3D printers las vegas
3D Printing Service Las Vegas
High quality and large scale 3D printing service in Las Vegas. Get high quality parts without the headache.
No signup required.
Contact us
What makes PrintAWorld different from the other Las Vegas 3D printing companies out there
Get high quality parts
Our SLA 3d printer can print high resolution parts that other large format printers can only dream of.
Fast turnaround
We know how tough deadlines can be. Let us know and we'll do our best to get your project done in no time.
Get expert help
From ideation, design to production, we'll help you every step of the way.
Some of the work that we did for our clients in Las Vegas
How our 3D printing service in Las Vegas works
0
1
.
Send us a few information
The material you need, quantities and a short description of your project.
If you're unsure, don't sweat it. We will guide you to the perfect solution!
0
2
.
Upload a 3D File
Send us your.stl or .obj files. Don't have a file ready? We also provide a professional 3D modeling service.
0
3
.
Receive a quote
You'll get an email and a call from us immediately so we can talk about the best and most cost effective way to approach your project. No minimum order quantities!
0
4
.
Pay and print
Once the quote is approved we will start 3D printing your idea. We'll keep you updated and we'll make sure the result is exactly what you want or even more.
 No minimum orders.
No minimum orders.0
5
.
Shipping or pickup
We offer nationwide delivery or you can pick it up from one of our local studios near you.
3D printing technologies that we use
These 3D printing technologies are what powers our 3D printing process
Fused Deposition Modeling (FDM)
We use Fused Deposition Modeling (FDM) for low-cost and simple 3d printed parts. We don't use this process as much because we find the quality lacking and the amount of post processing work involved negates the money you save from low material cost. This is good for prototyping but for manufacturing end products, they might not be cost effective as there are better printing methods. If you want to produce low-cost end use parts at a large volume, injection molding might be a better solution.
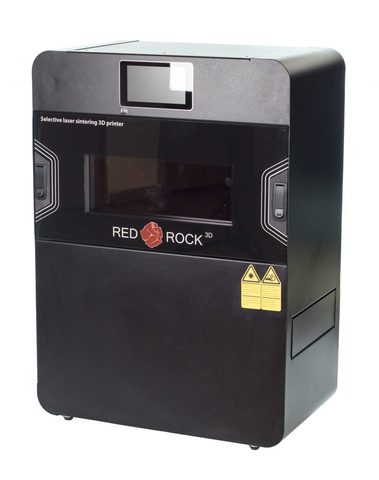
Selective Laser Sintering (SLS)
Selective laser sintering is another great additive manufacturing technology for rapid prototyping. SLS allows us to 3d print objects in different materials such as nylon and metal at large volume without the need for supports. SLS greatly reduces the time spent for post-processing.
SLS allows us to 3d print objects in different materials such as nylon and metal at large volume without the need for supports. SLS greatly reduces the time spent for post-processing.
Stereolithography (SLA)
Stereolithography allows us to 3d print accurate and high resolution prototypes . We us this process to create functional prototypes that are highly detailed. We recommend SLA for almost any 3d printing projects because we believe it produces the highest quality prints.
Multi-Jet Fusion (MJF)
Multi Jet Fusion is what helps us 3d print end-use production in 24 hours.
3D printing materials that we offer
Looking for a material that isn't listed here? Shoot us an email at [email protected]
ABS
ABS plastic is a strong and durable material. They're ideal for prototyping mechanical parts. For prototypes that require high-precision, consider CNC machining ABS or printing in other materials. For production parts, we suggest using injection molding instead.

Nylon PA12
Nylons is a strong and durable material that is also flexible. Ideal for live hinges and functional parts.
Standard Resin
Perfect for complex 3d models that require high details and smooth finishing.
SOMOS Resin
SOMOS resin is the industrial version of standard resin. It's perfect for almost any 3d that require smooth finishing and high details. We recommend this material for any projects such as high-detailed models, architecture, art sculptures and engineering prototypes.
SOMOS Waterclear 10122 Resin
Somos® WaterClear Ultra 10122 is a clear resin that produces colorless, functional and accurate parts that simulate an acrylic appearance. Parts produced from Somos® WaterClear Ultra 10122 exhibit excellent water and temperature resistance.
F.A.Q
How much does custom 3D printing cost?
Custom 3D printing can cost between $25 up to thousands of dollars depending on the size and volume of your 3D model. The 3D printing material used affects the price as well. At PrintAWorld, we use industrial SLA resin for our custom 3D printing as we believe it results in the best results for our clients. If you want to learn more, here's a breakdown of the cost of 3D printing.
The 3D printing material used affects the price as well. At PrintAWorld, we use industrial SLA resin for our custom 3D printing as we believe it results in the best results for our clients. If you want to learn more, here's a breakdown of the cost of 3D printing.
Vegas 3D Printing – Las Vegas 3D Prints
We love to create new things, fix little problems, and sometimes just make stuff for fun
-
Portable Sacrament Kit - 6 cups
Portable Sacrament Kit - 6 cups
- Regular price
- $20.00
- Sale price
- $20.00
- Regular price
-
- Unit price
- /per
Sale Sold out
-
Portable Sacrament Kit - 8 cups
Portable Sacrament Kit - 8 cups
- Regular price
- $30.
 00
00 - Sale price
- $30.00
- Regular price
-
- Unit price
- /per
Sale Sold out
-
Portable Sacrament Kit - 10 cups
Portable Sacrament Kit - 10 cups
- Regular price
- $40.00
- Sale price
- $40.00
- Regular price
-
- Unit price
- /per
Sale Sold out
We got our [Sacrament Kit] sets, frankly, very quickly, no wait. Both families used them last week. It was just nice to add that to our service. Will be ordering again for another son as soon as they complete their move.
Cathie
I bought one of these [Treble Clef Headphones Stands] as a gift for my musician wife. I gotta say: The quality of this object is amazing and almost indistinguishable from an injection molded piece. The finish on it is textured and beautiful. I’ve seen a lot of decorative shelf pieces at places like Homegoods, but they all left me worried about having it on the piano. Not this one.
Nate
We love our [Sacrament Kit]. It's absolutely perfect!
Jennifer
Our son-in-law picked our [Sacrament Kit] up on his way to visit from AZ. We love having them in our home. Thanks for making our sacrament experience even more special in our home.
Sophia
Use left/right arrows to navigate the slideshow or swipe left/right if using a mobile device
3D Printing on Order near you
705 3D Printing Services are ready to take your order now and ship the parts to LAS VEGAS, NV, United States. Through our platform, you can order 3D printing of prototypes, spare parts and any projects according to your own design without restrictions in size and quantity. If you know exactly which technology, material or application is right for your project, use the filters to narrow your search results. For clarity, study the portfolio of services with examples of printed products, as well as the rating. This will help evaluate the experience of the company with products of different types.
Download files to compare prices of local 3D printing services
Download filesor contact us for a discount on large orders.
If you are looking for a 3D printing service with delivery to LAS VEGAS, NV, United States, then you have come to the right place. All companies that provide prototyping and printing services near you are listed above.
How much does it cost to 3D print my products?
To find out the cost of services, select a company and use the "Quick order" button. Based on your 3D model in STL, PLY, OBJ or 3MF format, we will automatically determine the cost of 3D printing. If you are not sure which service to choose, use the order button at the top of the page to compare prices from all eligible print services.
How can I order a print without a 3D file?
3D printing starts with a model, so a 3D file is needed to make the part. Most printing and additive manufacturing companies can help you with a simple 3D design. For more complex modeling tasks, we recommend hiring a professional.
How to choose a 3D printing service?
Treatstock strives to provide a transparent workflow between the 3D printing company and the client for the best result.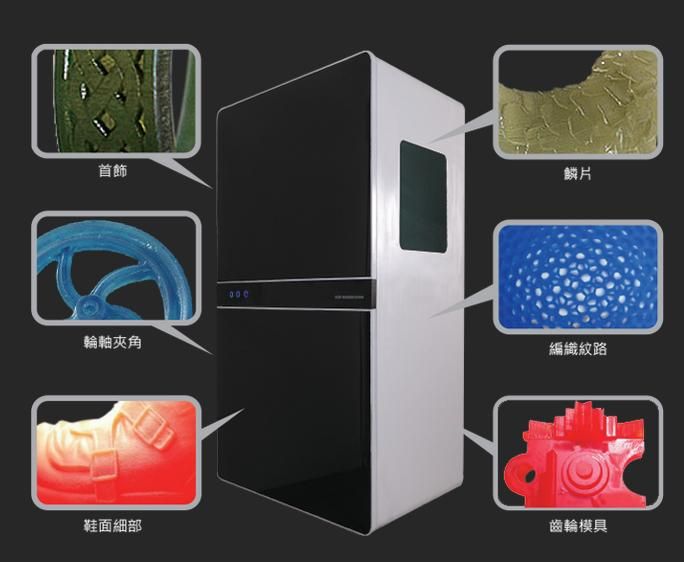 In order for you to have complete information about the future performer, we show the company's printers and customer ratings. On the public page of each service, you will also find a complete list of their services.
In order for you to have complete information about the future performer, we show the company's printers and customer ratings. On the public page of each service, you will also find a complete list of their services.
How does it work?
- Download 3D file for instant order;
- Specify order details and delivery address;
- Confirm order;
- Track the progress of your order in the Purchases section;
- Get your finished product.
Our support team is always ready to help. To learn more about the different types of 3D printing, check out our Technology Guide, as well as our Materials Guide for information on them.
 Digital methods for manufacturing these models, such as 3D printing, have become common methods as a solution to many of the problems associated with traditional manufacturing methods. Until recently, high-precision 3D printing was synonymous with large-format, expensive machines. However, with the advent of advanced desktop 3D printing technology, clinicians are using additive manufacturing as a cost-effective, scalable tool to introduce and expand digital modeling workflows. I worked closely with Formlabs to create clinically relevant benchmarks to perform an accuracy study using Dental Model 9 resin0003
Digital methods for manufacturing these models, such as 3D printing, have become common methods as a solution to many of the problems associated with traditional manufacturing methods. Until recently, high-precision 3D printing was synonymous with large-format, expensive machines. However, with the advent of advanced desktop 3D printing technology, clinicians are using additive manufacturing as a cost-effective, scalable tool to introduce and expand digital modeling workflows. I worked closely with Formlabs to create clinically relevant benchmarks to perform an accuracy study using Dental Model 9 resin0003 Resin on a Form 2 desktop stereolithography (SLA) 3D printer. The results of the study show that Formlabs Dental Model Resin polymer is capable of producing high-precision removable models with the precision and consistency required for successful clinical procedures. In addition, we fabricated Form 2 models with Dental Model Resin as part of a study to test the suitability of a mandibular ceramic crown that was successfully placed on a patient.
About the Author
Michael Scherer, MD, M.S. is an Assistant Clinical Professor at Loma Linda University, a Clinical Instructor at the University of Nevada-Las Vegas, and has a practice limited to Prosthodontics and Implant Dentistry in Sonora, California. He is a Fellow of the American College of Podiatrists and has published articles, educational DVDs, and comprehensive online courses related to implantology, clinical prosthodontics, and digital technology, with a particular focus on implant-retained prostheses. Actively addicted to technology and
computers, Dr. Scherer took part in the development of digital dental implantology, which led him to develop and use new technologies with surgical CAD / CAM systems, the introduction of interactive CBCT implant planning and non-standard radiographic imaging concepts. Dr. Scherer also hosts five YouTube channels: “LearnLOCATOR,” “LearnLODI,”
“LearnSATURNO,” “LearnLOCATOR F–Tx,” and “The 3D Dentist,” popular YouTube channels on dental implant procedures and digital dentistry.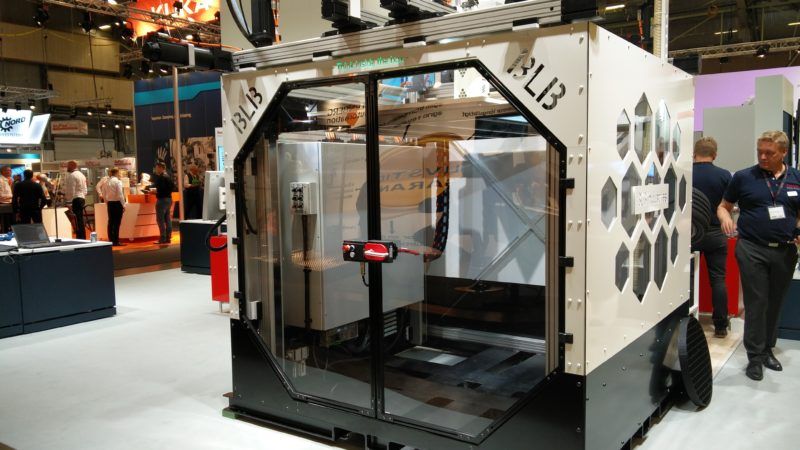 He also maintains a blog dedicated to 3D printing and individual and online courses for 3D printing (www.michaelschererdmd.com).
He also maintains a blog dedicated to 3D printing and individual and online courses for 3D printing (www.michaelschererdmd.com).
Introduction
With intraoral scanning techniques dramatically improving the practice of clinical dentistry and the accuracy of impression procedures, ¹-⁴ the advent of affordable high-precision 3D printing technology represents a game changer for the dental industry. The ability to reliably and consistently produce high-precision restorations in a private dental office or small dental laboratory can solve many of the problems associated with traditional methods, ⁴-⁵ and provide significant savings in manufacturing time and costs.
To achieve these changes, it is important that clinicians can trust that the models printed on the 3D printing system are accurate and precise. The ability to manually test the feel and fit of physical models, just like those created by traditional model making methods, is an important step in the process of working in the dental field. This is integral to the success of the final procedure.
This is integral to the success of the final procedure.
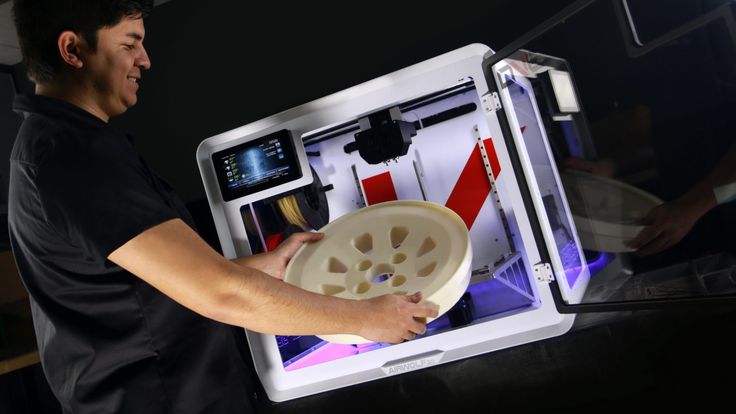
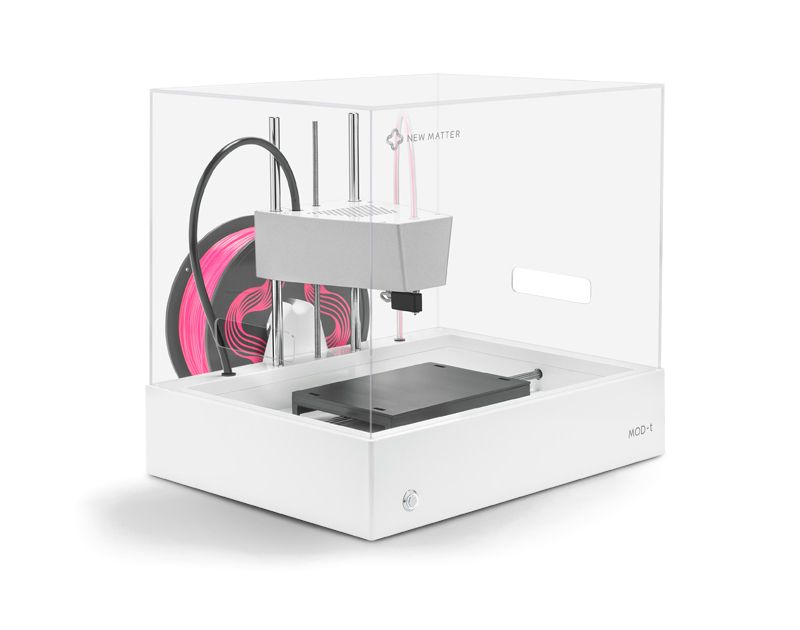
Until recently, most of the professional 3D printing market consisted of expensive large format 3D printers with high machine costs limiting access to large dental labs. In contrast, modern desktop 3D printers such as the Formlabs Form 2 have generated significant interest for creating models for dental labs and even clinical practices of all sizes.
Adopting cost-effective, scalable 3D printing internally allows a smooth transition to fully digital, streamlined workflows that quickly return on investment. However, in order to effectively evaluate which print technology to invest in, it is critical to check the accuracy.
So using Formlabs Dental Model Resin and a large selection of Form 2 3D printers, we set out to demonstrate that a desktop 3D printing system can accurately and repeatedly produce crown and bridge models with removable dies to acceptable clinical standards. An accuracy study was conducted using Formlabs Form 2 3D printers and Formalabs Dental Model Resin.
In this document, we first define accuracy and precision in order to determine what specific print characteristic we are trying to characterize. We then establish the appropriate benchmarks that a dental model must achieve in order to be clinically acceptable by extensively reviewing the literature and previous studies. We then describe the accuracy study that was performed for print characterization and review the results to conclude whether the Formlabs Form 2 can produce highly accurate dental models suitable for clinical practice. Finally, we will describe an example in which models were printed on a Form 2 using Dental Model Resin and used to verify the fit of a mandibular ceramic crown, which was then successfully placed on the patient.
Accuracy and Precision in 3D Printing
To achieve meaningful 3D printing performance for any application, both accuracy and precision must be considered. Accuracy is the closeness of a measurement to the true value. Precision measures the repeatability of a measurement—in other words, consistency and repeatability. It is essential to ensure both an acceptable level of accuracy and a high level of precision.
It is essential to ensure both an acceptable level of accuracy and a high level of precision.
What level of precision or accuracy is needed for dental 3D applications? To answer this question, we reviewed common practice, published literature, and previous research. We then set a meaningful specification for what kind of performance you can expect from a dental 3D printer.
Determining clinical accuracy needs for dental models
For a dental model to be effective for verifying restorations such as crowns or bridges, it is essential that it can be used to verify the marginal fit of the restorative design. A good marginal fit is key to the long-term clinical success of a restoration.
Large marginal gaps can adversely affect the acceptance rate of the restoration, which can lead to rejection and premature loss of the restoration.
It is therefore essential that the dental model accurately and accurately reproduces the anatomical neck of the tooth, also known as the gingival margin of the preparation, of the restoration. In addition, for a dental model used for large multilevel restorations, it is also important to achieve an acceptable level of accuracy throughout the model. Therefore, we have identified two markers for assessing the accuracy of dental models:
In addition, for a dental model used for large multilevel restorations, it is also important to achieve an acceptable level of accuracy throughout the model. Therefore, we have identified two markers for assessing the accuracy of dental models:
MARGINAL ACCURACY
Accuracy with which the gingival margin of the preparation and die surfaces above the margin are reproduced.
OVERALL ACCURACY
Overall accuracy of the model, measured through a full arc.
To assess the clinical needs for each of these specifications, we reviewed the methods used in general clinical practice, as well as published literature and previous studies.
Clinical Accuracy
The clinical accuracy of a restorative design, such as a ceramic crown, inlay, or implant prosthesis, is usually determined by subjective analysis by the clinician or laboratory technician. This analysis is mainly determined by visual methods such as the use of radiographic/X-ray imaging or staining media; variable finger pressure; single propeller design testing; helical resistance test; and special digital instruments, or tactile methods, such as the use of a physical instrument, performed directly on the restoration that connects the tooth or implant.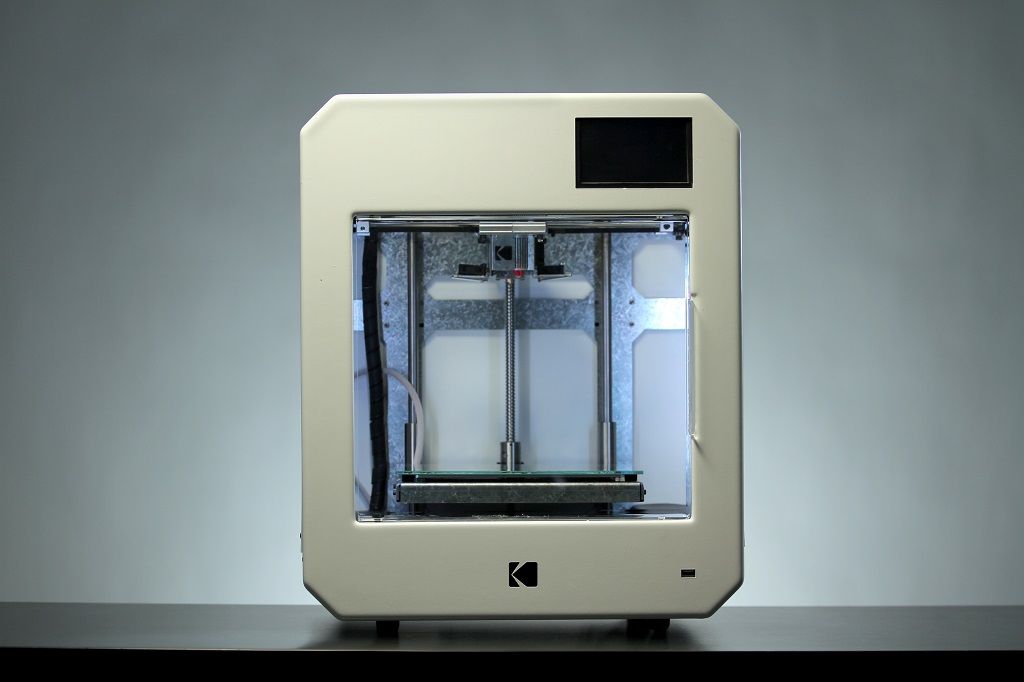
The great variability in this approach is evident in dentistry. While many clinicians generally argue that restorations should meet marginal fit differences of 10-30 µm, Christensen's studies evaluating this issue have shown that in practice, clinicians have accepted a range of 34 to 119 µm of marginal crown misplacement. .⁶ Moreover, nearly half of the clinicians were found to be inconsistent with their assessment methods; sometimes the same doctor denies the suitability of a restoration that he accepted earlier.
Although various methods have been promoted over the years, two gold standards for proper restoration are appropriate for clinical dentistry: tactile sensation with the examiner's instrument and visual assessment with radiographic imaging.
The image on the left shows two examples of very similar three-piece implants with fixed partial dentures. Both show clinically acceptable restorations, but no marginal fit (left) and slight clinically acceptable marginal fit (right).
TOUCH EVALUATION METHODS
Many clinicians use instruments such as a dental probe to make decisions about the clinical suitability of a restorative design. Clinicians use a research tool to explore the "feel" over the restorative design; if the instrument catches a groove near the margin, clinicians will reject the restoration, stating that it does not fit properly.
Using scanning electron microscopy, Rappold showed that a new, unused probe tip is 68 µm thick, which ultimately indicates that many clinicians can accept restorative design mismatches up to this magnitude.⁷ In addition, many clinicians routinely do not sharpen or do not purchase new equipment for each patient, thus potentially accepting higher levels of design mismatch
The probe is used to assess the clinical fit of a restoration using the tactile sensation of the instrument passing along the contours of the teeth. When the tip of the instrument slides over grooves or depressions in the surface of the tooth/restoration, it enables the clinician to evaluate the clinical fit of the restoration.
OPTICAL EVALUATION METHODS
Radiographic assessment of the fit of a restorative design is an important method used by both clinicians and third party payers such as dental insurance plans. The radiographic assessment uses a conventional radiographic image of the lateral or proximal portion of the dental crown to confirm that the margins of the tooth preparation are consistent with the margins of the restoration. Although this method of assessing clinical fit is subjective, it offers a high degree of predictability between clinicians. However, it is highly dependent on the angular deviation of the radiograph; increasing the angle reduces reliability. A radiographic angular deviation of ±10 degrees in the vertical plane can cause clinicians to potentially lose open margins or result in a 100 µm mismatch in the restorative design.⁸ As radiographic angular deviation approaches 20 degrees, this mismatch can increase to 700 µm.
Many clinicians rely on a dental mirror to assess the clinical fit of a restoration by visually checking whether there is an acceptable marginal fit
Considering many of these factors, studies have found that, in practice, failure of a restoration that considered acceptable is between 50 and 200 µm. ⁸ Based on many of the factors mentioned in this section, there is general agreement that the average clinician considers 100 µm to be the maximum acceptable mismatch for a crown, implant, or restorative that “fits”.
⁸ Based on many of the factors mentioned in this section, there is general agreement that the average clinician considers 100 µm to be the maximum acceptable mismatch for a crown, implant, or restorative that “fits”.
Converting Clinical Standards to Print Specifications
Based on these clinical acceptance criteria, we reverted to our three metrics of accuracy. With a marginal gap of up to 100 µm generally clinically acceptable, an accuracy range of less than half this value would be an acceptable range, i.e. ±50 µm. For contact points, the equivalent range of ±50 µm will also matter. From a full arc, i.e. a distance of 40 to 60 mm, a value of ± 100 µm was chosen. Expressed as a proportion, this would be between ±0.25 percent and ±0.17 percent.
| Clinically relevant target | |
| Marginal accuracy | ±50 µm |
| General accuracy | ±100 µm |
3D printing accuracy rating.
METHODOLOGY
We set out to evaluate the accuracy and precision of 3D printed crown and bridge models with removable dies on the Form 2 using Dental Model Resin, the highest precision resin in the Formlabs resin line. Since the accuracy depends on the material, this choice was deliberately made for the best results.
A total of 148 parts—many die and arc models—were printed directly on the build platform. After printing, each part was removed from the build platform, cleaned with isopropyl alcohol (IPA), post-cured for 60 minutes at 60°C in a UV curing chamber, and optically scanned using a 3Shape D900L desktop scanner. Each model scan was compared to the original .STL file using Convince Analyzer (3Shape).
Accuracy errors corresponding to the 80th surface percentile were measured. Surface percentiles represent the proportion of points on the surface of interest that are at a given distance from the nominal, i.e. desired position. Thus, the accuracy error of ± 38 µm for the 80th surface percentile is 80% of the surface that is within ± 38 µm of the nominal surface.
This process was performed on a representative sample of six different Form 2 printers. Using a wide range of Form 2 printers allows us to comment on the group as a whole - in terms of machine precision - and not just in terms of performance on a single machine
SIDE VIEW
ISOMETRIC VIEW
0212 die surfaces.
View
Isometric type
Results
| Reference object | Clinically relevant target | 80th percentile results | |||
| 100 micron print setting results (±µm) | 50 micron print setting results (±µm) | 25 micron print setting results (±µm) | |||
| Marginal accuracy | Removable die | ±50 µm | ±64.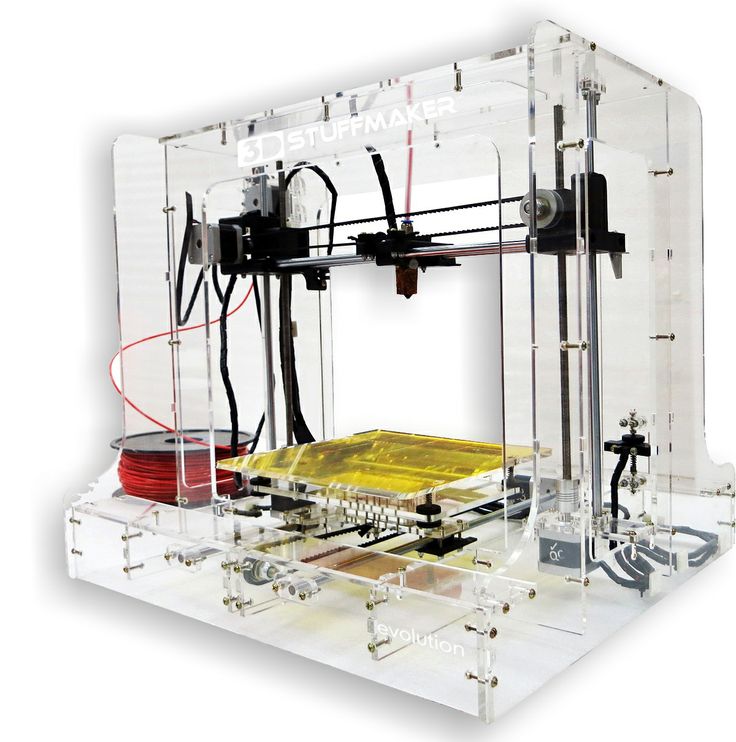 2 µm 2 µm | ±44.7 µm | ±30.5 µm |
| Total accuracy | full arc Model | ±100 µm | ±149.6 µm | ±104 µm | ±67.9 µm |
The results of the study provide strong evidence that printing at 50 micron or 25 micron settings will produce clinically acceptable models.
At a layer thickness of 100 µm, marginal and overall accuracy were outside of our originally defined limits. However, given the variability in clinical acceptance and testing methods, it is interesting to note that they are likely to be in the range that would be clinically acceptable for many users.
At print settings of 50 µm, marginal accuracy is in line with our defined target for marginal accuracy, and overall accuracy as measured on the sample dataset is out of the ±104 µm range. Taking into account the standard deviation of these measurements, it is practically in the range and probably has zero clinical significance. Therefore, it is clear that printing with a layer thickness of 50 microns will achieve acceptably accurate models for the purposes of bridge and crown models.
Therefore, it is clear that printing with a layer thickness of 50 microns will achieve acceptably accurate models for the purposes of bridge and crown models.
At 25 micron settings, the highest level of accuracy is achieved, both in terms of marginal and overall accuracy. While these high rates may be attractive to some clinicians, it is important to note that they far exceed the originally defined targets, and the performance difference between printing at 25 microns and 50 microns is likely to be of zero clinical significance.
This pattern of increased accuracy when printing at thinner layer thicknesses is due to how 3D models are sampled into layers for the 3D printer to print. When a part has any corner edges that are not directly on the Z or XY plane, the thickness of the layers determines the number of discrete points that the edges of the part fall into. Smaller, thicker layers lead to a step effect - the formation of a greater distance between discrete points.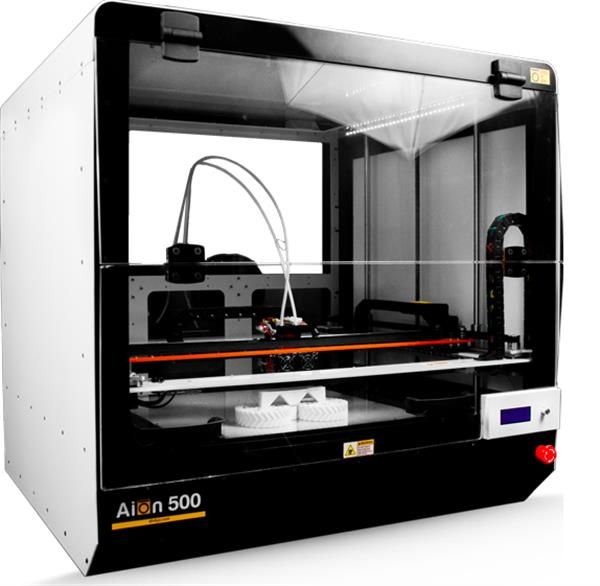 Many thin layers lead to
Many thin layers lead to
smoother, more detailed surfaces that will touch more discrete points and therefore closer to the scan, making the detail more accurate. Application example: single ceramic crown
A 52-year-old patient reported that he "had chipped one of his back molars". Clinical examination revealed a fractured distal-lingual cusp on the lower right first molar (tooth #30) (A). An x-ray was taken confirming the absence of caries, and the patient asked for a ceramic crown.
Local anesthesia was used. The crown was divided and removed using a diamond bur and gentle manipulation. The preparation was cleaned, the thread was placed and an optical impression was made (B). The optical impression system allows the clinician to reliably create a digital model of the patient's preparation, dentition, and surrounding soft tissue. In addition, scans of opposing teeth and occlusion were completed (C). The digital files were sent to the dental laboratory for further procedures. A temporary material was fabricated, cemented, and the patient was scheduled for a crown procedure.
A temporary material was fabricated, cemented, and the patient was scheduled for a crown procedure.
Files have been received and models have been imported and developed using dental CAD software. Three files were created: 1) an opposing denture model, 2) a provisional model with a notch corresponding to a delayed die, and 3) a model of a delayed preparation die (D-F). Each file was individually printed on a Form 2 3D printer using 50 micron thick Dental Model Resin. Each of the models was processed using the Formlabs Ready Kit, with 9 step washes.1% solution of isopropyl alcohol
(IPA) followed by UV curing in an industrial curing machine.
The models were printed with articulated objects (D), which allowed the laboratory technician to physically close the models and check the occlusion of the restoration. A pressed lithium disilicate crown was fabricated and mounted on the model, confirming contacts with adjacent teeth (E) and marginal integrity (F).
Patient returned for final clinical procedures.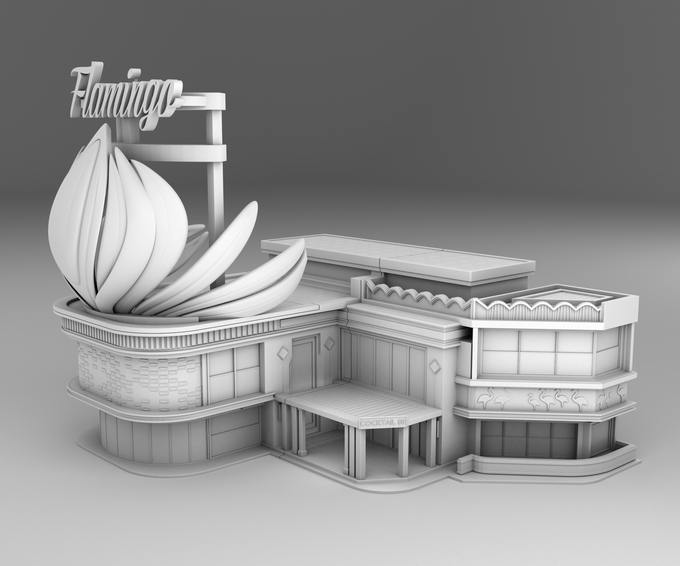 No anesthesia was required, the temporary structure was removed and the structure was cleaned prior to bonding. The restorative design was validated by checking contacts, marginal fit, and esthetics. Using established workflows in the dental industry in combination with Formlabs Dental Model Resin, minimal adjustments were required as the restoration conformed to incredible precision. The crown was cemented using resin cement (G-H) and radiographs were taken to ensure that all cement had been removed correctly (I). The occlusion was checked and the restoration was polished. The patient was very pleased with his new comfortable restorative design.
No anesthesia was required, the temporary structure was removed and the structure was cleaned prior to bonding. The restorative design was validated by checking contacts, marginal fit, and esthetics. Using established workflows in the dental industry in combination with Formlabs Dental Model Resin, minimal adjustments were required as the restoration conformed to incredible precision. The crown was cemented using resin cement (G-H) and radiographs were taken to ensure that all cement had been removed correctly (I). The occlusion was checked and the restoration was polished. The patient was very pleased with his new comfortable restorative design.
Comparison with other 3D printing systems
These results only cover the Formlabs Form 2 3D printer, demonstrating how a desktop 3D printing system can achieve the highest level of clinically meaningful performance in printing dental models. However, these results do not speak more broadly about the print performance of other desktop 3D printers, or about dental 3D printers in general.
Therefore, we wanted to compare the results with other 3D printers. This is a complex issue, complicated by the lack of a common standard for comparing printers.
One common misrepresentation of precision is the description of XY resolution as precision. For digital light processing (DLP), XY resolution is the size of the projected pixel. Many 3D printer systems use this predicted pixel size, or XY resolution, as a general measure of accuracy—for example, with a projected pixel size of 75 microns and a claim that the machine's accuracy is ±75 microns.
This data has no bearing on how accurate the printed part is.
There are many sources of error that still affect accuracy, from components, to calibration, to partial shrinkage after printing, and more. printing and measuring actual printed parts. To measure precision and be statistically significant, a large part sample size and a representative machine sample must be used.
With limited resources, this study was unable to complete such a large-scale comparison. However, to get an initial idea of how the results of this Form 2 study might compare to other 3D printing systems, we tried to compare actual print performance with two installed large format 3D printers that cost $35,000 and $75,000 . On each system, we printed an identical part on both the Form 2 and the system we were comparing.
However, to get an initial idea of how the results of this Form 2 study might compare to other 3D printing systems, we tried to compare actual print performance with two installed large format 3D printers that cost $35,000 and $75,000 . On each system, we printed an identical part on both the Form 2 and the system we were comparing.
The results of both tests showed that print results on the Form 2 were virtually indistinguishable from either system in terms of accuracy. Given limited resources and time, only two control models were compared, so statistical significance is limited. However, it provides evidence that, in terms of accuracy, the Form 2 performs just as well as these installed large format systems.
LARGE FORMAT DENTAL 3D printer
Form 2
Figure 5. Comparison 3D
We scanned and printed first. 1, second in rows 2 and 3) on an installed large format dental 3D printer currently used in a dental lab (shown in left column) and on a Formlabs Form 2 (shown in right column). As shown in the difference heat map, the accuracy achieved by each print is nearly identical. Large format printer costs about $75,000 and Form 2 is $3499 dollars.
As shown in the difference heat map, the accuracy achieved by each print is nearly identical. Large format printer costs about $75,000 and Form 2 is $3499 dollars.
Conclusion
The growing adoption of low-cost desktop 3D printing systems presents an opportunity for major change in the dental industry. The ability to use these printers to reliably print dental models for the verification of high-precision restorations offers a significant opportunity to reduce production time and costs.
The results of this study show that it is possible to fabricate high precision
precision removable die dental models on the Formlabs Form 2 using Dental Model Resin. Printing at 50 µm and 25 µm on a representative sample of the Form 2s is within clinically relevant accuracy, both in terms of gingival margin and die surface accuracy, as well as overall accuracy.
A small comparison with two large format 3D printers also showed that the Form 2's print performance is indistinguishable from systems already adopted and used by dental labs.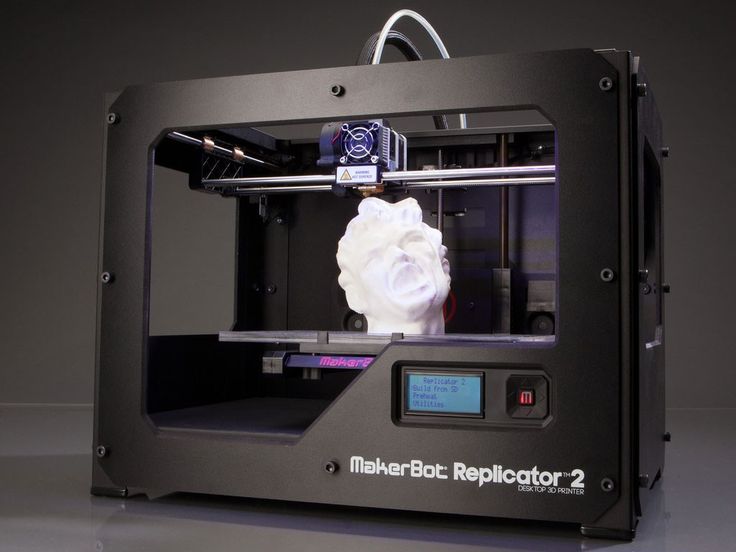 An in-depth comparison, including high print volumes and a representative sample of both desktop and industrial 3D printing systems, is required to draw deeper conclusions from a head-to-head comparison of 3D printing systems.
An in-depth comparison, including high print volumes and a representative sample of both desktop and industrial 3D printing systems, is required to draw deeper conclusions from a head-to-head comparison of 3D printing systems.
The ability to create highly accurate dental models in-house to the required clinical standards represents a huge opportunity for all dental professionals, solving many of the problems associated with traditional manufacturing methods and breaking down barriers to digital acceptance.
. Clin. Oral impl. Res. 00, 2015, 1–8.
- Syrek A., Reich G., Ranftl D., Klein C., Cerny B., Brodesser J. Clinical evaluation of all-ceramic crowns made from intraoral digital impressions based on the principle of active selective wavefront sampling.
 J Dent. 2010;38:553-9.
J Dent. 2010;38:553-9.
- Ng Y., Rousse D., Wyatt Z. Comparison of marginal fit between digital and conventional crowns. J Prosthet 2014;112:555-60.
- Ting-Shu S, Yian S. Intraoral digital impression technology: Review J 2015;24:313-21.
- Christensen G.J. Marginal fit of gold inlay castings. J Prosthet 1966 Mar-April;16(2):297-305.
- Rappold A.P., Ripps A.H., Ireland E.J. Probe sharpness relative to gingival margin evaluation. Oper Dent. January-February 1992;17(1):2-6.
- Sharkey S, Kelly A, Houston F, O'Sullivan M, Quinn F, O'Connell B. Radiographic analysis of implant component mismatch. Int J Oral Maxillofac Implants. Jul-Aug 2011;26(4):807-15.
- Ahlholm P., Sipila K., Vallittu P., Jakonen M., Kotiranta U. Digital and traditional impressions in prosthetic dentistry: A review J 2.08.2016
- Donovan T.E., Chee V.V. Review of modern impression materials and techniques. Dent Clean North Am. 2004;48:445-70.

Learn more