3D printed hearts
How Close Are We To Working 3D Printed Hearts?
What do you think the leading cause of death in the USA is? Here’s a clue, it’s not cancer.
That dark accolade instead goes to heart disease and cardiovascular problems, fueled by soft drinks and obesity. Over 26 million people suffer from heart failure worldwide, and 1 in 3 deaths are caused by heart problems.
The problem is there are just not enough hearts. Transplant organs are usually taken from car crash victim donors, but there is still a sizable waiting list which can take years.
Receiving a new heart doesn’t guarantee a full life either: organ recipients often die within 10 years of the transplant, either because the body rejects the new heart or the anti-rejection drugs suppress the immune system, increasing risk of illnesses such as cancer.
- If you find 3D bioprinting and 3D printed organs interesting, check out our full guide to 3D printed organs.
3D Printed Hearts: The Solution
This is where 3D bioprinting may be able to assist. The ability to 3D print an identical heart to yours, and from your own cells, erases the risk of rejection and the need to take these drugs.
But is this really possible? Can we just manufacture working human organs from thin air? This article involves extensive research into the area, and will seek to explain this in full detail, comprising two parts:
- Part 1: Research into 3D printing biological hearts made from human tissue that are exact replicas of existing hearts.
- Part 2: Research into 3D printing artificial hearts that would replace faulty hearts and beat artificially, made from silicone.
Advantages of 3D printed hearts
How to 3D Print a Heart: A short introduction
3D printing used to be limited to a few plastics like PLA and ABS, but now you can 3D print metal, and even living cells. Printing living cells into working tissues is how we aim to create 3D printed hearts.
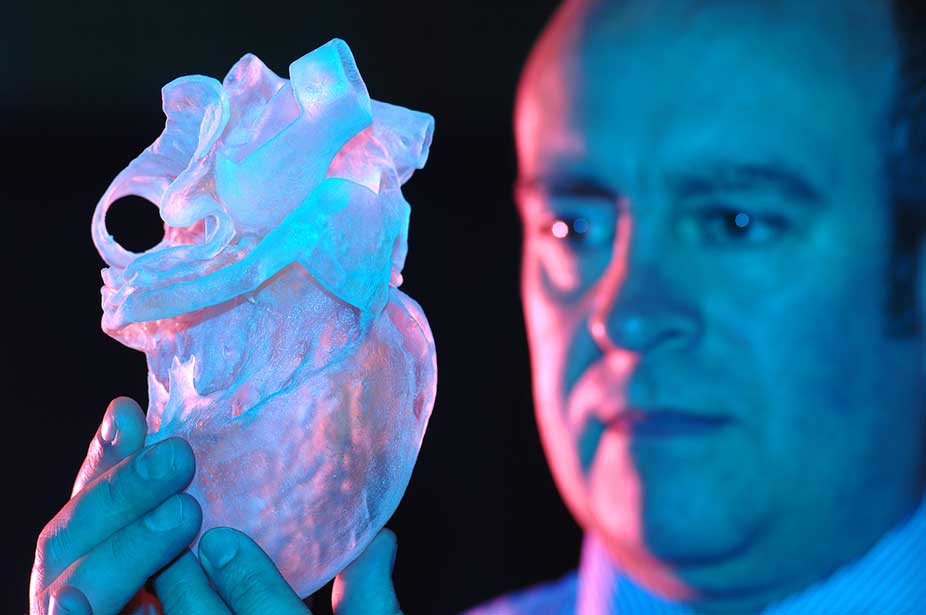
Stage 1: Scan the heart — To create an exact replica of the patient’s heart, you need to know the exact dimensions of the patient’s heart. This can be done via an MRI scan to create a digital 3D printed heart model.
This can be done via an MRI scan to create a digital 3D printed heart model.
Stage 2: Create the heart — Cells such as blood cells are taken from the patient — key to the body not interpreting the organ as foreign and rejecting it — and converted into stem cells, and infused within a bio-ink to be 3D bioprinted.
Stage 3: Transplant the heart — This has never been done before, but once a functional 3D printed heart is printed, it could be transplanted into a living patient.Another 3D printed heart design.
The process below does not yet work fully, and is still partly theoretical:
The most efficient way we currently know of to 3D print hearts is with a scaffold in place which defines the areas which the bio-ink and heart cells are to be printed in. Once the shape has been printed, this scaffold keeps the cells where they should be, allowing them to assemble into heart tissue. Miraculously, heart cells will just come together when in proximity, and will eventually start beating like a real heart does!
When the heart is mature enough to function without a scaffold, it is heated and melted off. This finished heart can then be transplanted into the patient with no chance of rejection and no need for anti-rejection drugs.
This finished heart can then be transplanted into the patient with no chance of rejection and no need for anti-rejection drugs.
Companies such as BioLife4D and Cellink both follow this philosophy, believing that creating real 3D printed hearts from native tissue is the way forward. We are currently able to create small tissues with a patient’s cells, and it does beat.
But there are problems on the very small scale. Capillaries are just one blood cell thick, and are plentiful inside the human body. No 3D printer on the planet can accurately print anywhere near that scale, yet.
Part 1: 3D Printed Hearts Made From Real Human Cells
The following examples are from companies and research facilities at institutions such as universities, that have made key discoveries that move us closer to 3D printed transplantable hearts.
Organovo: The company trying to 3D print hearts
A prominent company in the 3D printed heart and 3D printed organ space is Organovo. Founded in 2007 in San Diego, CA, Organovo design and create human tissues with 3D bioprinting and aim to create living human tissues that function identically to native tissues. The company has pioneered many of the bioprinting techniques known today.
The company has pioneered many of the bioprinting techniques known today.
Organovo’s first breakthrough came in 2009 when they created the first 3D bioprinted blood vessel. Since blood vessels are some of the main building blocks to creating organs (and therefore a successful 3D printed heart transplant), this was a tremendous achievement.
Organovo went on to develop 3D printed liver tissue, as well as partnering with L’Oreal to develop 3D printed skin tissue in 2015. They weren’t the only company trying to create 3D printed hearts and organs however, as companies such as Cellink, Biolife4D, EnvisionTEC, and more either build 3D bioprinters or research ways of printing organs.
Tel Aviv University 3D printed mini heart
At Tel Aviv University’s School of Molecular Cell Biology & Biotechnology in April 2019, a team 3D printed a small heart using human tissue, including working blood vessels. The 3D printed miniature heart does not pump or function yet, but does contract like a heart does. Tal Dvir, the lead scientist on the project, says it is the first time an entire heart with cells, blood vessels, ventricles and chambers has been printed.
The 3D printed miniature heart does not pump or function yet, but does contract like a heart does. Tal Dvir, the lead scientist on the project, says it is the first time an entire heart with cells, blood vessels, ventricles and chambers has been printed.
It is very small, around the size of a large rodent’s heart, but it is key progress towards a full-size, transplantable 3D printed heart. The heart was created using bioinks created by taking a biopsy of omental tissues from a human patient, separating the cellular and non-cellular components and reprogramming the cells to become stem cells, and then into cardiac or endothelial cells.
The plan now is to scale up to a human heart, which the team do not believe would require any different technology than they already have. They do however need to manage to make the hearts work and beat like a functional heart before they can start transplanting these hearts into patients.
- Read more about the project here.
 The small size is clear in relation to a human hand.
The small size is clear in relation to a human hand.BioLife4D
BioLife4D have a game plan for reaching a stage where 3D printed hearts will become a reality. The belief is that pharmaceutical companies will use these printable-on-demand hearts to test new drugs and their effects. Once this preliminary stage has been completed, BioLife4D intend to move on to making small animal hearts. Then, they will gravitate toward large animals, before making the eventual leap to real 3D printed human hearts.
Their first big breakthrough in 3D printed hearts was the printing of a patch of human heart tissue in 2018 capable of contracting like a heart does. Though just a patch of tissue, this is already enough for important surgeries whereby implanting strips of heart tissue onto the hearts of patients with acute heart failure can have parts of this damaged heart restored.
In September 2019, BioLife4D fulfilled their promise to produce a mini 3D printed heart, replicating many of the features of a human heart.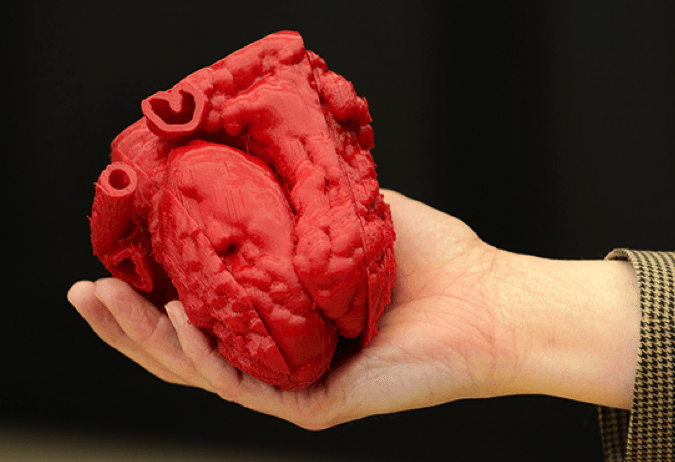 They believe that with this miniature version created, it is only a matter of time before they are able to scale up to a functional, human-size heart that can be transplanted into people.
They believe that with this miniature version created, it is only a matter of time before they are able to scale up to a functional, human-size heart that can be transplanted into people.
SWIFT — A New way of 3D printing hearts
At the Harvard Lewis Lab, SWIFT (sacrificial writing into functional tissue) promises to completely change how we use 3D bioprinting to save lives. The process involves taking human cells from patients and transforming them via stem cells into cardiac cells. These cells are packed together, and 3D printed vascular structures are then printed in gelatin ink into them, to create a channel network that mimics the structure of real-life human vascular networks.
The gelatin ink is then heated out of the mix, leaving just the vascular channel replicas within the tissue. These parts can then be linked with endothelial cells (the cells that line blood vessels) to mimic these blood vessels and help deliver oxygen.
Most excitingly, this discovery isn’t limited to just 3D printed hearts. Other organs with similar structures can also be created, and stem cells are so versatile that the system would not need to be overly tweaked for other functions.
Other organs with similar structures can also be created, and stem cells are so versatile that the system would not need to be overly tweaked for other functions.
The lab managed to create a strip of heart tissue slightly taller than a centimeter, and it managed to beat like a living heart for 7 days. This shows real progress towards creating larger, and functional, 3D printed hearts.
There is another school of thought however. If a foreign object can fulfill the same role as a human heart does, do we really need a human heart at all? 3D printing can help here also.
- Read more about the project here.
Part 2: 3D Printed Artificial Hearts
We are better at manufacturing objects from materials such as plastics and metals than we are from living tissues; our cities and houses are evidence of that. By this logic, it should be simpler for us to build artificial hearts that can pump blood round our bodies in the event that our heart fails.
The heart’s job doesn’t sound that difficult; it’s just pumping blood.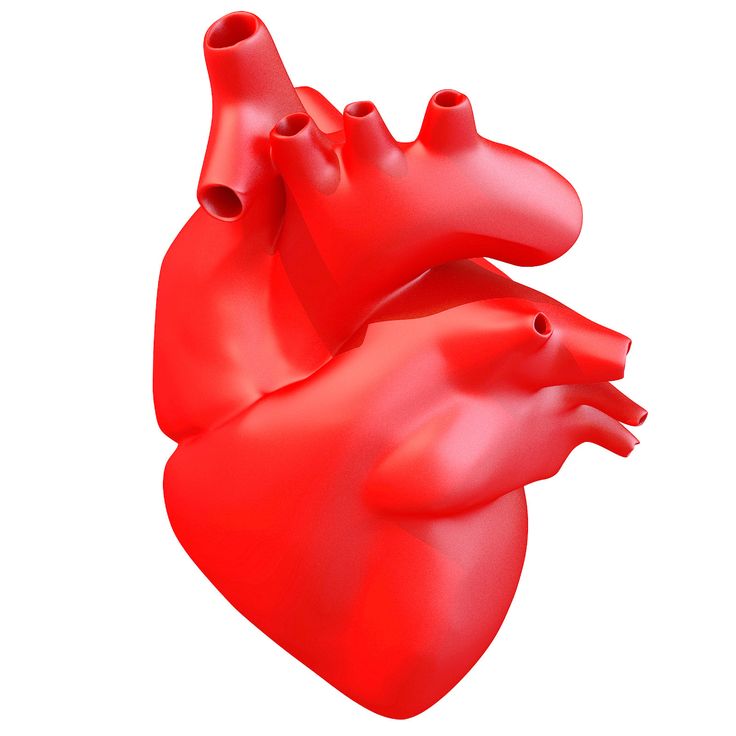 This shouldn’t be hard to do artificially, right? We can build skyscrapers and racecars, surely we can build a glorified pump?
This shouldn’t be hard to do artificially, right? We can build skyscrapers and racecars, surely we can build a glorified pump?
But alas no, it is not easy. Researchers at ETH Zurich found this out in July 2017.
ETH Zurich: 3D Printed Silicone Heart
Researchers at the Functional Materials Laboratory within ETH Zurich developed a silicone heart last year that beats almost like a human heart. There have been previous attempts to create artificial 3D printed hearts that work, but this is the first entirely soft artificial heart that pumps using pressurized air.
- We also have a guide to 3D printing silicone.
What’s more, the pumping mechanism mimics a real heart, and required no assembling. It was 3D printed as one large, assembled structure and includes a left and right ventricle. Only the input and output parts need to be attached post-print, where the blood is pumped in and out. It’s also the same size a human heart, so if perfectly it could be transplanted into humans. The silicone 3D printed heart designed to replace faulty human hearts.
The silicone 3D printed heart designed to replace faulty human hearts.
This extraordinary heart was developed by doctoral student Nicholas Cohrs — with a surname eerily similar to the French word for heart, coeur — and was led by Professor Wendelin Stark of Functional Materials at ETH. The heart was made from silicone using Lost Wax Casting, which is often used in the mold-making and 3D printed jewelry sectors. Weighing 390 grams, it is fairly similar to the weight of a real heart (310 grams), though this cloudy white contraption looks very alien.
3000 beats to heaven
When put under testing, ETH Zurich’s silicone heart lasted a few thousand beats before the material could no longer take the strain. Depending on your heart rate, this equates to between 30 and 45 minutes of human functioning. Therefore, it seems we still have a way to go before an artificial heart is possible.
We shouldn’t underestimate how dexterous our hearts are. They can work for a hundred years under the strain that our best alternatives cannot for an hour. Evolution is wonderful, and so is cardiac muscle. This does mean however that we are some way from a 3D printed heart implant.
Evolution is wonderful, and so is cardiac muscle. This does mean however that we are some way from a 3D printed heart implant.
Two years later in 2019, the same team designed 3D printed heart valves to replace damaged valves in patients. Unlike previous artificial heart valves, these 3D prints are formed from MRI scans to fit the patient perfectly, a key advantage over current transplantable valves.
ETH have shown that good progress has been made, so we have every reason to be positive. We must also however be humbled by the strength and power of our organs. They are temples, and we must treat them accordingly.
Conclusion: 3D printed hearts are several decades away
3D printed hearts offer an exciting alternative to current systems of organ donation. With self-driving cars promising to drop road accident deaths to a fraction of current levels, organs from donors is predicted to drop significantly. We need an alternative — and less demise-centered — way of harvesting organs, and 3D bioprinting could be what saves us.
It’s too early to tell how feasible this is, as fully developed organs are still far from reality. Though don’t dismiss it as sci-fi either, 3D printing is an exponential technology and prone to huge discoveries. The future is always exciting, and we will have to see what it presents us.
A conservative estimate for working 3D printed hearts is 30-50 years. This could all change if levels of investment change, or a sudden massive leap in progress occurs. It is handy that the heart is one of the simplest organs in the body however, as it fulfills no other role than to pump, pump, and pump some more.
Boston University's new 3D printed mini human heart beats on its own
0Shares
A research team led by Boston University has used 3D printing technology to develop a miniature replica of a human heart – and it beats like the real thing.
Named the cardiac miniaturized Precision-enabled Unidirectional Microfluidic Pump, aka the miniPUMP, the device was created using a combination of stem cell-derived human heart cells and micro-scale 3D printed acrylic parts. Designed to behave like a real heart chamber, the miniPUMP doesn’t rely on any external sources of power, instead beating by itself thanks to its live tissue.
Designed to behave like a real heart chamber, the miniPUMP doesn’t rely on any external sources of power, instead beating by itself thanks to its live tissue.
The researchers believe their heart chamber replica could serve as a testbed to study how the organ works in the human body. It can be used to track how the heart grows in an embryo, how heart tissue is affected by diseases, and how effective new medications are in treating said diseases, all without the need for human testing.
“We can study disease progression in a way that hasn’t been possible before,” says Alice White, a Boston University College of Engineering professor. “We chose to work on heart tissue because of its particularly complicated mechanics, but we showed that, when you take nanotechnology and marry it with tissue engineering, there’s potential for replicating this for multiple organs.”
Microscopic imaging of the miniPUMP and one of its internal 3D printed ‘blood vessels’. Image via Boston University.
The challenge of studying the heart
According to the Centers for Disease Control and Prevention, heart disease is the leading cause of death for both men and women in the US, with around 659,000 mortalities every year. That’s one in four deaths. As such, there’s an urgent need to study the vital organ.
However, due to its inaccessible location in the human body, the heart is a tricky thing to study as it can’t just be removed, examined, and replaced on a whim. To address this, researchers have tried several alternative approaches: they’ve manually pumped blood through cadaver hearts and they’ve spring-loaded lab-grown heart tissues to make them expand and contract. Unfortunately, we’re yet to find a suitable lifelike proxy as reanimated hearts can’t beat indefinitely and springs don’t contract like real muscle fibers.
With innovations like the miniPUMP, researchers could eventually mimic and study diseases such as hypertension and valve disease in a more accurate manner. The device is also expected to streamline the drug development process for upcoming medicines, enabling lab-based testing in lieu of costly and tedious human trials.
The device is also expected to streamline the drug development process for upcoming medicines, enabling lab-based testing in lieu of costly and tedious human trials.
How was the miniPUMP developed?
The miniPUMP measures just three square centimeters and features an acrylic scaffold 3D printed using two-photon direct laser writing, a very precise form of micro-SLA. The tiny acrylic valves within open and close to control the flow of fluid, while the miniature tubes serve as arteries and veins. To make the device beat, the researchers also integrated heart muscle cells called cardiomyocytes, which were differentiated from pluripotent stem cells.
The decision to make the miniPUMP so small was a deliberate one, as the 3D printed acrylic scaffolds had to be strong enough to support the structure but thin enough to bend and move with the contracting heart tissue.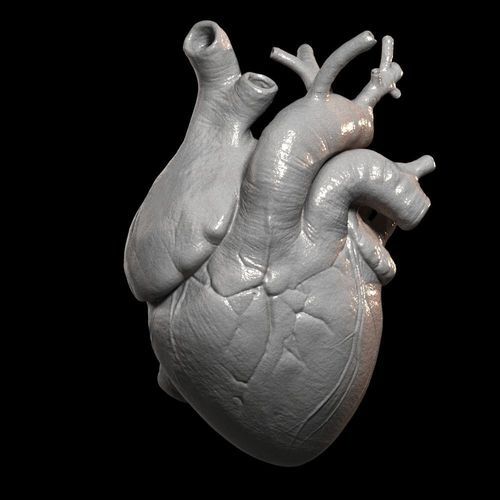
“The structural elements are so fine that things that would ordinarily be stiff are flexible,” adds White. “By analogy, think about optical fiber: a glass window is very stiff, but you can wrap a glass optical fiber around your finger. Acrylic can be very stiff, but at the scale involved in the miniPUMP, the acrylic scaffold is able to be compressed by the beating cardiomyocytes.”
As far as next steps go, the miniPUMP research team aims to refine the technology and find ways of manufacturing it reliably. The work can also eventually be applied to implantable patches that may fix defects in the heart, as well as other organs such as livers.
The project is being conducted as part of CELL-MET, a joint National Science Foundation Engineering Research Center in Cellular Metamaterials led by Boston University. The center’s ultimate goal is to create devices capable of regenerating diseased human heart tissue.
A side view image of the miniPUMP being taken in the lab. The scaffold that gives structure to the heart cells can be seen through the tissue. Photo via Jackie Ricciardi.
Photo via Jackie Ricciardi.The 3D printing of human heart replicas and models is something we’ve seen before. Just last month, researchers from the Technical University of Munich (TUM) and the University of Western Australia developed 3D printed artificial heart valves made from a patient’s own cells that grow as the individual ages. The approach hopes to overcome the drawbacks of conventional prosthetic heart valves, which only last a limited number of years and therefore require multiple replacement surgeries.
Elsewhere, researchers from the Chinese Academy of Sciences (CAS) recently converted a six-axis robotic arm into a 3D bioprinter and used it to fabricate a complex-shaped blood vessel scaffold. The 3D printed vascularized heart tissue remained alive and beating for six months, and could demonstrate a feasible method of bioprinting functional tissues and organs in the future.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter, liking us on Facebook, and tuning into the 3D Printing Industry YouTube Channel.
You can also stay connected by following us on Twitter, liking us on Facebook, and tuning into the 3D Printing Industry YouTube Channel.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows a side view image of the miniPUMP being taken in the lab. Photo via Jackie Ricciardi.
Tags Alice White Boston University CELL-MET miniPUMP
Kubi Sertoglu
Kubi Sertoglu holds a degree in Mechanical Engineering, combining an affinity for writing with a technical background to deliver the latest news and reviews in additive manufacturing.
Living heart printed on a 3D printer - Kommersant FM - Kommersant
In Israel, for the first time in the world, a living heart was created on a 3D printer, which consists of tissues and blood vessels, and also has cameras. True, at the moment it can only suit a rabbit because of its small size. But scientists from the University of Tel Aviv are confident that in the future they will be able to print a heart for a person. How did you manage to create an organ on the printer? And can we talk about a revolution in medicine? Anna Nikitina and Gleb Silko will tell.
But scientists from the University of Tel Aviv are confident that in the future they will be able to print a heart for a person. How did you manage to create an organ on the printer? And can we talk about a revolution in medicine? Anna Nikitina and Gleb Silko will tell.
Photo: Yaroslav Chingaev, Kommersant / buy photo
The world's first 3D-printed heart resembles a berry: its size is about 2.5 cm, although it took more than three hours to print. However, even now the achievement of Israeli scientists is called a medical breakthrough. The heart is made from human fat cells and connective tissue. Previously, synthetic substances were used for this.
In the future, this new technology will not only solve the problem of the shortage of organs for transplantation, but will also facilitate the transplantation process as much as possible, says Israeli journalist Sasha Vilensky: “The most global problem is the rejection of a transplanted organ by the body. There is always such a danger. But the whole point of interest is that in the case of a 3D printer, we are dealing with what is grown and printed from the cells of the patient himself, thus simply removing the issue of rejection. This is genius".
There is always such a danger. But the whole point of interest is that in the case of a 3D printer, we are dealing with what is grown and printed from the cells of the patient himself, thus simply removing the issue of rejection. This is genius".
The problem of organ shortages around the world is really acute. In Russia, for example, in 2017, there were only 900 donors per 6 million people. And the most complex organ - the heart - was transplanted 250 times in a year, while it required almost 2 million people. The experience of Israeli scientists in printing hearts is impressive, and it can be used in other countries, says Yousef Hesuani, executive director of the 3D Bioprinting Solutions laboratory. True, according to him, it is still too early to talk about a revolution in medicine: “Scientists have used a very interesting material based on collagen - this is a protein in the body of mammals. In addition, it is from the point of view of creating a complex three-dimensional structure that the researchers are great, they did a really good job. However, the form does not yet determine the function, especially if we are talking about such a complex organ as the heart.
New approaches have been used, but unfortunately it is too early to say that there has been an incredible breakthrough in this area.
When, for example, the native organ is removed and a new one is transplanted, and the function is fully restored, this will become an unconditional revolution.”
Tel Aviv University itself, where the heart was printed, says that in the future the necessary organs can be printed directly in hospitals. Now similar developments are being carried out all over the world. Russian companies, for example, are trying to create an artificial liver and kidneys. True, this process is too expensive, and it is unlikely that in the near future the technology will be introduced on a mass level, says the director of the National Medical Center for Transplantation and Artificial Organs. Shumakova Sergei Gauthier: “What the Israeli doctors did is just great. This proves that these possibilities can really be used to create some kind of anatomical structures. As for other organs, such as the kidney and liver, our institute is also working on this. We also have bioprinters, but frankly, growing such tissue complexes is a rather complicated and expensive technology, which is very different from the traditional method of organ transplantation.”
This proves that these possibilities can really be used to create some kind of anatomical structures. As for other organs, such as the kidney and liver, our institute is also working on this. We also have bioprinters, but frankly, growing such tissue complexes is a rather complicated and expensive technology, which is very different from the traditional method of organ transplantation.”
There are already examples in the world when doctors managed not only to create artificial organs on a 3D printer, but also successfully transplant them, for example, a few years ago in Russia a thyroid gland was printed, which took root in a patient. And last year, scientists from Jerusalem implanted a prosthesis for the skull on a patient, and it was also created using three-dimensional technologies.
During this year, Israeli scientists plan to test printed hearts on rabbits and rats, and then start working on creating a human heart.
3D printed heart saved 4-year-old Mia Gonzalez / Habr
Welcome to the iCover blog. In surgery, there are cases when the task facing the specialist allows the use of several surgical methods. And only one of them is the most correct. 3D technologies helped the specialists of the Nicklaus Cardiovascular Center Clinic in Miami to find and make such a decision. About 4-year-old Mia Gonzalez, whose health was restored thanks to a 3D printer and the prospects for a new approach to surgery using the capabilities of 3D prototyping, we will tell in our article.
In surgery, there are cases when the task facing the specialist allows the use of several surgical methods. And only one of them is the most correct. 3D technologies helped the specialists of the Nicklaus Cardiovascular Center Clinic in Miami to find and make such a decision. About 4-year-old Mia Gonzalez, whose health was restored thanks to a 3D printer and the prospects for a new approach to surgery using the capabilities of 3D prototyping, we will tell in our article.
Little Mia Gonzalez was destined to meet the first serious trials in the first years of her life. And to be exact, the first 3.5 years, during which she underwent at least 10 hospitalizations, turned into one continuous test for the girl. Endless pathological colds and runny noses, which became her faithful companions, completely deprived the baby of her usual childhood joys. In recent months, to support respiratory functions at a vital level, the girl had to take special medications.
Examinations done during Mia's stay at the local clinic led the doctors to a disappointing conclusion: the child suffers from a rare pathology called "double aorta", the incorrect position of which leads to compression of the trachea and, as a result, problems with breathing and swallowing. The conclusion of the doctors shocked the parents: 4-year-old Mia will need open-heart surgery to correct the aorta to bring the situation under control.
The conclusion of the doctors shocked the parents: 4-year-old Mia will need open-heart surgery to correct the aorta to bring the situation under control.
The complexity and non-standard nature of the case served as a reason for doctors to turn to innovative 3D printing technologies for help. A 3D-printed model of Mia's heart helped to find the only correct solution from the intricate labyrinth of equiprobable outcomes.
Augmented Reality Mia
The latest 3D printer, which the Niklaus Children's Cardiovascular Surgery Clinic in Miami received in 2015, has already been used to print exact copies of the organs of 25 children with congenital heart defects who need complex surgical treatment. The ability to accurately visualize organs subject to surgical intervention “in the original”, taking into account all the individual characteristics of the patient, allowed Dr. Burke to find and make decisions that, according to him, he would never have dared to be guided only by logic, knowledge and accumulated experience. And the results of this approach exceeded all expectations.
And the results of this approach exceeded all expectations.
As in the previous cases, an in-depth analysis of the situation was preceded by making an exact copy of the girl's heart affected by pathological changes. As in the case of previous patients, MRI and CT scan data were used as an “information template” for printing Mia’s heart model, and plastic or rubber was used as the starting material.
It took Redmond Burke, the leading surgeon of the clinic, more than two weeks to plan the operation and find the most gentle technology. And here, again, an invaluable help was provided by the exact prototype made, with which the doctor often went to his colleagues to clarify some ambiguous question. As a result, reflections on Mia's case and the accumulated useful information formed the basis of a non-standard decision - to make an incision not on the left side of the sternum, as prescribed in such cases, but on the right. This, according to Burke, greatly increased the chances of baby Mia for a successful operation and a speedy postoperative rehabilitation.
"If not for this model, I would have had to make a larger incision, which could have made the girl suffer much more, and also require more time for rehabilitation," Burke said, adding that it helped to put aside any doubts when making a decision, mainly the 3D printer.
Method prospects
Despite the fact that the method used in the operational practice of the Niklaus Clinic does not involve printing and replacing a biological organ, an exact prototype in many cases will eliminate the need for transplantation, limiting itself to local surgical intervention. According to information provided by Scott Rader, general manager of Stratasys, which supplies 3D printers to the world market, today there are already 200 such models in operation in the world and 75 of them are in US clinics.
Until recently, the use of 3D printing in medicine was limited to prototyping surgical instruments and performing some simple operations. And only in the last few years, the proposed technologies have made it possible to print exact copies of the organs of patients using the results of hardware laboratory studies. Printed prototypes, according to Rader, are an indispensable tool for complex operations, which include the removal of a brain tumor. The modeling of pathologies in the organs of complex patients also opens up excellent prospects for use within the walls of medical universities.
Printed prototypes, according to Rader, are an indispensable tool for complex operations, which include the removal of a brain tumor. The modeling of pathologies in the organs of complex patients also opens up excellent prospects for use within the walls of medical universities.
“It is very important that having a prototype organ of a patient who is preparing for surgery at his disposal, the surgeon has a unique opportunity to practice the technique of surgical intervention on the model as many times as necessary in order to find the best option,” says Reider.
In the coming years, according to Scott Rader, surgeons will be able to print new organs for people on printers, using “ink” based on human cells instead of plastic and rubber. But 3D printed organ imitation is certainly “a breakthrough technology that is fundamentally affecting how we communicate with patients, how we prepare for surgery, how we do it, and how we educate medical students,” says the Harvard professor. medical school and member of the Simulation Science Circle at Beth Israel Deaconess Medical Center in Boston, Daniel W. Jones.
medical school and member of the Simulation Science Circle at Beth Israel Deaconess Medical Center in Boston, Daniel W. Jones.
Selling 200 printers worldwide is a drop in the ocean. Today, the situation is more like “… a big secret, kept in deep secrecy,” says Dr. Jones, who has devoted all his time to studying the views of surgeons on the new technology. At the same time, the situation with its implementation inspires optimism, since the cost of equipment becomes more affordable, and the results achieved should be recognized as the most convincing argument.
“A similar 3D printer and related software typically cost up to $100,000, which is less than a CT or MRI lab suite,” says Scott Reider. And taking into account the indicators of the effectiveness of surgical treatment and the reduction of the time required for the operation and rehabilitation of the patient, the use of 3D organ prototyping technology opens up the most brilliant prospects.
It's been 4 months since Mia's surgery.