Wake forest institute for regenerative medicine 3d printing
ABCs of Organ Engineering | Wake Forest University School of Medicine
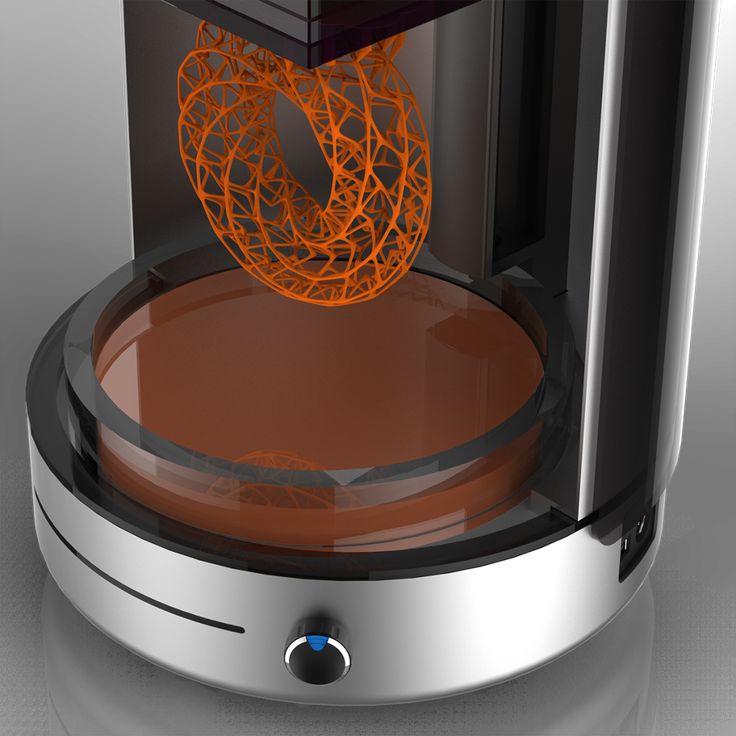
Bioprinting
Using 3D Printing Technology to Print Organs and Tissue
Can replacement organs one day come from a printer? That's the ultimate goal of the institute's bioprinting program. Institute scientists were the first to create a laboratory-grown organ implanted into a human, but they quickly realized the need to scale up the manufacturing process.
Living tissues are composed of many cell types that are arranged in a very specific order. When engineering replacement tissues and organs in the lab, maintaining this order is essential to ensuring that the replacement tissues have the same function that original body parts have.
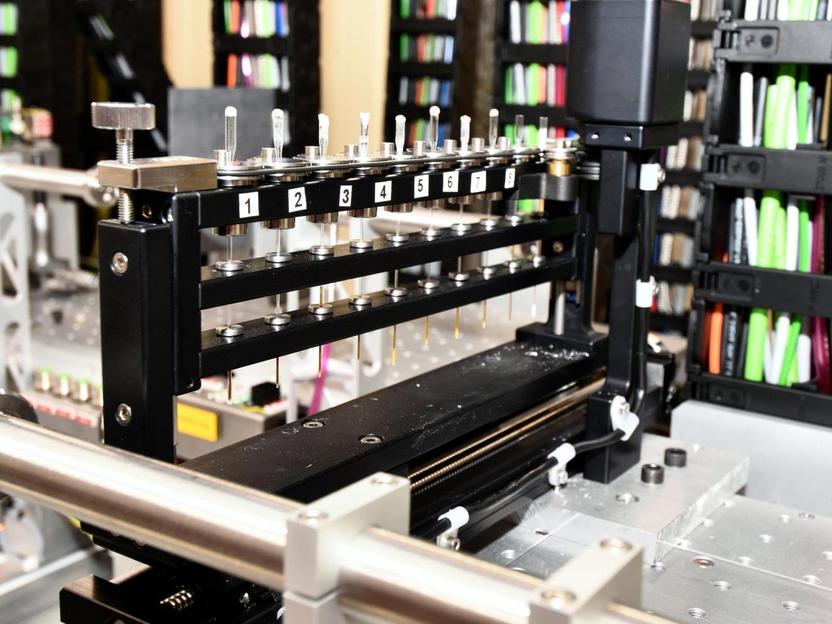
Because of the precision of printing, researchers at the Wake Forest Institute for Regenerative Medicine have been investigating the possibility printing tissues and organs. In their first efforts, they used an actual inkjet desktop printer that was modified to print cells into a 3D shape. Cells were placed in the wells of the ink cartridge and the printer was programmed to print them in a certain order. The printer is now part of the permanent collection of the National Museum of Health and Medicine.
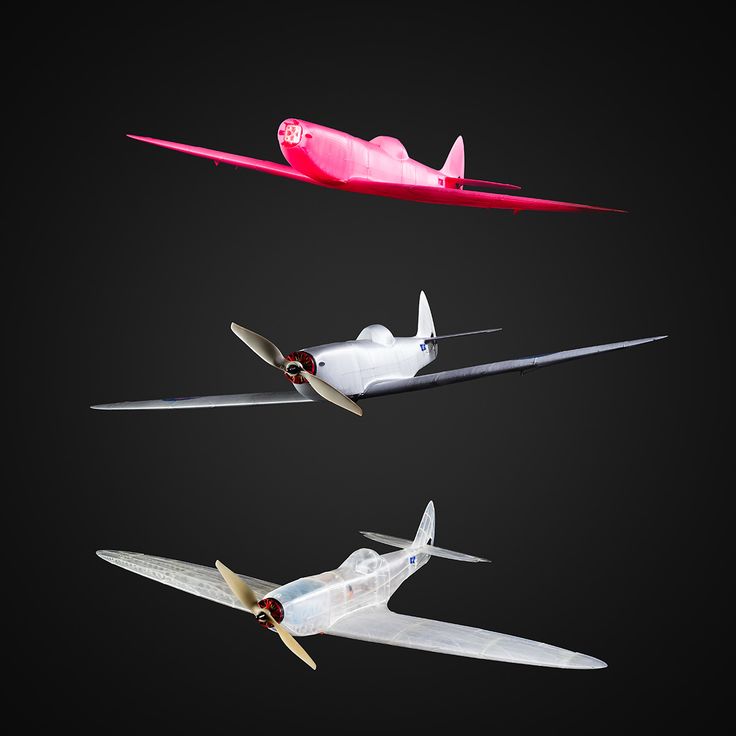
In 2016, the institute announced success printing living tissue structures using a specialized 3D printer that its researchers designed over a decade. The scientists printed ear, bone and muscle structures that, when implanted in animals, matured into functional tissue and developed a system of blood vessels. These early results indicate that the printed structures have the right size, strength and function for use in humans. The series of experiments proved the feasibility of printing living tissue structures to replace injured or diseased tissue in patients.
Skin Printing
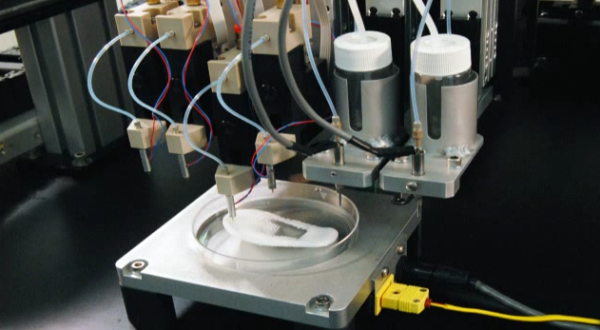
In the not too distant future, a bioprinter filled with a patient's own cells can be wheeled right to the bedside to treat large wounds or burns by printing skin, layer by layer, to begin the healing process. WFIRM scientists have created such a mobile skin bioprinting system -- the first of its kind -- that allows bi-layered skin to be printed directly into a wound. The mobility of the system and the ability to provide on-site management of extensive wounds by scanning and measuring them in order to deposit the cells directly where they are needed to create skin is what makes it so unique.
WFIRM scientists have created such a mobile skin bioprinting system -- the first of its kind -- that allows bi-layered skin to be printed directly into a wound. The mobility of the system and the ability to provide on-site management of extensive wounds by scanning and measuring them in order to deposit the cells directly where they are needed to create skin is what makes it so unique.
Affecting millions of Americans, chronic, large or non-healing wounds such as diabetic pressure ulcers are especially costly because they often require multiple treatments. It is also estimated that burn injuries account for 10-30 percent of combat casualties in conventional warfare for military personnel. The researchers demonstrated proof-of-concept of the system by printing skin directly onto pre-clinical models. The next step is to conduct a clinical trial in humans.
Quality Assurance
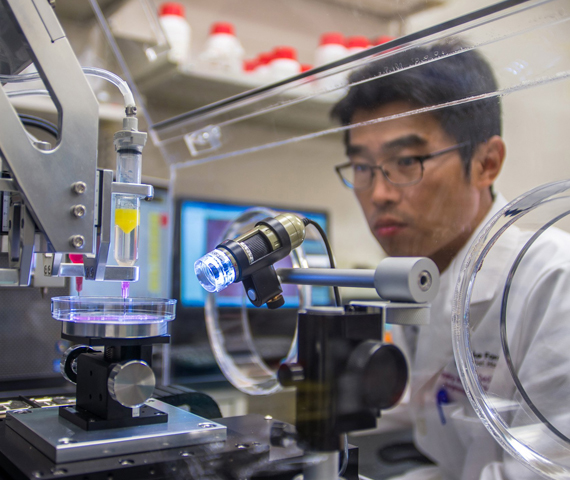
Using High-Powered Microscopes to Ensure the Effectiveness of Engineered Cells
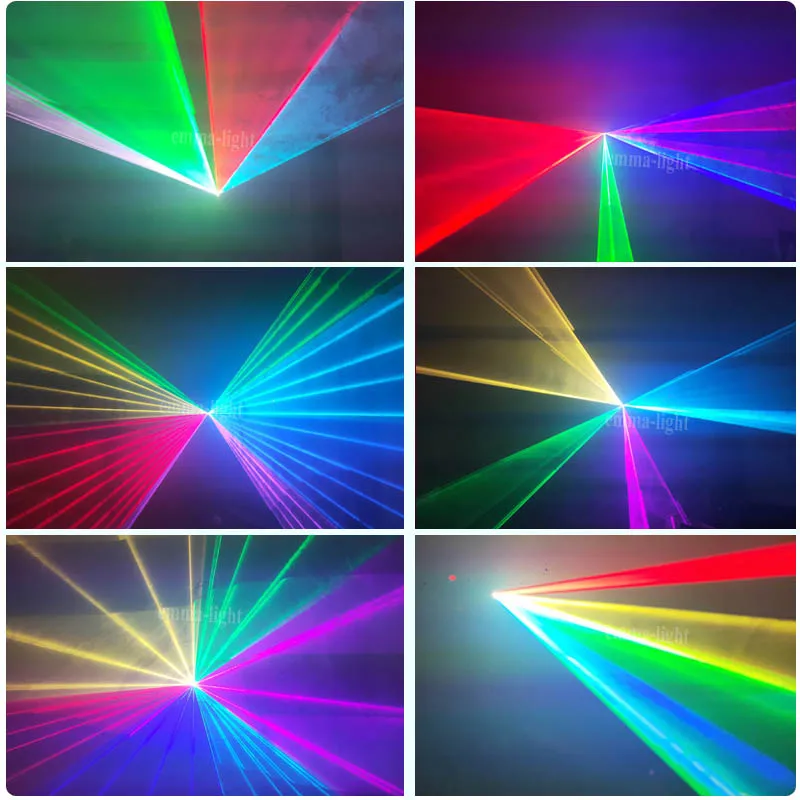
High-powered microscopes are critical to the field of tissue engineering and regenerative medicine. Light microscopes, which use light to detect small objects, allow scientists to assess the size, shape and activity of engineered cells to ensure that they will function properly in the body. Light microscopy is also commonly used to visualize whole engineered tissues and organs.
Light microscopes, which use light to detect small objects, allow scientists to assess the size, shape and activity of engineered cells to ensure that they will function properly in the body. Light microscopy is also commonly used to visualize whole engineered tissues and organs.
Conofocal laser scanning microscopy is used to obtain high-resolution images of thick samples, including tissue. Using a process known as optical sectioning, the technology enables images to be acquired point-by-point and then reconstructed with a computer, which provides three-dimensional images.
Scanning electron microscopy uses electrons to create images of the tiny details on the surface of materials. The scanning electron microscope at the Wake Forest Institute for Regenerative Medicine is specially designed to investigate biological specimens such as scaffolds and engineered tissue. Because scanning electron microscopy provides images that greatly exceed the magnification of conventional microscopes, this technology allows us to view scaffolds intricately to determine if cells are adhering properly.
Testing Functionality
Organ Baths Test the Functionality of Engineered Tissue
Tissues and organs that are developed in the laboratory have to do more than simply look like the tissue and organs they will replace; they have to function like them as well. We utilize an organ bath, an experimental set-up, to test laboratory-engineered tissue. With organ bath experiments, we can study how our generated tissues respond to chemical agents and electrical impulses to ascertain whether their responses are normal.
In our organ baths, tissue is suspended in a temperature-controlled chamber. The tissue's contractile function is recorded on a computer. Through a comparison of the tissue's contraction and relaxation responses to that of normal tissue, we're able to assess the functionality of engineered tissue.
A Record of Firsts - Wake Forest Institute for Regenerative Medicine
Achievements of Institute scientists include engineering replacement tissues and organs in all four categories: flat structures, tubular tissues, hollow organs and solid organs.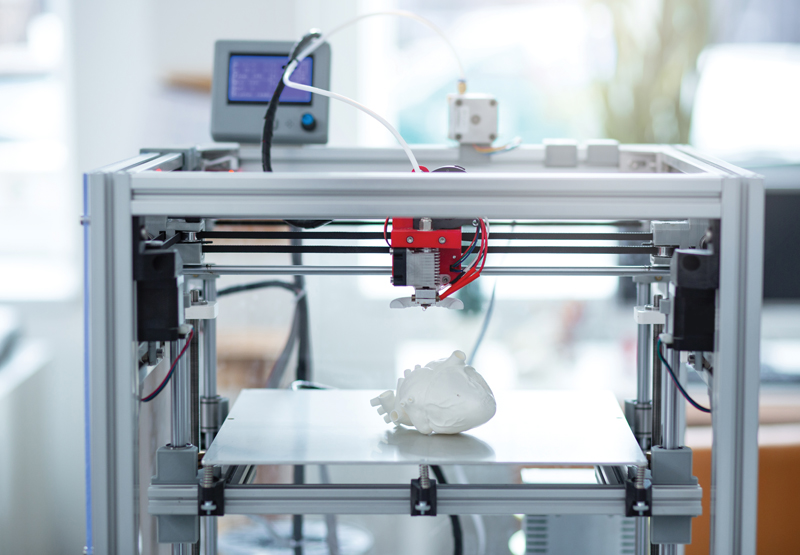
- First to demonstrate that complex, layered tissue structures can be engineered using cells. (1994)
- Developed the first tissue-engineered product to go to the U.S. Food and Drug Administration for Phase 1 approval for clinical applications, consisting of cells and biomaterials for injectable therapy. (1995)
- First to use biomaterials alone, without addition of cells, implanted in patients for the regeneration of organs. (1996)
- First to create a laboratory-grown organ — engineered bladder tissue (hollow organ) that was successfully implanted in patients. (1999 first implantation; publication 2006)
- First to create a functional experimental solid organ, a miniature kidney that secretes urine. (2003)
- Led the team that engineered tubular organs (urine conduits) and implanted them in patients.
(2004 first implantation; publication 2011) - Founded the Regenerative Medicine Foundation, a non-profit organization dedicated to the advancement of regenerative medicine treatments and therapies.
 (2005)
(2005) - Proved feasibility of printing living tissue structures to replace injured or diseased tissue in patients. (2006)
- Identified and characterized a new source of stem cells derived from amniotic fluid and placenta, which show promise for the treatment of many diseases. (2007)
- Selected to co-lead the Armed Forces Institute of Regenerative Medicine, an $85 million, federally funded effort to apply regenerative medicine to battlefield injuries. (2008)
- Started the first initiative for regenerative medicine manufacturing, through the establishment of a joint industrial engineering program (2008), and the Regenerative medicine Manufacturing Society. (2016)
- First to engineer functional experimental solid organs (penile tissue and livers) using a strategy to recycle donor organs, with potential applications to other solid organs, such as the kidney and pancreas. (2009 and 2010)
- Led the team that implanted engineered vaginas into four girls with a rare genetic defect.
 (2005 first implantation; publication 2014)
(2005 first implantation; publication 2014) - Selected to lead the second phase of the Armed Forces Institute of Regenerative Medicine (AFIRM II), a $75-million project (2013)
- Developed a 3D bioprinter (the Integrated Tissue and Organ Printing System) over a 14-year period specifically designed to print living tissue structures. (publication 2016)
- Developed a highly functional body-on-a-chip platform that integrates multiple normal human cell derived tissues with a common “blood” supply system for drug toxicity testing and personalized medicine. (2017)
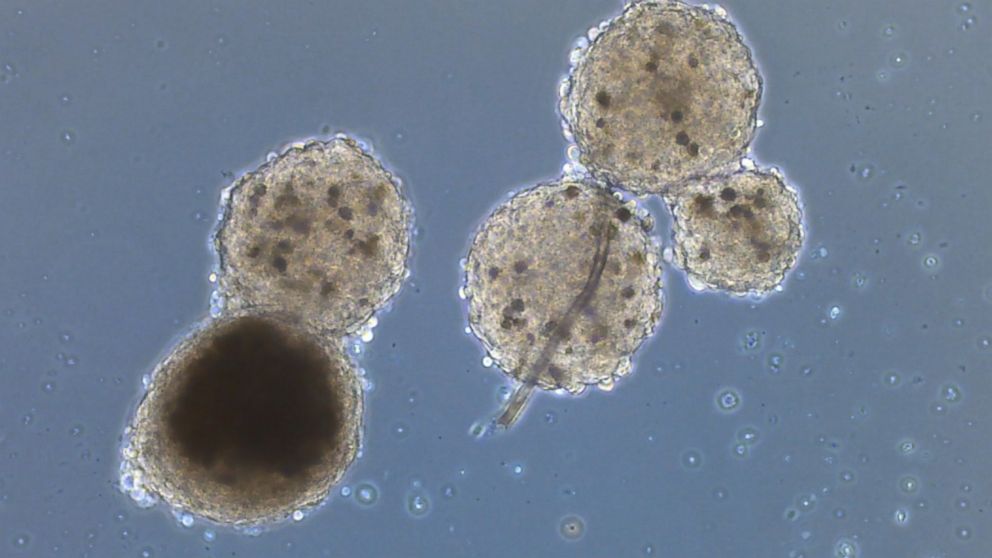
- Developed miniature 3D human brains (organoids), the first engineered tissue equivalent to naturally resemble the normal human blood brain barrier, containing all six major cell types found in organs. (publication 2018)
- Developed an engineered uterus that can sustain pregnancy and live delivery pre-clinically. (publication 2020)
- WFIRM team won 1st and 2nd place in the NASA Vascular Tissue Challenge, creating vascularized liver tissues with two different 3D bioprinting methods.
 (2021)
(2021)
3D Printed Organs Are Here
3D Printed Organs Are Here - BBC News Russian ServiceBBC News, Russian Servicebrowser
3D printed organs are here
0003
Wake Forest Institute for Regenerative Medicine learned how to print human noses, ears and skin.
They fit perfectly, because they are created from the stem cells of the patients themselves, based on samples of their tissues.
Scientists have not yet figured out how to grow more complex organs like the heart, liver or lungs. And the technologies available are still expensive enough for anyone to use.
Read also
Video, Our correspondent was 3D printed, Duration 1.06
Three-dimensional printers - until recently a novelty outlandish - are increasingly becoming part of our lives. They also found application in art.
They also found application in art.
The most popular video
9000-
Video, Anton Krasovsky: We compare the words of the journalist now and nine years ago, duration 4.50
-
video, video, video, video, video, video, video, video, video, video, video, video. Shelters: what they look like and how shelters are prepared in Russia, Germany and Finland, Duration 3.43
-
Video, Oil, gas and a can of soup: British authorities against environmental activists, Duration 3.17
9002 9002 what people in Belgorod think about the invasion of Ukraine, Duration 2. -
Video, "I can't even work remotely." Residents of Kharkiv about power outages, Duration 2.21
-
Video, how Ukraine gets rid of toponyms and characters of the total history with Russia, duration 7.15
9000 -
, will Putin press the red button? Top Nuclear Threat Questions, Duration 15.24
-
Video, New British Prime Minister. Five facts about Rishi Sunak, Duration 6.22
-
videos, which talk about the threat of a "dirty bomb" in Moscow, Kyiv and in the West, duration 3.24
-
, crime in Bucca: carnage survivor's story Duration 5.
 18
18
 07
07 3D printed mini-organs could enable safe testing of COVID-19 therapy
0006 Morgan Frey
While some technology companies are using 3D printing or additive manufacturing to address the shortage of personal protective equipment caused by the new coronavirus, others are using 3D printing technology to create samples of human organs and tissues for testing on coronavirus.
Source: Wake Forest Institute of Regenerative Medicine
As public health officials and philanthropists seek to find treatments for COVID-19, the respiratory illness caused by the novel coronavirus, researchers at universities and companies such as Novoheart Holdings Inc. are trying to speed up the development of traditional medicines and vaccines without compromised patient safety using 3D bioprinting.
Like traditional 3D printing, bioprinting uses a device to build a three-dimensional model created by a computer-aided design system. However, instead of using plastic filaments, bioprinters use cells mixed with biocompatible materials called bioinks to create 3D systems that act like human organs and tissues. These systems can then be deployed in drug developer trials or, in some cases, introduced into the human body.
However, instead of using plastic filaments, bioprinters use cells mixed with biocompatible materials called bioinks to create 3D systems that act like human organs and tissues. These systems can then be deployed in drug developer trials or, in some cases, introduced into the human body.
This process of creating human organs and tissues from existing cells is not a new concept; The Wake Forest Institute for Regenerative Medicine has been hand-crafting new organs for transplant patients for years, said Anthony Atala, director of the institute.
Mini Organs, Basic Research
But 3D printing machines have allowed Atala and his team to automate the process of regenerative medicine, and a new field of bioprinting has emerged: miniature organs.
These 3D printed organ samples are placed on microchips that are connected to a microfluidics system, says Atala, so they act like real human organs. With these organs, researchers can test drugs and treatments for toxicity in humans without testing in human or animal models.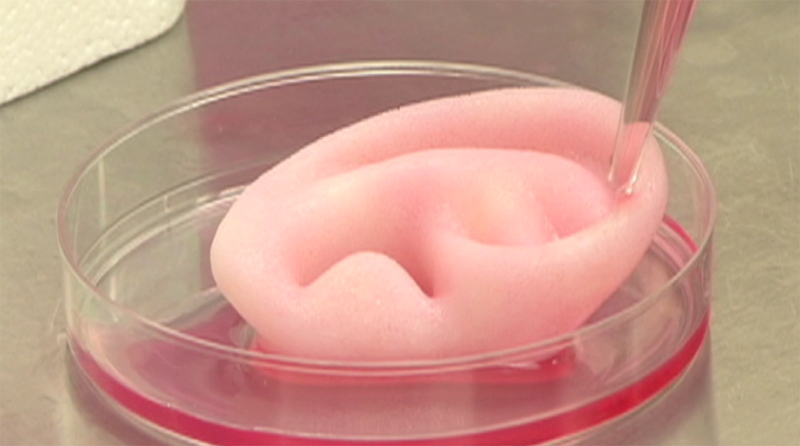
Atala said that some drugs may not show toxicity in cell cultures, animal models, and human clinical trials, but after years on the market these drugs are found to be harmful to humans.
For example, in 2000 the US Food and Drug Administration recalled the diabetes drug Rezulin after it was found to cause liver failure and 63 people died.
However, Atala said that when his team tested Rezulin on their miniature organ systems, they found liver toxicity within two weeks.
Although these miniature organs have proven to be effective in testing, Atala does not expect human clinical trials to disappear anytime soon. Organs need to be standardized and validated, and from a regulatory standpoint, human trials are still needed.
“The hope is to initially use these systems to help select the best treatments before they reach patients,” Atala said.
Banked heart
Researchers are now using these miniature organs to select the best therapy to fight COVID-19.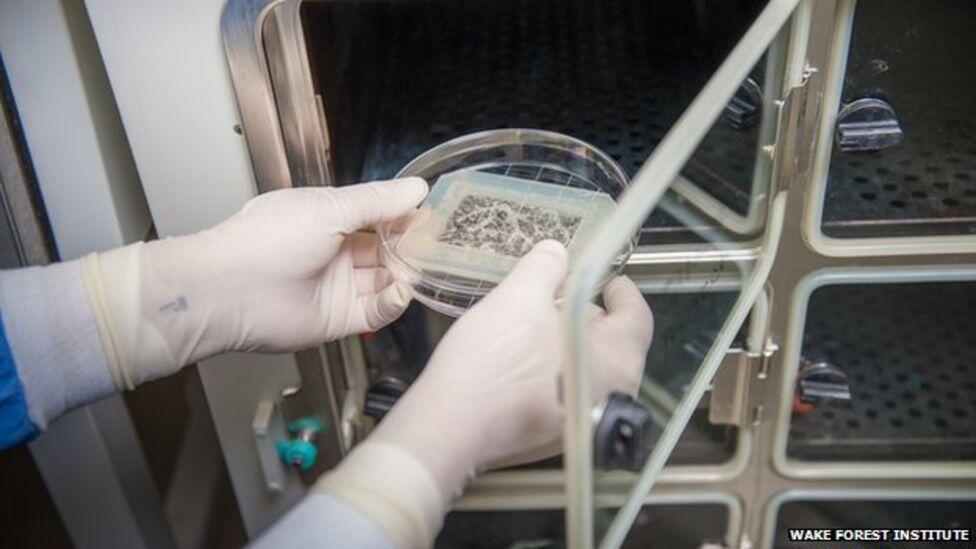
Novoheart uses 3D bioprinting to create a human heart ventricular organoid chamber, called a 3D heart in a jar.
Novoheart's 3D Heart in a Jar
Source: Novoheart
like hydroxychloroquine and azithromycin, on the heart.
This is especially important as the US FDA recently warned patients against using hydroxychloroquine for use against COVID-19often taken in combination with azithromycin due to reports of serious heart rhythm problems.
Miniature hearts allow researchers to observe the mechanisms by which these drugs cause arrhythmia in the heart without human testing, Roger Hajjar, Novoheart's chief medical officer, said in an interview with S&P Global Market Intelligence.
Another advantage is that they can also study the direct effects of the coronavirus on the heart. Hajar said researchers at Novoheart, along with researchers at the Hong Kong Infectious Diseases Laboratory, have found that the virus can cause myocarditis, or inflammation of the heart muscle, in COVID-19 patients.