3D printed cartilage to treat osteoarthritis
3D-printed living tissues could spell the end of arthritis
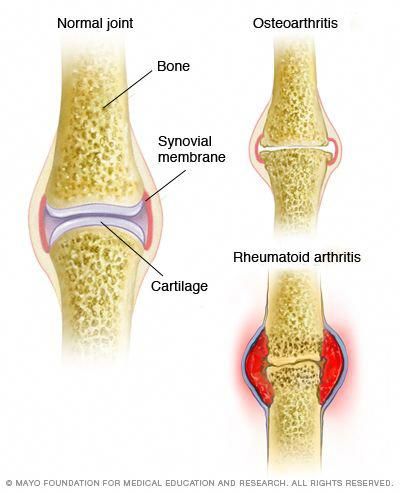
It’s a development that could reduce the discomfort and pain of the one in 10 people who will suffer from arthritis over their lifetime. Arthritis acts by breaking down the rubbery cartilage tissue found in joints, leading to pain, stiffness and swelling.
But 3D printing technology could enable new cartilage to be printed on demand using patients’ own cells as the building blocks – a technique known as bioprinting.
Professor Jos Malda is working with such 3D bioprinting in his lab at the University Medical Centre Utrecht in the Netherlands. As part of a project called 3D-JOINT, his team is working to make bioprinted tissues that can be implanted into a living joint to replace the damaged part. These would eventually mature into a tissue that is the same as the original healthy cartilage.
Already, stem cells can be deposited by 3D printers according to a precise blueprint, creating complex tissues layer by layer. Yet that doesn’t mean they can instantly transform into new organs or body parts.
‘Printing is not the last step in biofabrication, since printing something in the shape of a heart does not make it a heart,’ said Prof. Malda. ‘The printed construct needs time and the correct chemical and biophysical cues to mature into a functional tissue.’
One challenge is maintaining the right conditions for the cellular building material.
Traditional 3D printing uses plastics, which are flexible enough to be pushed through a printer nozzle, but are also solid enough to keep their shape afterwards.
But because bioinks contain living cells, scientists are having to develop new solutions. One option is to use a hydrogel - a type of material that consists of networks of large molecules known as polymers, swollen with water.
‘For bioprinting, the material has to be able to keep cells alive. This demands aqueous conditions and processing under a relatively low temperature, which makes hydrogel-based materials ideal candidates,’ Prof. Malda said.
Malda said.
But while the squishy nature of such hydrogels makes them very good at delivering cells, it is also their weakness. They are unable to withstand the mechanical load certain tissues undergo in the body.
Strong
To solve that, Prof. Malda and his team are experimenting with additive materials, which can make the hydrogels strong enough to act as replacement cartilage.
‘Reinforcing the hydrogel makes it stronger – just like steel rods are combined with soft cement to create the reinforced concrete that makes the foundations of our homes,’ Prof. Malda explained.
His team is using melt electrowriting, a 3D-printing technique that combines melted polycaprolactone, a type of polyester, with an electrical field that creates fibres as thin as a hair.
Using these microfibres, the team creates scaffolding to be combined with the cell-containing hydrogel – already with good results.
“'Printing something in the shape of a heart does not make it a heart.
Professor Jos Malda, University Medical Centre Utrecht, the Netherlands'
‘The combination of the hydrogel with the fibres acts in synergy, increasing the strength of the composite over 50 times while still allowing the cells to generate extracellular matrix and mature into a cartilage-like tissue,’ Prof. Malda said.
His team is working on upscaling that process to create larger constructs, while bringing together different materials for combined bone and cartilage tissue replacements. The ultimate goal is to eventually 3D print a complete joint.
In addition to acting as a replacement for lost cartilage and bone, printing cells in this way can also help the body to repair damaged tissues.
Professor Daniel Kelly at Trinity College in Dublin, Ireland, is working as part of a project called JointPrinting to develop such a system – quite a challenge given that the field is still emerging.
‘There are relatively few examples in the literature demonstrating the capacity of bioprinted tissues to actually regenerate damaged tissues in appropriate pre-clinical (animal) models,’ Prof. Kelly said.
Kelly said.
He is working to develop bioinks that are not only printable but which also spur stem cells to make new cartilage by altering the molecules that support and surround the printed cells, instructing them to generate the correct type of tissue.
The idea is that these newly printed stem cells can help repair damaged tissue after they are implanted in the body.
Prof. Kelly’s team is also working with using substances known as growth factors to stimulate the formation of new blood vessels in injured tissues.
‘We sometimes incorporate VEGF (vascular endothelial growth factor) into our bioprinted tissues … to encourage new blood vessels to form in regions of a damaged bone or joint where we want bone to grow,’ he said.
‘We introduce gradiants of VEGF into the bioprinted tissues that directs host blood vessels (to form) into the appropriate regions of our implants.’
Though scientists are focusing on cartilage and bone, demands on joints can differ dramatically depending on where they are located in the body.
To test the printed tissues, Prof. Kelly uses specialised mechanical testing machines to determine their stiffness and elasticity, as well as computational modelling to better understand how the structure and composition of the implants can be tuned to function within specific environments.
All in all, Prof. Kelly is optimistic about the future applications of bioprinting.
‘I think bioprinting will have two main applications. Firstly, as a source of new tissues and organs in regenerative medicine. Secondly, as a tool to better understand human disease and to test the safety and efficacy of new drugs targeting such diseases.’
The research in this article was funded by the EU. If you liked this article, please consider sharing it on social media.
" width=
3D bioprinting research aims to treat osteoarthritis with cartilage replacements
0Shares
Scientists from the Chalmers University of Technology, Gothenburg, Sweden have demonstrated cartilage tissue engineering using 3D Bioprinting.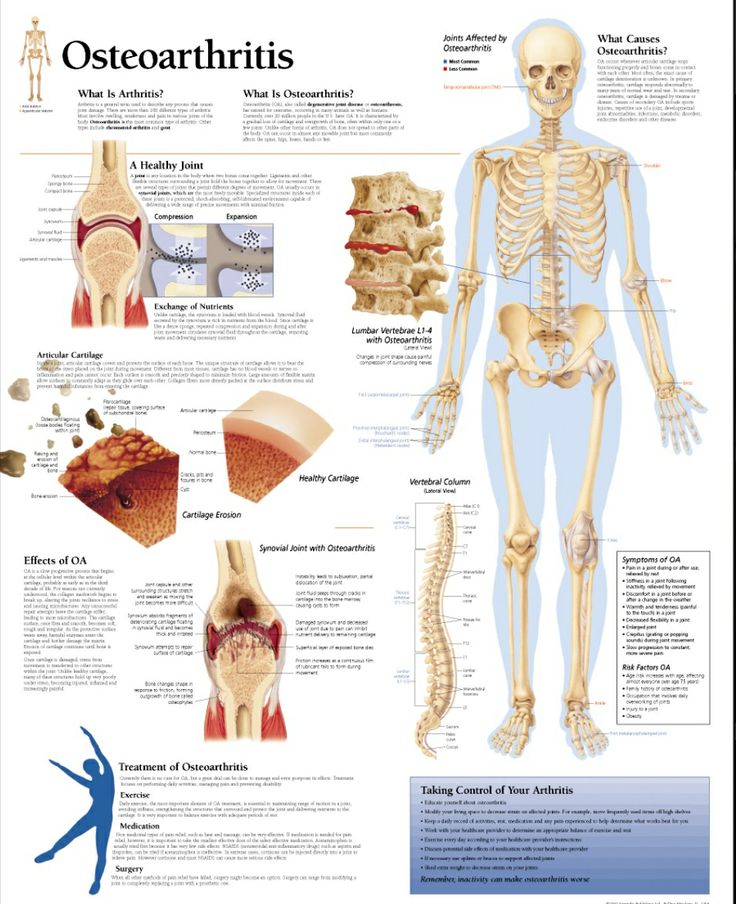 The new research uses 3D printing to produce cartilage replacements and could be used to treat osteoarthritis.
The new research uses 3D printing to produce cartilage replacements and could be used to treat osteoarthritis.
As 3D Printing Industry reported last year, an interdisciplinary project to research 3D printing skin called SkinResQU is also underway and includes Sahlgrenska University Hospital and the University of Gothenburg and Chalmers.
In a new article published by Scientific Reports, the researchers describe how 3D bioprinting, “is anticipated to radically change regenerative medicine because it would enable tissues and organs to be printed on demand.”
Stina Simonsson, Associate Professor of Cell Biology, led the research and said, “In nature, the differentiation of stem cells into cartilage is a simple process, but it’s much more complicated to accomplish in a test tube. We’re the first to succeed with it, and we did so without any animal testing whatsoever.”
A cartilage sample from the new research at the University of Gothenburg.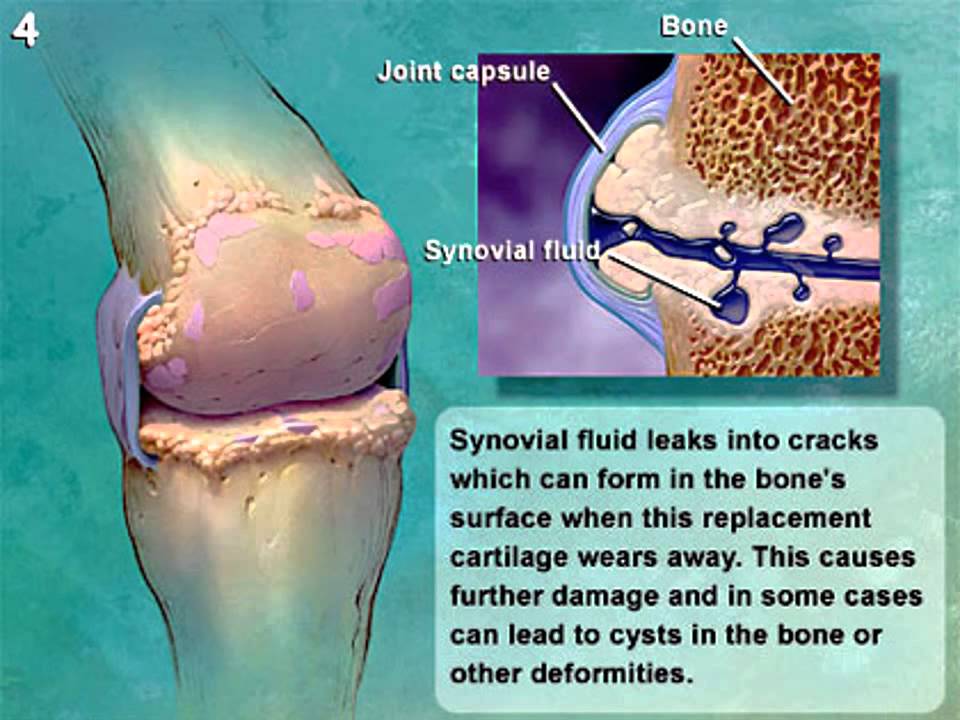
Bioinks fabricated with alginate
The work investigates bioprinted cartilage replacements and may find early clinical application for the treatment of secondary osteoarthritis (OA) and chondral and osteochondral injuries. To conduct the research two bioinks using nanofibrillated cellulose (NFC) were investigated, NFC with alginate (NFC/A) and hyaluronic acid (NFC/HA).
NFC provides structural and mechanical support for forming the physiological mimetic environment. In the case of cartilage, the NFC mimics the bulk collagen matrix, alginate simulates proteoglycans, and hyaluronic hydrogel substitutes for the hyaluronic acid found in cartilage.
A 3D Discovery bioprinter made by regenHu of Switzerland was used with a 300-µm nozzle to conduct the research.
Simonsson explains, “We investigated various methods and combined different growth factors. Each individual stem cell is encased in nanocellulose, which allows it to survive the process of being printed into a 3D structure. We also harvested mediums from other cells that contain the signals that stem cells use to communicate with each other so called conditioned medium.”
We also harvested mediums from other cells that contain the signals that stem cells use to communicate with each other so called conditioned medium.”
3D bioprinting research advances
Other research teams such the ReconRegen group in Swansea are also investigating the use of NFC’s. American Process Inc are working with the ReconRegen group and CEO Theodora Retsina believes that the growing biomedical engineering market will increase from $23 billion currently to over $94 billion by 2022.
Furthermore, researchers at Bristol University have made a bio-ink from two polymers, one of which is extracted from seaweed. The 3D bioprinting work may also have application as a cartilage material.
In conclusion the team of scientists in Sweden found, “that NFC/A bioink is suitable for bioprinting iPSCs to support cartilage production in co-cultures with irradiated chondrocytes.”
“In layman’s terms, our theory is that we managed to trick the cells into thinking that they aren’t alone,” said lead researcher Stina Simonsson.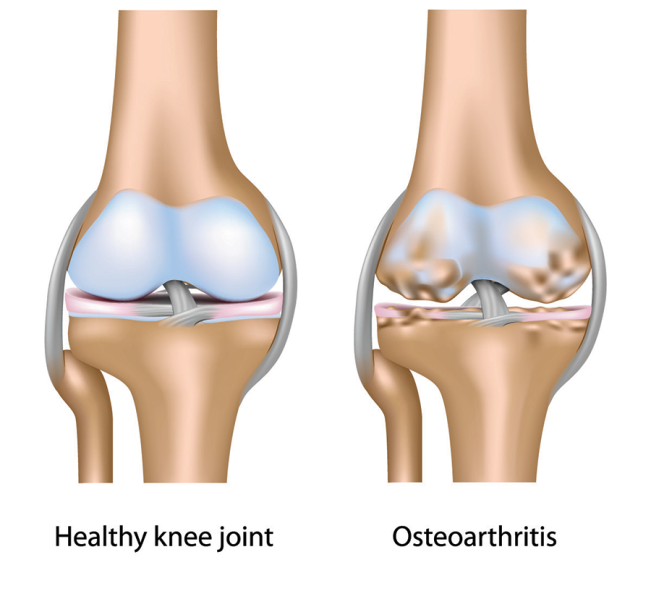
The research article, “Cartilage Tissue Engineering by the 3D Bioprinting of iPS Cells in a Nanocellulose/Alginate Bioink” is available here. The authors of the study are Duong Nguyen, Daniel A. Hägg, Alma Forsman, Josefine Ekholm, Puwapong Nimkingratana, Camilla Brantsing, Theodoros Kalogeropoulos, Samantha Zaunz, Sebastian Concaro, Mats Brittberg, Anders Lindahl, Paul Gatenholm, Annika Enejder and Stina Simonsson.
For all the latest news about the 3D printing industry, subscribe to our newsletter and follow our active social media accounts.
Featured image shows Stina Simonsson who led the research into 3D bioprinting cartilage. Photo via University of Gothenburg/Elin Lindström Claessen.
Tags Alma Forsman Anders Lindahl Annika Enejder Camilla Brantsing Daniel A. Hägg Duong Nguyen Josefine Ekholm Mats Brittberg Paul Gatenholm Puwapong Nimkingratana Samantha Zaunz Sebastian Concaro Stina Simonsson Theodoros Kalogeropoulos
Michael Petch
Michael Petch is the editor-in-chief at 3DPI and the author of several books on 3D printing. He is a regular keynote speaker at technology conferences where he has delivered presentations such as 3D printing with graphene and ceramics and the use of technology to enhance food security. Michael is most interested in the science behind emerging technology and the accompanying economic and social implications.
He is a regular keynote speaker at technology conferences where he has delivered presentations such as 3D printing with graphene and ceramics and the use of technology to enhance food security. Michael is most interested in the science behind emerging technology and the accompanying economic and social implications.
Doctor 3D prints knee cartilage
Archive
Subscribe author
Subscribe
Don't want
Dr. Darryl D'Lima and colleagues at Scripps Clinic in La Jolla, California are working on new technology 3D bioprinting, which will allow the implantation of living cartilage tissue into the patient's body, thereby providing better treatment for knee injuries.
Colleagues consider Dr. D'Lim a very resourceful person. He is a doctor and scientist who uses new technologies from various fields of science to help his patients.
Recently, Dr. D'Lima has been working on a technology to implant 3D-printed cartilage tissue into the patient's body to restore the structure of damaged knees.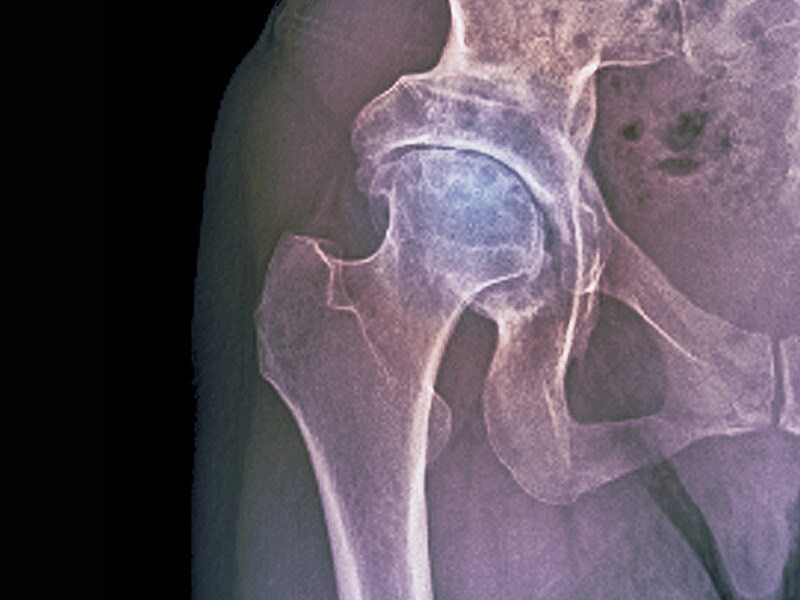 Cartilage is the tissue that connects the knee joints. It is known that it heals slowly and painfully.
Cartilage is the tissue that connects the knee joints. It is known that it heals slowly and painfully.
Doctors now advise patients to endure the pain unless an artificial joint is needed. This procedure also causes severe pain and rarely solves the problem.
Hoping to find an alternative to traditional joint implants, Dr. D'Lima and his team decided to make a 3D bioprinter out of an old HP inkjet printer and print living cartilage tissue on it. The 3D printer sprays a mixture of cartilage progenitor cells and a liquid that hardens under ultraviolet light. Bone cells are also printed on it, which are placed where the cartilage connects to the bone. The volume of a drop of liquid with living cells is 1 picoliter, which is quite enough to correct even microscopic disorders of the patient's bone or cartilage.
Dr. D'Lima compares the process of implanting cartilage into the knee with filling in potholes: “You automatically fill in the depressions during printing. You get cartilage that is perfectly shaped to the existing tissue, which we have never been able to do with conventional implants,” said D’Lima.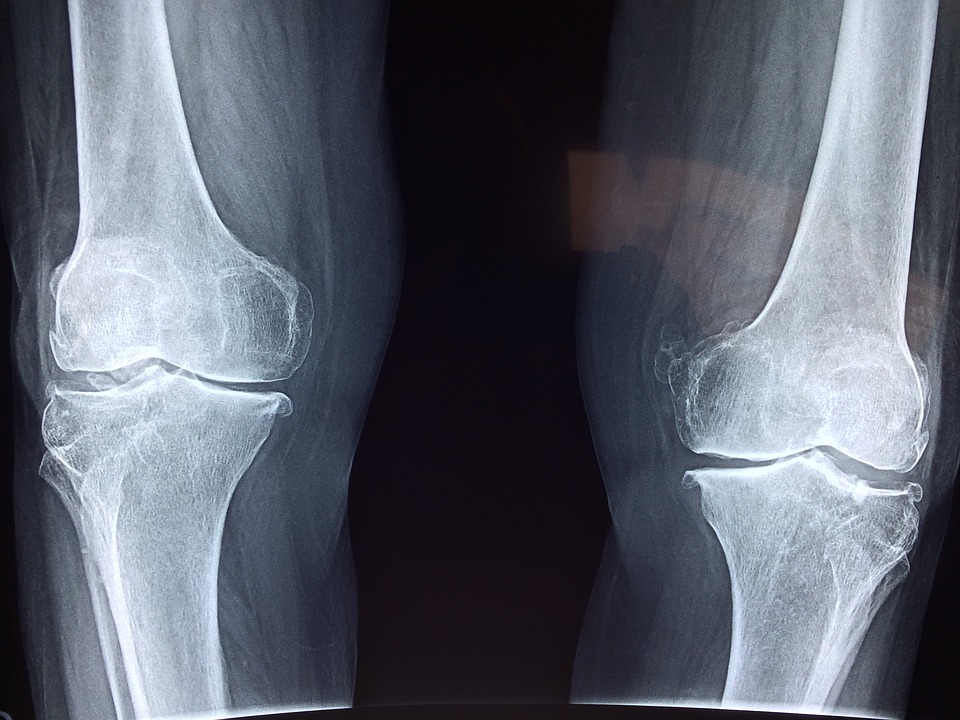 Printing on a pre-existing joint provides a better fit for new and old cartilage than grafting lab-grown cartilage that has to be trimmed to fit better. Another advantage of cartilage printing is that there is no longer a need to postpone the operation for later - it can be done right away.
Printing on a pre-existing joint provides a better fit for new and old cartilage than grafting lab-grown cartilage that has to be trimmed to fit better. Another advantage of cartilage printing is that there is no longer a need to postpone the operation for later - it can be done right away.
People born during the "baby boom" age, and the problem of excess weight is becoming more and more aggravated. This means that in the future, knee injuries will become an even more serious cause for concern. According to a GlobalData report, the knee implant market will grow by 6.8% annually from 2010 to 2017.
Dr. D'Lim and his team's research has been recognized by several institutes. He received a $3.1 million grant from the California Institute for Regenerative Medicine Stem Cell Research Agency to research the use of natural and artificial embryonic stem cells in cartilage growth.
D'Lima believes that it will take at least a year to create a full-fledged 3D bioprinter. He is currently conducting animal experiments to prove the promise of his idea, which is sponsored by the George Schaeffer Family Foundation.
He is currently conducting animal experiments to prove the promise of his idea, which is sponsored by the George Schaeffer Family Foundation.
Similar 3D bioprinting inventions are popping up around the world. Just last month, a prototype 3D printed BioPen was handed over to researchers at St Vincent's Hospital in Melbourne, and Organovo created the world's first 3D printed liver tissue on a printer in its labs.
However, the printing of living tissue is still a very difficult task. For example, to print muscle tissue, you need to synthesize different types of cells and a whole network of blood vessels. Organovo temporarily solved this problem by limiting the thickness of its liver tissue so that it is supplied with blood without vessels.
D'Lima says cartilage is easier to 3D print because it doesn't have blood vessels. He sees far-reaching prospects in the development of 3D bioprinting technology, since it can also be used to recreate other tissues, such as retinal tissue.
Article prepared for 3dtoday.ru
Follow author
Follow
Don't want
Even more interesting articles
7
Subscribe to the author
Subscribe
Don't want
Mikhail Kozenko, a schoolboy from Volgograd, joined the ranks of 3D makers by designing his own 3D...
Read more
7
Subscribe to the author
Subscribe
Don't want
So, you are thinking about the possibility of making money on 3D printing. How realistic is this? Quite, although the way...
Read more
3
Subscribe to the author
Subscribe to the author
Don't want to
More and more RepRap 3D printers based on modeling technology are on the market today.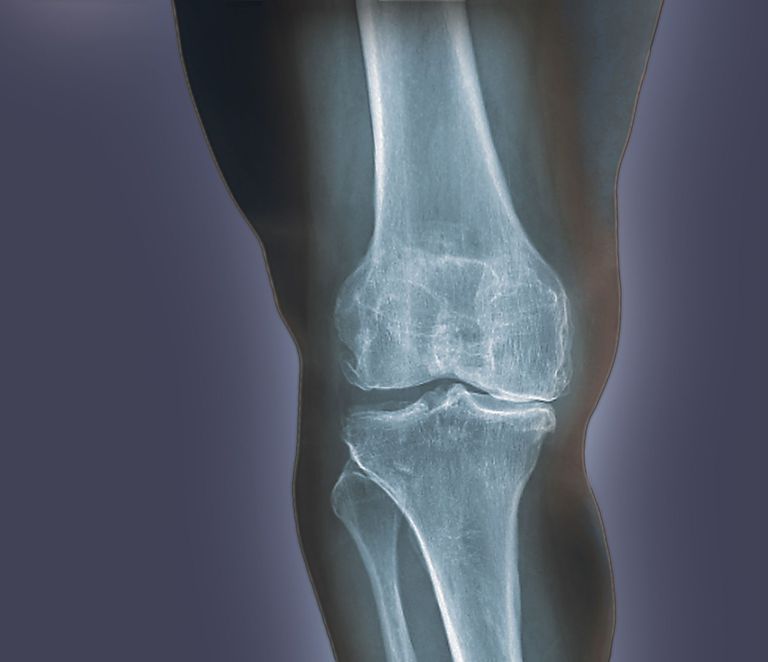 ..
..
Read more
| 3DNews Technologies and IT market. News printers, print servers, scanners, copiers... The new material allows you to print knee... The most interesting in the reviews 05/02/2017 [14:13], Konstantin Khodakovsky Scientists from the American Duke University have created a material that imitates human cartilage and can eventually be used by surgeons for 3D printing of implants to replace damaged parts of the knee joint, individually shaped to the anatomy of each patient. Human knees have a pair of menisci, crescent-shaped cartilages that act as shock absorbers. But over years of stress, these important parts of the joint can wear out, or be severely damaged by one wrong move while playing football or tennis. The result is pain and an increased risk of developing arthritis. Scientists claim their hydrogel-based material is the first to match the strength and elasticity of human cartilage while remaining stable inside the body and allowing it to be used in the 3D printing process. To prove their point, the researchers used a $300 3D printer to print custom menisci for a plastic model of the knee. Duke University Associate Professor of Chemistry and Published Author Benjamin Wiley notes: “We have now made it possible for everyone to print implants that are very similar in medical properties to human cartilage in a fairly simple and relatively inexpensive way.” . It is worth noting that this is indeed an important achievement. The fact is that torn or damaged menisci are very capricious to the process of self-healing. Surgeons often have to partially or completely remove them, and existing implants either do not match the strength and elasticity of the original, or have poor biocompatibility and prevent the healing of the damaged area. |