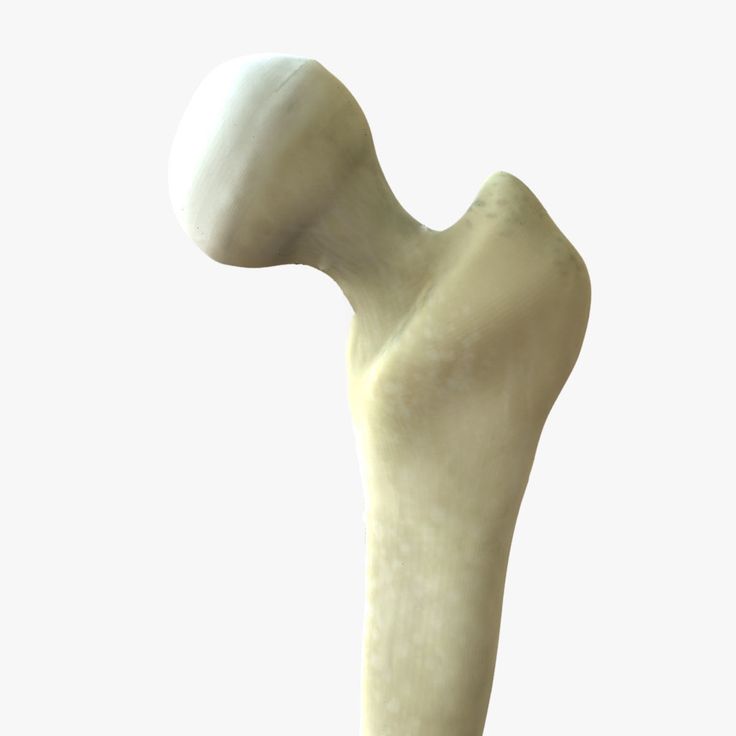
3D printed titanium femur
Titanium femurs are real, but so are their risks
For February, we’re focusing on the body parts that shape us, oxygenate us, and power us as we take long walks on the beach. Bony bonafide bones. These skeletal building blocks inspire curiosity and spark fear in different folks—we hope our stories, covering everything from surgeries and supplements to good old-fashioned boning, will only do the first. Once you’ve thoroughly blasted your mind with bone facts, check out our previous themed months: muscle and fat.
In a 2017 episode of ABC’s medical drama, The Good Doctor, a patient’s thigh bone is so shattered following an accident that, instead of amputating the leg, the physicians in the show 3D-print a titanium femur and insert it into the man’s leg. Presto: The limb is saved. The episode is called “Not Fake”—a reference to the fact that the artificial bone is real. It’s just not biological.
The plot resonated with me because I have a real artificial hip, a prosthesis made of titanium, ceramic, and polyethylene plastic. And I’m happy about it; it’s done a better job at getting me out of pain than previous hip surgeries, which didn’t involve replacing the joint, did. And while I expected the idea of a giant artificial femur to be TV fiction, they’re actually real, too. They’re rare, and not without the possibility of major complications, but they could allow a surgeon to save a limb—just not in the way that The Good Doctor presents.
“They do exist,” says Michael Alexiades, an orthopedic surgeon at the Hospital for Special Surgery in New York, “and they don’t necessarily need to be 3D-printed.” Instead, medical-device companies like Zimmer or Stryker manufacture full replacements or sections of a femur, and surgeons can adjust the size of the implant to fit the patient. An artificial humerus, the big bone in the upper arm, also exists.
These “megaprostheses” are only used as an extreme option. One of the main reasons a patient might need an artificial femur—called a “total femur” in the medical industry—isn’t a traumatic accident: It’s cancer. “There are specific tumors that have a predilection for the femur itself,” says Neil Sheth, the chief of orthopedic surgery at Pennsylvania Hospital. Most of a femur’s growth happens in the area down by the knee, and as that growth is happening, a tumor can develop there. In those events a surgeon may need to replace part of the femur, or the entire bone, with a megaprosthesis.
“There are specific tumors that have a predilection for the femur itself,” says Neil Sheth, the chief of orthopedic surgery at Pennsylvania Hospital. Most of a femur’s growth happens in the area down by the knee, and as that growth is happening, a tumor can develop there. In those events a surgeon may need to replace part of the femur, or the entire bone, with a megaprosthesis.
Another is because of complications that can stem from having an artificial joint. Surgeons install hundreds of thousands of artificial hips and knees into patients each year in the US. Experts have fine-tuned the procedure and devices over the decades so that a patient can receive a new hip and go home the same day, as I did; the new part can last for an estimated 25 years or more. But some artificial joints become infected or develop other problems, forcing surgeons to revise earlier work and replace them. That can lead to bone loss in the areas that the artificial joint attaches to.
In those cases—a tumor on the bone, or severe problems resulting from artificial joints—the surgeon may install a total femur, connecting an artificial hip with an artificial knee. Having one is a sign that a patient has been through some serious medical trauma: “Something went very wrong somewhere along the way,” Sheth says.
Having one is a sign that a patient has been through some serious medical trauma: “Something went very wrong somewhere along the way,” Sheth says.
Using these kinds of big prosthetics is a last resort before amputation, and surgeons always prefer to preserve as much of the body’s natural biological material. Once it’s out, it’s not going back in, and the replacement hardware can cause further complications. For instance, if a total femur becomes infected, Sheth says a patient may potentially lose the entire leg.
While artificial hips are typically a successful procedure, total femurs are dicier. One small study from Munich, Germany of 22 cases pegs the failure rate at nearly 60 percent. Failure in that context means that the patient needed another surgery because of serious complications, like a deep infection or the hardware mechanically breaking. (The study’s first author is aware of at least two individuals who ended up having their leg amputated anyway after the study period ended. ) Meanwhile, Nicolas Piuzzi, an orthopedic surgeon at the Cleveland Clinic in Ohio, puts the risk of needing a subsequent surgery slightly lower, from 20 to 50 percent at five years following a megaprosthesis’s implantation. In short, it’s risky.
) Meanwhile, Nicolas Piuzzi, an orthopedic surgeon at the Cleveland Clinic in Ohio, puts the risk of needing a subsequent surgery slightly lower, from 20 to 50 percent at five years following a megaprosthesis’s implantation. In short, it’s risky.
It’s reasons like these that surgeons say the main goal is to avoid having to put a big prosthesis in patients in the first place: Their aim is to keep or even regenerate the body’s natural tissue if they can. After all, bones are made of living cells. “The frontier is really in trying to restore native things,” says Geoffrey Marecek, an orthopedic trauma surgeon at Keck Medicine of the University of Southern California.
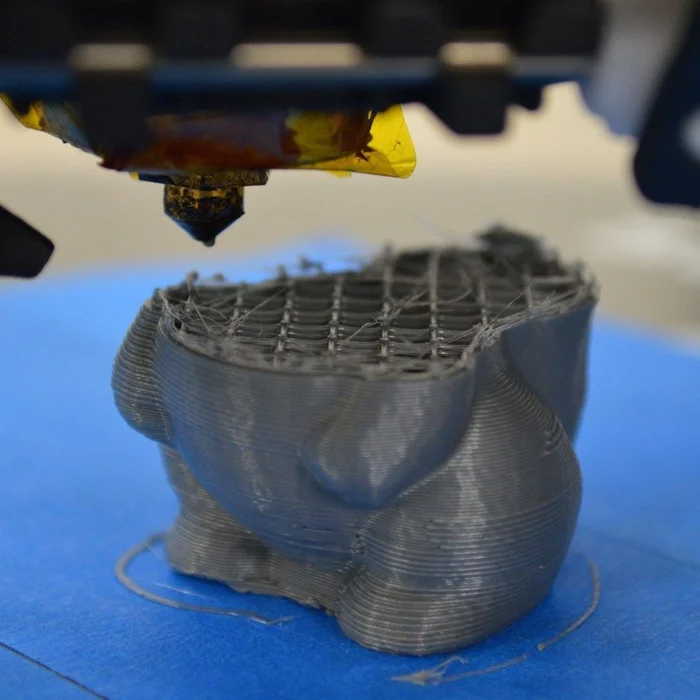
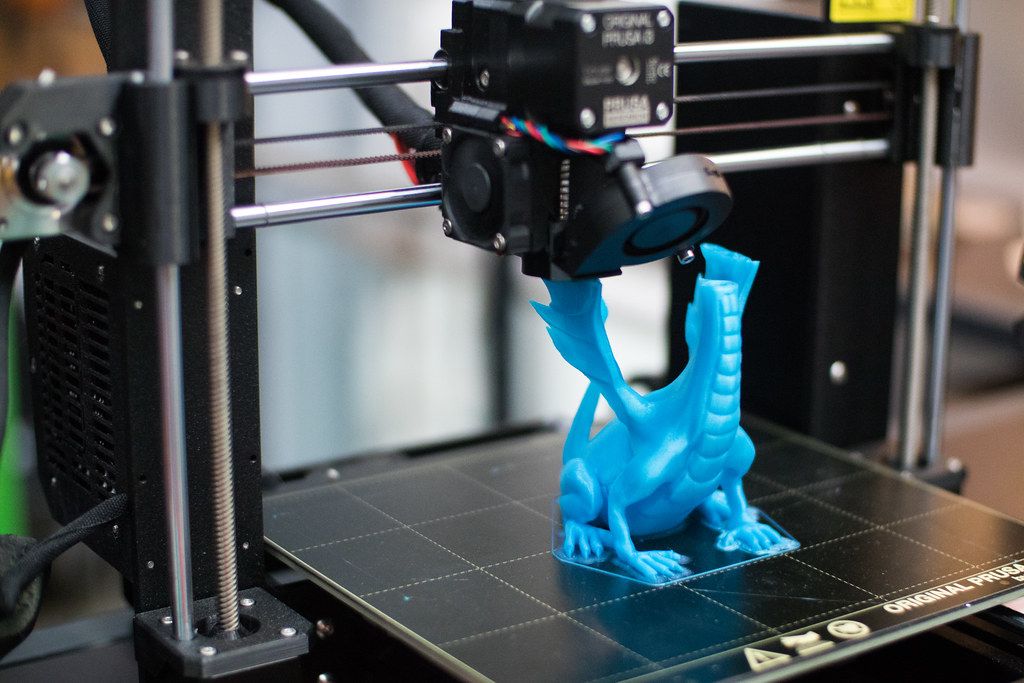
Instead of 3D printing a titanium femur like in The Good Doctor, a better use of synthetic materials would be to employ it to guide new bone growth. Marecek envisions a scenario where practitioners 3D print scaffolding in the shape of a patient’s bone, and then add stem cells, or perhaps bone from elsewhere in the patient’s body. “With that we’re able to actually generate a new femur, rather than having to resort to using a metal and plastic new femur,” he says.
“With that we’re able to actually generate a new femur, rather than having to resort to using a metal and plastic new femur,” he says.
“That’s where we’re all trying to get,” he adds. It’s a push-pull between using artificial materials where they work well—like in prosthetic hips—and looking for new ways to not have to use synthetic substitutes.
At NYU Langone Health, Timothy Rapp, a surgeon who focuses on removing tumors from bones, does something in between the two ideas. In some rare cases, like removing a tumor from a patient’s pelvis, he’ll use a 3D printed-plastic component that’s been custom-created based on CT scans of the patient’s anatomy. The part (which he says resembles a dog toy) then becomes a template for cutting. “We can use these custom-made jigs that you can screw into somebody’s bone, and then accurately cut out the bone that you want and reconstruct it,” Rapp says.
Other 3D-printed plastic can then help them carefully excise healthy bone from another part of the patient’s anatomy, like the fibula, to fill the space where they’ve cut out the tumor.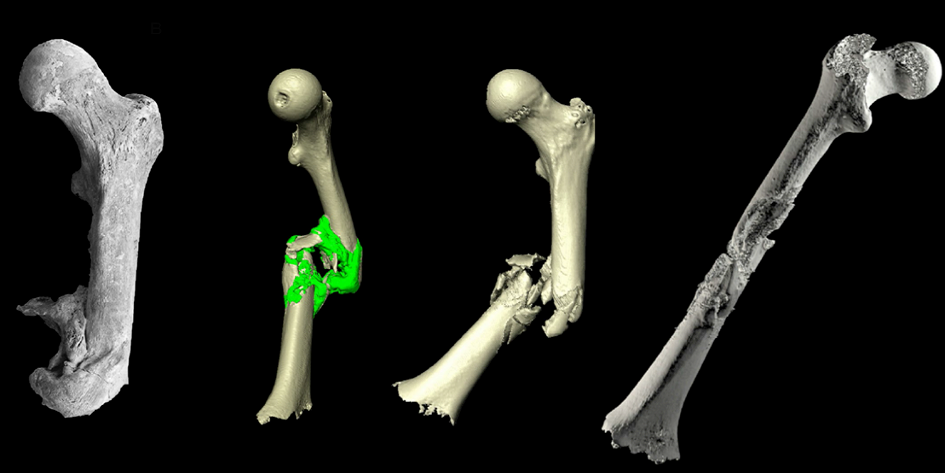 Rapp credits the technique with speeding up his work in the operating room.
Rapp credits the technique with speeding up his work in the operating room.
When the situation calls for it, however, Rapp will implant a megaprosthesis like a total or partial femur. The goal in those cases, as usual, is to prevent amputation. “It’s not going to make them a robot,” he says. “It’s not going to make them perfect.”
In other words, artificial femurs are imperfect but serve a crucial purpose. “Patients that come in that need a total femur replacement—their expectations are on the ground,” says Sheth of Pennsylvania Hospital. “If I can put this in, get them out of pain, and save their limb, their expectation has been so superseded compared to what they thought was going to happen.” That’s in stark contrast to someone receiving a hip replacement, who expects the new joint to be better than the natural one they had before.
Like Marecek, however, Sheth hopes for something beyond artificial components. “I truly believe that in the next half century-plus, people will probably think that we were barbarians, replacing joints with metal and plastic,” he says. “They’ll come up with a biologic solution at some point.”
“They’ll come up with a biologic solution at some point.”
Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty
. 2017 Aug;35(8):1774-1783.
doi: 10.1002/jor.23445. Epub 2016 Oct 4.
Sajad Arabnejad 1 , Burnett Johnston 1 , Michael Tanzer 2 , Damiano Pasini 1
Affiliations
Affiliations
- 1 Department of Mechanical Engineering, McGill University, Macdonald Engineering Building, Rm 372, 817 rue Sherbrooke Ouest, Montreal, Quebec, h4A0C3, Canada.
- 2 Division of Orthopaedics, Department of Surgery, McGill University, Jo Miller Orthopaedic Research Laboratory, Montreal, Quebec, h4G1A4, Canada.

- PMID: 27664796
- DOI: 10.1002/jor.23445
Free article
Sajad Arabnejad et al. J Orthop Res. 2017 Aug.
Free article
. 2017 Aug;35(8):1774-1783.
doi: 10.1002/jor.23445. Epub 2016 Oct 4.
Authors
Sajad Arabnejad 1 , Burnett Johnston 1 , Michael Tanzer 2 , Damiano Pasini 1
Affiliations
- 1 Department of Mechanical Engineering, McGill University, Macdonald Engineering Building, Rm 372, 817 rue Sherbrooke Ouest, Montreal, Quebec, h4A0C3, Canada.
- 2 Division of Orthopaedics, Department of Surgery, McGill University, Jo Miller Orthopaedic Research Laboratory, Montreal, Quebec, h4G1A4, Canada.
- PMID: 27664796
- DOI: 10.1002/jor.23445
Abstract
Current hip replacement femoral implants are made of fully solid materials which all have stiffness considerably higher than that of bone. This mechanical mismatch can cause significant bone resorption secondary to stress shielding, which can lead to serious complications such as peri-prosthetic fracture during or after revision surgery. In this work, a high strength fully porous material with tunable mechanical properties is introduced for use in hip replacement design. The implant macro geometry is based off of a short stem taper-wedge implant compatible with minimally invasive hip replacement surgery. The implant micro-architecture is fine-tuned to locally mimic bone tissue properties which results in minimum bone resorption secondary to stress shielding. We present a systematic approach for the design of a 3D printed fully porous hip implant that encompasses the whole activity spectrum of implant development, from concept generation, multiscale mechanics of porous materials, material architecture tailoring, to additive manufacturing, and performance assessment via in vitro experiments in composite femurs. We show that the fully porous implant with an optimized material micro-structure can reduce the amount of bone loss secondary to stress shielding by 75% compared to a fully solid implant. This result also agrees with those of the in vitro quasi-physiological experimental model and the corresponding finite element model for both the optimized fully porous and fully solid implant.
The implant macro geometry is based off of a short stem taper-wedge implant compatible with minimally invasive hip replacement surgery. The implant micro-architecture is fine-tuned to locally mimic bone tissue properties which results in minimum bone resorption secondary to stress shielding. We present a systematic approach for the design of a 3D printed fully porous hip implant that encompasses the whole activity spectrum of implant development, from concept generation, multiscale mechanics of porous materials, material architecture tailoring, to additive manufacturing, and performance assessment via in vitro experiments in composite femurs. We show that the fully porous implant with an optimized material micro-structure can reduce the amount of bone loss secondary to stress shielding by 75% compared to a fully solid implant. This result also agrees with those of the in vitro quasi-physiological experimental model and the corresponding finite element model for both the optimized fully porous and fully solid implant. These studies demonstrate the merit and the potential of tuning material architecture to achieve a substantial reduction of bone resorption secondary to stress shielding. © 2016 Orthopaedic Research Society. Published by Wiley Periodicals, Inc. J Orthop Res 35:1774-1783, 2017.
These studies demonstrate the merit and the potential of tuning material architecture to achieve a substantial reduction of bone resorption secondary to stress shielding. © 2016 Orthopaedic Research Society. Published by Wiley Periodicals, Inc. J Orthop Res 35:1774-1783, 2017.
Keywords: additive manufacturing; digital image correlation; porous biomaterial; stress shielding; total hip arthroplasty.
© 2016 Orthopaedic Research Society. Published by Wiley Periodicals, Inc.
Similar articles
-
Strain shielding inspired re-design of proximal femoral stems for total hip arthroplasty.
Cilla M, Checa S, Duda GN. Cilla M, et al. J Orthop Res. 2017 Nov;35(11):2534-2544. doi: 10.1002/jor.23540. Epub 2017 Mar 2. J Orthop Res. 2017. PMID: 28176355
-
Design optimization of skeletal hip implant cross-sections using finite-element analysis.

Beulah P, Sivarasu S, Mathew L. Beulah P, et al. J Long Term Eff Med Implants. 2009;19(4):271-8. doi: 10.1615/jlongtermeffmedimplants.v19.i4.40. J Long Term Eff Med Implants. 2009. PMID: 21083533
-
Multiscale design and multiobjective optimization of orthopedic hip implants with functionally graded cellular material.
Arabnejad Khanoki S, Pasini D. Arabnejad Khanoki S, et al. J Biomech Eng. 2012 Mar;134(3):031004. doi: 10.1115/1.4006115. J Biomech Eng. 2012. PMID: 22482684
-
Femoral Stems With Porous Lattice Structures: A Review.
Liu B, Wang H, Zhang N, Zhang M, Cheng CK. Liu B, et al. Front Bioeng Biotechnol. 2021 Nov 17;9:772539. doi: 10.3389/fbioe.2021.772539. eCollection 2021.
 Front Bioeng Biotechnol. 2021. PMID: 34869289 Free PMC article. Review.
Front Bioeng Biotechnol. 2021. PMID: 34869289 Free PMC article. Review. -
Long-term implant fixation and stress-shielding in total hip replacement.
Sumner DR. Sumner DR. J Biomech. 2015 Mar 18;48(5):797-800. doi: 10.1016/j.jbiomech.2014.12.021. Epub 2014 Dec 18. J Biomech. 2015. PMID: 25579990 Review.
See all similar articles
Cited by
-
On the Evolution of Additive Manufacturing (3D/4D Printing) Technologies: Materials, Applications, and Challenges.
Mahmood A, Akram T, Chen H, Chen S. Mahmood A, et al. Polymers (Basel). 2022 Nov 3;14(21):4698. doi: 10.3390/polym14214698. Polymers (Basel). 2022. PMID: 36365695 Free PMC article. Review.

-
Stress Shielding and Bone Resorption of Press-Fit Polyether-Ether-Ketone (PEEK) Hip Prosthesis: A Sawbone Model Study.
Naghavi SA, Lin C, Sun C, Tamaddon M, Basiouny M, Garcia-Souto P, Taylor S, Hua J, Li D, Wang L, Liu C. Naghavi SA, et al. Polymers (Basel). 2022 Oct 29;14(21):4600. doi: 10.3390/polym14214600. Polymers (Basel). 2022. PMID: 36365594 Free PMC article.
-
Minimum 2-Year Outcomes of a Novel 3D-printed Fully Porous Titanium Acetabular Shell in Revision Total Hip Arthroplasty.
Berlinberg EJ, Kavian JA, Roof MA, Shichman I, Frykberg B, Lutes WB, Schnaser EA, Jones SA, McCalden RW, Schwarzkopf R. Berlinberg EJ, et al. Arthroplast Today. 2022 Oct 12;18:39-44. doi: 10.1016/j.artd.2022.08.007. eCollection 2022 Dec.
 Arthroplast Today. 2022. PMID: 36267391 Free PMC article.
Arthroplast Today. 2022. PMID: 36267391 Free PMC article. -
Mechanical micromodeling of stress-shielding at the bone-implant interphase under shear loading.
Hériveaux Y, Le Cann S, Fraulob M, Vennat E, Nguyen VH, Haïat G. Hériveaux Y, et al. Med Biol Eng Comput. 2022 Nov;60(11):3281-3293. doi: 10.1007/s11517-022-02657-2. Epub 2022 Sep 28. Med Biol Eng Comput. 2022. PMID: 36169903
-
Investigation of the Performance of Ti6Al4V Lattice Structures Designed for Biomedical Implants Using the Finite Element Method.
Alkentar R, Máté F, Mankovits T. Alkentar R, et al. Materials (Basel). 2022 Sep 13;15(18):6335. doi: 10.3390/ma15186335. Materials (Basel). 2022. PMID: 36143651 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Grant support
- CIHR/Canada
3D Printed Titanium Implant Improves Hip Revision Surgery - surgical-techniques
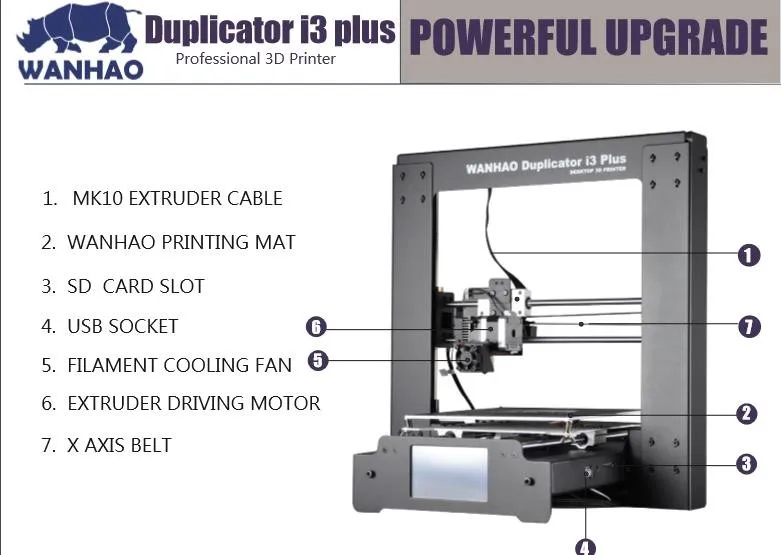
Porous REDAPT Acetabular Revision Cup (photo courtesy of Smith & Nephew).
The innovative, fully porous implant mimics the structure of natural cancellous bone, providing bone ingrowth to secure the implant in place.
The Porous REDAPT Acetabular Revision Cup is intended for use in cases where defective bone makes fixation and stabilization of the implant difficult, requiring the use of a cementless cup that allows for bone ingrowth. To this end, additive manufacturing technology for titanium is being used to create an alternative to external porous coatings such as sintered pellets or fiber meshes used in other cementless implants. The result of the additive process is a fully porous implant that mimics the natural architecture of human bone.
The cup is also available for use with the new variable angle locking screws that can be used to increase implant stability and minimize micromotion after surgery. The screws work within the unique geometry of the implant to provide both compression and rigid attachment to the acetabulum. The cup can also be used with traditional, non-locking screws. The REDAPT Revision Acetabular Cup is a product of Smith & Nephew (London, United Kingdom) and has been approved by the US Food and Drug Administration (FDA).
The cup can also be used with traditional, non-locking screws. The REDAPT Revision Acetabular Cup is a product of Smith & Nephew (London, United Kingdom) and has been approved by the US Food and Drug Administration (FDA).
“We are thrilled that the new manufacturing process provides surgeons and their patients with this opportunity,” said Mike Donoghue, Vice President of Global Reconstruction at Smith & Nephew. cups for complex revision procedures is just one example of this remarkable technology."
"This fully porous cup gives surgeons flexibility never before possible. The cup is based on efficient technology that makes it amazing," said Prof. Craig Della Valle, Orthopedic Surgeon and Dr. of Rush University Medical Center (Chicago, Illinois, USA), who was involved in the surgical development team of the new REDAPT cup - Retaining screws, a proven screwing system, specialized gaskets and screw hole templates optimized for hard-to-reach areas, really beneficial distinguish it in the process of revision procedure".
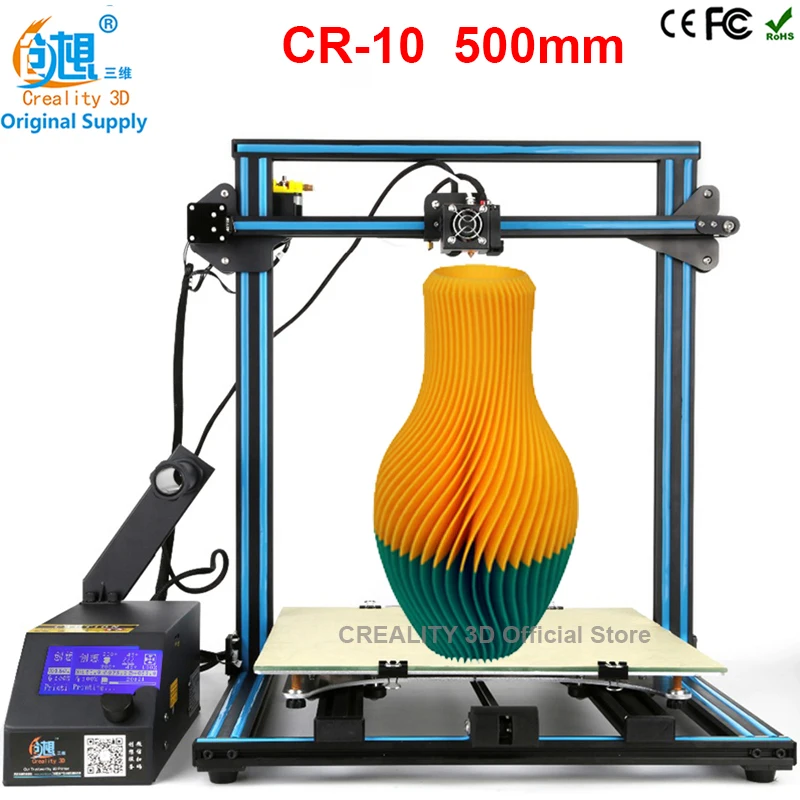
With the CONCELOC technology used to create the REDAPT cup, the laser must be precisely aimed at a thin layer of titanium powder (Ti-6Al-4V). The heat generated by the laser fuses the powder layer by layer until a fully formed titanium structure is formed. The manufacturing process allows the creation of complex structural geometries that are difficult to reproduce, expensive, or impossible using traditional fabrication methods. For example, solid reinforcements can be built directly into the porous structure to provide additional strength at desired locations.
Related Links:
Smith & Nephew
Visit expo >
BMP Whole Blood Analyzer: GEM Premier ChemSTAT
Automated, Random Access Chemistry Analyzer
LIDA 300
Urinalysis Dipstick Control
Dipper Urinalysis Dipstick Control
New
H.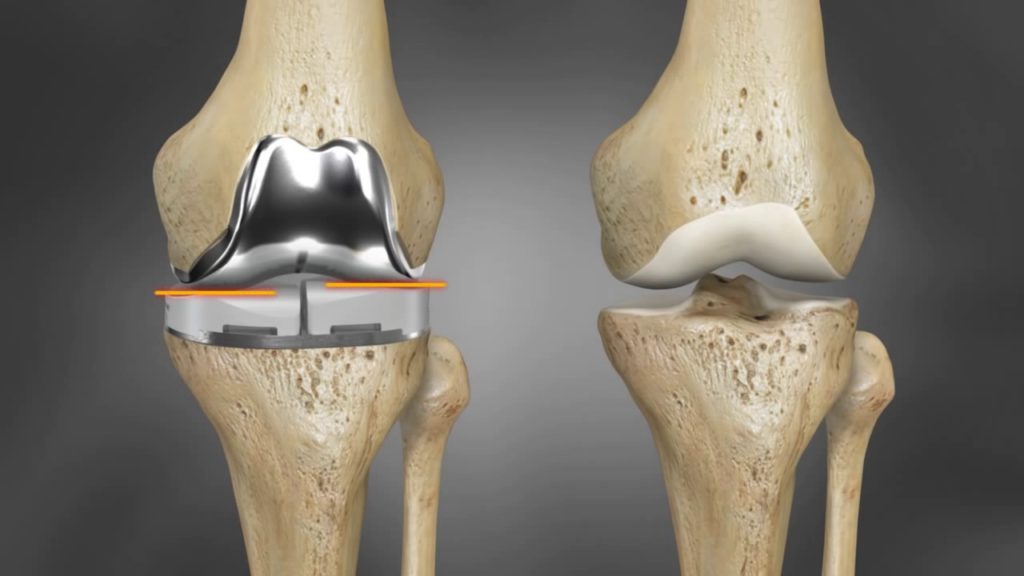 pylori Diagnostic Kit
pylori Diagnostic Kit
Helicosign Dry
Why Medicine Needs 3D Printers
In practice, it looks like this: a patient with a severe injury, skeletal deformity is admitted to the clinic. He is examined, CT and MRI scans are taken. After that, doctors, together with engineers, develop a digital biomodel of the joint to be replaced: they calculate the load, individual shape, design features for a particular patient. On the one hand, the work is "piece". On the other hand, hundreds of operations have already been performed in Russia using 3D printing over the past two years.
- A doctor and an engineer interact remotely: we managed to reduce the manufacturing time of a unique individual titanium implant to one week: from the moment a patient is performed a CT scan to the receipt of the product in the clinic, - says the director of the clinic, head of the Department of Traumatology, Orthopedics and Disaster Surgery, Professor Sechenovsky University Alexei Lychagin.
Which joints can be replaced with "printed" prostheses and implants? Hip, knee and shoulder. In addition, using 3D imaging, doctors correct bone defects in the foot and ankle, knee joint, femur and tibia.
- This method is designed for severe cases, when standard factory implants cannot be dispensed with, a person cannot fully live without an individual prosthesis, notes Alexey Lychagin. - However, in general, the technology allows to solve the problem of almost any bone or joint deficiency. It has proved itself so well in terms of manufacturing accuracy and technical capabilities that in the coming years we plan to use it for wider indications. For example, during the rehabilitation of cancer patients who have lost a large amount of bone tissue. Implant designs will become even more complex over time, they can be used in almost all anatomical regions of the skeleton.
Implants are printed with a metal powder that is 95 percent titanium. Under high temperature, it is laid out layer by layer in a 3D printer strictly according to the form specified by doctors.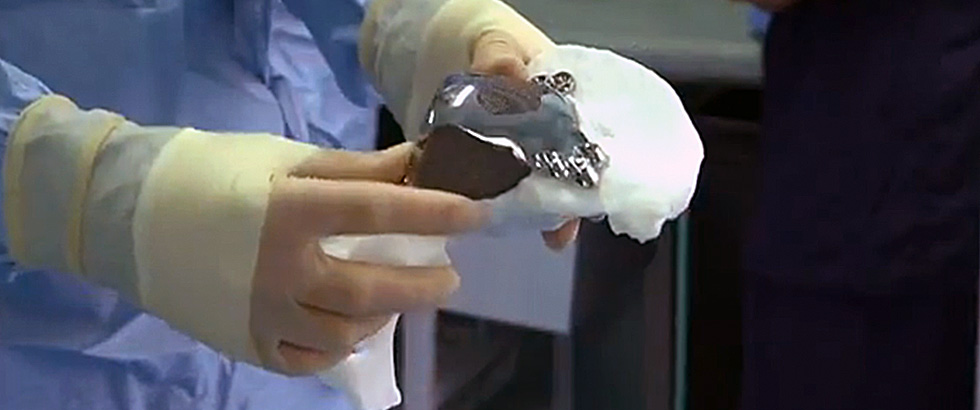 After that, the prosthesis goes through several more stages of heat treatment. As a result, it turns out to be very strong, biocompatible, well integrated into human bone.
After that, the prosthesis goes through several more stages of heat treatment. As a result, it turns out to be very strong, biocompatible, well integrated into human bone.
Hundreds of operations have already been carried out in Russia with the help of 3D printing over the past two years
Sechenov University specialists plan to reduce the entire 3D chain to one to three days. This means that the implant will be ready as soon as the patient undergoes the necessary preoperative examination. You will no longer have to wait for a new titanium "bone" and postpone the operation because of this.
- For faster implantation of such structures, new surgical instruments specially oriented to 3D technology will be developed, - says Alexey Lychagin. - All this will make it possible to carry out the most complex orthopedic operations at the level of those that are considered standard today. The number of operations using individual designs will increase, and the time of the operations themselves will decrease.