3D printed tracheal splint
3D-Airway Printed Splint | Otolaryngology | Michigan Medicine
Tracheomalacia in babies occurs when cartilage in the trachea, or windpipe, develops abnormally. As a result, the tracheal walls can collapse, making it difficult to breathe.
Tracheomalacia cases vary in severity. For most children, symptoms are mild and subsist by age three, once the tracheal cartilage has had time to grow stronger. But for approximately 5,000 babies in the United States, symptoms are life-threatening and require a tracheotomy and ventilator. Although these babies are often able to have the tracheotomy ventilator removed by age three, the medical costs and impact on quality of life are significant.
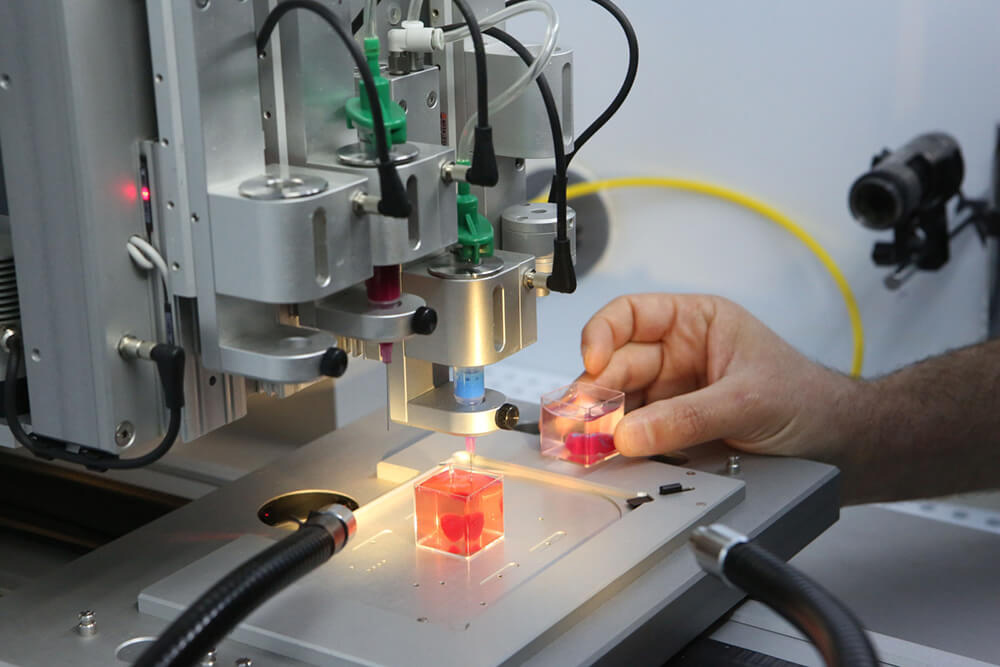
Researchers in our department are investigating a treatment for severe cases of tracheomalacia. Dr. Glenn Green, pediatric otolaryngologist, and Dr. Scott Hollister, professor of biomedical engineering, have developed a biodegradable scaffolding, which can be designed and manufactured into a tracheal splint using patient imaging, computer aided design based on the patients image, and a laser-based 3D printing system. This splint is attached to the outer side of the trachea, holding the airway open and preventing collapse associated with tracheomalacia.
The tracheal splint is still in the research phase and therefore not available for clinical use. But in February 2012, a life or death situation put the splint to the test. Three-month-old Kaiba of Dayton, Ohio was rushed to a local hospital after suffering a respiratory arrest at home. Diagnosed with a severe case of tracheomalacia, Kaiba received a tracheotomy and ventilator and required heavy sedation in the hospital. Despite these efforts, he continued to require resuscitation. Knowing there was nothing else they could do for him, Kaiba’s healthcare providers referred him to the capable and experienced hands of Dr. Green.
Kaiba Gionfriddo
Dr. Green was faced with an important decision: attain emergency approval to use the biodegradable scaffolding or inform Kaiba’s parents that their baby boy would die. The answer was simple, and soon Dr.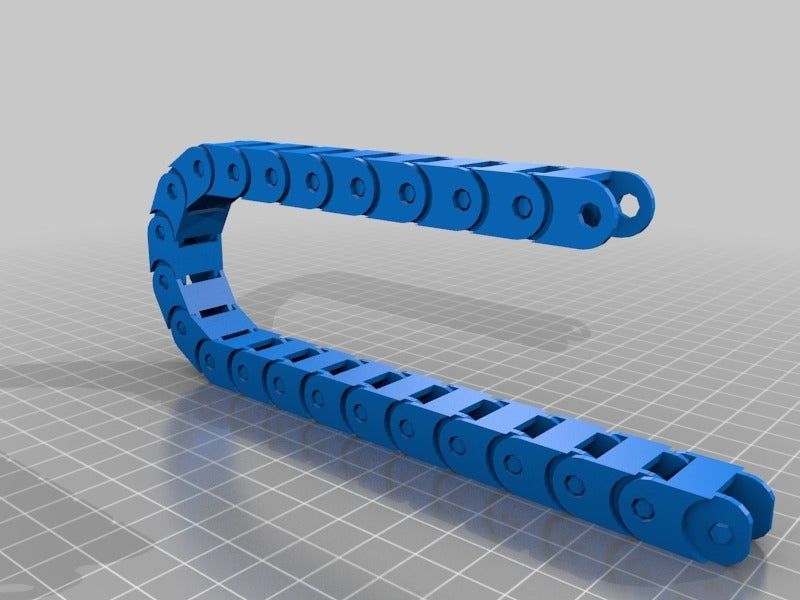 Green was working with the Federal Drug Administration, Institutional Review Board and hospital administration to secure permission. One week later, Dr. Green received approval to use the biodegradable tracheal splint, making Kaiba the first baby on earth to receive this treatment. Today, Kaiba is thriving. He is well on his way to living a normal childhood, one that would not have existed without the important work of Drs. Green and Hollister and this innovative technology.
Green was working with the Federal Drug Administration, Institutional Review Board and hospital administration to secure permission. One week later, Dr. Green received approval to use the biodegradable tracheal splint, making Kaiba the first baby on earth to receive this treatment. Today, Kaiba is thriving. He is well on his way to living a normal childhood, one that would not have existed without the important work of Drs. Green and Hollister and this innovative technology.
Hollister and Green again used provisions for emergency clearance from the FDA to create and implant a tracheal splint for Garrett. Hollister created a 3D model of Garrett’s airway and specially designed splints for a custom fit on the baby’s bronchi. He was then was able to make the custom-designed, custom-fabricated splint using high-resolution imaging and computer-aided design. The device was created directly from a CT scan of Garrett's trachea and bronchi, integrating an image-based computer model with laser-based 3D printing to produce the splint.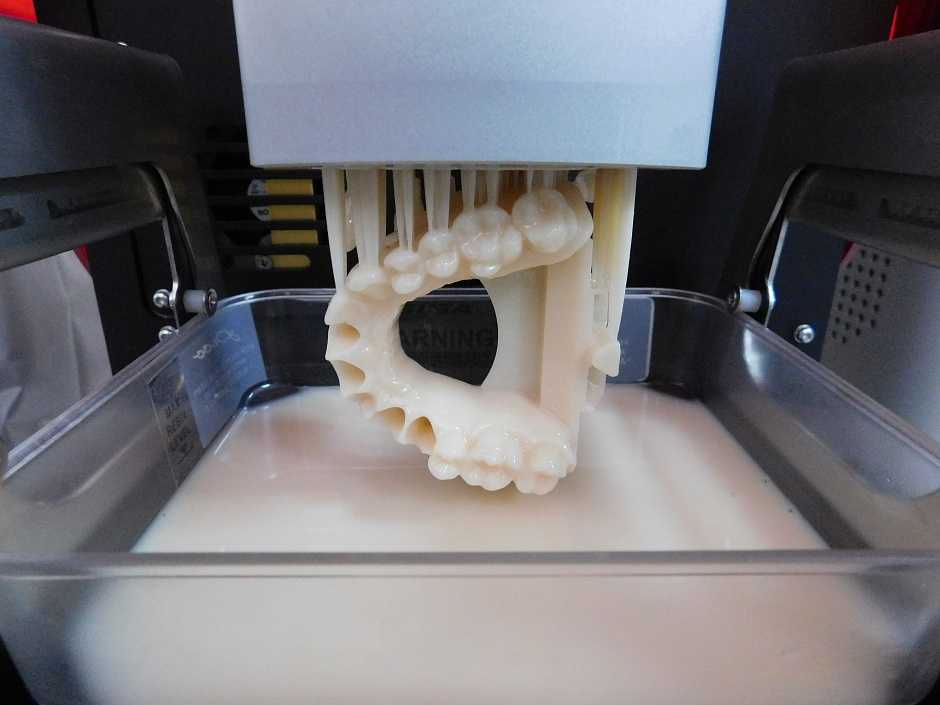
Garrett Peterson
Then in January 2014, Drs. Green and Hollister again had the opportunity to use their new device. Garrett has a condition called tetralogy of Fallot with absent pulmonary valve, which can put tremendous pressure on the airways. In Garrett’s case, he developed severe tracheobronchomalacia. Richard G. Ohye, M.D., the head of pediatric cardiovascular surgery at C.S. Mott, took on the intricate task of sewing two devices on two spots of Garrett’s airway, assisted by Green. The splints were sewn around Garrett’s right and left bronchi to expand the airways and give it external support to aid proper growth. Hollister says it is hoped that Garrett will need about two to three years for his trachea to remodel and grow into a healthy state. That’s about how long this material will take to dissolve into the body.
“Severe tracheobronchomalacia has been a condition that has frustrated me for years,” says Green. “I’ve seen children die from it. To see this device work, for a second time, it’s a major accomplishment and offers hope for these children. ”
”
It is thrilling to have a treatment to offer children like Kaiba and Garrett, but the splint cannot be made available on a wider scale until research is complete. That research comes at a great cost. If you would like to donate to this cause, please click on the button below.
Groundbreaking 3D-Printed Splint Restores a Baby’s Breathing
Ann Arbor, Mich. – Every day, their baby stopped breathing, his collapsed bronchus blocking the crucial flow of air to his lungs. April and Bryan Gionfriddo watched helplessly, just praying that somehow the dire predictions weren’t true.
“Quite a few doctors said he had a good chance of not leaving the hospital alive,” says April Gionfriddo, about her now 20-month-old son, Kaiba. “At that point, we were desperate. Anything that would work, we would take it and run with it.”
They found hope at the University of Michigan, where a new, bioresorbable device that could help Kaiba was under development. Kaiba’s doctors contacted Glenn Green, M.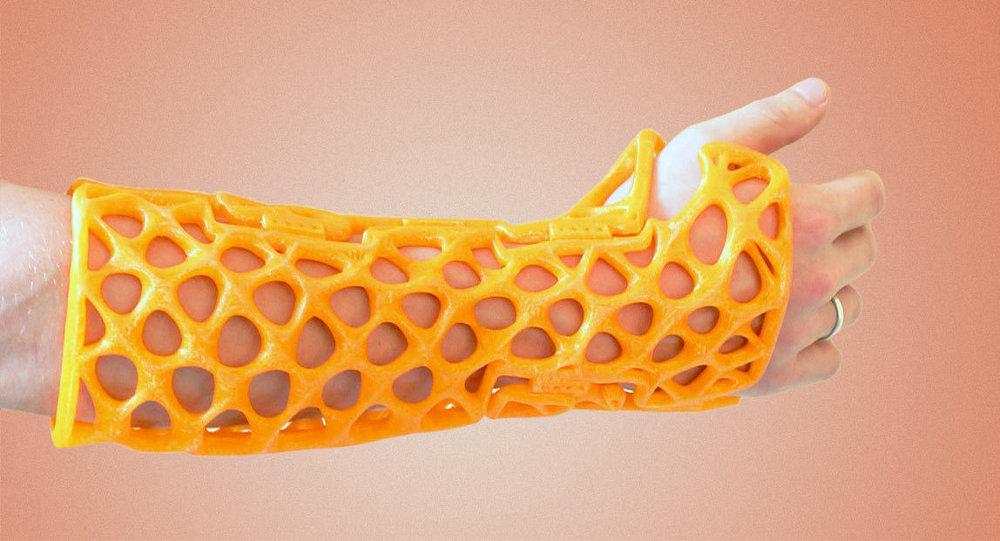 D., associate professor of pediatric otolaryngology at the University of Michigan.
D., associate professor of pediatric otolaryngology at the University of Michigan.
Green and his colleague, Scott Hollister, Ph.D., professor of biomedical engineering and mechanical engineering and associate professor of surgery at U-M, went right into action, obtaining emergency clearance from the Food and Drug Administration to create and implant a tracheal splint for Kaiba made from a biopolymer called polycaprolactone.
On February 9, 2012, the specially-designed splint was placed in Kaiba at C.S. Mott Children’s Hospital. The splint was sewn around Kaiba’s airway to expand the bronchus and give it a skeleton to aid proper growth. Over about three years, the splint will be reabsorbed by the body. The case is featured today in the New England Journal of Medicine.
“It was amazing. As soon as the splint was put in, the lungs started going up and down for the first time and we knew he was going to be OK.”— Glenn Green, M.
 D. Associate Professor of Pediatric Otolaryngology
D. Associate Professor of Pediatric OtolaryngologyGreen and Hollister were able to make the custom-designed, custom-fabricated device using high-resolution imaging and computer-aided design. The device was created directly from a CT scan of Kaiba's trachea/bronchus, integrating an image-based computer model with laser-based 3D printing to produce the splint. Materialise’s Mimics Innovation Suite software played a role in the design and sizing of the device.
“Our vision at the University of Michigan Health System is to create the future of health care through discovery. This collaboration between faculty in our Medical School and College of Engineering is an incredible demonstration of how we achieve that vision, translating research into treatments for our patients,” says Ora Hirsch Pescovitz, M.D., U-M executive vice president for medical affairs and CEO of the U-M Health System.
“Groundbreaking discoveries that save lives of individuals across the nation and world are happening right here in Ann Arbor. I continue to be inspired and proud of the extraordinary people and the amazing work happening across the Health System.”
I continue to be inspired and proud of the extraordinary people and the amazing work happening across the Health System.”
Kaiba was off ventilator support 21 days after the procedure, and has not had breathing trouble since then.
“The material we used is a nice choice for this. It takes about two to three years for the trachea to remodel and grow into a healthy state, and that’s about how long this material will take to dissolve into the body,” says Hollister.
“Kaiba’s case is definitely the highlight of my career so far. To actually build something that a surgeon can use to save a person’s life? It’s a tremendous feeling.”— Scott Hollister, Ph.D. Professor of Biomedical Engineering and Mechanical Engineering
The image-based design and 3D biomaterial printing process can be adapted to build and reconstruct a number of tissue structures. Green and Hollister have already utilized the process to build and test patient specific ear and nose structures in pre-clinical models. In addition, the method has been used by Hollister with collaborators to rebuild bone structures (spine, craniofacial and long bone) in pre-clinical models.
In addition, the method has been used by Hollister with collaborators to rebuild bone structures (spine, craniofacial and long bone) in pre-clinical models.
Severe tracheobronchomalacia is rare. About 1 in 2,200 babies are born with tracheomalacia and most children grow out of it by age 2 or 3, although it often is misdiagnosed as asthma that doesn’t respond to treatment.
Severe cases, like Kaiba’s, are about 10 percent of that number. And they are frightening, says Green. A normal cold can cause a baby to stop breathing. In Kaiba’s case, the family was out at a restaurant when he was six weeks old and he turned blue.
“Severe tracheobronchomalacia has been a condition that has bothered me for years,” says Green. “I’ve seen children die from it. To see this device work, it’s a major accomplishment and offers hope for these children.”
Before the device was placed, Kaiba continued to stop breathing on a regular basis and required resuscitation daily.
“Even with the best treatments available, he continued to have these episodes./cdn0.vox-cdn.com/uploads/chorus_asset/file/3654746/morrison2HR.0.jpg) He was imminently going to die. The physician treating him in Ohio knew there was no other option, other than our device in development here,” Green says.
He was imminently going to die. The physician treating him in Ohio knew there was no other option, other than our device in development here,” Green says.
Kaiba is doing well and he and his family, including an older brother and sister, live in Ohio.
“He has not had another episode of turning blue,” says April. “We are so thankful that something could be done for him. It means the world to us.”
The University of Michigan is becoming a leader in pediatric device manufacturing, as is the case with the manufacturing process device used to save this baby's life. The FDA-funded University of Michigan Pediatric Device Consortium (M-PED) offers product development guidance and strategic support for advancing devices to market. In a new medical product manufacturing video released by M-PED, Green, Hollister and other U-M and industry experts share their experiences and advice.
Journal reference: DOI: 10.1056/1 NEJMc1206319
Additional authors: Of the University of Michigan: David A. Zopf, M.D., Richard G. Ohye, M.D. Of Akron Children’s Hospital: Marc E. Nelson, M.D.
Zopf, M.D., Richard G. Ohye, M.D. Of Akron Children’s Hospital: Marc E. Nelson, M.D.
About C.S. Mott Children’s Hospital: Since 1903, the University of Michigan C.S. Mott Children’s Hospital has led the way in providing comprehensive, specialized health care for children. From leading-edge heart surgery that's performed in the womb to complete emergency care that's there when you need it, families from all over come to the University of Michigan C.S. Mott Children's Hospital for our pediatric expertise. In 2013, C.S. Mott Children’s Hospital was ranked eighth in the nation in Parents Magazine’s 10 Best Children’s Hospitals ranking. To learn more, visit the Mott Children' Hospital website.
3D printer in tire making.
Creativity
Subscribe to the author
Subscribe
Don't want
116
Many of my friends are still trying to convince me of the uselessness of a 3D printer, they say, 'well, you can print cubes, snakes, and all sorts of bushings and get bored'.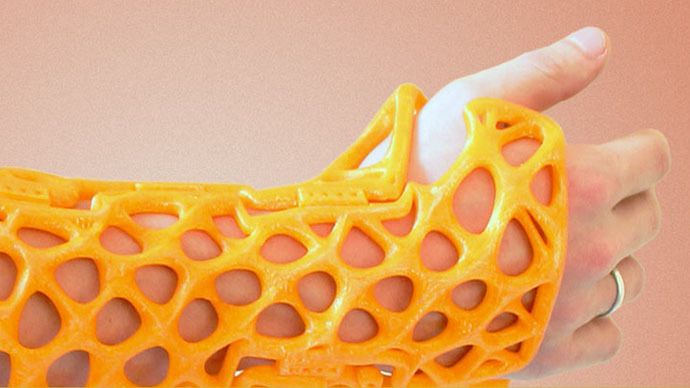 But nifiga, not tired =). I found another use for a 3D printer in another detail.
But nifiga, not tired =). I found another use for a 3D printer in another detail.
A long time ago I made tires from silicone, by pouring into an epoxy matrix. About how the matrix was made is a completely different story.
Well, that's it. There is a 3D printer ... but, so that, I think not to print a matrix on it? Ay, yes.
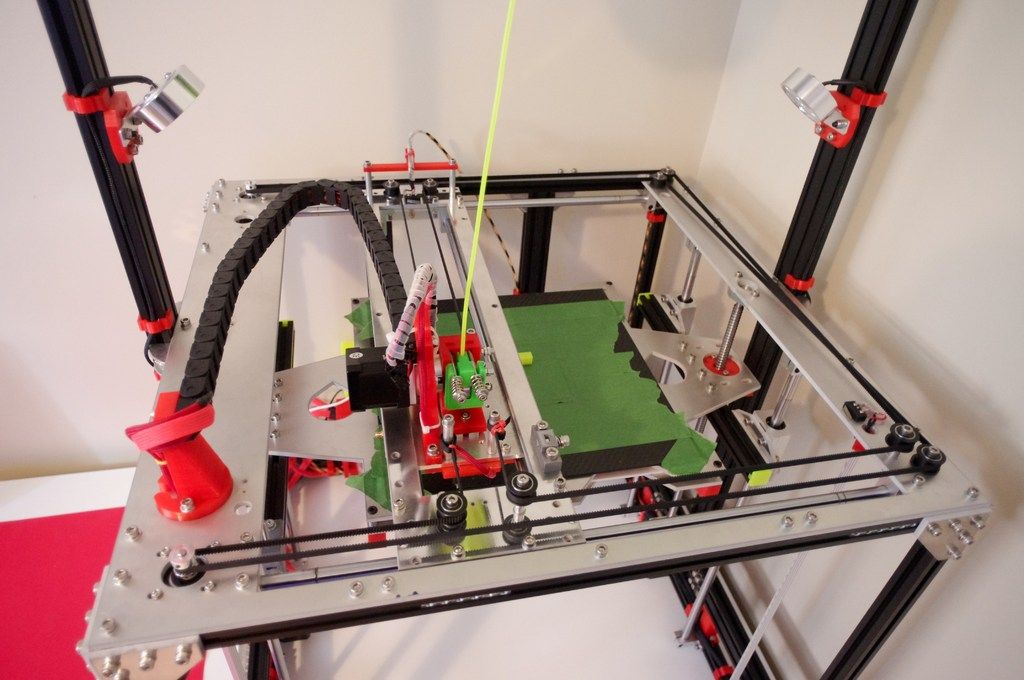
We model the tire, cut the tread and in the halves of the matrix with the 'indent' element we make the drawings on it.
We make an insert between the halves to select an extra volume and make the tire profile.
Due to the specific shape of the insert, I made the supports myself. Width 0.3. I have long understood that in such models it is better to do supports yourself than to watch how the corners of the model lie between the grids / support lines (and this is on filling the support with 40% !sic)
A little background, to the current version:
Initially I tried to print a treadless donut with a selection inside. Everything worked out, the result pleased.
Everything worked out, the result pleased.
In the last one, I already decided to pour a solid tire with a transparent sealant. The thin profile turned out to be too thin and wrinkled a lot. But after pulling it out of the matrix, there were sprues on the tire, like on real tires =)
Something like a ship mine...
...let's return to the current upgraded tire model:
Dip the brush into the starch and smuggle the entire matrix. The starch will act as a separator. We mix silicone with starch
Put it into the mold and tighten it all with screws. Cool worms crawled out
Silicone with starch hardens (polymerizes) to moderate hardness in 40 minutes. It's always humid there. You can also pour water into it
The disk for the tire can be made in any shape you like, it all depends on the imagination. I made a simple blank and put a tire on it so that it would be fun to ride it all.
I made a simple blank and put a tire on it so that it would be fun to ride it all.
Of course, this tire is not reinforced and is not designed for high speeds. The speed was checked by touching the grinding wheel, the tire was already visually inflated at 4k rpm. There is an idea to make tires with sickle reinforcement, at least along the layer under the tread. Then it should be less inflated.
Small performance characteristics of tires:
- diameter - 70 mm
- weight - 37 g
- width 25 mm
- plastic left - 47m
) Kamaz model or similar.
Here is another use of a 3D printer in an intermediate stage and without the use of flex.
I bow out for this, I still have things to do =)
Loading
11/18/2022
482
12
Follow author
Follow
Don't want
And again, hello everyone!
I continue to shoot video in a new format, let's see how fast. ..
..
Read more
Egen_M
Loading
11/16/2022
2397
eleven
Subscribe to the author
Subscribe
Don't want
The New Year is getting closer and closer, preparations are in full swing, in anticipation of this event, another was born ...
Read more
176
Subscribe to the author
Subscribe
Don't want
Hello again, dear colleagues!
I'll start my story with a joke of hum...
Read more
Uptis - 3D Printed Airless & Puncture Resistant Tire
Uptis - 3D Printed Airless & Puncture Resistant Tire
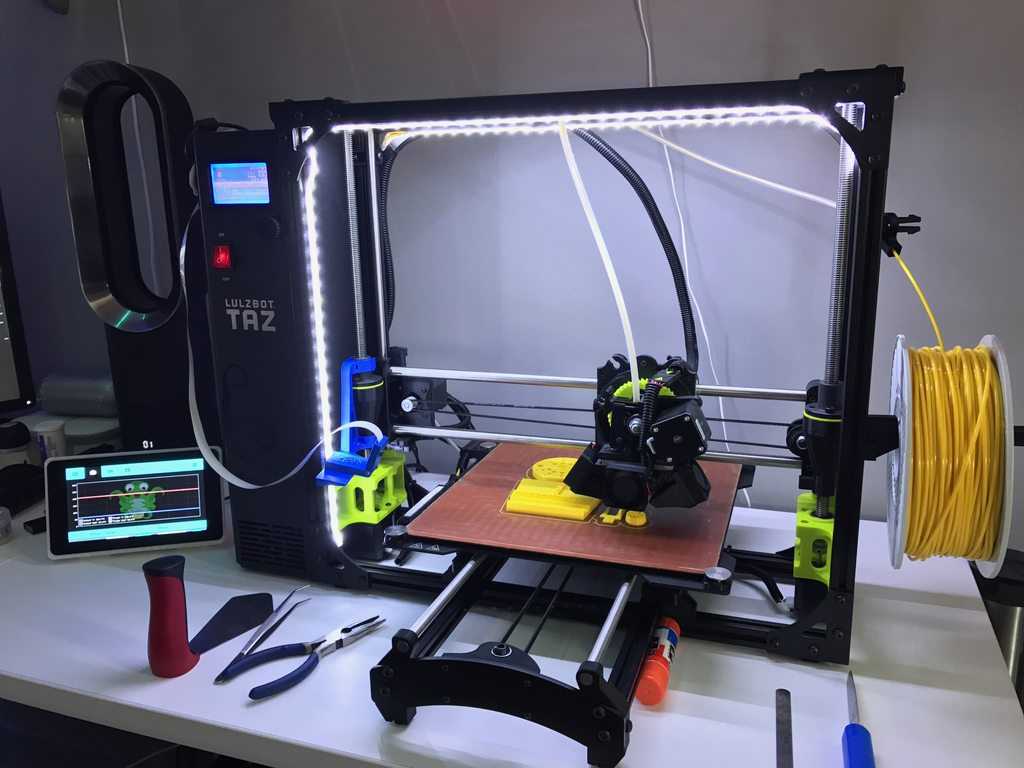
French tire maker Michelin has unveiled its first additive manufacturing-supported prototype tire – called Uptis (French for Unique Puncture Resistant System) and is a mounted assembly engineered without air to avoid all punctures.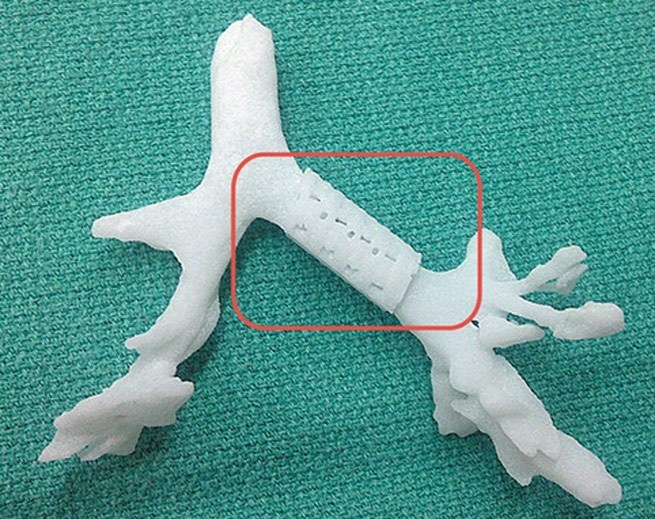 The company worked with US manufacturer General Motors, which is already a user of 3D printed , to unveil a 3D printed prototype at the Movin'On Sustainable Mobility Summit in Montreal. With this puncture-resistant tire, they hope to reduce the number of discarded tires due to punctures and provide better safety for motorists.
The company worked with US manufacturer General Motors, which is already a user of 3D printed , to unveil a 3D printed prototype at the Movin'On Sustainable Mobility Summit in Montreal. With this puncture-resistant tire, they hope to reduce the number of discarded tires due to punctures and provide better safety for motorists.
In 2017, Michelin introduced a new Vision tire concept based on four main features: it is a connected airless system with a tread pattern printed on 3D printer , easily adjustable and developed with biomaterials. Their new Uptis tire could well equip some vehicles by 2024. According to the company, about 20% of the world's tires are discarded due to punctures, which equates to 200 million units! This is a startling observation that Michelin and General Motors want to solve with an airless tire.
Uptis, is the future of tires possible with 3D printing?
The two partners did not disclose more information about how this tire was made - it is not known if it will contain a 3D-printed tread. However, 3D technology was used to build the prototype and we can tell that Michelin wants to develop the Vision concept. They explained that they used composite materials to manufacture Uptis, materials that are fully compatible with additive manufacturing. Eric Viness, Michelin Group vice president of research and development, said: “The Uptis prototype demonstrates Michelin's ability to innovate both in high-tech materials and in its development approach in close collaboration with GM. This partnership further strengthens our innovation roadmap, based on our Vision concept.”
However, 3D technology was used to build the prototype and we can tell that Michelin wants to develop the Vision concept. They explained that they used composite materials to manufacture Uptis, materials that are fully compatible with additive manufacturing. Eric Viness, Michelin Group vice president of research and development, said: “The Uptis prototype demonstrates Michelin's ability to innovate both in high-tech materials and in its development approach in close collaboration with GM. This partnership further strengthens our innovation roadmap, based on our Vision concept.”
This airless tire should significantly reduce the number of punctures, giving motorists some peace of mind as well as improving performance for all professional operations. Finally, the ultimate goal of Uptis is above all to conserve materials, reduce waste and promote more sustainable mobility. Michelin and General Motors will conduct the first tests on vehicles such as the Chevrolet Bolt EV in the United States later this year.