3D printed ovary
3-D printed ovaries produce healthy offspring
Bioprosthetic ovaries produced mouse pups in otherwise infertile mice
May 16, 2017 | By Kristin Samuelson
- Feinberg School of Medicine
- McCormick
- Women’s Health
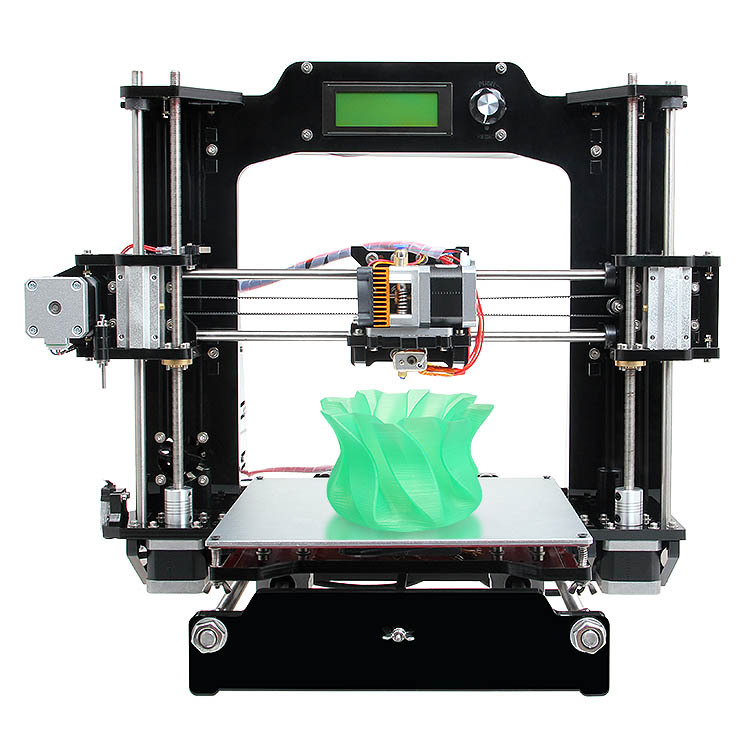
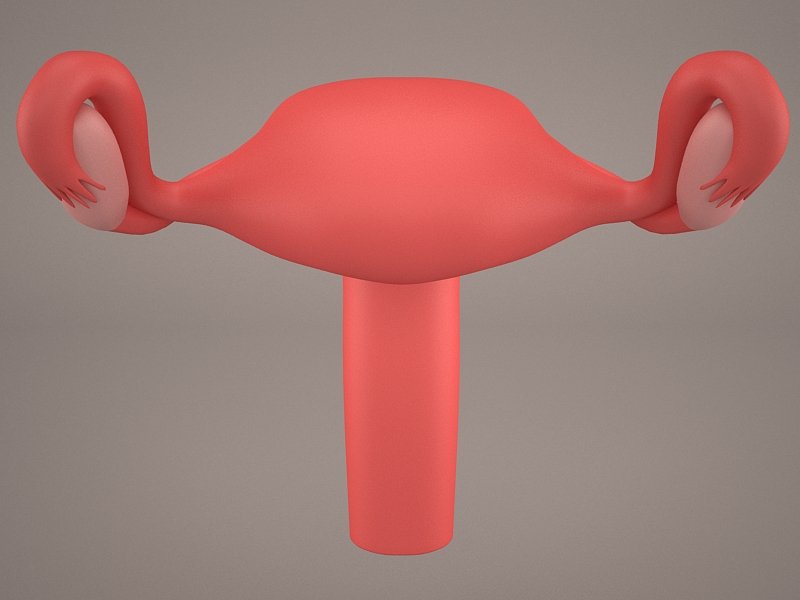
CHICAGO - The new world of 3-D printed organs now includes implanted ovary structures that, true to their design, actually ovulate, according to a study by Northwestern University Feinberg School of Medicine and McCormick School of Engineering.
By removing a female mouse’s ovary and replacing it with a bioprosthetic ovary, the mouse was able to not only ovulate but also give birth to healthy pups. The moms were even able to nurse their young.
The holy grail of bioengineering for regenerative medicine”
Teresa K.Director of the Women's Health Research Institute
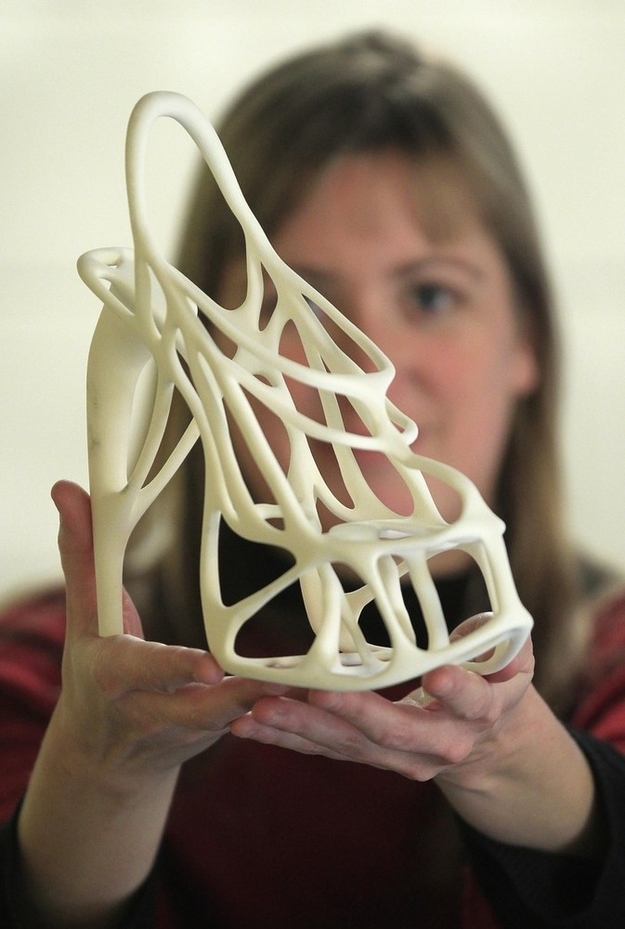
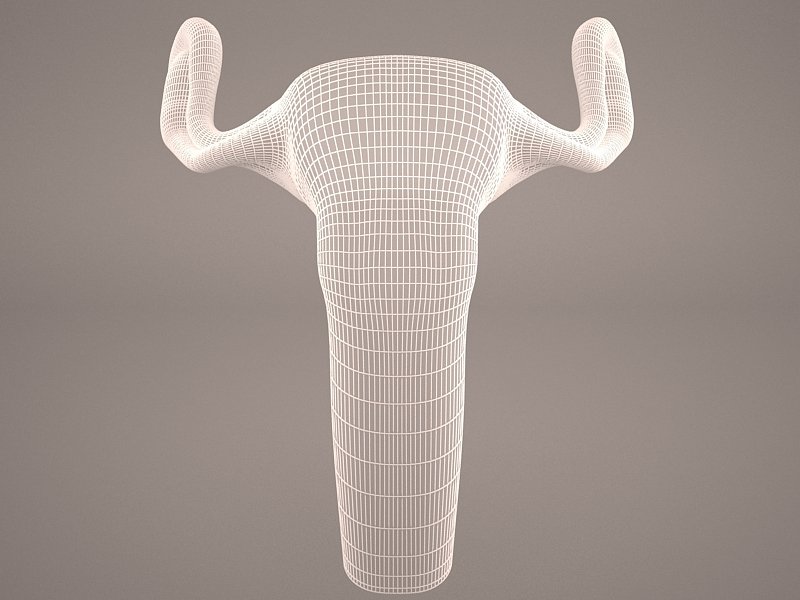
The bioprosthetic ovaries are constructed of 3-D printed scaffolds that house immature eggs, and have been successful in boosting hormone production and restoring fertility in mice, which was the ultimate goal of the research.
“This research shows these bioprosthetic ovaries have long-term, durable function,” said Teresa K. Woodruff, a reproductive scientist and director of the Women’s Health Research Institute at Feinberg. “Using bioengineering, instead of transplanting from a cadaver, to create organ structures that function and restore the health of that tissue for that person, is the holy grail of bioengineering for regenerative medicine.”
The paper was published today, May 16, in Nature Communications.
How is this research different from other 3-D printed structures?
What sets this research apart from other labs is the architecture of the scaffold and the material, or “ink,” the scientists are using, said Ramille Shah, assistant professor of materials science and engineering at McCormick and of surgery at Feinberg.
That material is gelatin, which is a biological hydrogel made from broken-down collagen that is safe to use in humans. The scientists knew that whatever scaffold they created needed to be made of organic materials that were rigid enough to be handled during surgery and porous enough to naturally interact with the mouse’s body tissues.
“Most hydrogels are very weak, since they’re made up of mostly water, and will often collapse on themselves,” Shah said. “But we found a gelatin temperature that allows it to be self-supporting, not collapse, and lead to building multiple layers. No one else has been able to print gelatin with such well-defined and self-supported geometry.”
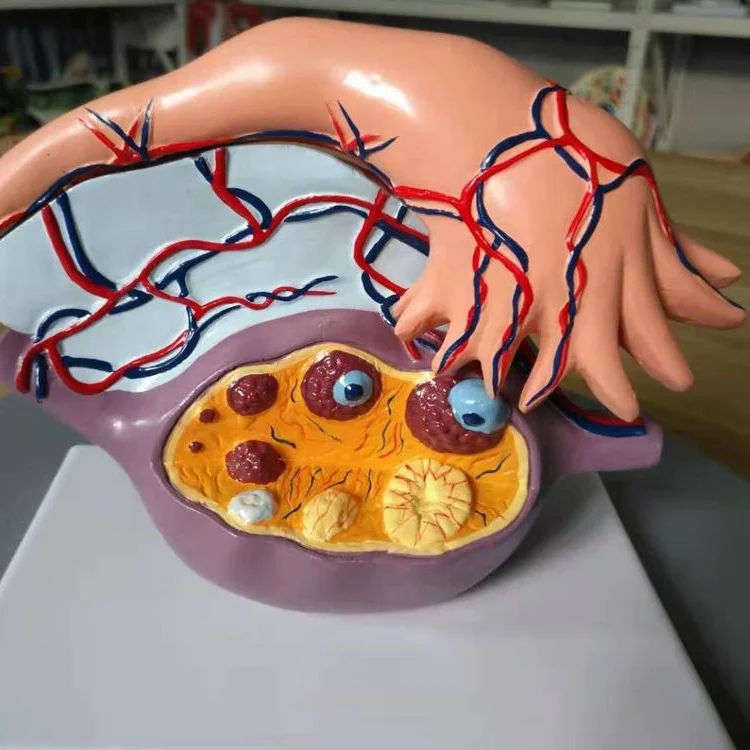
That geometry directly links to whether or not the ovarian follicles, organized hormone-producing support cells surrounding an immature egg cell, will survive in the ovary, which was one of the bigger findings in the study.
“This is the first study that demonstrates that scaffold architecture makes a difference in follicle survival,” Shah said. “We wouldn’t be able to do that if we didn’t use a 3-D printer platform.”
“We wouldn’t be able to do that if we didn’t use a 3-D printer platform.”
How does this impact humans?
The scientists’ sole objective for developing the bioprosthetic ovaries was to help restore fertility and hormone production in women who have undergone adult cancer treatments or those who survived childhood cancer and now have increased risks of infertility and hormone-based developmental issues.
“What happens with some of our cancer patients is that their ovaries don’t function at a high enough level and they need to use hormone replacement therapies in order to trigger puberty,” said Monica Laronda, co-lead author of this research and a former post-doctoral fellow in the Woodruff lab. “The purpose of this scaffold is to recapitulate how an ovary would function. We’re thinking big picture, meaning every stage of the girl’s life, so puberty through adulthood to a natural menopause.”
Laronda is now an assistant professor at the Stanley Manne Children’s Research Institute at the Ann & Robert H. Lurie Children’s Hospital.
Lurie Children’s Hospital.
Additionally, the successful creation of 3-D printed implants to replace complex soft tissue could significantly impact future work in soft tissue regenerative medicine.
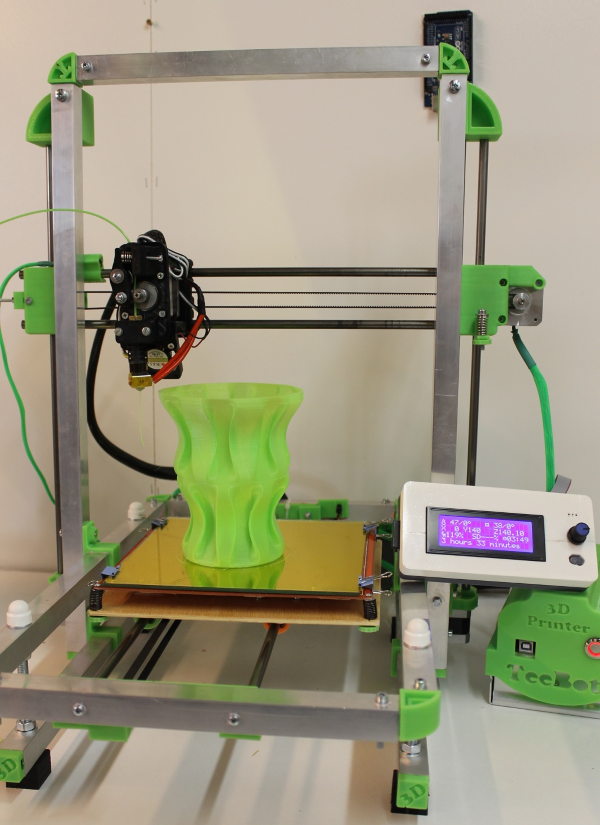
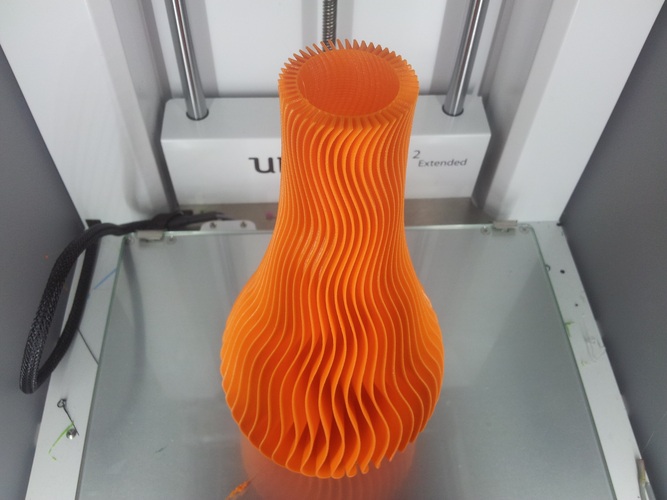
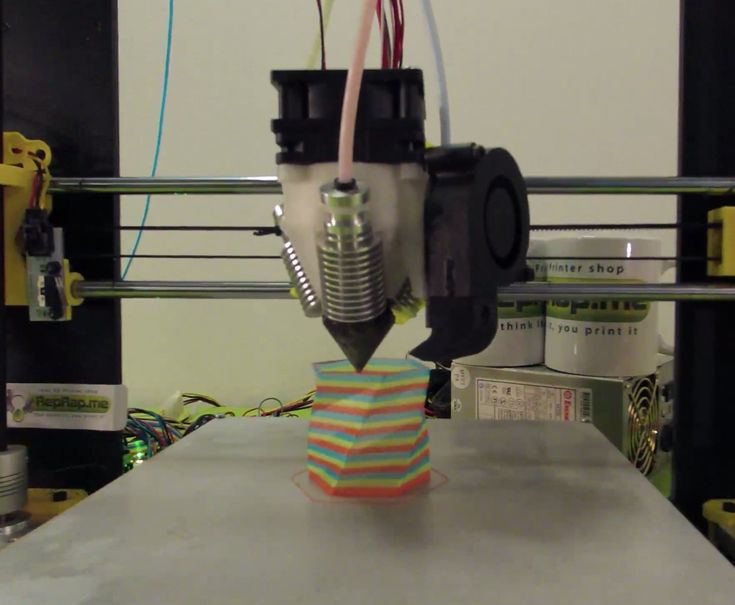
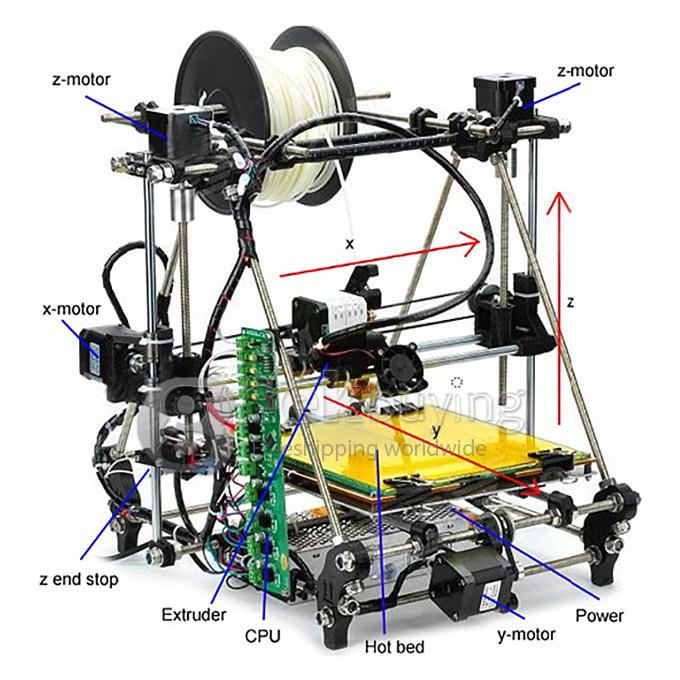
Technically, how does biological 3-D printing work?
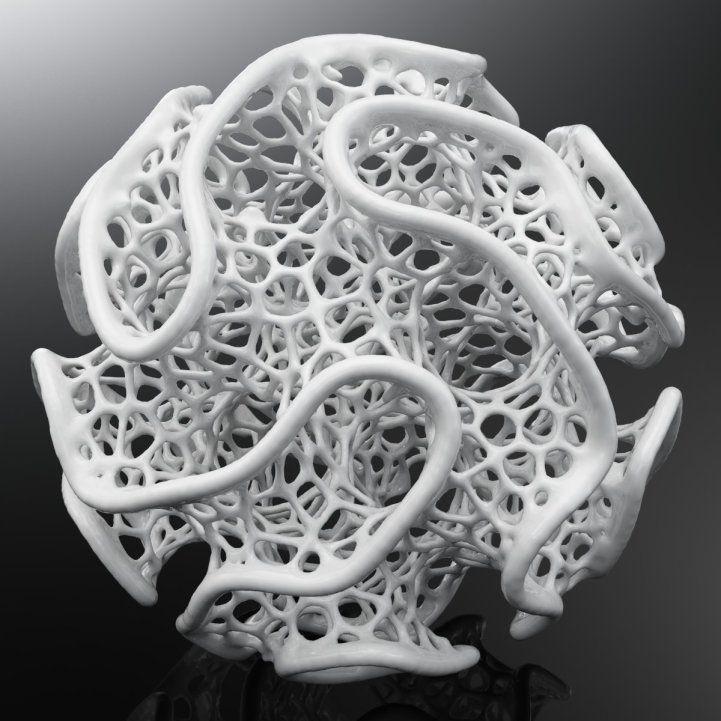
3-D printing an ovary structure is similar to a child using Lincoln Logs, said Alexandra Rutz, co-lead author of the study and a former biomedical engineering graduate fellow in Shah’s Tissue Engineering and Additive Manufacturing (TEAM) lab at the Simpson Querrey Institute. Children can lay the logs at right angles to form structures. Depending on the distance between the logs, the structure changes to build a window or a door, etc.
“3-D printing is done by depositing filaments,” said Rutz, who is now a Whitaker International Postdoctoral Scholar at École Des Mines De Saint-Étienne in Gardanne, France. “You can control the distance between those filaments, as well as the advancing angle between layers, and that would give us different pore sizes and different pore geometries. ”
”
In Northwestern’s lab, the researchers call these 3-D printed structures “scaffolds,” and liken them to the scaffolding that temporarily surrounds a building while it undergoes repairs.
“Every organ has a skeleton,” said Woodruff, who also is the Thomas J. Watkins Memorial Professor of Obstetrics and Gynecology and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “We learned what that ovary skeleton looked like and used it as model for the bioprosthetic ovary implant.”
In a building, the scaffolding supports the materials needed to repair the building until it’s eventually removed. What’s left is a structure capable of holding itself up. Similarly, the 3-D printed “scaffold” or “skeleton” is implanted into a female and its pores can be used to optimize how follicles, or immature eggs, get wedged within the scaffold. The scaffold supports the survival of the mouse’s immature egg cells and the cells that produce hormones to boost production.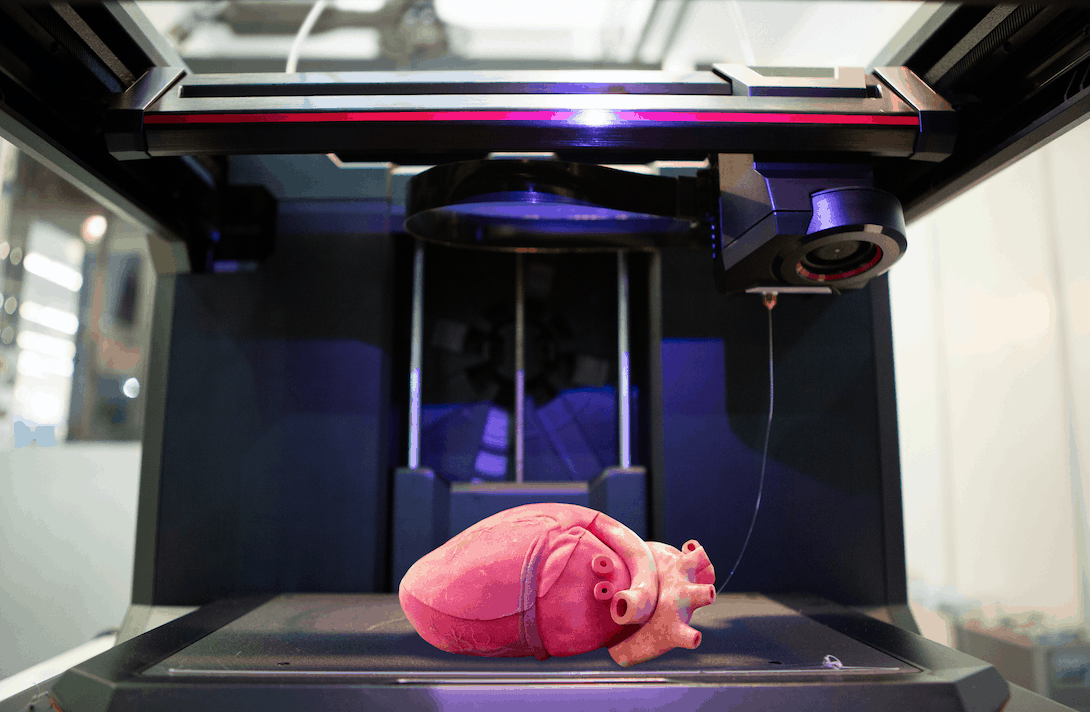 The open structure also allows room for the egg cells to mature and ovulate, as well as blood vessels to form within the implant enabling the hormones to circulate within the mouse bloodstream and trigger lactation after giving birth.
The open structure also allows room for the egg cells to mature and ovulate, as well as blood vessels to form within the implant enabling the hormones to circulate within the mouse bloodstream and trigger lactation after giving birth.
The all-female McCormick-Feinberg collaboration for this research was “very fruitful,” Shah said, adding that it was motivational to be part of an all-female team doing research towards finding solutions to female health issues.
“What really makes a collaboration work are the personalities and being able to find the humor in the research,” Shah said. “Teresa and I joked that we’re grandparents of these pups.”
Editor’s Picks
A campus resource that helps first-generation and low-income students succeed at Northwestern
October 27, 2022
Northwestern invites community feedback on new Ryan Field plan
October 28, 2022
Practice the art of looking — at art
October 27, 2022
Never miss a story:
Get the latest stories from Northwestern Now sent directly to your inbox.
Subscribe
Three-dimensional bioprinting of artificial ovaries by an extrusion-based method using gelatin-methacryloyl bioink
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Taylor & Francis
Full text links
. 2022 Apr;25(2):170-178.
2022 Apr;25(2):170-178.
doi: 10.1080/13697137.2021.1921726. Epub 2021 May 17.
T Wu 1 2 3 , Y Y Gao 1 2 3 , J Su 4 , X N Tang 1 2 3 , Q Chen 1 2 3 , L W Ma 1 2 3 , J J Zhang 1 2 3 , J M Wu 4 , S X Wang 1 2 3
Affiliations
Affiliations
- 1 National Clinical Research Center for Obstetrical and Gynecological Diseases, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- 2 Key Laboratory of Cancer Invasion and Metastasis, Ministry of Education, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- 3 Department of Obstetrics and Gynecology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- 4 State Key Laboratory of Materials Processing and Die & Mould Technology, School of Materials Science and Engineering, Huazhong University of Science and Technology, Wuhan, China.
- PMID: 33993814
- DOI: 10.1080/13697137.2021.
 1921726
1921726
T Wu et al. Climacteric. 2022 Apr.
. 2022 Apr;25(2):170-178.
doi: 10.1080/13697137.2021.1921726. Epub 2021 May 17.
Authors
T Wu 1 2 3 , Y Y Gao 1 2 3 , J Su 4 , X N Tang 1 2 3 , Q Chen 1 2 3 , L W Ma 1 2 3 , J J Zhang 1 2 3 , J M Wu 4 , S X Wang 1 2 3
Affiliations
- 1 National Clinical Research Center for Obstetrical and Gynecological Diseases, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.

- 2 Key Laboratory of Cancer Invasion and Metastasis, Ministry of Education, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- 3 Department of Obstetrics and Gynecology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- 4 State Key Laboratory of Materials Processing and Die & Mould Technology, School of Materials Science and Engineering, Huazhong University of Science and Technology, Wuhan, China.
- PMID: 33993814
- DOI: 10.1080/13697137.2021.
 1921726
1921726
Abstract
Purpose: The aim of this study was to design and fabricate a three-dimensional (3D) printed artificial ovary.
Methods: We first compared the printability of gelatin-methacryloyl (GelMA), alginate and GelMA-alginate bioinks, of which GelMA was selected for further investigation. The swelling properties, degradation kinetics and shape fidelity of GelMA scaffolds were characterized by equilibrium swelling/lyophilization, collagenase processing and micro-computed tomography evaluation. Commercial ovarian tumor cell lines (COV434, KGN, ID8) and primary culture ovarian somatic cells were utilized to perform cell-laden 3D printing, and the results were evaluated by live/dead assays and TUNEL detection. Murine ovarian follicles were seeded in the ovarian scaffold and their diameters were recorded every day.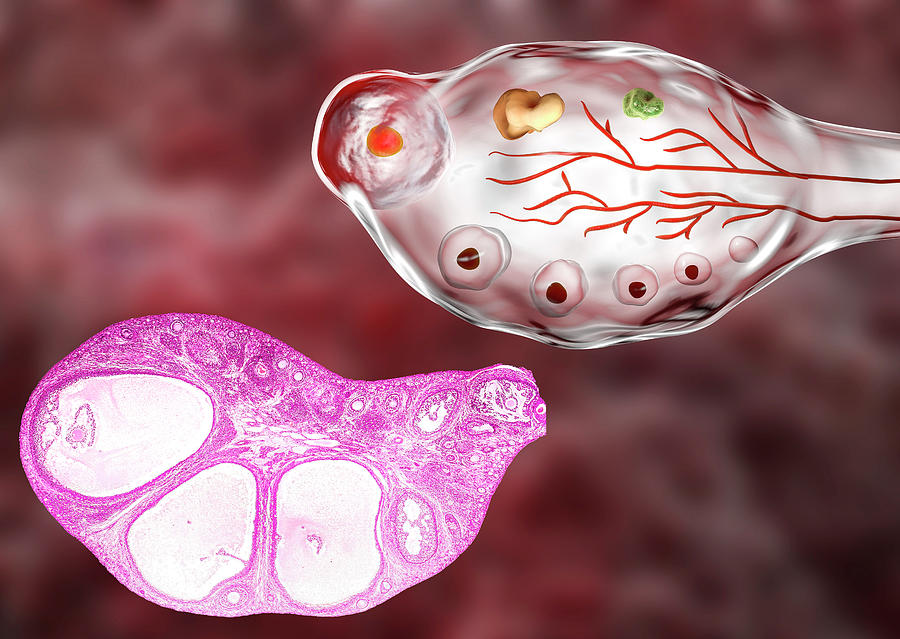 Finally, in vitro maturation was performed, and the ovulated oocytes were collected and observed.
Finally, in vitro maturation was performed, and the ovulated oocytes were collected and observed.
Results: Our results indicated that GelMA was suitable for 3D printing fabrication. Its scaffolds performed well in terms of hygroscopicity, degradation kinetics and shape fidelity. The viability of ovarian somatic cells was lower than that of commercial cell lines, suggesting that extrusion-based 3D culture fabrication is not suitable for primary ovarian cells. Nevertheless, the GelMA-based 3D printing system provided an appropriate microenvironment for ovarian follicles, which successfully grew and ovulated in the scaffolds. Metaphase II oocytes were also observed after in vitro maturation.
Conclusions: The GelMA-based 3D printing culture system is a viable alternative option for follicular growth, development and transfer.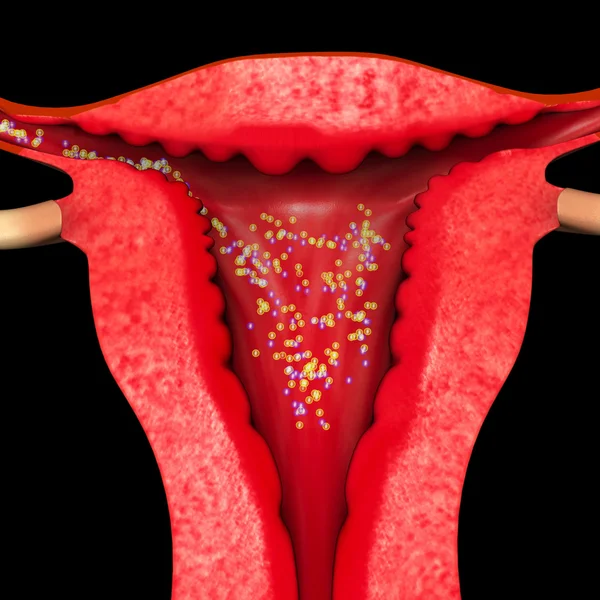 Accordingly, it shows promise for clinical application in the treatment of female endocrine and reproductive conditions.
Accordingly, it shows promise for clinical application in the treatment of female endocrine and reproductive conditions.
Keywords: 3D bioprinting; alginate; artificial ovary; gelatin-methacryloyl.
Similar articles
-
3D Bioprinting of Low-Concentration Cell-Laden Gelatin Methacrylate (GelMA) Bioinks with a Two-Step Cross-linking Strategy.
Yin J, Yan M, Wang Y, Fu J, Suo H. Yin J, et al. ACS Appl Mater Interfaces. 2018 Feb 28;10(8):6849-6857. doi: 10.1021/acsami.7b16059. Epub 2018 Feb 15. ACS Appl Mater Interfaces. 2018. PMID: 29405059
-
Coaxial extrusion bioprinting of 3D microfibrous constructs with cell-favorable gelatin methacryloyl microenvironments.
Liu W, Zhong Z, Hu N, Zhou Y, Maggio L, Miri AK, Fragasso A, Jin X, Khademhosseini A, Zhang YS. Liu W, et al. Biofabrication. 2018 Jan 12;10(2):024102. doi: 10.1088/1758-5090/aa9d44. Biofabrication. 2018. PMID: 29176035 Free PMC article.
-
Embedded 3D Bioprinting of Gelatin Methacryloyl-Based Constructs with Highly Tunable Structural Fidelity.
Ning L, Mehta R, Cao C, Theus A, Tomov M, Zhu N, Weeks ER, Bauser-Heaton H, Serpooshan V. Ning L, et al. ACS Appl Mater Interfaces. 2020 Oct 7;12(40):44563-44577. doi: 10.1021/acsami.0c15078. Epub 2020 Sep 23. ACS Appl Mater Interfaces. 2020. PMID: 32966746
-
A review on alginate-based bioinks, combination with other natural biomaterials and characteristics.
Shams E, Barzad MS, Mohamadnia S, Tavakoli O, Mehrdadfar A.
 Shams E, et al. J Biomater Appl. 2022 Aug;37(2):355-372. doi: 10.1177/08853282221085690. Epub 2022 May 5. J Biomater Appl. 2022. PMID: 35510845 Review.
Shams E, et al. J Biomater Appl. 2022 Aug;37(2):355-372. doi: 10.1177/08853282221085690. Epub 2022 May 5. J Biomater Appl. 2022. PMID: 35510845 Review. -
Recent Advances on Bioprinted Gelatin Methacrylate-Based Hydrogels for Tissue Repair.
Rajabi N, Rezaei A, Kharaziha M, Bakhsheshi-Rad HR, Luo H, RamaKrishna S, Berto F. Rajabi N, et al. Tissue Eng Part A. 2021 Jun;27(11-12):679-702. doi: 10.1089/ten.TEA.2020.0350. Epub 2021 Mar 9. Tissue Eng Part A. 2021. PMID: 33499750 Review.
See all similar articles
Cited by
-
Are we ready for the revision of the 14-day rule? Implications from Chinese legislations guiding human embryo and embryoid research.
Xue Y, Shang L.
 Xue Y, et al. Front Cell Dev Biol. 2022 Oct 24;10:1016988. doi: 10.3389/fcell.2022.1016988. eCollection 2022. Front Cell Dev Biol. 2022. PMID: 36353513 Free PMC article. Review.
Xue Y, et al. Front Cell Dev Biol. 2022 Oct 24;10:1016988. doi: 10.3389/fcell.2022.1016988. eCollection 2022. Front Cell Dev Biol. 2022. PMID: 36353513 Free PMC article. Review. -
Automatic Evaluation for Bioengineering of Human Artificial Ovary: A Model for Fertility Preservation for Prepubertal Female Patients with a Malignant Tumor.
Wang W, Pei C, Isachenko E, Zhou Y, Wang M, Rahimi G, Liu W, Mallmann P, Isachenko V. Wang W, et al. Int J Mol Sci. 2022 Oct 17;23(20):12419. doi: 10.3390/ijms232012419. Int J Mol Sci. 2022. PMID: 36293273 Free PMC article.
-
Construction of Artificial Ovaries with Decellularized Porcine Scaffold and Its Elicited Immune Response after Xenotransplantation in Mice.
Wu T, Gao YY, Tang XN, Zhang JJ, Wang SX.
 Wu T, et al. J Funct Biomater. 2022 Sep 28;13(4):165. doi: 10.3390/jfb13040165. J Funct Biomater. 2022. PMID: 36278634 Free PMC article.
Wu T, et al. J Funct Biomater. 2022 Sep 28;13(4):165. doi: 10.3390/jfb13040165. J Funct Biomater. 2022. PMID: 36278634 Free PMC article. -
Application Prospect and Preliminary Exploration of GelMA in Corneal Stroma Regeneration.
Su G, Li G, Wang W, Xu L. Su G, et al. Polymers (Basel). 2022 Oct 9;14(19):4227. doi: 10.3390/polym14194227. Polymers (Basel). 2022. PMID: 36236174 Free PMC article. Review.
-
Bioengineering trends in female reproduction: a systematic review.
Francés-Herrero E, Lopez R, Hellström M, de Miguel-Gómez L, Herraiz S, Brännström M, Pellicer A, Cervelló I. Francés-Herrero E, et al. Hum Reprod Update. 2022 Nov 2;28(6):798-837. doi: 10.1093/humupd/dmac025. Hum Reprod Update.
 2022. PMID: 35652272 Free PMC article.
2022. PMID: 35652272 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Full text links
Taylor & Francis
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Ovary printed on a 3D printer: alev_biz — LiveJournal
? 3D-printed gelatin base for the ovary proved to be egg-friendly.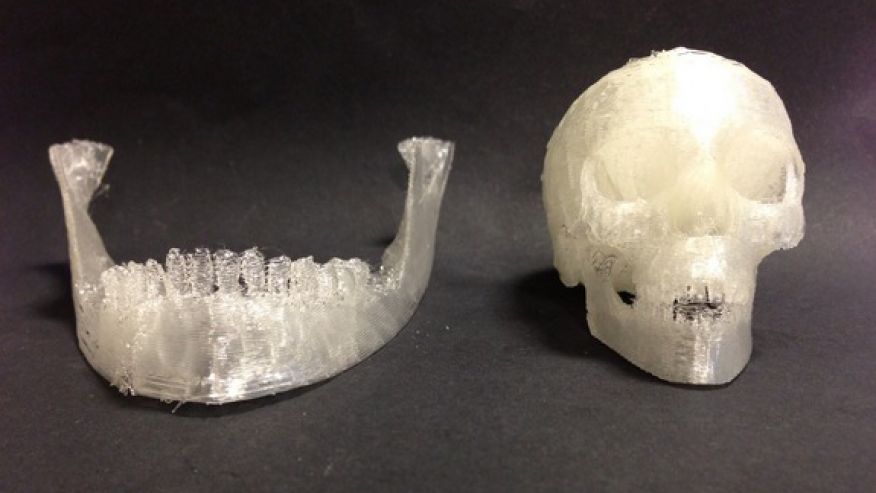
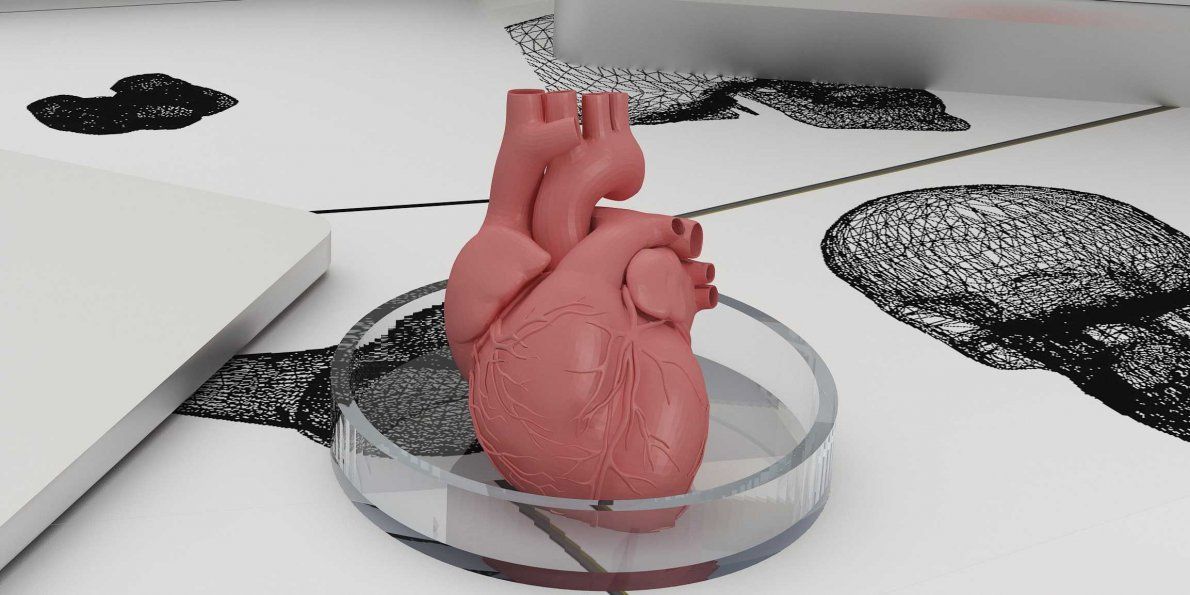
Modern medicine is increasingly mastering the method of three-dimensional printing: now with the help of 3D printers they have already learned how to make artificial auricles (there was an article about this a year ago in Nature Biotechnology ), heart valves (article in Science Advances in 2015), bone-like implants ( Science Translational Medicine ).
Human sperm and egg.
A new article published recently in Nature Communications describes even more incredible things: it turns out that it is possible to print an ovary on a 3D printer, which, after being transplanted into the body of a female, will work like a real one.
Here, however, it is worth immediately clarifying that researchers from Northwestern University did not print the entire ovary - after all, it is a rather complex, multicomponent organ. As you know, in the ovaries, the maturation of eggs occurs, which are located in special structures - follicles. The follicles themselves are immersed in connective tissue.
The follicles themselves are immersed in connective tissue.
Immature mouse egg between printed layers of gelatin (layer A, layer B).
Monica Laronda ( Monica M. Laronda ) and her colleagues created the connective tissue base of the ovary using 3D printing: the printer was charged with gelatin, which was obtained from collagen, one of the main proteins of connective tissue - collagen was in the form in which it is usually present in the ovaries of animals. Then, mouse follicles with eggs inside were immersed in the resulting (printed) gelatin base.
The point was to test how the different arrangement of the gelatin fibers would affect the viability of the egg follicles. The fibers were laid in layers at different angles to each other, so that different variants of the gelatin base with different porosity were obtained.
In the most successful case, the egg remained alive for eight days - and it was these semi-artificial ovaries that were transplanted into seven mice to replace their own. Once transplanted, the blood vessels penetrated the gelatinous base, supplying the follicles with nutrients and hormones, so that the eggs eventually went through all the necessary stages of development and became ready for fertilization. And when males were provided to the experimental female mice, three of them became pregnant and gave birth to completely healthy offspring - that is, the follicles, which themselves produce the hormones necessary for reproduction, worked as they should in these females.
Once transplanted, the blood vessels penetrated the gelatinous base, supplying the follicles with nutrients and hormones, so that the eggs eventually went through all the necessary stages of development and became ready for fertilization. And when males were provided to the experimental female mice, three of them became pregnant and gave birth to completely healthy offspring - that is, the follicles, which themselves produce the hormones necessary for reproduction, worked as they should in these females.
Perhaps in the future, with the help of such ovaries, it will be possible to get rid of some forms of infertility; True, semi-artificial ovaries will need to be scaled to fit a person and make sure that the blood vessels can fully provide them with everything they need in the female body.
Author: Kirill Stasevich
Link to source
Tags: bioprinting, biotechnology, medicine, science, transplantation
Subscribe to Telegram channel alev_biz
Subscribe
-
Superbugs come to people from other people
Superbugs are bacteria that are resistant to antibiotics, and some become resistant to several at once.
 About such ...
About such ... -
Interesting patient: swim in a warm pond and try to survive
Today a boy who loves roller coasters, plays baseball, is fond of botany and nature, and tomorrow a bedridden man with ...
-
Covid-19 brain anomalies found on MRI images
Using one of the types of MRI - magnetic susceptibility-weighted imaging - scientists have found in people who have had Covid-19, ...
Photo
Hint 90 ://pics.livejournal.com/igrick/pic/000r1edq
Ovary printed on a 3D printer: alev_biz — LiveJournal
?- Technology
- Medicine
- Cancel
Immature mouse egg between printed layers of gelatin (layer A, layer B)
In a new article published recently in Nature Communications , even more incredible things are described: it turns out that it is possible to print an ovary on a 3D printer, which, after being transplanted into the body of a female, will work like a real one.
Here, however, it is worth immediately clarifying that researchers from Northwestern University did not print the entire ovary - after all, this is a rather complex, multicomponent organ. As you know, in the ovaries, the maturation of eggs occurs, which are located in special structures - follicles. The follicles themselves are immersed in connective tissue.
Monica M.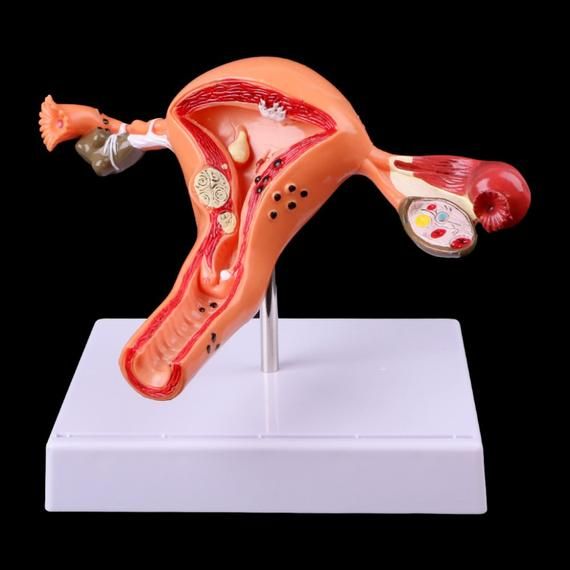 Laronda ( Monica M. Laronda ) and her colleagues created the connective tissue base of the ovary using 3D printing: the printer was charged with gelatin, which was obtained from collagen, one of the main proteins of connective tissue - the collagen was in the form in which it is usually present in the ovaries of animals. Then, mouse follicles with eggs inside were immersed in the resulting (printed) gelatin base.
Laronda ( Monica M. Laronda ) and her colleagues created the connective tissue base of the ovary using 3D printing: the printer was charged with gelatin, which was obtained from collagen, one of the main proteins of connective tissue - the collagen was in the form in which it is usually present in the ovaries of animals. Then, mouse follicles with eggs inside were immersed in the resulting (printed) gelatin base.
The point was to test how the different arrangement of the gelatin fibers would affect the viability of the egg follicles. The fibers were laid in layers at different angles to each other, so that different variants of the gelatin base with different porosity were obtained.
In the most successful case, the egg remained alive for eight days - and it was these semi-artificial ovaries that were transplanted into seven mice to replace their own. Once transplanted, the blood vessels penetrated the gelatinous base, supplying the follicles with nutrients and hormones, so that the eggs eventually went through all the necessary stages of development and became ready for fertilization.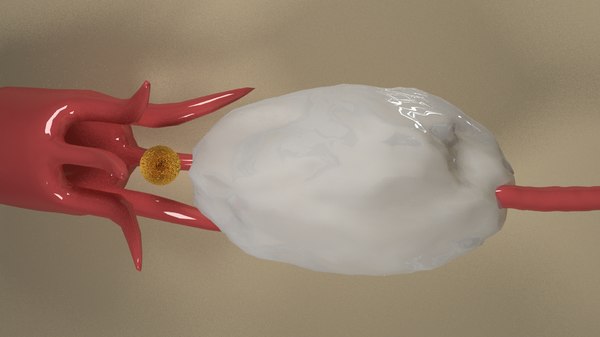 And when males were provided to the experimental female mice, three of them became pregnant and gave birth to completely healthy offspring - that is, the follicles, which themselves produce the hormones necessary for reproduction, worked as they should in these females.
And when males were provided to the experimental female mice, three of them became pregnant and gave birth to completely healthy offspring - that is, the follicles, which themselves produce the hormones necessary for reproduction, worked as they should in these females.
Perhaps in the future, with the help of such ovaries, it will be possible to get rid of some forms of infertility; True, semi-artificial ovaries will need to be scaled to fit a person and make sure that the blood vessels can fully provide them with everything they need in the female body.
Author: Kirill Stasevich
Link to source
Tags: bioprinting, biotechnology, artificial organs, medicine, transplantation
Subscribe to Telegram channel alev_biz
Subscribe
-
Synthetic mouse embryo that has a heartbeat and develops a brain
According to an article published in the journal Nature, after 10 years of research, scientists have grown in vitro a synthetic mouse embryo that…
-
Doctors successfully transplanted artificial corneas from porcine collagen into humans
Corneal implants obtained by bioengineers based on pig skin were successfully transplanted into 20 patients.
Learn more