3D printed liver transplant
3D printed implant keeps liver patients alive as they hold out for donors
0Shares
Scientists at the Catholic University of Korea and Asan Medical Center have 3D printed a novel device that could be used to stabilize Acute Liver Failure (ALF) patients as they wait for a life-saving organ donation.
Composed of a 3D printed container and semipermeable membrane, the team’s implant allows for the rapid delivery of the drugs needed to save those in danger of succumbing to ALF. Once implanted, the device also acts as a ‘bioartificial support system,’ functioning as the patient’s liver while reducing any dysfunction caused to their other internal organs, keeping them alive until a transplant becomes available.
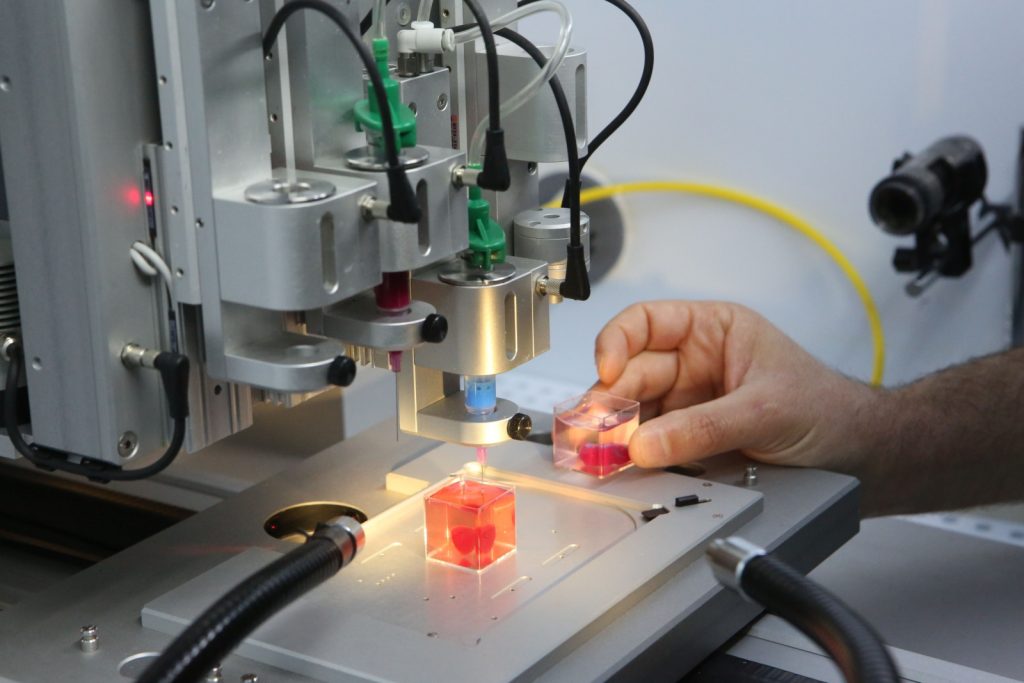
The team’s 3D printed device features a liver-treating drug-loaded reservoir. Image via the Advanced Healthcare Materials journal.ALF: a transplant emergency
In many cases, ALF patients suffer such severe liver damage that their organ’s constituent hepatocyte cells begin to malfunction, in a rapidly deteriorating situation that can prove fatal. With regards to treatment, orthotopic liver transplantation is the only proven cure for final-stage liver disease, and in practice, donor scarcity often limits its use.
Additionally, liver transplants can be costly, and due to organ incompatibility and issues surrounding patient body rejection, the procedure also brings with it a significant risk of mortality. As a result, scientists have increasingly sought to identify new ways of delivering life-saving Active Pharmaceutical Ingredients (or APIs) to damaged liver tissues, via complex implantable drug-delivery devices.
Earlier this year, for instance, a group of researchers developed a novel method of using encapsulated stem cells to treat chronic liver injuries, but according to the Korean team, their approach has low repeatability, and the device itself proved difficult to shape into the geometry necessary for treating damaged liver tissues.
The scientists tested their 3D printed device by transplanting it into 34 different lab mice. Image via the Advanced Healthcare Materials journal.
Image via the Advanced Healthcare Materials journal. A lifesaving delivery device
To get around the structural limitations seen in previous designs, the researchers used a Cubicon Style 3D printer to produce a set of implantable TPU API-loaded reservoirs. Thanks to 3D printing’s inherent flexibility, the team was able to iteratively develop drug delivery devices in multiple forms, with each featuring a ‘port’ that enables the medication to be continuously delivered to damaged tissues.
Interestingly, by configuring the pore size of their reservoir, the scientists found they could customize their devices to selectively deliver drugs of various weights, and specifically design their prototypes’ ports for the connection of syringes, thus during initial implantation tests on lab mice, the team was able to refill their devices multiple times and at will.
Even more impressively, over a four-week period, none of the scientists’ test subjects showed any sign of changes to either their behavior or body weight. Having established that their device was capable of consistent drug delivery, the researchers later tested its efficacy by ‘treating’ thirty-four 70%-scale resected mouse liver models.
Having established that their device was capable of consistent drug delivery, the researchers later tested its efficacy by ‘treating’ thirty-four 70%-scale resected mouse liver models.
Of these tiny livers, only one died within three days of surgery, while the scientists observed no “abnormal clinical signs,” and some models responded to API infusion by growing back 85% of their mass. Consequently, citing their testing success, the team concluded their device to represent a novel ‘bridge therapy,’ with the potential to not just keep patients’ livers alive, but actually instigate organ regrowth.
However, while the Korean team is confident in their system’s therapeutic capabilities, they have conceded that in practice, its non-biodegradable nature means it would need to be removed via a painful secondary surgery and could even trigger bodily rejection, thus they say future iterations should be built from more human-friendly materials instead.
“[Our] biodegradable implants have long-term potential as a foreign material that remains in the abdominal cavity of mice, [but] this can require additional secondary surgery for implant removal,” concluded the team in their paper. “Thus, for clinical approaches, a biodegradable device or permanent version, should be selected for acute therapy or long-term effects, respectively.”
A bioprinted liver alternative?
While 3D bioprinting full human organs remains a long way from reality, the Korean team’s device shows how the technology can be deployed to heal existing tissues instead. Likewise, in a similar study, T&R Biofab revealed earlier this month that it had managed to 3D bioprint and implant liver ‘lobule’ tissues, with potential regenerative medicine applications.
When recently questioned on the viability of bioprinting as an animal testing substitute, the Brain Research Institute’s Juan Carlos Marvizon was also broadly supportive of this view. According to Marvizon, the technology’s potential lies in regenerative medicine rather than drug testing, where interactions between human tissues are often very difficult to replicate.
Elsewhere, in terms of drug delivery innovation, 3D printing’s research community has really come up trumps over the last year, with scientists at the University of Kent and the University of Strathclyde creating a novel transdermal drug delivery system, while at ETH Zurich, another team has 3D printed microbots capable of ‘carrying’ drugs along blood vessels.
The researchers’ findings are detailed in their paper titled “Design and Usability Evaluations of a 3D-Printed Implantable Drug Delivery Device for Acute Liver Failure in Preclinical Settings.”
The study was co-authored by Shin-Young Kim, Ginam Han, Da-Bin Hwang, Dong-Hoon Won, Yoo-Sub Shin, Changuk Kim, Jeon Min Kang, Jung-Hoon Park, Hyun-Do Jung, Wooram Park, and Jun-Won Yun.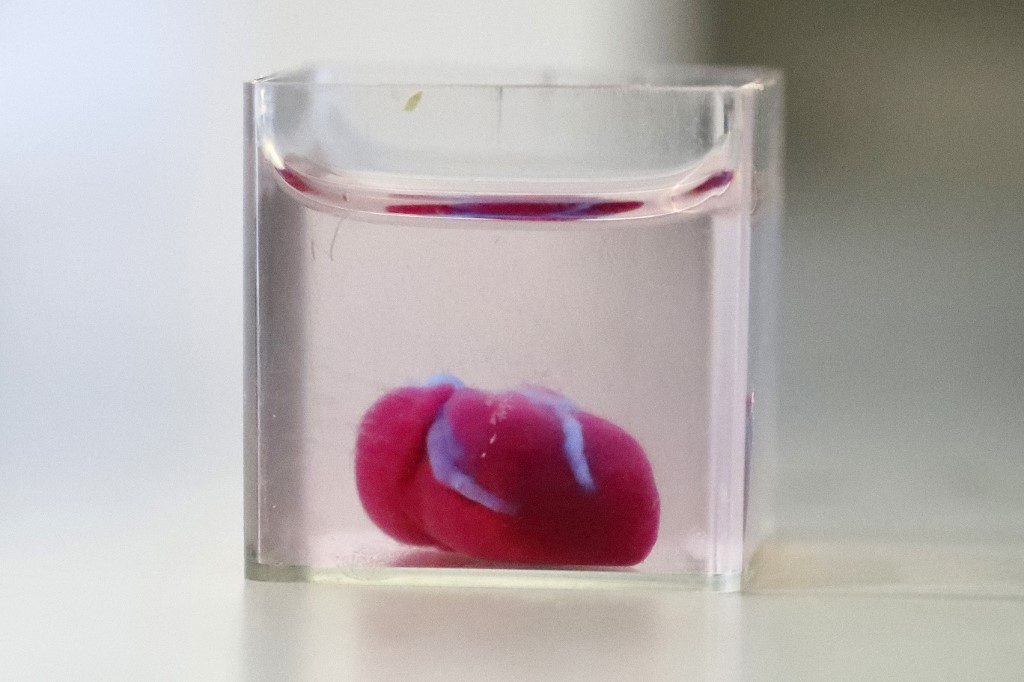
The nominations for the 2021 3D Printing Industry Awards are now open. Who do you think should make the shortlists for this year’s show? Have your say now.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
For a deeper dive into additive manufacturing, you can now subscribe to our Youtube channel, featuring discussion, de-briefs, and shots of 3D printing in-action.
Are you looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows the layout of the Korean researchers’ 3D printed drug-delivery device. Image via the Advanced Healthcare Materials journal.
Tags Asan Medical Center Brain Research Institute Catholic University of Korea Cubicon Style ETH Zurich Juan Carlos Marvizon T&R Biofab University of Kent University of Strathclyde
Paul Hanaphy
Paul is a history and journalism graduate with a passion for finding the latest scoop in technology news.
T&R Biofab pulls-off breakthrough 3D bioprinted liver tissue transplant
0Shares
Korean 3D bioprinter manufacturer T&R Biofab has successfully fabricated liver tissues and transplanted them into an animal test subject for the first time.
Using one of the firm’s modified 3DX bioprinters, its researchers have been able to pattern spherical microtissues into structures, which replicate those of the ‘lobules’ found inside the human liver. Once implanted into lab mice, the resulting ‘micro-organs’ have shown excellent viability and structural stability, potentially making them a significant step towards the regenerative liver therapies of the future.
“What our research has highlighted for the first time is that 3D bioprinting can actually make a difference in [cellular] 3D structures,” said Paulo André Marinho, Head of Scientific Strategy at T&R Biofab. “We’ve made a phenotypically-relevant tissue that, once injected into animals, engrafts substantially better than 3D counterparts without structure. ”
”
The researchers’ 3D bioprinting and implantation technique. Image via the Advanced Materials journal.“We seem to be the first to successfully fully-bioprint highly-organized constructs that, once transplanted, had nearly no cell death or fibrotic tissue observed.”
Bioprinting liver lobules
Generally speaking, the human body is composed of several different multiscaled tissues and organs, with the liver being a particularly highly-vascularized example. Of the human liver, around 80% is made up of small functional units called hepatic lobules, and advances in 3D bioprinting are increasingly making it possible to replicate these building blocks, and create thicker, more viable soft tissue models.
However, cultivating these hepatocytes continues to prove difficult, particularly when attempting to bioprint organs with sufficient vascularization and cell viability for potential transplantation. One of the main drawbacks to bioprinting lobules lies in the technology used to create them, as UV-based approaches often require the use of cross-linker which can be toxic to liver cells, damaging their viability..jpg)
Likewise, where livers have been bioprinted on a microscale and transplanted in previous studies, they’ve only kept animal test subjects alive for 5 to 25 extra days, limiting the human applications of such methods. To get around this, and develop a means of producing more viable tissues with a greater level of cell placement precision, T&R Biofab’s team developed a novel extrusion technique last year.
In effect, the researchers’ revised method involved using a lobule-shaped cartridge with slots for hepatocyte cells, endothelial cells and cell-free bio-inks to produce vascularized structures, but extruding these materials into 3D layers still proved troublesome, and their risk of collapse was found to depend highly on the properties of their constituent materials.
Now, building on the success of their initial research, the Korean team have embraced a microfluidic approach to develop a second iteration of their technology, which is capable of producing lobule-like spheroids with a dramatically improved viability, that lends them potential within human cell-based therapeutic applications and the R&D of patient-specific medicines.
Liver tissue-transplant success
With their new technique, the T&R Biofab scientists have essentially combined extrusion with microfluidic emulsification, to produce spheroids at high-speed with a uniform size, without the need for crosslinking. In practise, the team’s approach saw them once again fill precursor cartridges with cells, but this time they deposited them into cross-sectional shapes, lending them a natural durability.
“The use of microfluidics enabled the generation of micro-liver spheres without the need of cutting the fiber into pieces,” explained Marinho. “This instantly brings high throughput drug screening, development and, luckily for us as we demonstrated in the paper, very high reproducibility without loss of viability in cells.”
During testing, the team assessed their improved methodology by producing several lobular microtissue spheroids, which compared to non-structured samples, each showed enhanced cell viability. What’s more, by four days after the initial experiment, the vascular structure had grown to a width of around 20 µm, a resolution that remains out of reach for many conventional extrusion bioprinters.
What’s more, by four days after the initial experiment, the vascular structure had grown to a width of around 20 µm, a resolution that remains out of reach for many conventional extrusion bioprinters.
“Making a sphere as small as 250 micrometers with a highly compartmentalized structure that mimics the phenotype of in-vivo tissues is unheard of.”
Having demonstrated the efficacy of their technique, the researchers proceeded to test the implantation potential of their printed lobules by injecting them into lab mice. Not only did the lobular samples form blood vessels in-vivo, but their structural integrity improved significantly compared to non-structured alternatives, while experiencing nearly no loss of viability.
As a result, the T&R Biofab scientists believe that although their spheroids themselves aren’t novel, they possess a compartmentalized in-vivo structure that “is unheard of” in the industry, thus with sufficient R&D, the technique used to create them could be deployed to develop “revolutionary” treatments, which restore functionality to damaged human organs.
“We did not do clinical trials, so we cannot affirm that results are the same in humans,” concluded Marinho. “But, if any researcher wants to increase the chance of making tissue therapy a success, he/she should at the very minimum consider if his/her engineered tissues could be better, if they were phenotypically-similar to in-vivo tissues prior to transplantation.”
Organ 3D bioprinting’s potential
While techniques such as that being developed by T&R Biofab could eventually forgo the need for fully-printed organs altogether, multiple groups of researchers are currently working to achieve just that. For instance, through its Print to Perfusion program, 3D Systems is developing an ultra-precise means of 3D bioprinting fully-sized, vascularized human lung scaffolds.
In a similar vein, EPFL spin-out Readily3D has made significant progress in its work towards developing a 3D printed human pancreas model. Developed as part of the EU-funded Enlight project, the firm’s technology is reportedly capable of producing tissues within just 30 seconds for diabetes drug-testing applications.
Elsewhere, 3D bioprinting experts have remained split about its viability for creating transplantable organs, with the interaction between natural and synthetic tissues being identified as a potential issue. According to the Brain Research Institute’s Juan Carlos Marvizon, such organs can theoretically be programmed to prevent rejection from their hosts, although this hasn’t yet been tested in practise.
The researchers’ findings are detailed in their paper titled “Production of Multiple Cell-Laden Microtissue Spheroids with Biomimetic Hepatic Lobule-like Structure.”
The study was co-authored by Gyusik Hong, Jin Kim, Hyeongkwon Oh, Seokhwan Yun, Chul Min Kim, Yun-Mi Jeong, Won-Soo Yun, Jin-Hyung Shim, Ilho Jang, C-yoon Kim and Songwan Jin.
The nominations for the 2021 3D Printing Industry Awards are now open. Who do you think should make the shortlists for this year’s show? Have your say now.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
For a deeper-dive into additive manufacturing, you can now subscribe to our Youtube channel, featuring discussion, de-briefs and shots of 3D printing in-action.
Are you looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows lab mice with both structured and unstructured 3D bioprinted lobular implants. Photo via the Advanced Materials journal.
Tags 3D Systems Brain Research Institute EPFL Juan Carlos Marvizon Paulo André Marinho Readily3D T&R Biofab
Paul Hanaphy
Paul is a history and journalism graduate with a passion for finding the latest scoop in technology news.
The liver will go to print - Nauka - Kommersant
Professor Vladimir Mironov is working to create spare parts for the human body as simply as for a car: take and print a human organ on a 3D printer.
Professor Vladimir Mironov
Photo: Courtesy of 3D Bioprinting Solutions Lab
People are already well versed in printing houses, cars, weapons, intricate details - just about everything. But the human organ, of course, is a much more complicated thing: firstly, in manufacturing, and secondly, then it will have to be used for a long time! A task for the Creator!
But the human organ, of course, is a much more complicated thing: firstly, in manufacturing, and secondly, then it will have to be used for a long time! A task for the Creator!
In 2003, Professor Vladimir Mironov discovered that individual ring fragments of the heart of a chicken embryo can merge, collect into a tube, when placed in a hydrogel in the form of a ring. Having discovered this, Professor Mironov and his colleagues took an inkjet printer, instead of ink, they placed cells in it and printed it. And a miracle: the cells survived. The authors of the miracle wrote an article in a scientific journal, and the idea of 3D bioprinting of biological objects was born.
And now there is a bioprinting company, 3D Bioprinting Solutions: Vladimir Mironov accepted the invitation of Alexander Ostrovsky, managing partner of Invitro, to become the head of the first laboratory in Russia that will directly deal with bioprinting, that is, the printing of living organs. In 2013, the laboratory began work.
“Five major achievements over the years, which show that we do not waste time in vain,” says Mironov, raising his hand with spread fingers.
3D bioprinting requires raw materials. In bioprinting, this role is played by tissue spheroids - microballoons consisting of thousands of living cells. The spheroids are stacked layer by layer, forming what should become a living organ. Previously, in tissue engineering, they used the technology of scaffolds (scaffolding, if in Russian): they did not allow the structure to fall apart. The first achievement of the 3D Bioprinting Solutions laboratory was to establish the production of tissue spheroids of standard shape and size, which made it possible to significantly speed up the bioprinting process.
Bioprinted mouse thyroid construct
Photo: Courtesy of 3D Bioprinting Solutions
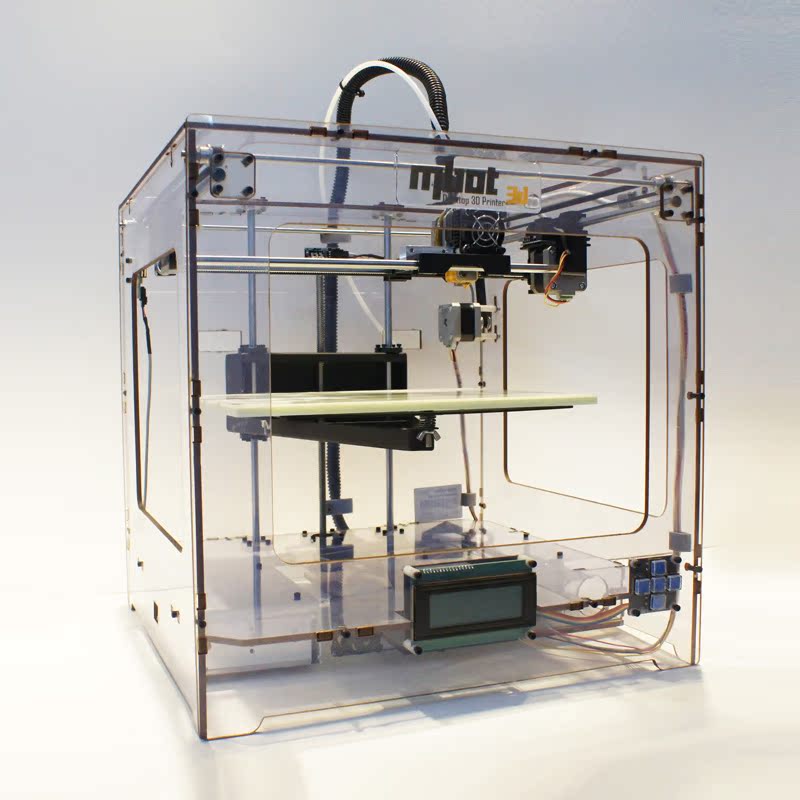
The second achievement is the 3D printer itself, it was called Fabion: fabrication plus biology, Professor Mironov explains and says with a smile that the main thing is still beautiful sound . Approximately 80 companies produce such printers, Fabion is consistently in the top five, ahead of only a few competitors from the USA, Germany and Switzerland.
Approximately 80 companies produce such printers, Fabion is consistently in the top five, ahead of only a few competitors from the USA, Germany and Switzerland.
“The process of bioprinting is similar to creating a book on a printing press, that is, ink is needed,” says Vladimir Mironov, and if we follow the analogy, then 3D Bioprinting Solutions figured out how to make bioink - they became a viscous collagen (pork) protein. And that was the third achievement.
It's time to print the organ!
Question - which one? The heart or kidneys are too complicated, there are a lot of blood vessels. The liver is more homogeneous, but it is a large organ. Thyroid!
Raw material taken from mouse embryos. It took only nine spheroids (three for the gland itself, six for the vessels) to print the organ. The printed gland was then transplanted into a mouse whose own organ had been killed by targeted radiation. The implanted organ took root and began to work - albeit only by 50%, but this allowed the sufferer to live on.
“Thus, for the first time in the world, a functional, vascularized (that is, with vessels) mouse organ has been printed,” Vladimir Mironov minted every word.
This was the fourth achievement.
And here we come to the fifth, but the first most spectacular achievement of the laboratory 3D Bioprinting Solutions.
“We created an organ in space,” Professor Mironov effectively concludes the story.
— Why?
“It's all about weightlessness,” he replies.
There is a magnetic levitation, that is, in a floating state, bioassembly: the object is created not from the bottom up, but from all sides at once. The installation, which creates the necessary magnetic field, operates in the Dutch city of Nijmegen. 3D Bioprinting Solutions won a grant and received five days to install. Everything went great. But the electricity for the experiments took so much that it would be enough for the whole of Nijmegen. It became clear that an alternative method was needed.
Space, Professor Mironov understood. In two years, a bioprinter with six magnets instead of two was created, it received the name “Organ. Aut". Roscosmos supported the idea, and in October 2018 the bioprinter went into space on the Soyuz-10 spacecraft. Alas, it was an emergency launch. The astronauts, fortunately, managed to evacuate, and the remains of Organ. Avta can now be seen on display in the laboratory, they will soon be transferred to the Museum of Cosmonautics.
“Can you imagine our situation? Two years of work!” the professor winces.
But by December, in just two months, 3D Bioprinting Solutions had made a new Organ. Aut". And for the first time in the world, human cartilage and the thyroid gland of a mouse were printed in space using magnetic levitation on a 3D printer.
Professor Mironov had to hear many skeptical comments after the results of the experiment were made public: is it advisable to use such resources? And the criticism can not be called unfounded. But Vladimir Mironov explains: space technology is the 22nd century, European and American colleagues spend huge amounts of money on such projects, we must not fall behind!
But Vladimir Mironov explains: space technology is the 22nd century, European and American colleagues spend huge amounts of money on such projects, we must not fall behind!
And the value of a printed organ in the conditions of a catastrophic shortage of donor organs is cosmically high. Now patients are waiting for a transplant for several years - and they do not always wait, complains the director of the National Medical Research Center for Transplantology and Artificial Organs. Academician V. I. Shumakov Sergei Gauthier: “If bioprinting helps us create new organs as quickly as required, I will only support it. But so far, although there are successes, they are quite far from the final success. The mouse thyroid gland is undoubtedly a big step forward, but it should not be confused with a full-fledged human organ, even if only because of its size.”
Bioprinting will only make sense if the organ is printed directly from the patient's cells, academician Gauthier is sure: “If the organ is initially created from foreign cells, then for the patient, from the point of view of both ethical and purely medical aspects, it will be just as alien organ, as in organ donation.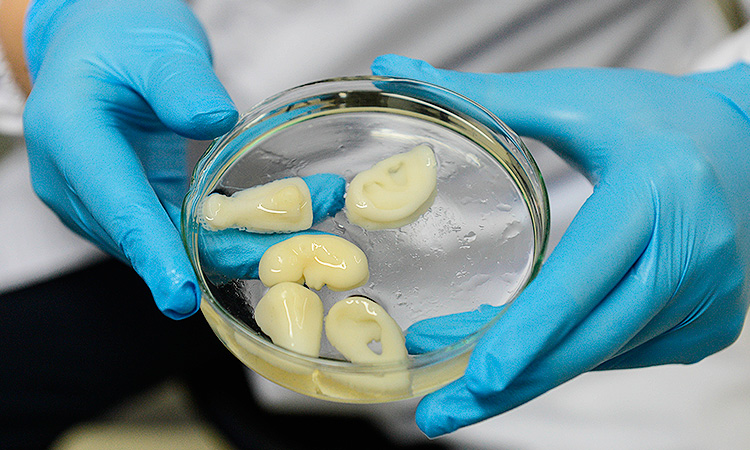 Although, in my opinion, bioprinting does not solve the ethical issue of transplantology simply because this issue simply does not exist, the ethics of transplantation is an international and generally recognized concept. Bioprinting should solve the problem of shortage of donor organs.”
Although, in my opinion, bioprinting does not solve the ethical issue of transplantology simply because this issue simply does not exist, the ethics of transplantation is an international and generally recognized concept. Bioprinting should solve the problem of shortage of donor organs.”
Of course, not only Professor Mironov has the results: in April, Israeli scientists managed to print a real heart exactly as Academician Gauthier says - from the patient's fat cells, which were converted into heart muscle stem cells, and then mixed with connective tissue and placed in a 3D printer.
Here the professor expresses skepticism: “Firstly, in their article, Israeli scientists call the heart personalized, although it is about two and a half centimeters in size, which corresponds to the size of a rabbit's heart. Is the rabbit a person? Secondly, so far it is just a piece of meat, not suitable for transplantation, or for anything else. No experiments have been done to confirm that the heart can function successfully. ”
”
— Why do we have an atomic bomb? - Vladimir Mironov asks a rhetorical question. - Because the state invested huge resources in its creation, and scientists were given opportunities and means for serious work. In China alone, two and a half million people are waiting for organ transplants. What kind of market is this? And we can take over a large part of this market. We have smart young people, we have experience and understanding of where and how to develop. The only thing missing is sufficient financial support!
— All hope for the state?
— Well, why is it necessary for the state? What, we have few wealthy people?
— And if there is enough funding, then when will we be able to...
— You understand, — Vladimir Mironov interrupts, — it's hard to answer this question, and I really don't like it when people ask me it. We work at the level of the Nobel Prize, but we will never get it. But the more active the funding is, the sooner the day will come when a 3D-printed organ will be successfully transplanted into a human. And whoever does this will have every chance of winning the Nobel Prize.
And whoever does this will have every chance of winning the Nobel Prize.
Yousef Hesuani, co-founder and managing partner of 3D Bioprinting Solutions, gave a more specific answer to this question: “I have less faith in private investors. Still, the time when their investments can pay off is still quite far away. Therefore, in my opinion, the state should play a leading role here.”
According to Mr. Khesuani, countries like South Korea or Singapore should be followed, where there are whole government programs to support young scientists involved in bioprinting research.
— When do you think, with sufficient funding, when will a printed organ be successfully transplanted into a human?
“It's hard to say exactly, but, according to rough estimates, by 2030,” he says.
Vladimir Mironov actually sees the same prospects as Khesuani: “My dream is to create a Russian national bioprinting center, in ten years to be the first in the world to print a functional, vascularized human organ and successfully transplant it into a patient. ”
”
Kuzma Lebedev
Print the liver | Articles
3D bioprinting is one of the hottest topics in modern transplantology. First of all, this fact confirms: the analytical companies Gartner and RBC, as well as the largest American advertising agency JWT, included bioprinting in the rating of the most innovative technologies. Izvestia tried to figure out whether the "printing" of organs would be an important step that would allow doctors around the world to make significant progress in growing artificial tissues and organs. Or can such experiments still be attributed to single scientific experiments?
To begin with, a few high-profile sensations of recent months: in early July, researchers from the universities of Sydney, Harvard, Stanford and the Massachusetts Institute of Technology printed an artificial vascular network on a 3D bioprinter that completely replicates the human circulatory system. Shortly before this, doctors from the American hospitals of St.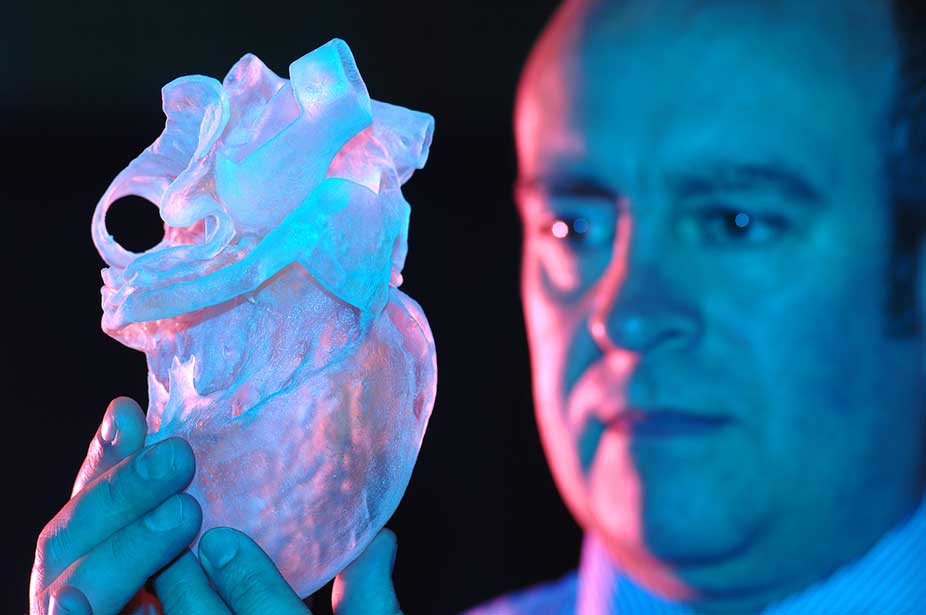 Luke and Roosevelt created a model of an artificial trachea in the same way. Foreign scientists highly appreciate the results of their work.
Luke and Roosevelt created a model of an artificial trachea in the same way. Foreign scientists highly appreciate the results of their work.
“One of the biggest challenges in creating large tissues and organs is growing a network of blood vessels and capillaries,” says Dr. Luis Bertassoni from the University of Sydney. “As a result, thousands of people die each year due to a lack of organs for transplantation. And now just imagine that you are able to come to the hospital and print the desired organ with all the cells, proteins and blood vessels, just by pressing the print button on the computer. And our discovery is an important new step towards achieving this goal.”
Quickly affects, but takes a long time
In general, the enthusiasm of Western colleagues is also supported by domestic doctors, but with some reservations. “The actively developing technology for growing tissues and organs using a 3D printer is not yet applicable to all parts of the human body,” comments Alexei Zhao, surgeon, MD, deputy director of the A.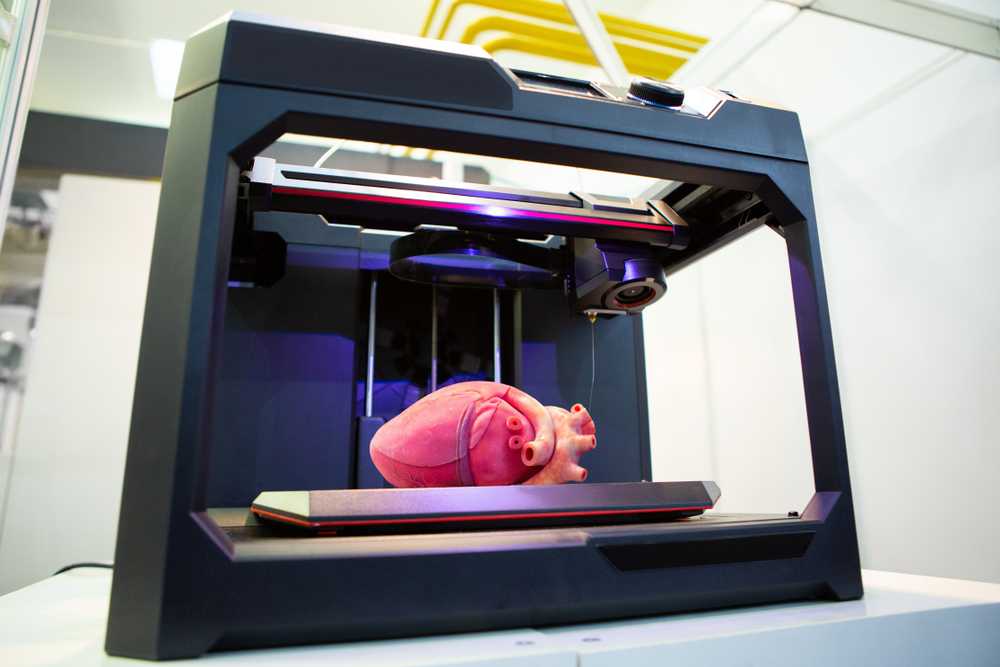 V. Vishnevsky on scientific work. - Yes, you can print the trachea, blood vessels, bone tissue, bladder tissue. But creating a heart, liver or kidneys with a printer is much more difficult, although in theory this is possible.
V. Vishnevsky on scientific work. - Yes, you can print the trachea, blood vessels, bone tissue, bladder tissue. But creating a heart, liver or kidneys with a printer is much more difficult, although in theory this is possible.
According to him, there has not yet been a single case of transplantation of artificial organs grown from stem cells in this way in Russia. “Like in all countries of the world, we are carrying out numerous developments,” said Alexey Zhao. “Yes, bioprostheses are already being used, but we have not yet learned how to clearly model tissues and organs according to individual sizes and transplant them even into animals.”
There are no examples of organs transplanted from stem cells to people in other countries. So, at the end of last year, Organovo scientists announced that they had managed to create an artificial liver using a 3D printer, which fully functioned for 40 days. However, according to Mike Renard, vice president of Organovo, the created liver, although excellent for drug testing, was still not ready for human transplantation.
Away with donors - the way for printers?
“The principle of operation of a bioprinter is based on cell fusion,” explains Vladimir Mironov, tissue engineer, author of the world's first publication on organ printing, scientific director of the Russian company 3D Bioprinting Solutions. - This principle was discovered by a scientist named Bohr, who conducted an experiment with tadpoles. During the experiment, his wife came into his office and called the scientist to dinner. After dinner, Bohr completely forgot that he had left the tadpoles on his desk. In the morning it turned out that they had grown together. But this is background. The very idea of creating artificial organs using bioprinting has been in the air for the last 15–20 years. At first, such machines were used to "print" ceramics, polymers, titanium particles. My idea was to start using living cells in printers.”
How are artificial body parts created in a bioprinter?
Initially, stem cells are taken from the patient in the laboratory.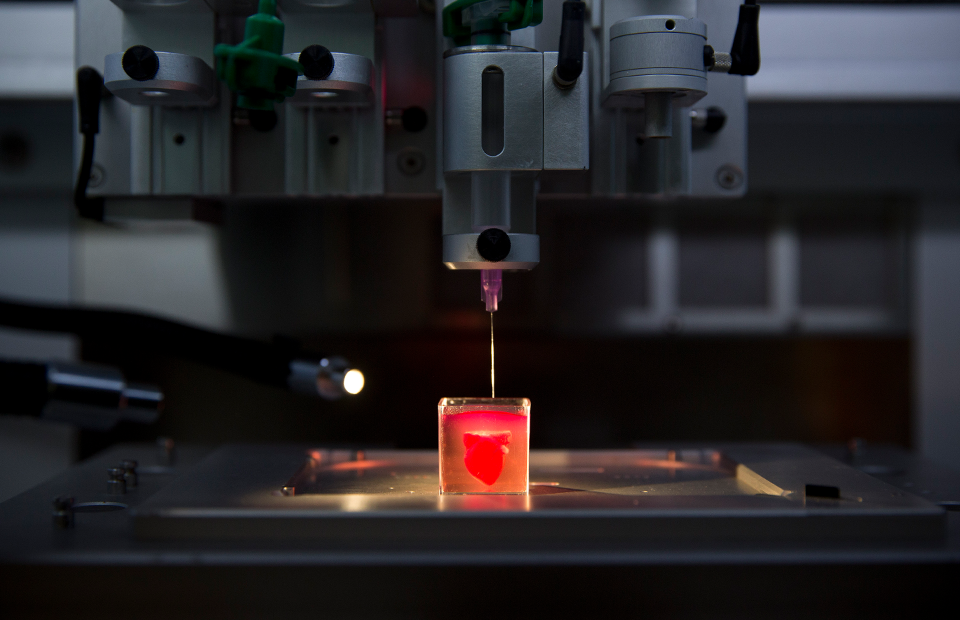 They are used to make spheroids: balls placed in a hydrogel, which later merge vertically and horizontally, forming a three-dimensional model of the desired organ. When the model is ready, it is converted into a special file. This file is given to a 3D printer, which can, relatively speaking, print cells and understands at what point in three-dimensional space it needs to “put” a particular type of cell. As a result of such “printing”, a certain sample of fabric is obtained. Then everything is simple: the sample is placed in a special bioreactor, where it matures, after which it can be transplanted to the patient.
They are used to make spheroids: balls placed in a hydrogel, which later merge vertically and horizontally, forming a three-dimensional model of the desired organ. When the model is ready, it is converted into a special file. This file is given to a 3D printer, which can, relatively speaking, print cells and understands at what point in three-dimensional space it needs to “put” a particular type of cell. As a result of such “printing”, a certain sample of fabric is obtained. Then everything is simple: the sample is placed in a special bioreactor, where it matures, after which it can be transplanted to the patient.
According to Vladimir Mironov, the advantages of bioprinters are obvious. In order to receive an artificial organ, the patient does not need to look for and wait for a donor, which greatly increases his chances of recovery: an organ can be printed in 30 minutes. More precisely, not an organ, but a tissue-engineering structure, which then needs to be placed in a bioreactor. Another advantage is that the printers do not use inorganic scaffolds, which are needed in order to maintain the shape of an artificial organ.
Another advantage is that the printers do not use inorganic scaffolds, which are needed in order to maintain the shape of an artificial organ.
“We want to print human organs, or at least the functional parts of human organs,” the engineer shared his plans. “This method is different from tissue engineering, because our goal is not just to create 3D tissues, but rather 3D parts of living human organs, primarily the liver and kidney. This is the next level of complexity in the hierarchical structure of the organization of the human body.”
Beautiful is far…
As experience shows, almost every innovation immediately acquires supporters and opponents. Surprisingly, the real benefits of using bioprinters are recognized by all members of the medical community. Another thing is that many of them are extremely skeptical that such a high-tech machine will ever appear that can accurately reproduce the unique parts of the human body. And even if it appears, how much will such a miracle device cost?. .
.
“The advantages of 3D printing of organs are obvious, only they will be printed in 100 years,” notes Igor Pogrebnichenko, Professor, Head of the Organ Donation Coordination Department of the Federal Scientific Center for Transplantology and Artificial Organs. ak. IN AND. Shumakov. “Already now, in principle, any organ can be printed, but not one of them lives. Why? Because growing an organ is not like making a wooden prosthesis. Speaking of living tissues, we are dealing with incredibly complex structural elements.”
As the specialist emphasizes, in order to maintain life, their cells need constant access to nutrients, oxygen and an efficient system of "waste disposal". Cells die without adequate blood flow as the blood carries the oxygen necessary for them to grow and perform their various functions in the body. “It is not as easy to artificially recreate such processes as it seems, therefore, for now, bioprinters remain something from the realm of fantasy and are very far from the real state of medicine,” the professor concludes.
...and still expensive
Igor Pogrebnichenko refused to suggest even approximate prices for bioprinters and printed organs. “Until there is a well-established technology, it cannot be assessed in terms of cost,” he replied. At the same time, the problem of determining the exact cost of 3D printers lies in the fact that there is no competition in this market yet. So, a Swiss printer costs $500,000, and a German printer costs the same. The American one is twice cheaper, about $200-250 thousand, but it is inferior in quality by the same amount. At the same time, ordinary 3D printers cost a penny compared to their biobrothers.
“A regular printer now costs about $70,” calculates Vladimir Mironov. - It works along the X and Y coordinate axes, that is, when printing, it "travels" to the right and left. We add the third coordinate axis - Z - this is about another $50 in monetary terms. This is the real cost of a 3D printer. Nevertheless, the cheapest models so far cost no less than $300. And if bioprinters cost the same, it would be a real salvation, because every day almost twenty people die from those who are waiting for a donor to appear for them.” Plus, if bioprinters become publicly available, then the state will also benefit. So, for each patient with a transplanted artificial kidney, in total it will be possible to save almost $500,000 for every ten years of his life.
And if bioprinters cost the same, it would be a real salvation, because every day almost twenty people die from those who are waiting for a donor to appear for them.” Plus, if bioprinters become publicly available, then the state will also benefit. So, for each patient with a transplanted artificial kidney, in total it will be possible to save almost $500,000 for every ten years of his life.
The race of scientists for the common good
The real benefit that the state will receive from the large-scale introduction of bioprinters is not limited to dry numbers in the annual estimate. Thus, the state that will be able to launch bioprinters into mass production faster than others and begin to actively introduce them into the work of medical institutions will be able to make a big leap in the most prestigious - innovative - rating of countries. The fact is that the large-scale creation of living human organs is the ultimate goal of all regenerative medicine, and 3D bioprinting is considered the fastest and most promising way.