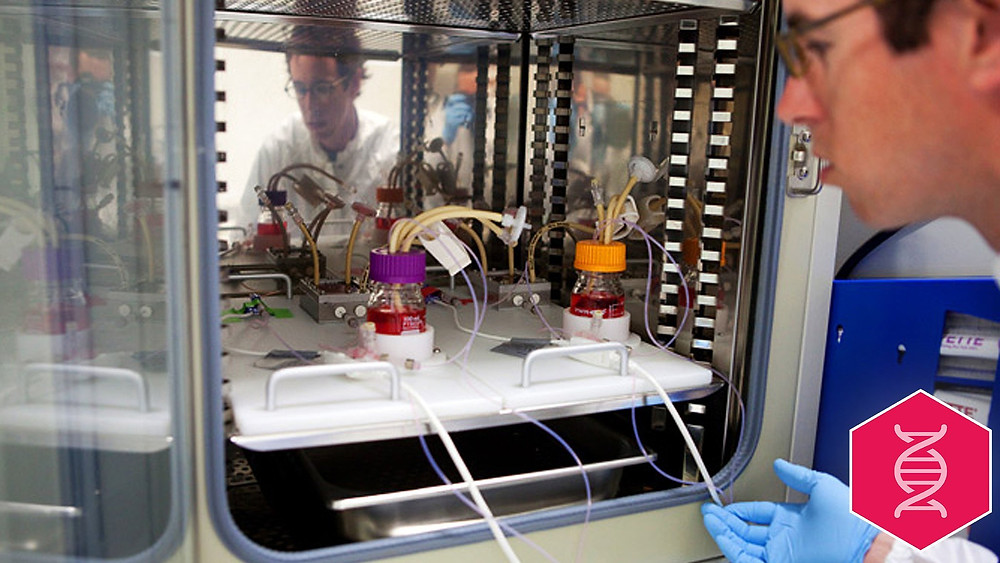 “There’s so many factors in terms of manufacturing and the (US Food and Drug Administration regulation). At the end of the day, our interest, of course, is to make sure the technologies are safe for the patient above all.”
“There’s so many factors in terms of manufacturing and the (US Food and Drug Administration regulation). At the end of the day, our interest, of course, is to make sure the technologies are safe for the patient above all.”
Whenever bioprinting organs becomes an available option, affordability for patients and their caregivers shouldn’t be an issue.
They’ll be “accessible for sure,” Atala said. “The costs associated with organ failures are very high. Just to keep a patient on dialysis is over a quarter of a million dollars per year, just to keep one patient on dialysis. So, it’s a lot cheaper to create an organ that you can implant into the patient. ”
”
The average kidney transplant cost was $442,500 in 2020, according to research published by the American Society of Nephrology – while 3D printers retail for around a few thousand dollars to upward of $100,000, depending on their complexity. But even though low-cost printers are available, pricey parts of bioprinting can include maintaining cell banks for patients, culturing cells and safely handling biological materials, Lewis said.
Some of the major costs of current organ transplantation are “harvesting the organ from the donor, the transport costs and then, of course, the surgery that the recipient goes through, and then all the care and monitoring,” Lewis said.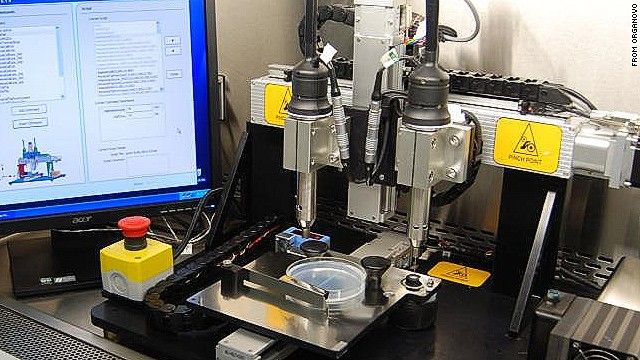 “Some of that cost would still be in play, even if it was bioprinted.”
“Some of that cost would still be in play, even if it was bioprinted.”
The next frontier in 3-D printing: Human organs
Story highlights
3-D printers may someday be producing complex -- and controversial -- human organs
Their precise process can reproduce vascular systems required to make organs viable
Doctor: "It has the potential for being a very important breakthrough"
Researcher: Bioprinting will spark a major ethical debate by 2016
CNN —
The emerging process of 3-D printing, which uses computer-created digital models to create real-world objects, has produced everything from toys to jewelry to food.
Soon, however, 3-D printers may be spitting out something far more complex, and controversial: human organs.
For years now, medical researchers have been reproducing human cells in laboratories by hand to create blood vessels, urine tubes, skin tissue and other living body parts. But engineering full organs, with their complicated cell structures, is much more difficult.
Enter 3-D printers, which because of their precise process can reproduce the vascular systems required to make organs viable. Scientists are already using the machines to print tiny strips of organ tissue. And while printing whole human organs for surgical transplants is still years away, the technology is rapidly developing.
“The mechanical process isn’t all that complicated. The tricky part is the materials, which are biological in nature,” said Mike Titsch, editor-in-chief of 3D Printer World, which covers the industry. “It isn’t like 3-D printing plastic or metal. Plastic doesn’t die if you leave it sitting on an open-air shelf at room temperature for too long.”
Lawrence Bonassar, a professor of biomedical engineering at Cornell University, with an artificial ear made via 3-D printing and injectable molds.
From Cornell University Photography The idea of printing a human kidney or liver in a lab may seem incomprehensible, even creepy. But to many scientists in the field, bioprinting holds great promise. Authentic printed organs could be used for drug or vaccine testing, freeing researchers from less accurate methods such as tests on animals or on synthetic models.
Authentic printed organs could be used for drug or vaccine testing, freeing researchers from less accurate methods such as tests on animals or on synthetic models.
Then there’s the hope that 3-D printers could someday produce much-needed organs for transplants. Americans are living longer, and as we get deeper into old age our organs are failing more. Some 18 people die in the United States each day waiting in vain for transplants because of a shortage of donated organs – a problem that Anthony Atala, director of the Wake Forest Institute for Regenerative Medicine and a pioneer in bioprinting, calls “a major health crisis.”
An ‘exciting new area of medicine’
Bioprinting works like this: Scientists harvest human cells from biopsies or stem cells, then allow them to multiply in a petri dish. The resulting mixture, a sort of biological ink, is fed into a 3-D printer, which is programmed to arrange different cell types, along with other materials, into a precise three-dimensional shape. Doctors hope that when placed in the body, these 3-D-printed cells will integrate with existing tissues.
The process already is seeing some success. Last year a 2-year-old girl in Illinois, born without a trachea, received a windpipe built with her own stem cells. The U.S. government has funded a university-led “body on a chip” project that prints tissue samples that mimic the functions of the heart, liver, lungs and other organs.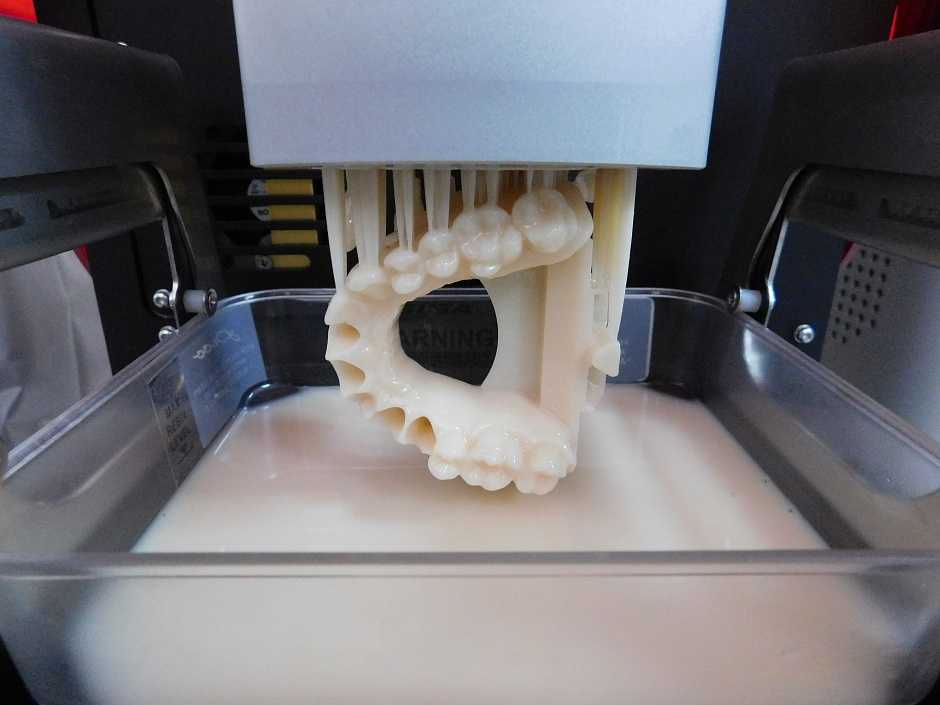 The samples are placed on a microchip and connected with a blood substitute to keep the cells alive, allowing doctors to test specific treatments and monitor their effectiveness.
The samples are placed on a microchip and connected with a blood substitute to keep the cells alive, allowing doctors to test specific treatments and monitor their effectiveness.
“This is an exciting new area of medicine. It has the potential for being a very important breakthrough,” said Dr. Jorge Rakela, a gastroenterologist at the Mayo Clinic in Phoenix and a member of the American Liver Foundation’s medical advisory committee.
One of Organovo's engineers oversees the construction of a vascular tissue construct on a NovoGen MMX bioprinter.
From Organovo “Three-D printing allows you to be closer to what is happening in real life, where you have multiple layers of cells,” he said.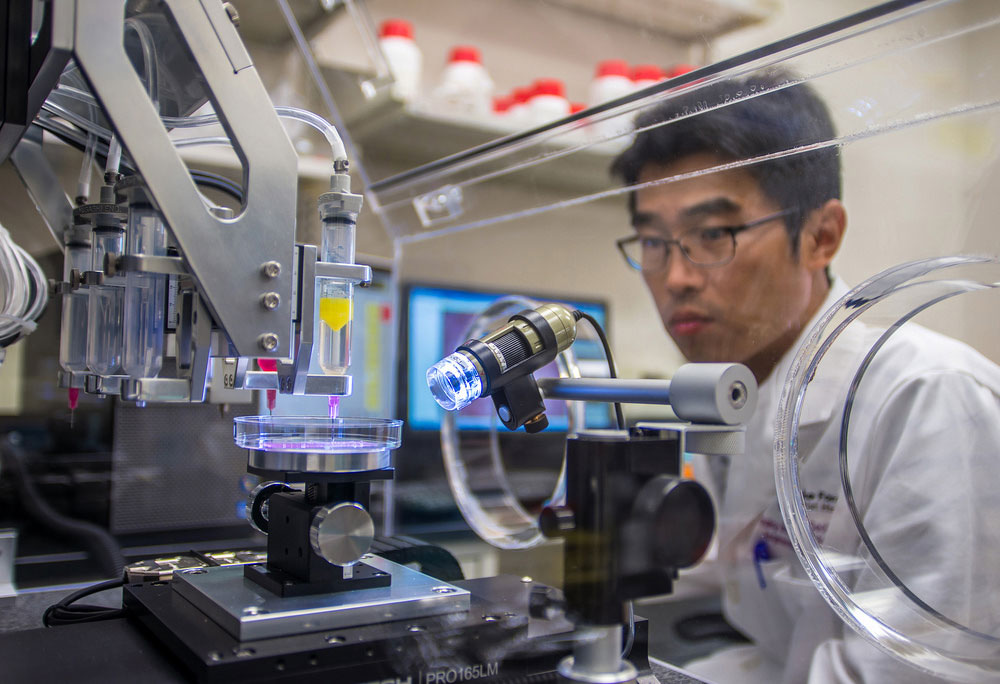 With current 2-D models, “if you grow more than one or two layers, the cells at the bottom suffocate from lack of oxygen.”
With current 2-D models, “if you grow more than one or two layers, the cells at the bottom suffocate from lack of oxygen.”
To accelerate the development of bioprinted organs, a Virginia foundation that supports regenerative medicine research announced in December it will award a $1 million prize for the first organization to print a fully functioning liver.
One early contender for the prize is Organovo, a California start-up that has been a leader in bioprinting human body parts for commercial purposes. Using cells from donated tissue or stem cells, Organovo is developing what it hopes will be authentic models of human organs, primarily livers, for drug testing.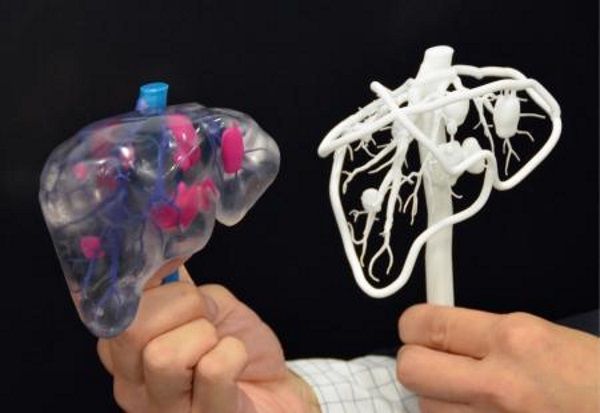
The company has printed strips of human liver tissue in its labs, although they are still very small: four by four by one millimeter, or about one-fourth the size of a dime. Each strip takes about 45 minutes to print, and it takes another two days for the cells to grow and mature, said Organovo CEO Keith Murphy. The models can then survive for about 40 days.
Organovo has also built models of human kidneys, bone, cartilage, muscle, blood vessels and lung tissue, he said.
“Basically what it allows you to do is build tissue the way you assemble something with Legos,” Murphy said.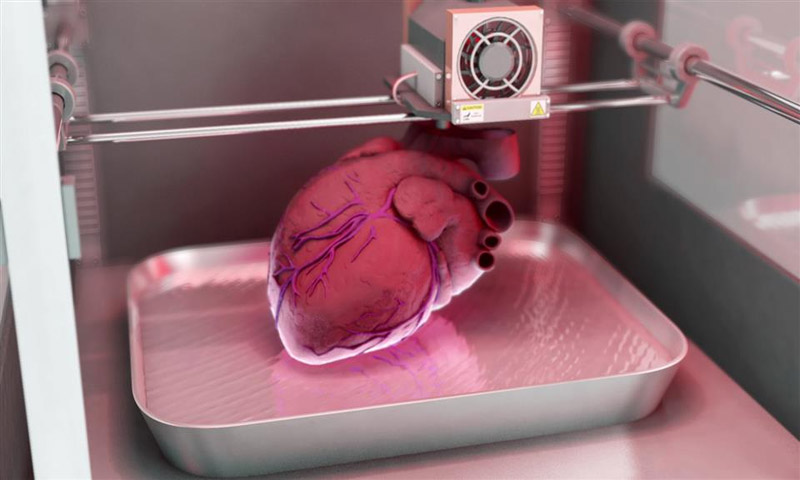 “So you can put the right cells in the right places. You can’t just pour them into a mold.”
“So you can put the right cells in the right places. You can’t just pour them into a mold.”
Ethical concerns
Not everyone is comfortable with this bold new future of lab-built body parts, however.
A research director at Gartner Inc., the information-technology research and advisory firm, believes 3-D bioprinting is advancing so quickly that it will spark a major ethical debate by 2016.
A 3-D printer at Cornell University produces an artificial ear.
“Three-D bioprinting facilities with the ability to print human organs and tissue will advance far faster than general understanding and acceptance of the ramifications of this technology,” Pete Basiliere said in a recent report.
“These initiatives are well-intentioned, but raise a number of questions that remain unanswered,” Basiliere added. “What happens when complex ‘enhanced’ organs involving nonhuman cells are made? Who will control the ability to produce them? Who will ensure the quality of the resulting organs?”
Bioprinted organs are also likely to be expensive, which could put them out of reach of all but the wealthiest patients.
Murphy said Organovo only uses human cells in creating tissues, and doesn’t see any ethical problems with what his company is doing.
“People used to worry about doing research on cadavers … and that dissipated very quickly,” he said. “We don’t think there’s any controversy if you’re producing good data and helping people with health conditions.”
Most experts, including Wake Forest’s Atala, don’t think we’ll see complex 3-D-printed organs, suitable for transplants, for years if not decades.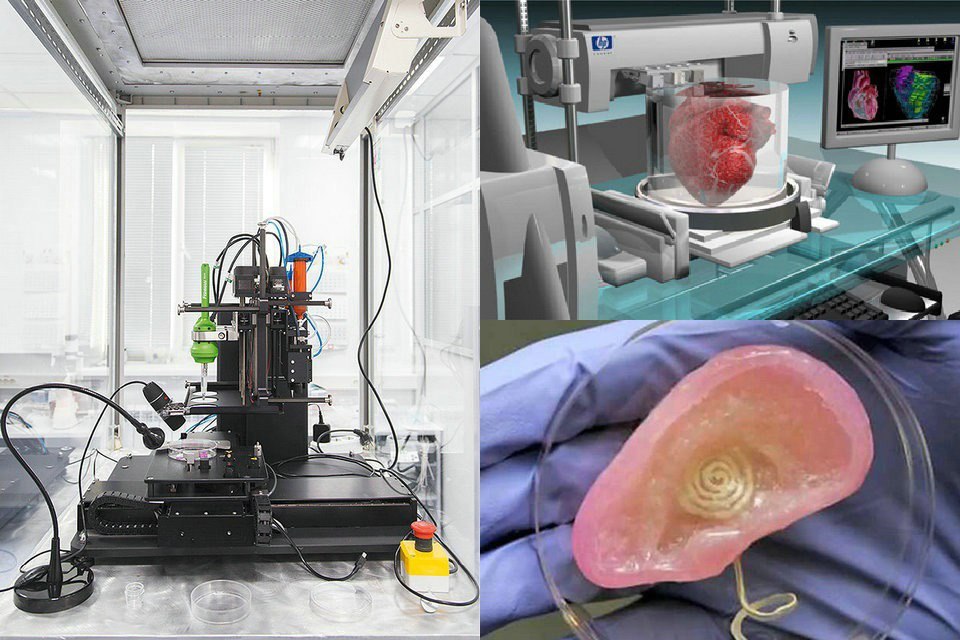 Instead, they believe the next step will be printing strips of tissue, or patches, that could be used to repair livers and other damaged organs.
Instead, they believe the next step will be printing strips of tissue, or patches, that could be used to repair livers and other damaged organs.
Organovo's NovoGen MMX bioprinter is small enough to fit into a cabinet.
From Organovo“We are very eager to put pieces of tissue to work for surgical transplants,” said Organovo’s Murphy, who hopes his company will be ready to begin clinical trials within five years.
Of course, any use of 3-D-printed tissue in surgical procedures would require approval by the U.S. Food and Drug Administration. That review process could take up to a decade.
By then, the notion of a surgeon putting a 3-D-printed kidney into a patient may not seem so bizarre. Then again, this swiftly evolving technology may create new moral conundrums.
“The ethical questions are bound to be the same concerns we have seen in the past. Many major medical breakthroughs have suffered moral resistance, from organ transplants to stem cells,” said Titsch of 3D Printer World.
“Will only the rich be able to afford it? Are we playing God? In the end, saving lives tends to trump all objections. ”
”
Printing organs: how ears, skin and noses are made with a 3D printer
- Natalka Pisnya
- BBC Russian Service, USA
it will help you sort things out.
Image copyright, Masela family archive
Photo caption,Luc Masela with his parents one month after the artificial bladder transplant. year 2001.
Luc Masela, now 27, is an athlete with a degree in economics, works for a major exhibition company, travels a lot and recently met, in his words, "the most beautiful girl in the world." Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
Luke was born with spina bifida - and although he was able to walk, his bladder was severely damaged. By the age of 10, he almost did not leave hospitals: due to improper functioning of the bladder, fluid began to return to the boy's kidneys, doctors diagnosed an irreversible pathology of the organ.
You need JavaScript enabled or a different browser to view this content
Video caption,"3D printed" organs are here
Doctors offered the family two solutions: lifelong dialysis or the creation of a new bladder from a segment of the intestine. This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
The urologist in charge of the boy suggested that Masela's family take part in an experimental program to grow a new bladder from his own cells. Then, in 2001, it sounded like science fiction: only nine people took part in the program before Luke. Despite this, his family agreed.
"The essence of the operation was reduced to two stages: first, a piece of bladder tissue was taken from me, and over the next two months, cells were grown in the laboratory in order to grow a new healthy bladder from them," says Luke.
Photo copyright, Masela family archive
Photo caption,Luc Masela, 17 years after the artificial bladder transplant
Next was the transplant operation, which, according to him, lasted 16 hours. “I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
“I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
The operation was performed by Dr. Anthony Atala, Pediatric Regenerative Surgeon. In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like a normal organ, taking root thanks to Luke’s own cells.
- An animal capable of regrowing its head
- The birth of a chimera: why do scientists need a human-animal hybrid?
- Swedish company 3D prints body parts
Luke and Dr. Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.
Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.
The professor took charge of the Wake Forest Institute of Regenerative Medicine in North Carolina in those 10 years, but Luke was never forgotten: his bladder was one of the most challenging and most successful projects in his early practice.
By 2018, Atala won the Christopher Columbus Award for "work on a discovery that will have a significant impact on society"; The Times and Scientific American magazines at various times named him "Physician of the Year", he was also recognized as "one of the 50 scientists on the planet who in the next 10 years will change the way we live and work."
How to print a new face
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.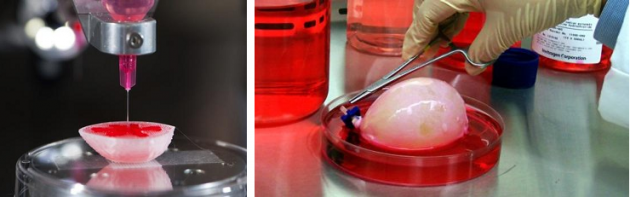
episodes
The End of the Story Podcast
In the mid-2000s, Atala's team turned their attention to an ordinary household 3D printer and wrote special software for it, later specialized machines were created for the laboratory. Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
One of the team's latest achievements is ears and noses grown outside the human body.
The main customer and sponsor of Atala's developments is the US Department of Defense, and many of the patients are military victims of military operations.
It works like this: first, a CT scan of the ear or nose is done. One of Atala's assistants, Joshua Corpus, jokes that at this stage, people often ask to "improve" the shape of the nose if they thought theirs was too wide or hooked, and the ears if they were too wide.
After that, a special computer code is written, and the printing of the base of the organs begins.
For this, a bioabsorbable polymer, polycaprolactam, is used. At the same time flexible and durable, in the human body it disintegrates within four years.
After printing, the layers of polycaprolactam resemble lace; after transplantation, their place will be taken by a person's own cartilage tissue in a few years after transplantation.
Polycaprolactam is then saturated with a gel created from the patient's cells, cooled to -18 degrees Celsius - so the cells, according to scientists, are not damaged, they are "alive and happy."
Image caption,Printing a test kidney sample on a bioprinter
In order for the polymer and gel structure to take shape and become something more durable, ultraviolet light is used in the laboratory - it does not damage cells.
The future implant is printed for 4-5 hours, then it is finally formed and inserted under the epidermis.
Skin can also be grown: children affected by the fires were the first to participate in the early trials of Atala - after the "printing" of the skin, scientists observed the patients for several more years. The new skin did not crack, did not burst, and grew with the children.
The new skin did not crack, did not burst, and grew with the children.
The most difficult job, according to the scientist, is facial wounds: it’s not enough just to stretch the skin, you need to accurately calculate the geometry, align swelling, bone structure, and understand how a person will look after that.
In addition to the skin and ears, Atala can "print" the bones of the jaws, grow blood vessels and cells of some organs - the liver, kidneys, lungs.
This technology is especially appreciated by oncologists: on the basis of patient cells, it is possible to recreate the body's response to various types of chemotherapy and observe the reaction to a particular type of treatment in the laboratory, and not on a living person.
But the liver, kidneys, lungs and heart are still being tested. Atala says he raised them in miniature, but creating organs from various tissues to real size requires a lot of additional research.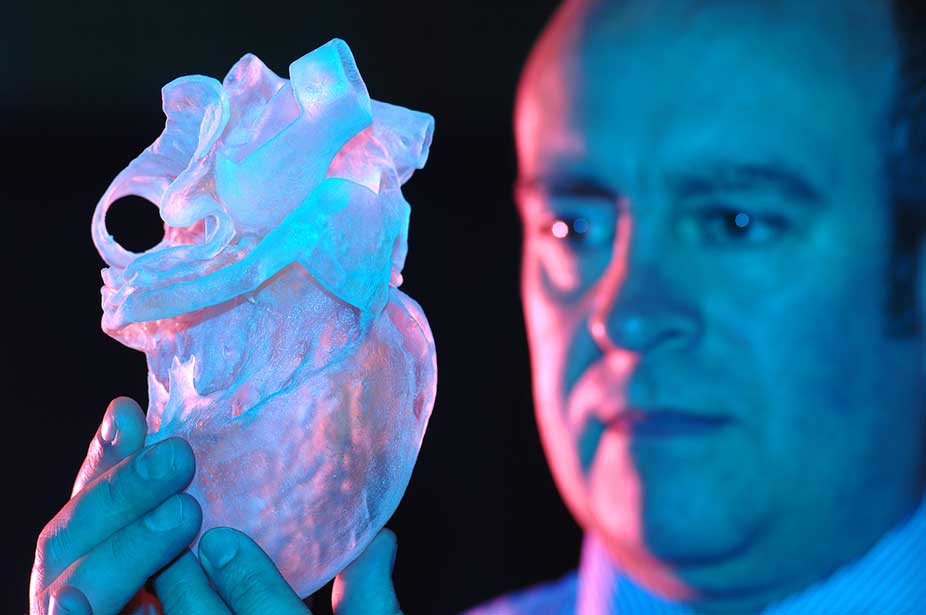
But, according to him, cells were grown in the laboratory and a vagina was created for a girl who was born several years ago with a congenital deformity of the genital organs - several years have passed since the transplant.
Image caption,Bioprinted polycaprolactam ear implant base
Atala smiles and adds that his team is also working on a working penis. This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
Among others, Igor Vasyutin, a Russian post-graduate student of the First Moscow State Medical University (MGMU) named after Sechenov, is working on this under laboratory conditions. He is a cell biologist, Atala's right hand.
Vasyutin has been in the USA for about a year - he came on an exchange. He is ready to talk about the behavior of stem cells for hours, but becomes less verbose when it comes to Russian science.
Vasyutin's alma mater has not reached mass regeneration of human organs and is still training on animals: local scientists "printed" a mouse thyroid gland on a 3D printer.
However, they are also involved in the study of human organs. According to the head of the Institute of Regenerative Medicine at MSMU Denis Butnar, several years ago the Institute recreated a special engineering design of the buccal mucosa. She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
Image caption,Test specimen of an ear implant exposed to ultraviolet light
In Russia, however, over the past few years, the Italian surgeon-transplantologist Paolo Macchiarini has been practicing - the man who was the first in history to perform an operation on transplanting a synthetic organ - a plastic tube that replaced the patient trachea.
- Paolo Macchiarini: the rise and fall of the famous surgeon
However, seven of his nine patients died, and the breathing tubes implanted in the remaining two subsequently had to be replaced with donor ones.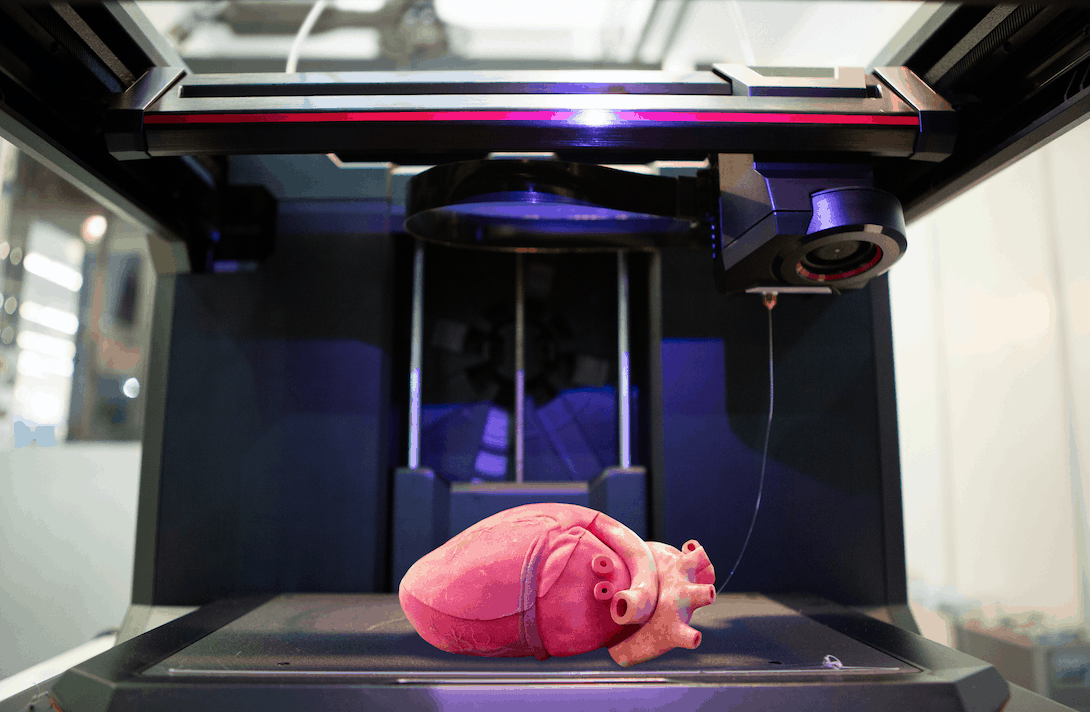
Several criminal cases were brought against him, including on charges of pressure on patients and fraud, and the world's leading doctors called Macchiarini's operations "ethical Chernobyl."
Will printed organs replace donors?
At the zenith of his career, Macchiarini argued that a new perspective is opening up for humanity: you can "print" any human organ on a printer, create an engineering structure from it, enriched with the patient's stem cells, and get the perfect prosthesis.
Be that as it may, complex human organs - the liver, kidneys, heart, lungs - have not yet been grown by any regenerative surgeon.
Bioprinting of the so-called simple organs, however, is already available in the USA, Sweden, Spain and Israel - at the level of clinical trials and special programs.
The US government is actively investing in such programs - in addition to Wake Forest, cooperating with the Pentagon, the Massachusetts Institute of Technology also receives significant amounts to recreate the functioning of the liver, heart and lungs.
Skin application test on a burnt wound
According to Professor Jorge Raquela, a gastroenterologist at the Mayo Clinic Research Center, "Bioprinting is one of the most exciting branches of modern medicine, it has huge potential, and the turning point of the most important discoveries is already close."
Meanwhile, Pete Basillier, head of R&D at analytics firm Gartner, insists technology is advancing much faster than understanding the implications of 3D printing.
Such developments, according to Basilière, even if created with the best of intentions, give rise to a set of questions: what will happen when "improved" organs are created, the basis of which will not only be human cells - will they have "superpowers"? Will a regulatory body be created to monitor their production? Who will check the quality of these organs?
More than 150,000 Americans are on the waiting list for organ transplants every year, according to a report from the US National Library of Medicine.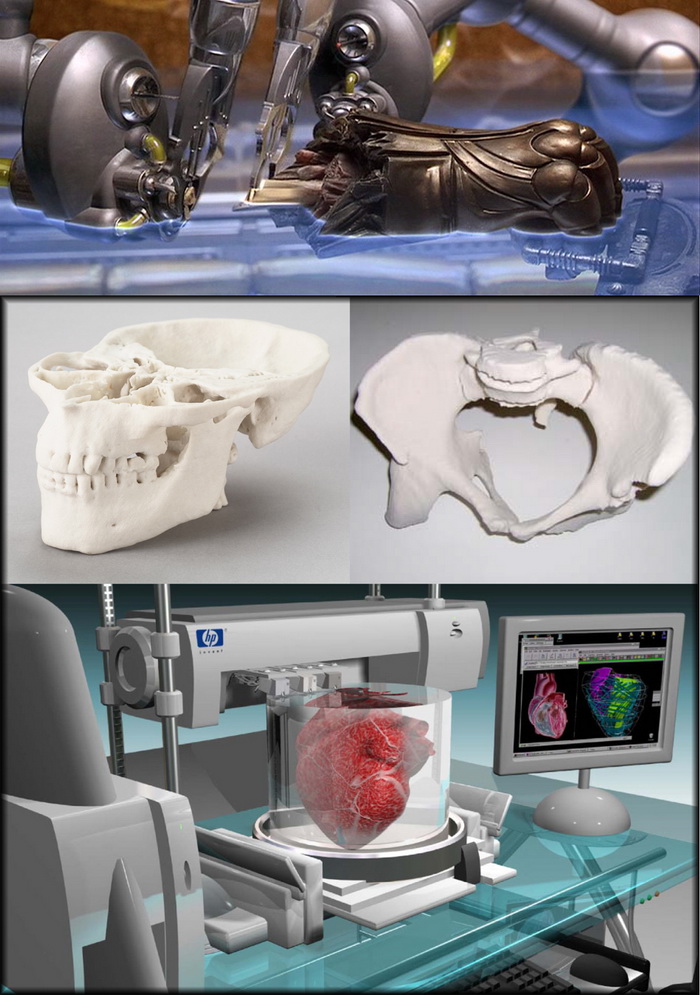 Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
- A 3D printer helped a cyclist who lost his jaw
- Genetically modified pigs - human organ donors?
- The world's first child who received both hands transplanted plays baseball
Most Americans are potential donors: upon obtaining a driver's license, they voluntarily answer the question of whether they agree to donate their organs in the event of a car accident or other dangerous incident . In case of consent, a small "heart" and the word "donor" appear in the corner of the document.
Professor Atala's driver's license is the same - despite all his achievements and faith in the press, he is ready to share his with others.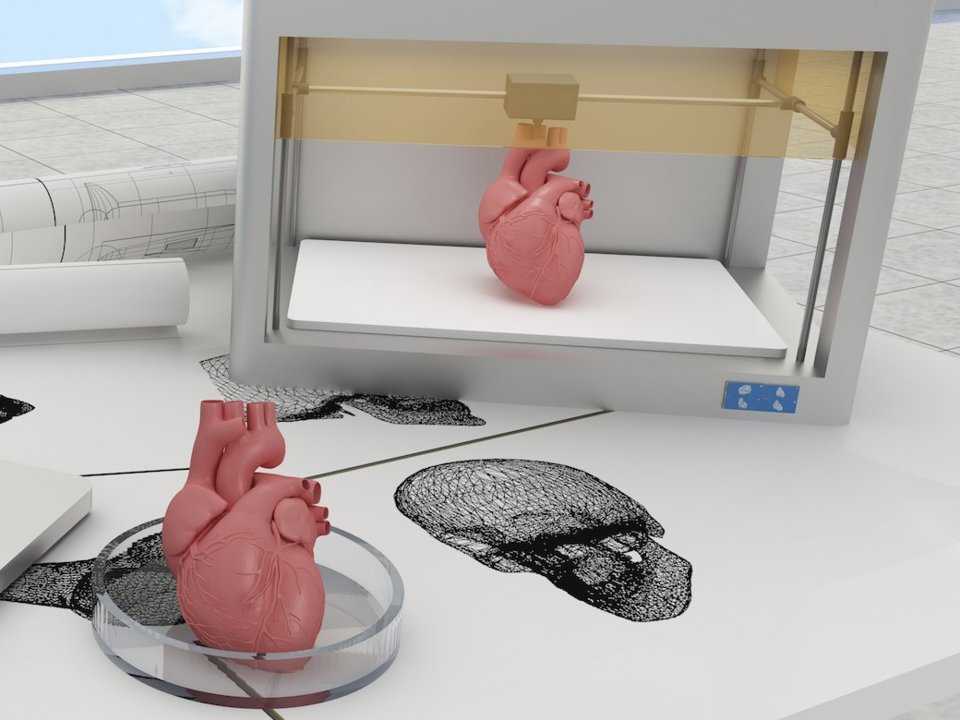
Neither the professor himself, nor his subordinates hide the fact that science is not yet able to "print" organs for thousands of those who need transplantation right now. According to him, it will take several decades to replace donor organs with grown ones at the mass market level.
The work of Atala and others in the field of regenerative medicine remains more probing than mainstream, and still tailored to the individual patient.
The most unexpected things created on a 3D printer
Airplane, ear, rocket engine, food, blood vessels, weapons, building, artificial limbs. And this is not the whole list of things that were created on a 3D printer.
\n\n
Here are the masterpieces of 3D printing technology.
\n\n
Sweets and fast food (Food 3D printers)
\n\n
Cornell University specialists have developed a new technology "Solid Freeform Fabrication", thanks to this technology, Loading hydrogels, which are widely used in the food industry, 3D printer can print chocolate, whipped cream, apple, banana, bread, cheese, biscuit, marshmallow and more.
\n\n
In turn, Los Angeles-based Sugar Lab has demonstrated the ability to 3D print geometric shapes made entirely of sugar, more like works of art than sweets.
\n\n
3D food printers printers work on the same principle as a conventional inkjet printer, only food ingredients are used to “refuel” the printer. A huge list of recipes can be stored in the memory of a food printer and it is possible to add your own. The technology is so promising that NASA awarded a grant to build a printer capable of printing food for astronauts - this will be a real alternative to food from tubes.
\n\n
\n\n
3D Printing Musical Instruments
\n\n
The 3D printer made it possible to create a real violin with amazing sound. South West Music School student Laura gave a showcase performance on CNN using this unique musical instrument.
\n\n
In addition, 3D printing technology allows you to create a unique design of any musical instrument , while maintaining all its functions.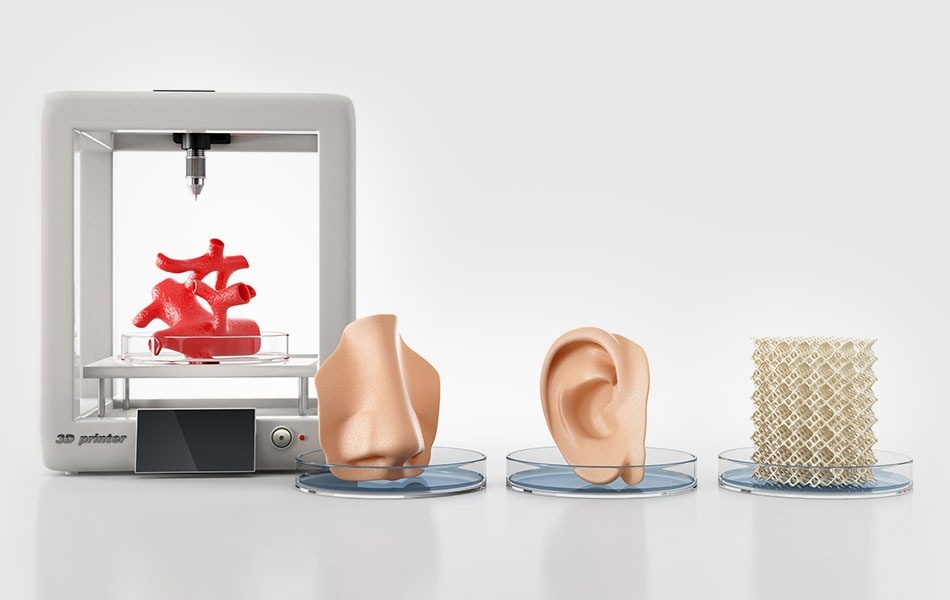
\n\n
\n\n
3D printed weapon
\n\n
University of Texas student Cody Wilson created the first 3D weapon . The Liberator Pistol is made entirely of plastic except for the metal trigger mechanism. The weapon was tested with 380mm bullets.
\n\n
\n\n
Clothes and shoes are now 3D printed
\n\n
Iris Van Herpen (famous Dutch fashion designer) presented her "Tension" collection at Paris Fashion Week, all models of this collection were created using 3D printing technologies.
\n\n
Multiple materials can be used to create a single piece of clothing on a 3D printer, so these items are more durable and elastic.
\n\n
\n\n
Jenna Feasel and Mary Hong (designers at Continuum Studio) created the world's first 3D printed bikini.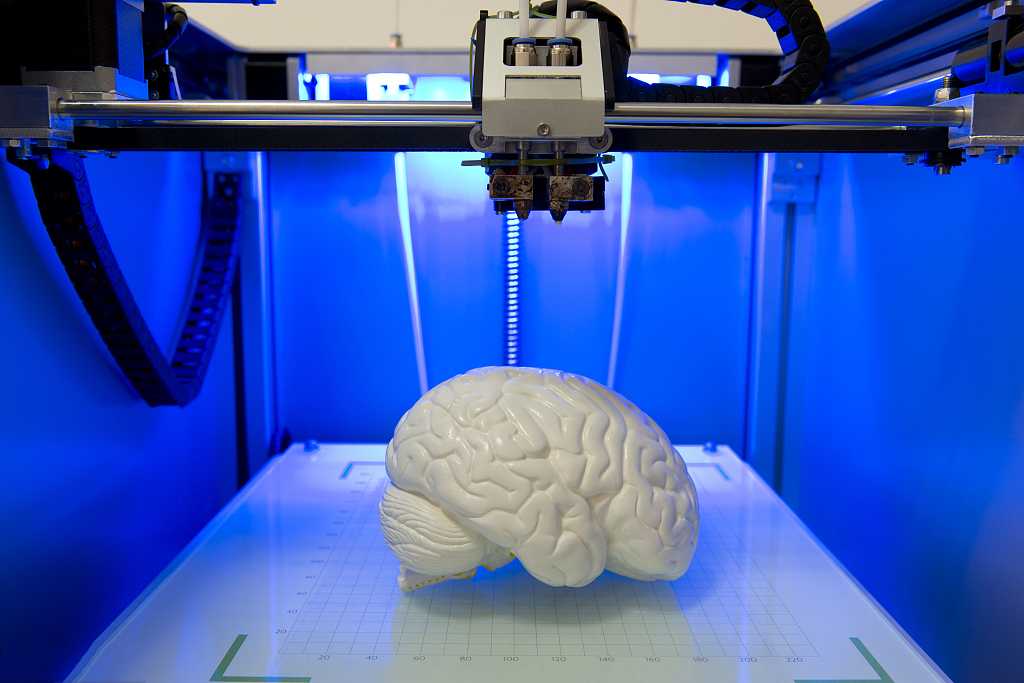 Bikinis are round nylon plates connected by thin springs.
Bikinis are round nylon plates connected by thin springs.
\n\n
In 2011, also appeared the first pair of shoes printed on the 3D printer through the efforts of Swedish students. Today, such three-dimensional shoes are present on the world's leading catwalks. Three-dimensional shoes take into account all the individual characteristics of the future owner, even the shape of the foot. Materials for creating "3D shoes" are rubber, plastic and polyurethane.
\n\n
\n\n
Medicine
\n\n
Bionic ear Calf cells, silver nanoparticles and a polymer gel were used to create a bio-ear. The bio-ear is able to perceive radio waves that are outside the range of human hearing. It is planned that such an ear will be directly connected to the neurons of the brain.
\n\n
\n\n
Own embryo
\n\n
The Japanese company Fasotec can print a 3D model of the baby's fetus based on images from a magnetic resonance imaging scanner - t .
\n\n
\n\n
Stem cells.
\n\n
\n\n
Human organs and tissues
\n\n
By loading organic substances and cell compounds into a 3D printer, it is possible to form tissues of a human organ. In 2011, an experiment was carried out to print a kidney , in 2013, scientists at Oxford University created an analogue of the nervous tissue . In addition, artificial tissues created by 3D technologies do not have a genome, which excludes the process of their rejection by the human body.
\n\n
European clinics use heart model for training to improve the practical skills of surgeons.
\n\n
\n\n
Wheelchairs. Each seat has been created with the individual parameters of the players in mind.
\n\n
\n\n
Reproductions and robots (3D printing of museum exhibits)
\n\n
Using a high-tech scanner and 3D printer , the Smithsonian Research Institute created a reproduction of Thomas Jefferson.
Learn more