3D printing face transplant
World’s First Successful Double Hand and Face Transplant
Materialise’s 3D printing and surgical planning tools provide increased speed and accuracy
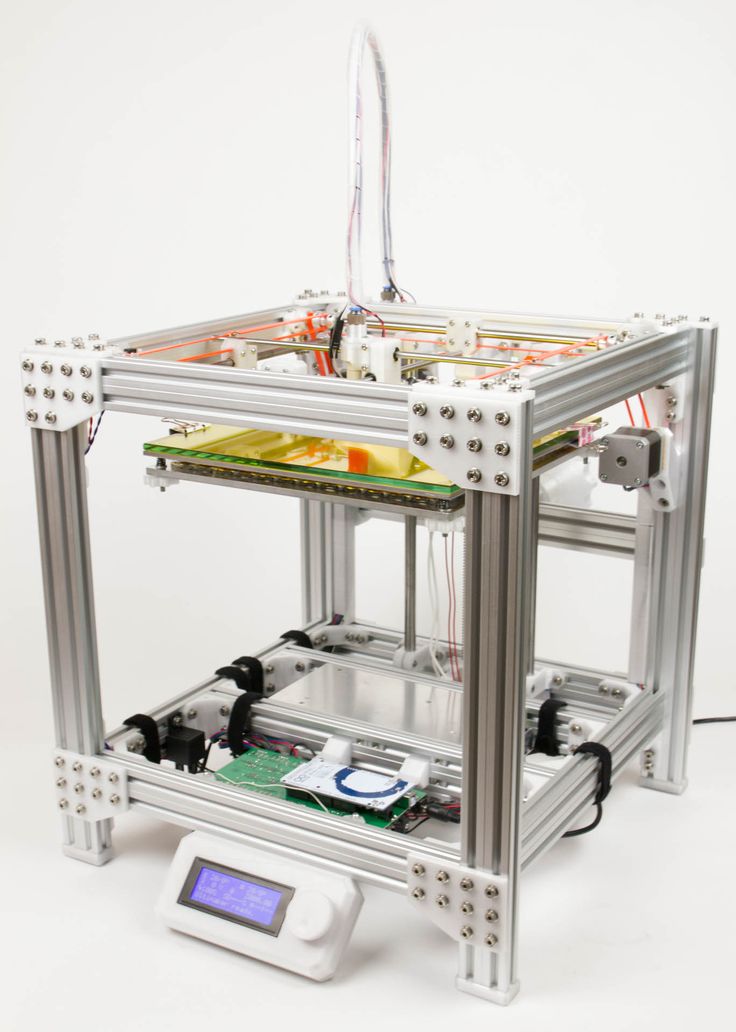
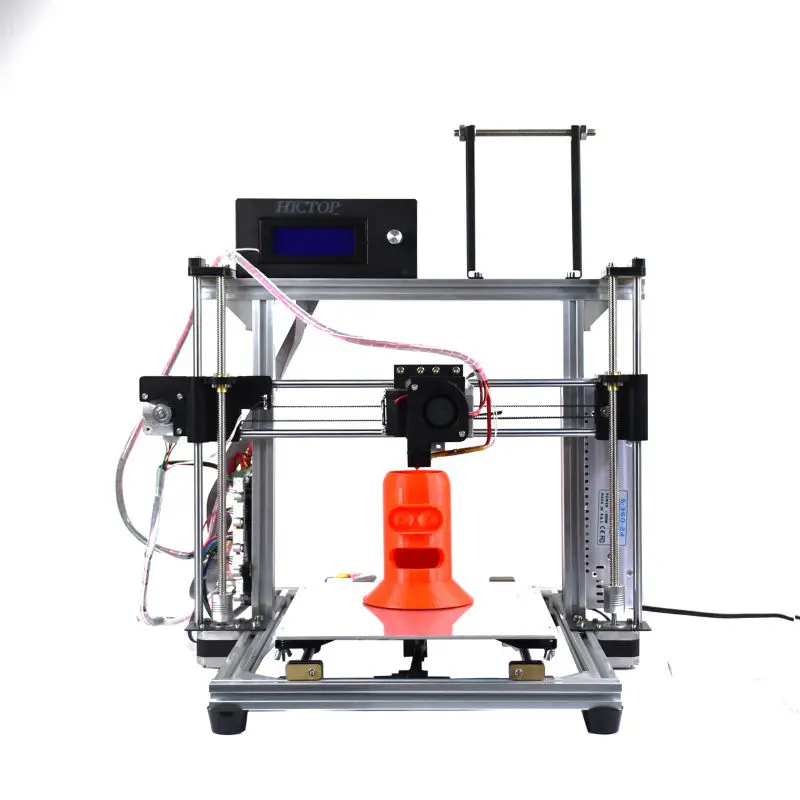
New York - February 3, 2021. 3D technologies, developed by Materialise, played a crucial role in the world’s first simultaneous double hand and face transplant that was successfully performed at NYU Langone Health in Manhattan, NY. Materialise’s innovative 3D planning and printing tools enable the speed and accuracy required for such a complex medical procedure. 3D printed personalized tools such as those used in the double hand and face transplant, are also increasingly common for use in routine surgery, providing surgeons with an additional level of confidence which results in improved patient outcome.
Joe DiMeo before and after the surgery. Image courtesy of NYU Langone.
The 22-year old patient suffered burn wounds resulting from a car accident, leaving him with severe injuries to his face and both arms. He suffered significant damage to his soft tissue, which severely limited his ability to lead a normal life. During a preparation period of 14 months, Materialise clinical engineers formed a cohesive team alongside NYU Langone surgeons, rehearsing the operation in a lab environment to develop and fine-tune the surgical plan. Once a suitable donor was found, the team, led by Dr. Eduardo D. Rodriguez, the Helen L. Kimmel Professor of Reconstructive Plastic Surgery and chair of the Hansjörg Wyss Department of Plastic Surgery at NYU Langone, had only 24 hours to begin the procedure that would improve the patient’s function, appearance and quality of life.
Image-based planning and medical 3D printing have completely revolutionized personalized patient care by providing surgeons with detailed insights and an additional level of confidence before entering the operation room.
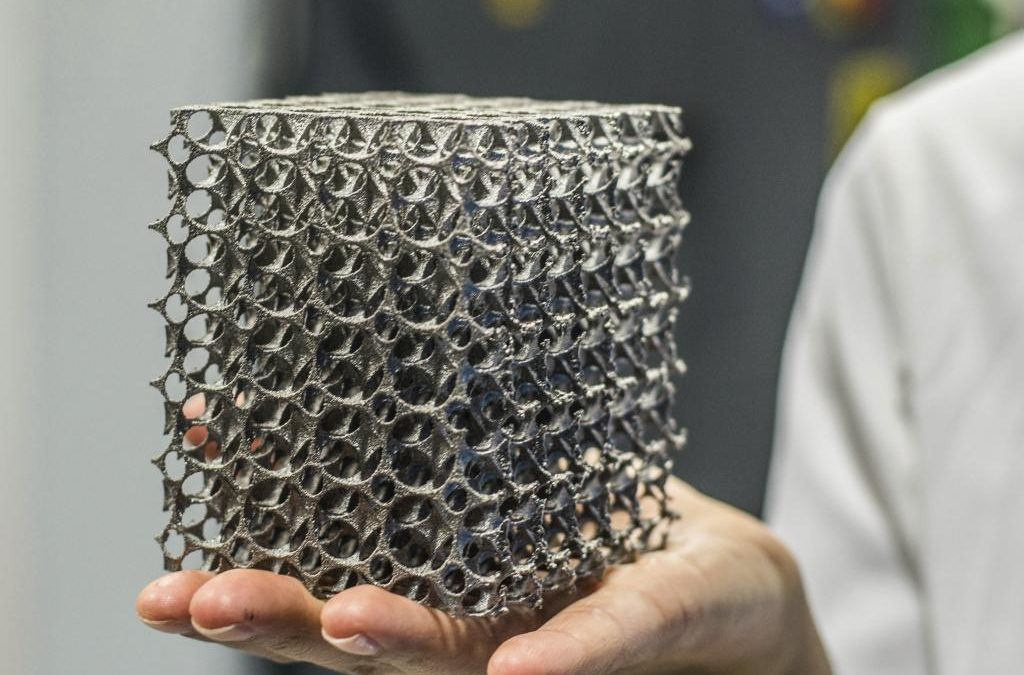
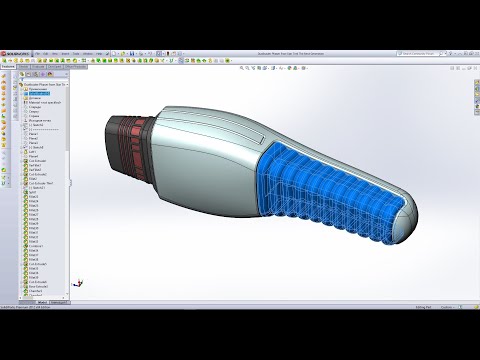
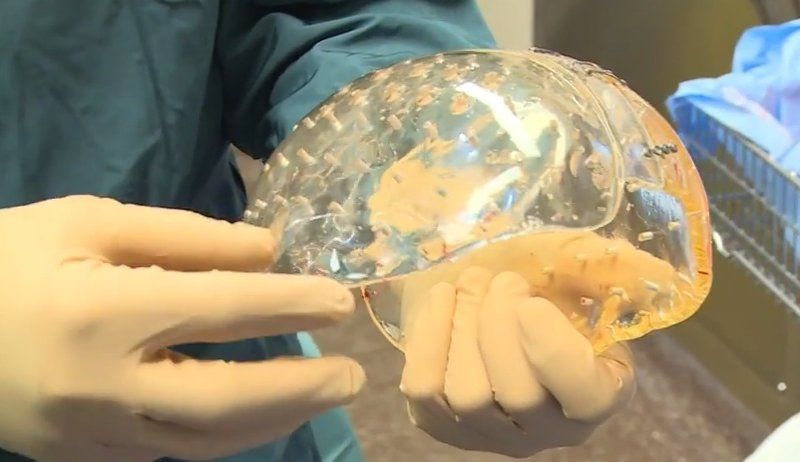
In the months leading up to the surgery Materialise engineers coordinated the development of a surgical plan and created an on-screen 3D model based on CT-scans. This allowed the surgeons and clinical engineers to virtually plan the procedure and visualize different scenarios in three dimensions, creating an in-depth understanding of the anatomical bone structure and determining the optimal surgical flow. Pre-surgical planning also made it possible for surgeons to virtually select and position various medical implants to predict the optimal anatomical fit. Once the surgical plan was finalized, Materialise 3D printed the personalized surgical guides, anatomical models and tools for use during the transplant surgery.
This allowed the surgeons and clinical engineers to virtually plan the procedure and visualize different scenarios in three dimensions, creating an in-depth understanding of the anatomical bone structure and determining the optimal surgical flow. Pre-surgical planning also made it possible for surgeons to virtually select and position various medical implants to predict the optimal anatomical fit. Once the surgical plan was finalized, Materialise 3D printed the personalized surgical guides, anatomical models and tools for use during the transplant surgery.
During this momentous procedure, Rodriguez and his surgical team of sixteen used Materialise’s 3D printed cutting and drilling guides. This fully guided system for bone fragment repositioning and fixation was unique to the patient’s anatomy and helped position the medical tools with great precision, reducing the overall surgery time. Additionally, Materialise created 3D printed sterilizable identification tags for nerves and blood vessels, 3D printed models that were used during donor transport, and 3D printed splints, enabling optimal donor hand position during soft tissue reconstruction.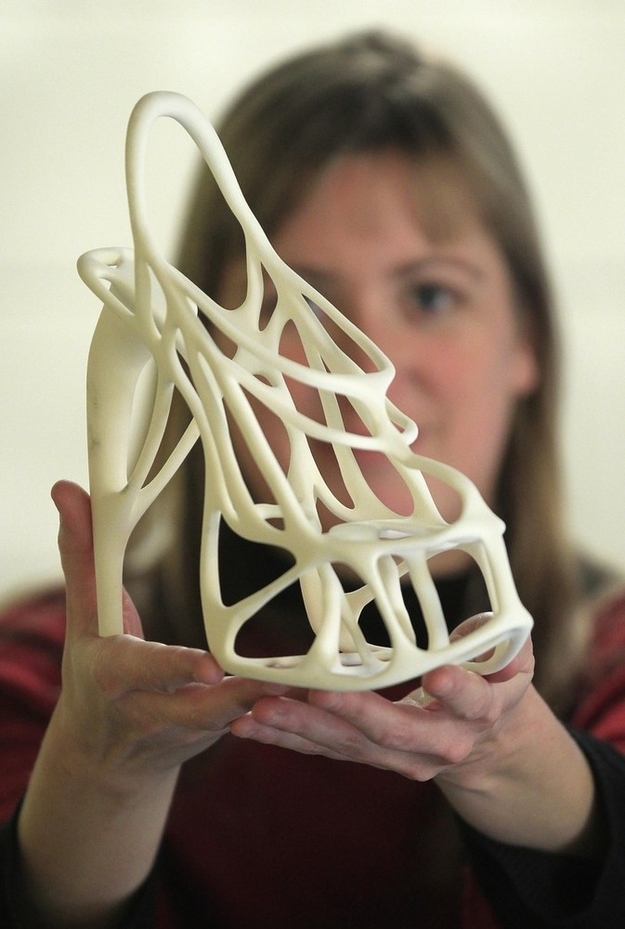
During a preparation period of 14 months, Materialise clinical engineers formed a cohesive team alongside NYU Langone surgeons, rehearsing the operation in a lab environment to develop and fine-tune the surgical plan.
“Complex transplant surgery like this brings together a large team of specialists and presents new and unique challenges”, says Dr. Rodriguez. “This demands careful planning and makes timing, efficiency and accuracy absolutely critical. Virtually planning the surgery in 3D and creating 3D printed, patient-specific tools offers additional insights in the pre-operative phase and increased levels of speed and accuracy during a time-critical surgery”.
“Image-based planning and medical 3D printing have completely revolutionized personalized patient care by providing surgeons with detailed insights and an additional level of confidence before entering the operation room,” says Bryan Crutchfield, Vice President and General Manager – North America. “As a result, leading hospitals are adopting 3D planning and printing services as part of their medical practices because they create a level of predictability that would be impossible to achieve without the use of 3D technologies.”
“As a result, leading hospitals are adopting 3D planning and printing services as part of their medical practices because they create a level of predictability that would be impossible to achieve without the use of 3D technologies.”
Materialise has pioneered many leading medical applications of 3D printing and enables researchers, engineers, and clinicians to develop innovative, personalized treatments that help improve and save lives. The Materialise platform of software and services forms the foundation of certified medical 3D printing in clinical and research environments, offering virtual planning software tools, 3D-printed anatomical models, and personalized surgical guides and implants.
About Materialise
Materialise incorporates three decades of 3D printing experience into a range of software solutions and 3D printing services, which together form the backbone of the 3D printing industry. Materialise’s open and flexible solutions enable players in a wide variety of industries, including healthcare, automotive, aerospace, art and design, and consumer goods, to build innovative 3D printing applications that aim to make the world a better and healthier place.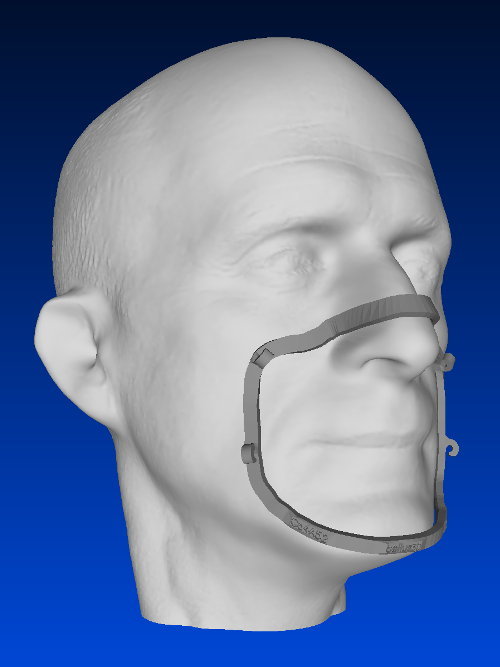 Headquartered in Belgium, with branches worldwide, Materialise combines the largest group of software developers in the industry with one of the largest 3D printing facilities in the world.
Headquartered in Belgium, with branches worldwide, Materialise combines the largest group of software developers in the industry with one of the largest 3D printing facilities in the world.
L-101788
Materialise press contact
Nils Torke
Email: [email protected]
[email protected]
Twitter: @MaterialiseNV
Pictures:
During a preparation period of 14 months, Materialise clinical engineers formed a cohesive team alongside NYU Langone surgeons, rehearsing the operation in a lab environment to develop and fine-tune the surgical plan.
Materialise engineers coordinated the development of a surgical plan and created an on-screen 3D model based on CT-scans.
Pre-surgical planning made it possible for surgeons to virtually select and position various medical implants to predict the optimal anatomical fit.
A fully guided system for bone fragment repositioning and fixation was unique to the patient’s anatomy and helped position the medical tools with great precision, reducing the overall surgery time.
Mixed Reality and 3D Printed Models for Planning and Execution of Face Transplantation
. 2021 Dec 1;274(6):e1238-e1246.
doi: 10.1097/SLA.0000000000003794.
Ki-Hyun Cho 1 , Francis A Papay 1 , Jeff Yanof 2 , Karl West 2 , Bahar Bassiri Gharb 1 , Antonio Rampazzo 1 , Brian Gastman 1 , Graham S Schwarz 1
Affiliations
Affiliations
- 1 Department of Plastic Surgery, Cleveland Clinic Foundation, Cleveland, OH.

- 2 Department of Biomedical Engineering, Lerner Research Institute, Cleveland Clinic Foundation, Cleveland, OH.
- PMID: 32224738
- DOI: 10.1097/SLA.0000000000003794
Ki-Hyun Cho et al. Ann Surg. .
. 2021 Dec 1;274(6):e1238-e1246.
doi: 10.1097/SLA.0000000000003794.
Authors
Ki-Hyun Cho 1 , Francis A Papay 1 , Jeff Yanof 2 , Karl West 2 , Bahar Bassiri Gharb 1 , Antonio Rampazzo 1 , Brian Gastman 1 , Graham S Schwarz 1
Affiliations
- 1 Department of Plastic Surgery, Cleveland Clinic Foundation, Cleveland, OH.

- 2 Department of Biomedical Engineering, Lerner Research Institute, Cleveland Clinic Foundation, Cleveland, OH.
- PMID: 32224738
- DOI: 10.1097/SLA.0000000000003794
Abstract
Objective: The aim of this study was to evaluate a novel holographic craniofacial surgical planning application and its implementation throughout the planning and operative stages of facial transplantation by performing a critical analysis of comparative utility, cost, and limitations of MR and 3D printing.
Summary of background data: Face transplantation is a highly complex form of craniofacial reconstruction requiring significant planning, knowledge of patient-specific spatial relationships, and time-sensitive decision making.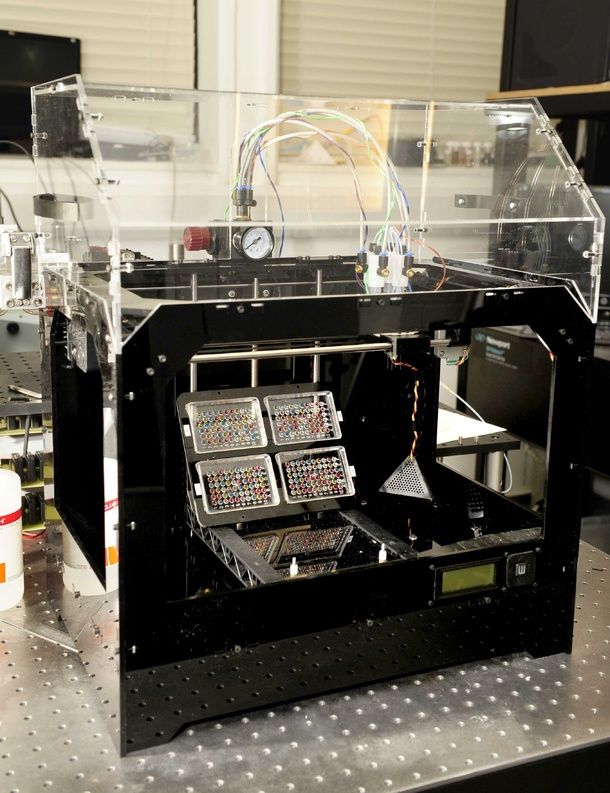 Computer-aided 3D modeling has improved efficiency and outcomes of complex craniofacial reconstruction by enabling virtual surgical planning and 3D printed model generation. MR technology can enhance surgical planning, improve visualization, and allow manipulation of virtual craniofacial biomodels within the operative field.
Computer-aided 3D modeling has improved efficiency and outcomes of complex craniofacial reconstruction by enabling virtual surgical planning and 3D printed model generation. MR technology can enhance surgical planning, improve visualization, and allow manipulation of virtual craniofacial biomodels within the operative field.
Methods: Accounting for the time-sensitive nature of face transplantation, a unique, highly coordinated workflow for image acquisition and processing was designed to facilitate rapid holographic rendering and 3D printing. During recent face transplantation, both holographic and 3D printed models were utilized, and the time and cost of fabrication were compared.
Results: Holographic models required less time and cost for fabrication. They provided both comprehensive visualization of 3D spatial relationships and novel means to perform VSP and virtual face transplantation by interacting with and manipulating patient-specific, anatomic holograms.
Conclusion: Time efficiency, low-cost biomodel production, provision of unlimited preoperative surgical rehearsal, and potential for intraoperative surgical guidance makes holographic VSP and MR highly promising technology for use in complex craniofacial surgery.
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Conflict of interest statement
The authors report no conflicts of interest.
Similar articles
-
Customized "In-Office" Three-Dimensional Printing for Virtual Surgical Planning in Craniofacial Surgery.
Mendez BM, Chiodo MV, Patel PA. Mendez BM, et al. J Craniofac Surg. 2015 Jul;26(5):1584-6.
 doi: 10.1097/SCS.0000000000001768. J Craniofac Surg. 2015. PMID: 26106998
doi: 10.1097/SCS.0000000000001768. J Craniofac Surg. 2015. PMID: 26106998 -
Three-dimensional Printing and Augmented Reality: Enhanced Precision for Robotic Assisted Partial Nephrectomy.
Wake N, Bjurlin MA, Rostami P, Chandarana H, Huang WC. Wake N, et al. Urology. 2018 Jun;116:227-228. doi: 10.1016/j.urology.2017.12.038. Epub 2018 May 22. Urology. 2018. PMID: 29801927
-
3D mixed reality holograms for preoperative surgical planning of nephron-sparing surgery: evaluation of surgeons' perception.
Checcucci E, Amparore D, Pecoraro A, Peretti D, Aimar R, DE Cillis S, Piramide F, Volpi G, Piazzolla P, Manfrin D, Manfredi M, Fiori C, Porpiglia F. Checcucci E, et al. Minerva Urol Nephrol. 2021 Jun;73(3):367-375.
 doi: 10.23736/S2724-6051.19.03610-5. Epub 2019 Sep 5. Minerva Urol Nephrol. 2021. PMID: 31486325
doi: 10.23736/S2724-6051.19.03610-5. Epub 2019 Sep 5. Minerva Urol Nephrol. 2021. PMID: 31486325 -
Applications of three-dimensional surgical planning in facial feminization surgery: A systematic review.
Escandón JM, Morrison CS, Langstein HN, Ciudad P, Del Corral G, Manrique OJ. Escandón JM, et al. J Plast Reconstr Aesthet Surg. 2022 Jul;75(7):e1-e14. doi: 10.1016/j.bjps.2022.02.073. Epub 2022 Mar 7. J Plast Reconstr Aesthet Surg. 2022. PMID: 35400593 Review.
-
Virtual Surgical Planning (VSP) in Craniomaxillofacial Reconstruction.
Vyas K, Gibreel W, Mardini S. Vyas K, et al. Facial Plast Surg Clin North Am. 2022 May;30(2):239-253. doi: 10.1016/j.fsc.2022.01.016. Facial Plast Surg Clin North Am.
 2022. PMID: 35501062 Review.
2022. PMID: 35501062 Review.
See all similar articles
Cited by
-
Review and Future/Potential Application of Mixed Reality Technology in Orthopaedic Oncology.
Wong KC, Sun YE, Kumta SM. Wong KC, et al. Orthop Res Rev. 2022 May 16;14:169-186. doi: 10.2147/ORR.S360933. eCollection 2022. Orthop Res Rev. 2022. PMID: 35601186 Free PMC article. Review.
-
The 2020 Facial Transplantation Update: A 15-Year Compendium.
Diep GK, Berman ZP, Alfonso AR, Ramly EP, Boczar D, Trilles J, Rodriguez Colon R, Chaya BF, Rodriguez ED. Diep GK, et al. Plast Reconstr Surg Glob Open. 2021 May 21;9(5):e3586. doi: 10.1097/GOX.0000000000003586. eCollection 2021 May. Plast Reconstr Surg Glob Open.
 2021. PMID: 34036025 Free PMC article.
2021. PMID: 34036025 Free PMC article. -
Novel Multimodal, Multiscale Imaging System with Augmented Reality.
Mela C, Papay F, Liu Y. Mela C, et al. Diagnostics (Basel). 2021 Mar 4;11(3):441. doi: 10.3390/diagnostics11030441. Diagnostics (Basel). 2021. PMID: 33806547 Free PMC article.
References
-
- Jacobs JMS, Dec W, Levine JP, et al. Best face forward: virtual modeling and custom device fabrication to optimize craniofacial vascularized composite allotransplantation. Plast Reconstr Surg 2013; 131:64–70.
-
- Mehra P, Miner J, D’Innocenzo R, et al. Use of 3-D stereolithographic models in oral and maxillofacial surgery.
 J Maxillofac Oral Surg 2011; 10:6–13.
J Maxillofac Oral Surg 2011; 10:6–13.
- Mehra P, Miner J, D’Innocenzo R, et al. Use of 3-D stereolithographic models in oral and maxillofacial surgery.
-
- Sosin M, Ceradini DJ, Hazen A, et al. Total face, eyelids, ears, scalp, and skeletal subunit transplant cadaver simulation: the culmination of aesthetic, craniofacial, and microsurgery principles. Plast Reconstr Surg 2016; 137:205–219.
-
- Dorafshar AH, Brazio PS, Mundinger GS, et al. Found in space: computer-assisted orthognathic alignment of a total face allograft in six degrees of freedom. J Oral Maxillofac Surg 2014; 72:1788–1800. doi:10.1016/j.joms.2014.01.016. - DOI
-
- Cignoni P, Callieri M, Corsini M, et al.
 MeshLab: an open-source mesh processing tool. Eurographics Ital Chapter Conf 2008; 129–136.
MeshLab: an open-source mesh processing tool. Eurographics Ital Chapter Conf 2008; 129–136.
- Cignoni P, Callieri M, Corsini M, et al.
Publication types
MeSH terms
3D Printing: Improving Face Transplantation
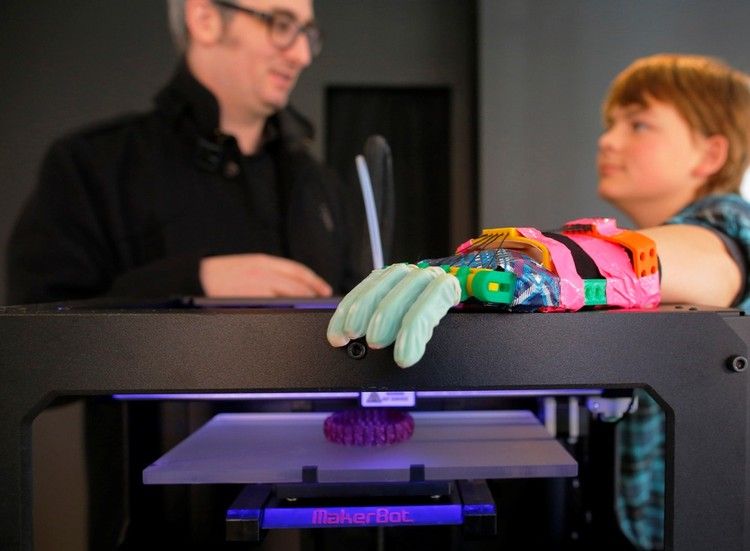
Surgeons have begun using new, high-precision 3D printers for face transplant surgery, allowing for faster procedures and better results.
The model of the face obtained with this printer helps to create bone grafts, metal plates and basic skull bones for grafting. This allows you to plan the operation, which in turn helps to reduce the time of the operation, according to FoxNews.
The new technique has already been used in face transplantation of several patients, including in two difficult cases. In the first case, in 2013, the face of Carmen Tarleton, who was crippled by her husband, was restored.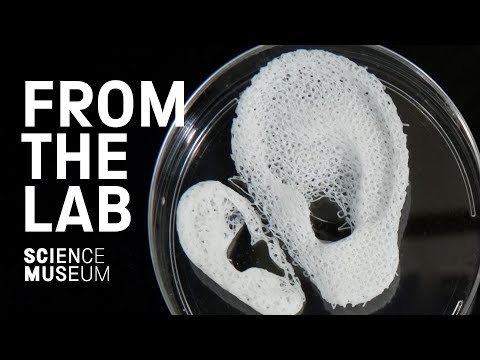 The second was a full face transplant for Dallas Vince, the first person in the United States to receive a full face transplant in 2011. These operations radically change the patient's life for the better.
The second was a full face transplant for Dallas Vince, the first person in the United States to receive a full face transplant in 2011. These operations radically change the patient's life for the better.
During these and several other operations, in addition to cosmetic problems, the ability to speak, breathe and eat was also restored, said Frank Ribiki, a doctor at the Women's Hospital in Boston, radiologist Frank Ribiki. He presented his observations at a general meeting of North American radiologists on December 1.
For patients, face transplantation is the end of a long-term treatment. “Before getting a face transplant, patients go through a lot of operations in order to survive,” recalled Dr. Ribiki.
This means that patients may have plates, screws, bone grafts, and other minor changes to the facial area, and yet the new face must be perfect. 3D printing allows employees to see changes in real time, helping to turn a normally 25-hour operation into a quick and fluid intervention.
The staff imprinted the soft tissues of Tarleton's face, which her husband sprinkled with lye on her face. Ribiki said that the lye completely burned the skin and soft tissues of the face to the very bones. “Soft tissue printing is done using special technologies, without a 3D printer it is quite difficult to get the right idea about them,” Ribiki commented.
Tarleton has improved since the operation in 2011. The new facial features became familiar to her, Ribiki said. The tissues have undergone significant restructuring and her face is now unlike both her previous face and that of the donor. According to Ribica's assessment, 3 years after the operation, looking at her face, it is impossible to even assume a face transplant.
Bryan Women's Hospital Plastic Surgeon Dr. Edward Caterson believes that a deeper understanding of the anatomy of the face will also help with minor facial reconstructions and lead to better outcomes.
For example, if the jaw bone is damaged, doctors usually take a small piece of leg or rib bone and grow it back. Since the tibia is straight, it is impossible to get an exact copy of the jaw. 3D printing gets the job done right, Carerson said.
Since the tibia is straight, it is impossible to get an exact copy of the jaw. 3D printing gets the job done right, Carerson said.
“We are getting new opportunities in surgical practice, in fact, some actions can be performed in the preoperative period,” he said.
3D printing allowed Caterson to assemble a jaw from a thigh bone. Doctors have long used the technology of increasing the jaw from the rib bone, but since it is deprived of blood supply, after a while the new jaw is destroyed and a new operation is needed. 3D modeling allows the use of the femur, which has its own blood supply.
Source
90,000 Press: how to make ears, skin and noses- Natalka Pisnya
- Russian service BBC, USA
Subscribe to our newsletter "Context": it will help you understand the events.
Image copyright, Masela family archive
Photo caption, Luc Masela with his parents one month after the artificial bladder transplant. year 2001.
year 2001.
Luc Masela, now 27, is an athlete with a degree in economics, works for a large exhibition company, travels a lot and recently met, in his words, "the most beautiful girl in the world." Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
Luke was born with spina bifida - and although he was able to walk, his bladder was severely damaged. By the age of 10, he almost did not leave hospitals: due to improper functioning of the bladder, fluid began to return to the boy's kidneys, doctors diagnosed an irreversible pathology of the organ.
You need to enable JavaScript or use a different browser to view this content
Video caption, "3D printed" organs are already here intestinal segment. This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
The urologist who was taking care of the boy invited the Masela family to take part in an experimental program: to grow a new bladder from his own cells. Then, in 2001, it sounded like science fiction: only nine people took part in the program before Luke. Despite this, his family agreed.
"The essence of the operation was reduced to two stages: first, a piece of bladder tissue was taken from me, and over the next two months, cells were grown in the laboratory in order to grow a new healthy bladder from them," says Luke.
Photo copyright, Masela family archive
Photo caption,Luc Masela, 17 years after the artificial bladder transplant
Then came the transplant, which he said took 16 hours. “I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.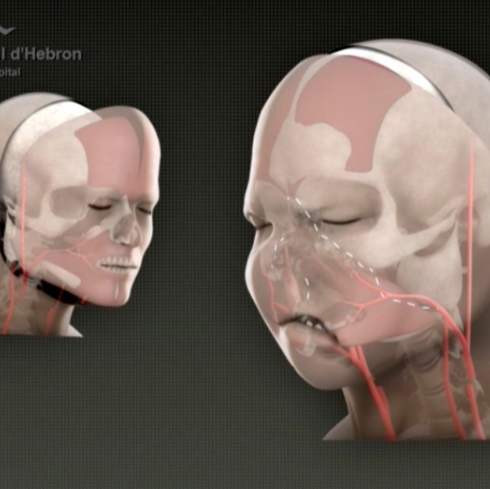
The operation was performed by Dr. Anthony Atala, Pediatric Regenerative Surgeon. In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like a normal organ, taking root thanks to Luke’s own cells.
- An animal capable of regrowing its head
- The birth of a chimera: why do scientists need a human-animal hybrid?
- Swedish company 3D prints body parts
Luke and Dr. Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.
The professor took charge of the Wake Forest Institute of Regenerative Medicine in North Carolina in those 10 years, but he never forgot about Luke: his bladder was one of the most challenging and most successful projects in his early practice.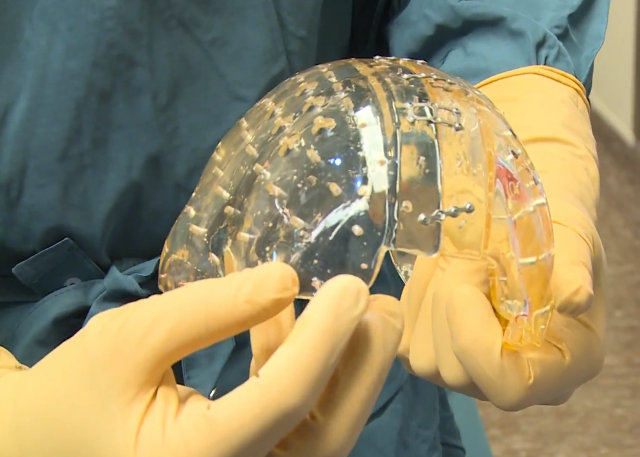
By 2018, Atala won the Christopher Columbus Award for "work on a discovery that will have a significant impact on society"; The Times and Scientific American magazines at various times named him "Doctor of the Year", he was also recognized as "one of the 50 scientists on the planet who in the next 10 years will change the way we live and work."
How to print a new face
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
In the mid-2000s, Atala's team turned their attention to an ordinary household 3D printer and wrote special software for it, later specialized machines were created for the laboratory. Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
One of the team's latest achievements is ears and noses grown outside the human body.
The main customer and sponsor of Atala's developments is the US Department of Defense, and many of the patients are military victims of military operations.
It works like this: first, a CT scan of the ear or nose is done. One of Atala's assistants, Joshua Corpus, jokes that at this stage, people often ask to "improve" the shape of the nose if they thought theirs was too wide or hooked, and the ears if they were too wide.
After that, a special computer code is written, and the printing of the basis of the organs begins.
For this, a bioresorbable polymer, polycaprolactam, is used. At the same time flexible and durable, in the human body it disintegrates within four years.
After printing, the layers of polycaprolactam resemble lace; after transplantation, their place will be taken by a person's own cartilage tissue in a few years.
Polycaprolactam is then saturated with a gel created from the patient's cells, cooled to -18 degrees Celsius - so the cells, according to scientists, are not damaged, they are "alive and happy."
Image caption,Printing a test kidney sample on a bioprinter
In order for the polymer and gel structure to take shape and become something more durable, ultraviolet light is used in the laboratory - it does not damage cells.
The future implant is printed for 4-5 hours, then it is finally formed and inserted under the epidermis.
Skin can also be grown: children affected by fires were the first to participate in the early trials of Atala - after the "printing" of the skin, scientists monitored patients for several more years. The new skin did not crack, did not burst, and grew with the children.
The most difficult work, according to the scientist, is facial wounds: it is not enough just to stretch the skin, you need to accurately calculate the geometry, align the swelling, the structure of the bones, and understand how a person will look after that.
In addition to the skin and ears, Atala can "print" the bones of the jaws, grow blood vessels and cells of some organs - the liver, kidneys, lungs.
This technology is especially appreciated by oncologists: on the basis of patient cells, it is possible to recreate the body's response to various types of chemotherapy and observe the reaction to a particular type of treatment in the laboratory, and not on a living person.
But the liver, kidneys, lungs and heart are still being tested. Atala says he raised them in miniature, but creating organs from various tissues to real size requires a lot of additional research.
But, according to him, cells were grown in the laboratory and a vagina was created for a girl who was born several years ago with a congenital deformity of the genital organs - several years have passed since the transplant.
Image caption,Bioprinted polycaprolactam ear implant base
Atala smiles and adds that his team is also working on a working penis. This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
Among others, Igor Vasyutin, a Russian post-graduate student of the First Moscow State Medical University (MSMU) named after Sechenov, is working on this under laboratory conditions. He is a cell biologist, Atala's right hand.
Vasyutin has been in the USA for about a year - he came on an exchange. He is ready to talk about the behavior of stem cells for hours, but becomes less verbose when it comes to Russian science.
Vasyutin's alma mater has not reached mass regeneration of human organs and is still training on animals: local scientists "printed" a mouse thyroid gland on a 3D printer.
However, they are also involved in the study of human organs. According to the head of the Institute of Regenerative Medicine at MSMU Denis Butnar, several years ago the Institute recreated a special engineering design of the buccal mucosa. She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
Test specimen of an ear implant exposed to ultraviolet light
In Russia, however, over the past few years, the Italian surgeon-transplantologist Paolo Macchiarini has been practicing, the man who was the first in history to perform a synthetic organ transplantation operation - a plastic tube that replaced the patient trachea.
- Paolo Macchiarini: the rise and fall of the famous surgeon
However, seven of his nine patients died, and the breathing tubes implanted in the remaining two subsequently had to be replaced with donor ones.
Several criminal cases were brought against him, including on charges of pressure on patients and fraud, and the world's leading doctors called Macchiarini's operations "ethical Chernobyl."
Will printed organs replace donors?
At the zenith of his career, Macchiarini argued that a new perspective is opening up for humanity: you can "print" any human organ on a printer, create an engineering structure from it, enriched with the patient's stem cells, and get the perfect prosthesis.
Be that as it may, complex human organs - the liver, kidneys, heart, lungs - have not yet been able to grow any regenerative surgeon.
Bioprinting of the so-called simple organs, however, is already available in the US, Sweden, Spain and Israel - at the level of clinical trials and special programs.
The US government is actively investing in such programs - in addition to Wake Forest, cooperating with the Pentagon, the Massachusetts Institute of Technology also receives significant amounts to recreate the work of the liver, heart and lungs.
Image caption,Skin application test on a burnt wound
According to Professor Jorge Raquela, a gastroenterologist at the Mayo Clinic Research Center, "Bioprinting is one of the most exciting branches of modern medicine, it has huge potential, and the turning point of the most important discoveries is already close."
Meanwhile, Pete Basillier, head of R&D at analytics firm Gartner, insists technology is advancing much faster than understanding the implications of 3D printing.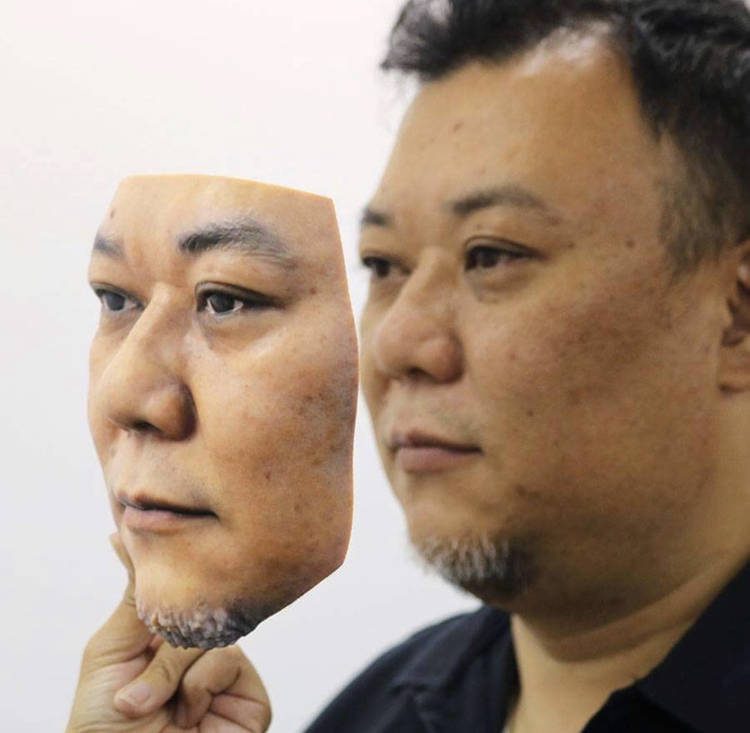
Such developments, according to Basilière, even if created with the best of intentions, give rise to a set of questions: what will happen when "improved" organs are created, the basis of which will not only be human cells - will they have "superpowers"? Will a regulatory body be created to monitor their production? Who will check the quality of these organs?
More than 150,000 Americans are on the waiting list for organ transplants each year, according to a report from the US National Library of Medicine. Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
- A 3D printer helped a cyclist who lost his jaw
- Genetically modified pigs - human organ donors?
- The world's first child with both hands transplanted plays baseball
Most Americans are potential donors: upon obtaining a driver's license, they voluntarily answer the question of whether they agree to donate their organs in the event of a car accident or other dangerous incident .