Orthopedics 3d printing
Medical 3D Printing applications in orthopedics
3D Printing in healthcare is becoming a huge trend as professionals (especially surgeons) find revolutionary ways to use it in the medical field.
How can 3D printing be used in the medical field?
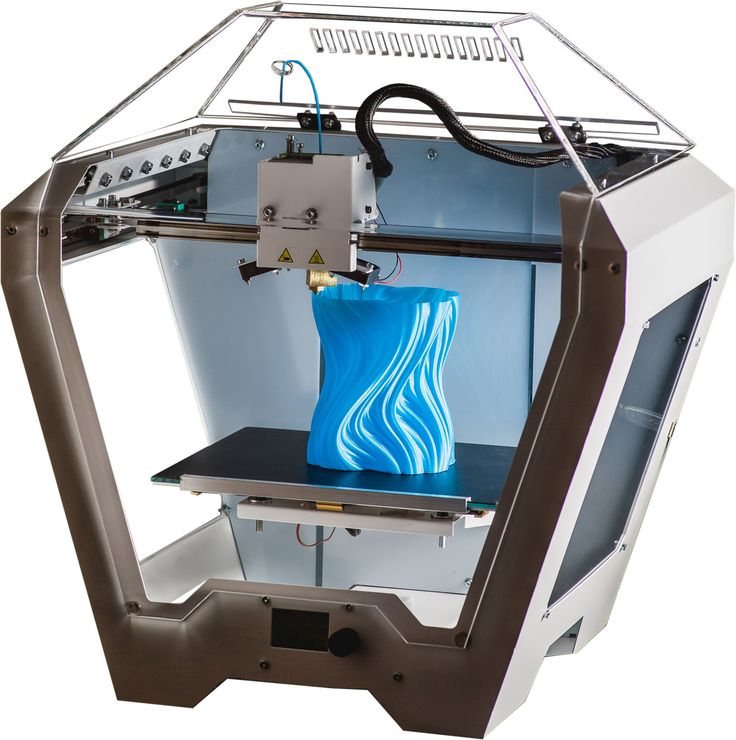
3D printing is the process of creating a dimensional solid object from a digital file – if you want to make it simple. The 3D Printer adds layer by layer, which creates a thinly sliced section of the object. Actually, 3D Printing is a common form of Additive Manufacturing.
3D printing for medical applications has a lot of potential to transform how we are treating some pathologies.
How is 3D printing used in Orthopedics?
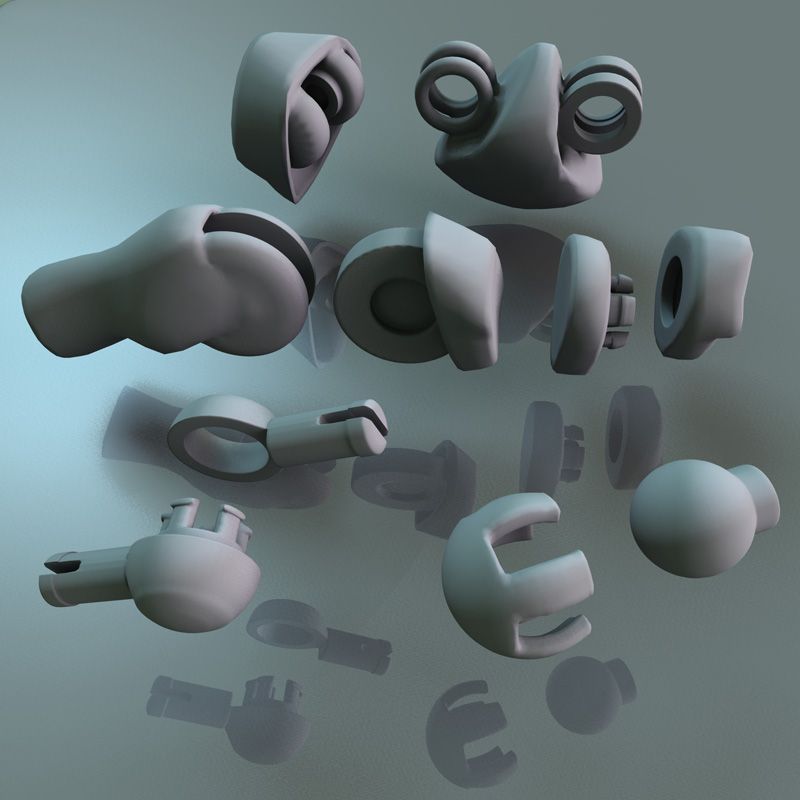
3D Printing is in the orthopedic commonly used to create personalized implants, devices, and instruments. In orthopedics, 3D Printing has also been used for preoperative planning and teaching both students and patients more about the procedures.
In this article, we will dig into how does 3D printing help the medical field and especially its applications in orthopedics. Especially the following topics:
- How to use it for preoperative planning
- Speeding production of 3D printed parts
- Bone reconstruction
- Patient-specific Instrumentation
- Robotic Surgery
- From planning to training
3D Printing in Orthopedics: how to use it for Preoperative Planning
Preoperative Planning and 3D Printing often come together. When it comes to surgical planning, it's widely used in order to manufacture 3D printed models that can be used in complex orthopedic cases.
For example, in a complex joint replacement, the surgeon can print an anatomical model replica of the joint to explore the possible obstacles and plan accordingly.
In trauma cases, the use of 3D printed replicas of bone fractures is very useful for surgeons and researchers to test methods before the surgery even begins.
The same applies to surgical guides. These guides can be used intraoperatively for taking precise bone cuts. This process decreases the surgical time and has widespread implications for the patient, the surgeon, and the hospital.
This process decreases the surgical time and has widespread implications for the patient, the surgeon, and the hospital.
The duration of the surgery, as well as its efficiency, can be improved while ensuring better outcomes for the patient. Cases like complex deformities can be dealt with more efficiently by using specific 3D printed guiding templates that fit directly onto the bone.
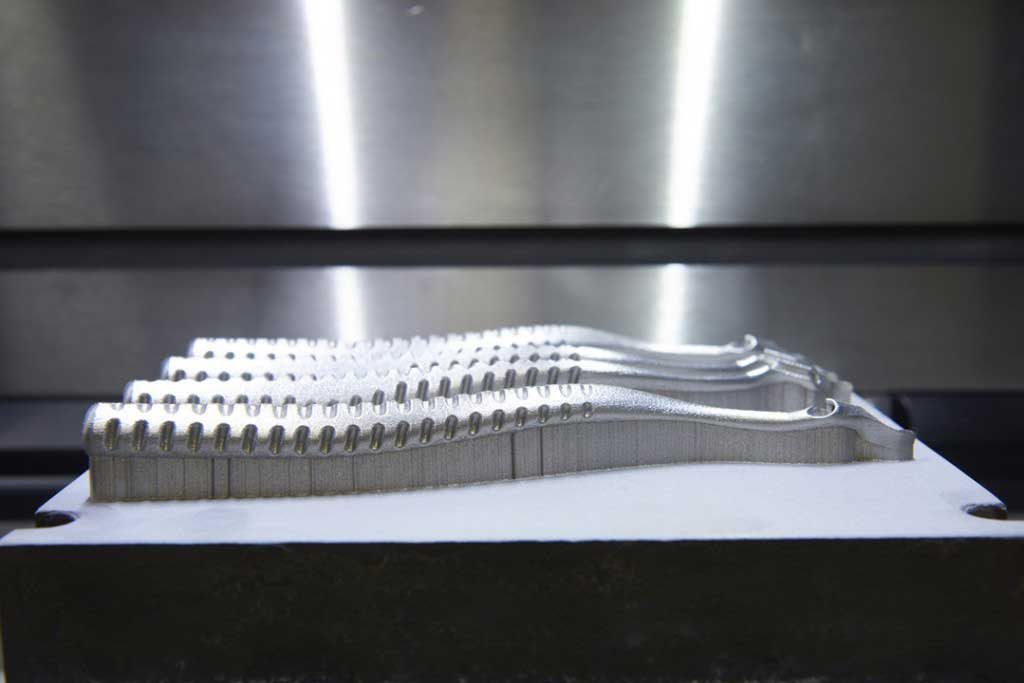
Speeding production developed 3D Printed Parts
Improvements in implant design, even small changes, take a long time using normal manufacturing.
Now, with 3D printing technology, the designer can quickly modify and develop products. This process is faster and much cheaper than the old implant designing protocols – boosting the product development process.
The designer can check the prototype for accuracy and can rapidly make necessary changes to the resultant product. Titanium has been approved to be used in these 3D printers and can help manufacture implants.
The speeding of production development opens the way to personalizations, making it is an especially growing field when it comes to 3D-printed Implants and replacement parts.
3D bone reconstructions to increase success in surgery
Bone reconstruction is another use of 3D printing in the medical field.
Using 3D printed replicas of bone fractures from patients is a perfect way of increasing successful first-time results of orthopedic trauma surgeries.
The 3D printed fracture replica lets physicians see exactly what is going on with a fracture before they even begin surgery or open up a fractured joint. In this case, the idea is to increase the success rate of the surgery on the first attempt so patients heal faster with no chronic pain.
Some broken bones can be set with a cast, others require orthopedic surgery if they don’t heal the right way, which can cause chronic pain for the patient.
Orthopedic specialists for years have been developing the technology to model and then create reconstructions of bone defects (often due to tumors or trauma). However, lead times, even up to a decade ago, were too long.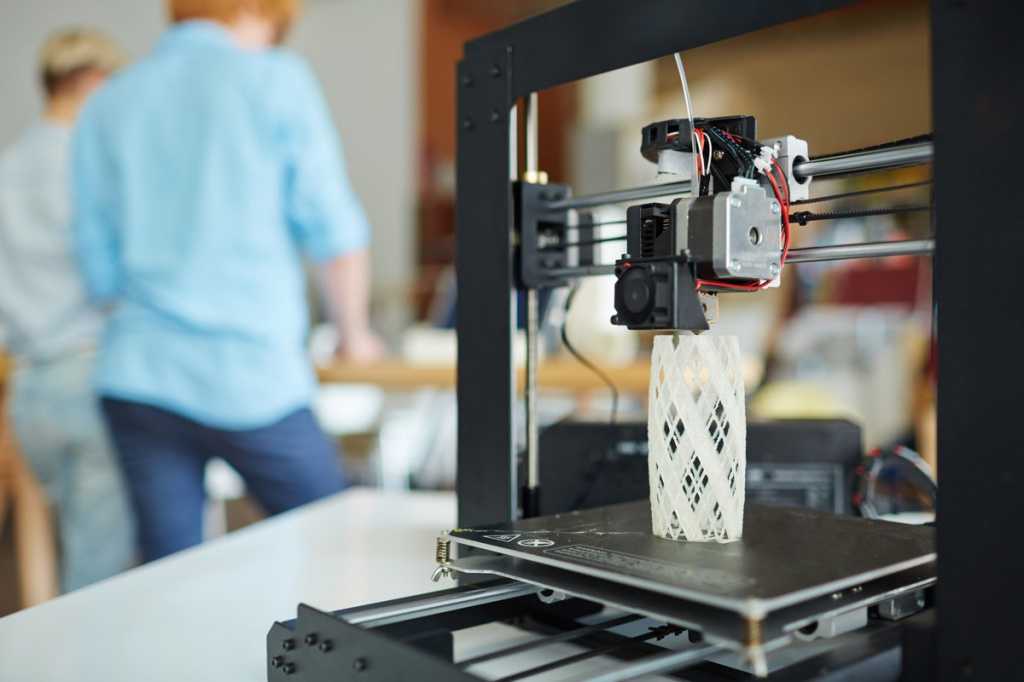
With the latest 3D printing technology, turnaround time can be as fast as six weeks-a significant leaps from the previous six-plus-month lead time. This means new surgery options, more precise bone reconstructions, along with the real possibility of a higher quality of life for patients post-op.
Patient-Specific Instrumentation and 3D Printing in orthopedic robotic surgery
3D Printing technologies are also taking an active role in Orthopedic Robotic surgery as it opens the path to design-free affordable tools. On top of that, this technology allows rapid prototyping.
As of today, surgeons use what is best described as rigid ‘one-size-fits-all’ tools for knee arthroscopy procedures, even though patients and their anatomy can vary significantly. These instruments, which are used to perform minimally invasive surgery, are rigid devices.
Now, as technology and 3D printing processes evolved, institutions have been developing patient-specific instrumentation (robotic surgical instruments) that align with patients’ anatomy.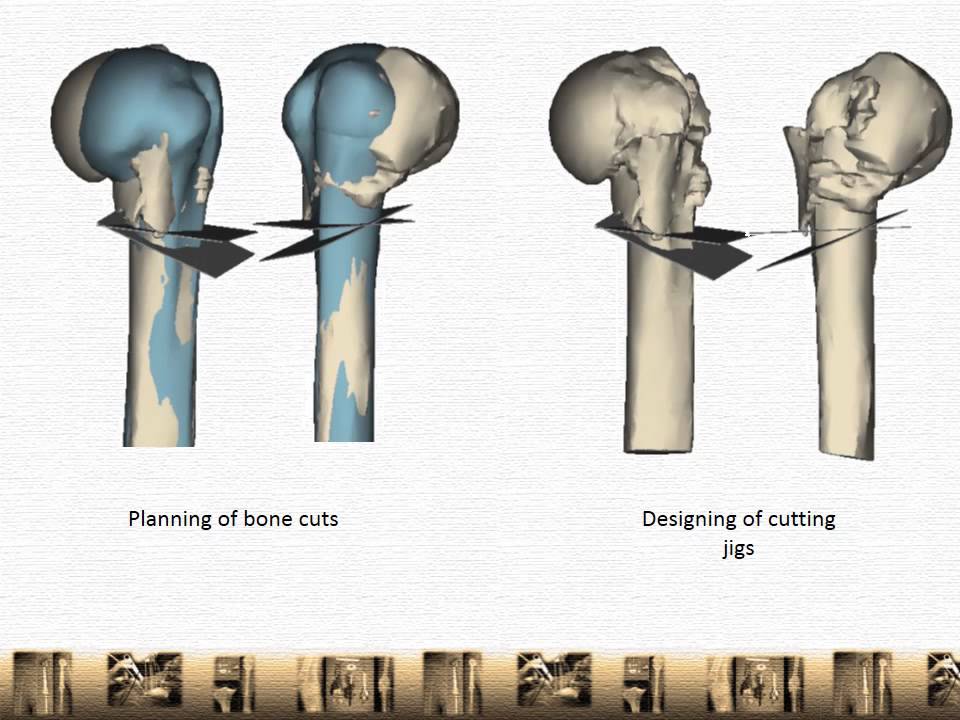
This would allow surgeons to image, for instance, a knee using an MRI machine and the resulting scan used to define where the robot can and cannot go. Targets are set and a path is defined for the robotic instrument to navigate.
This project is being developed as an evolutionary computational design algorithm that simulates how various “SnakeBots” can move through the digital 3D maze.
These generate trajectories that can be scored and the best candidates are chosen from a very large selection of these modular robots.
Once the best is selected, it can be quickly created ahead of the procedure using a 3D printer.
These tools navigate around obstacles in confined spaces such as the anatomy of the human body. Patient-specific Instrumentation (or “SnakeBots") are created specifically suited to flexibly maneuver and see inside a patient, doubling as a surgeon’s eyes and tools.
These 3D printed medical devices are similar to handy surgical tools and represent another application of artificial intelligence technology to the orthopedic.
3D Printing: from planning to training
3D printing is the perfect technology to support the ongoing evolution of personalized digital medicine.
Advantages in the medical imaging field and material development – such as surface finish and mechanical properties – will continue to transform the use of 3D printing in medicine.
And we are only scratching the surface, as we can take a huge advantage of combining this technology with the use of AI in Orthopedics.
As the clinical use of 3D printing technology continues to evolve, orthopedic surgeons should embrace it and incorporate it into their clinical practice to develop patient-specific orthopedic applications and therapeutics.
3D printing also affects future generations of doctors and not only clinical practice, as it has a huge potential to teach medical students. It can help demonstrate procedures to novice surgeons and students, testing the procedure on patient-specific anatomy and so on.
As a whole, 3D printing can have huge combinations with preoperative planning solutions like PeekMed. From rulers to angle tools and simulated cuts, every orthopedic surgeon can combine simulations of different scenarios in both 2D and 3D environments in a very easy way.
From rulers to angle tools and simulated cuts, every orthopedic surgeon can combine simulations of different scenarios in both 2D and 3D environments in a very easy way.
3D printing: clinical applications in orthopaedics and traumatology
1. Pham DL, Xu C, Prince JL. A survey of current methods in medical image segmentation. Annu Rev Biomed Eng 2000; 2:315-38. [PubMed] [Google Scholar]
2. Raut S, Raghuvanshi M, Dharaskar R, Raut A. Image segmentation - a state-of-art survey for prediction. ICACC ‘09 Proceedings of the 2009 International Conference on Advanced Computer Control, 2009; 420-4. [Google Scholar]
3. Gonzales RC, Woods RE, Eddins SL. Digital image processing using Matlab. Upper Saddle River, New Jersey: Pearson Prentice Hall, 2004. [Google Scholar]
4. Sharma N, Aggarwal LM. Automated medical image segmentation techniques. J Med Phys 2010;35:3-14. [PMC free article] [PubMed] [Google Scholar]
5. Elnakib A, Gimel’farb G, Suri J, El-Baz A.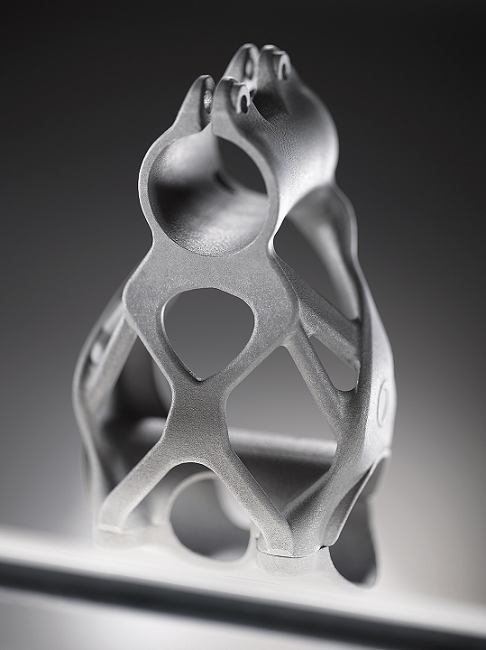 Medical image segmentation: a brief survey in multi modality state-of-the-art medical image segmentation and registration methodologies. New York: Springer, 2011. [Google Scholar]
Medical image segmentation: a brief survey in multi modality state-of-the-art medical image segmentation and registration methodologies. New York: Springer, 2011. [Google Scholar]
6. Hu YC, Grossberg MD, Mageras GS. Survey of recent volumetric medical image segmentation techniques. In: Barros de Mello CA, ed. Biomedical engineering. Vienna: Intech, 2009:321-46. [Google Scholar]
7. No authors listed. Itk-SNAP. http://www.itksnap.org (date last accessed 11 February 2016).
8. No authors listed. NiftySeg. http://cmictig.cs.ucl.ac.uk/wiki/index.php/NiftySeg (date last accessed 11 February 2016).
9. No authors listed. SPM: by members & collaborators of the Wellcome Trust Centre for Neuroimaging. http://www.fil.ion.ucl.ac.uk/spm/software/ (date last accessed 11 February 2016).
10. No authors listed. 3D slicer: a multi-platform, free and open source software package for visualization and medical image computing. http://www.slicer.org (date last accessed 11 February 2016).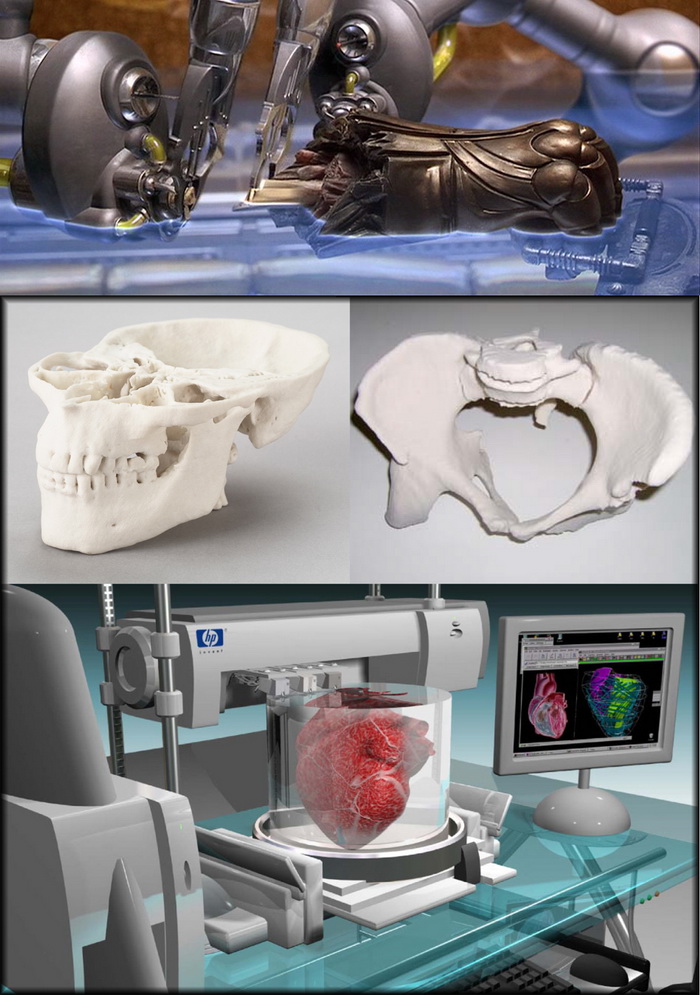
11. Wollny G, Kellman P, Ledesma-Carbayo MJ, et al. MIA - a free and open source software for gray scale medical image analysis. Source Code for Biology and Medicine, 2013;8-20:1-20. [PMC free article] [PubMed] [Google Scholar]
12. Yushkevich PA, Piven J, Cody Hazlett H, et al. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 2006; 31:1116-28. [PubMed] [Google Scholar]
13. Gibson I, Rosen D, Stucker B. Additive manufacturing technologies: 3D printing, rapid prototyping, and direct digital manufacturing. Second ed. New York: Springer, 2010. [Google Scholar]
14. Scott J, Gupta N, Weber C, et al. Additive manufacturing: status and opportunities. Washington, DC: Science and Technology Policy Institute, 2012. https://cgsr.llnl.gov/content/assets/docs/IDA_AdditiveM3D_33012_Final.pdf (date last accessed 11 February 2016). [Google Scholar]
15. No authors listed. Committee F42 on additive manufacturing technologies. http://www.astm.org/COMMITTEE/F42.htm (date last accessed 11 February 2016).
http://www.astm.org/COMMITTEE/F42.htm (date last accessed 11 February 2016).
16. No authors listed. 3D printing healthcare. http://www.osteo3d.com (date last accessed 11 February 2016).
17. No authors listed. Medical modeling. http://www.medicalmodeling.com (date last accessed 11 February 2016).
18. Sanghera B, Naique S, Papaharilaou Y, Amis A. Preliminary study of rapid prototype medical models. Rapid Prototyping Journal 2001;7:275-84. [Google Scholar]
19. Potamianos P, Amiss AA, Forestes AJ, McGurk M, Bircher M. Rapid prototyping for orthopaedic surgery. Proc Inst Mech Eng H 1998;212:383-93. [PubMed] [Google Scholar]
20. Frame M, Huntley JS. Rapid prototyping in orthopaedic surgery: a user’s guide. ScientificWorldJournal 2012:838575. PMID:22666160. [PMC free article] [PubMed] [Google Scholar]
21. Mahaisavariya B, Sitthiseripratip K, Oris P, Tongdee T. Rapid prototyping model for surgical planning of corrective osteotomy for cubitus varus: report of two cases. Inj Extra 2006; 37:176-80. [Google Scholar]
Inj Extra 2006; 37:176-80. [Google Scholar]
22. Sheth U, Theodoropoulos J, Abouali J. Use of 3-dimensional printing for preoperative planning in the treatment of recurrent anterior shoulder instability. Arthrosc Tech 2015;4:e311-e316. PMID:26759768. [PMC free article] [PubMed] [Google Scholar]
23. Wu ZX, Huang LY, Sang HX, et al. Accuracy and safety assessment of pedicle screw placement using the rapid prototyping technique in severe congenital scoliosis. J Spinal Disord Tech 2011;24:444-50. [PubMed] [Google Scholar]
24. Sugawara T, Higashiyama N, Watanabe N, Uchida F, Kamishina H, Inoue N. 3D computer technology for future spinal surgery J-STAGE 2015;24:318-26. [Google Scholar]
25. Ogden K, Ordway N, Diallo D, Tillapaugh-Fay G, Aslan C. Dimensional accuracy of 3D printed vertebra progress in biomedical optics and imaging. Proceedings of SPIE 2014; 9036:903629. [Google Scholar]
26. King R. (2008, October 6). Printing in 3-D gets practical. BusinessWeek Online. http://www.businessweek.com/technology/content/oct2008/tc2008103_077223.htm (date last accessed 21 September 2015).
http://www.businessweek.com/technology/content/oct2008/tc2008103_077223.htm (date last accessed 21 September 2015).
27. Berman B. 3-D printing: The new industrial revolution. Bus Horiz 2012;55:155-62. [Google Scholar]
28. D’Urso PS, Redmonda MJ. A method for the resection of cranial tumours and skull reconstruction. Br J Neurosurg 2000;14-16. [PubMed] [Google Scholar]
29. Tam MD, Laycock SD, Bell D, Chojnowski A. 3-D printout of a DICOM file to aid surgical planning in a 6 year old patient with a large scapular osteochondroma complicating congenital diaphyseal aclasia. J Radiol Case Rep 2012;6:31-7. PMID:22690278. [PMC free article] [PubMed] [Google Scholar]
30. No authors listed. LayerWise. http://www.layerwise.com (date last accessed 11 February 2016).
31. No authors listed. Lima corporate orthopaedic motion. http://www.lima.it/homepage.html (date last accessed 11 February 2016).
32. Zhanga Y, Zhuc J, Wanga Z, Zhoua Y, Zhanga X. Constructing a 3D-printable, bioceramic sheathed articular spacer assembly for infected hip arthroplasty.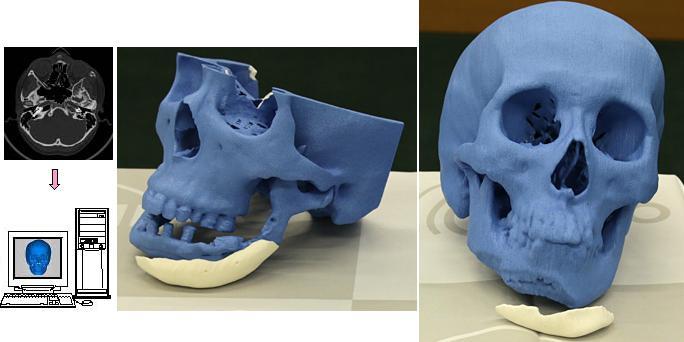 Journal of Medical Hypotheses and Ideas 2015;9:13-9. [Google Scholar]
Journal of Medical Hypotheses and Ideas 2015;9:13-9. [Google Scholar]
33. Imanishi J, Choong PF. Three-dimensional printed calcaneal prosthesis following total calcanectomy. Int J Surg Case Rep 2015;10:83-7. [PMC free article] [PubMed] [Google Scholar]
34. Singare S, Yaxiong L, Dichen L, et al. Fabrication of customised maxillo-facial prosthesis using computer-aided design and rapid prototyping techniques. Rapid Prototyping J 2006;12:206-13. [Google Scholar]
35. Singare S, Dichen L, Bingheng L, Yanpu L, Zhenyu G, Yaxiong L. Design and fabrication of custom mandible titanium tray based on rapid prototyping. Med Eng Phys 2004;26:671-6. [PubMed] [Google Scholar]
36. Stoora P, Suomalainenb A, Lindqvista C, et al. Rapid prototyped patient specific implants for reconstruction of orbital wall defects. Journal of Cranio-Maxillofacial Surgery 2012;42:1644-9. [PubMed] [Google Scholar]
37. El Halabi F, Rodriguez JF, Rebolledo L, Hurtós E, Doblaré M. Mechanical characterization and numerical simulation of polyether–ether–ketone (PEEK) cranial implants. J Mech Behav Biomed Mater 2011;4:1819-32. PMID:22098881. [PubMed] [Google Scholar]
J Mech Behav Biomed Mater 2011;4:1819-32. PMID:22098881. [PubMed] [Google Scholar]
38. Mazzarese B, Nicotera N, Theriault H. Modeling bone fixation implants with absorbable polymers using 3-D printing Biomedical Engineering Conference (NEBEC), 2015 41st Annual Northeast 2015; 7117129. [Google Scholar]
39. Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 2010;5:335-41. PMID:20467825. [PubMed] [Google Scholar]
40. Stevens B, Yang Y, Mohandas A, Stucker B, Nguyen KT. A review of materials, fabrication methods, and strategies used to enhance bone regeneration in engineered bone tissues. J Biomed Mater Res B Appl Biomater 2008;85:573-82. PMID:17937408. [PubMed] [Google Scholar]
41. No authors listed. 3D printed spine implant. https://www.rmit.edu.au/news/all-news/2015/august/australias-first-3d-printed-spine-implant/ (date last accessed 10 April 2016).
42. Pati F, Song TH, Rijal G, Jang J, Kim SW, Cho DW. Ornamenting 3D printed scaffolds with cell-laid extracellular matrix for bone tissue regeneration. Biomaterials 2015;37:230-41. PMID:25453953. [PubMed] [Google Scholar]
Pati F, Song TH, Rijal G, Jang J, Kim SW, Cho DW. Ornamenting 3D printed scaffolds with cell-laid extracellular matrix for bone tissue regeneration. Biomaterials 2015;37:230-41. PMID:25453953. [PubMed] [Google Scholar]
43. Arafat MT, Lam CX, Ekaputra AK, Wong SY, Li X, Gibson I. Biomimetic composite coating on rapid prototyped scaffolds for bone tissue engineering. Acta Biomater 2011;7:809-20. PMID:20849985. [PubMed] [Google Scholar]
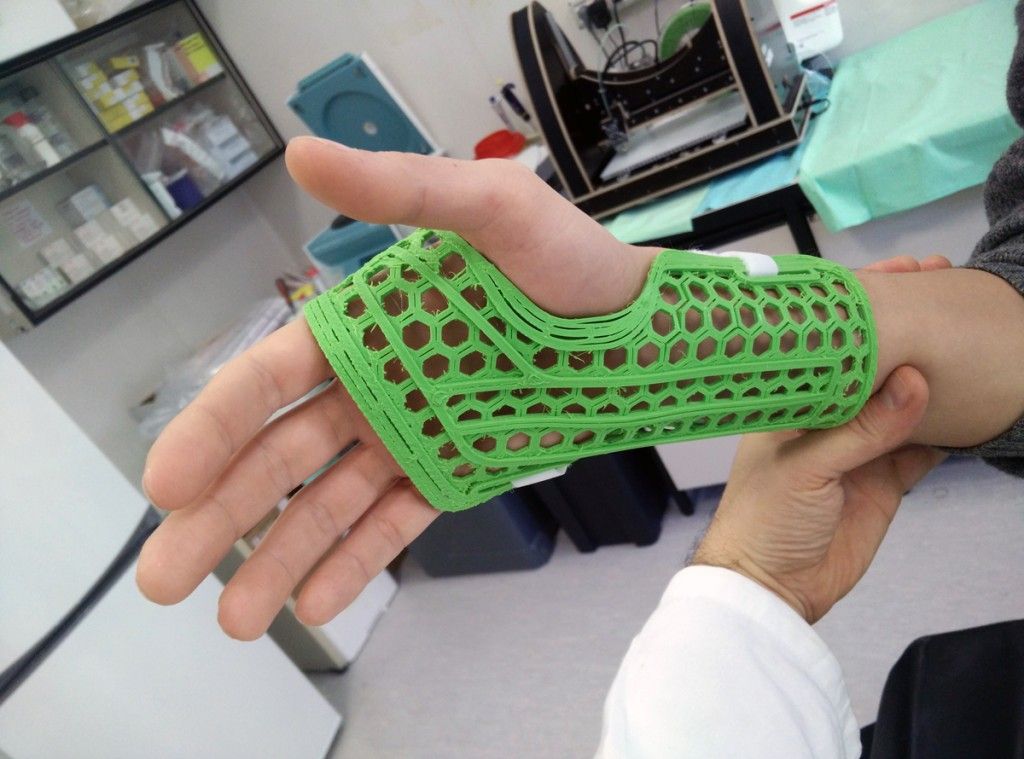
44. Mavroidis C, Ranky RG, Sivak ML, et al. Patient specific ankle-foot orthoses using rapid prototyping. J Neuroeng Rehabil 2011;12;8:1 8-12. [PMC free article] [PubMed] [Google Scholar]
45. No authors listed. Cortex: exoskeleton protecting the internal skeleton. http://www.evilldesign.com/cortex (date last accessed 11 February 2016).
46. Zhang YZ, Lu S, Chen B, Zhao JM, Liu R, Pei GX. Application of computer-aided design osteotomy template for treatment of cubitus varus deformity in teenagers: a pilot study. J Shoulder Elbow Surg 2011;20:51-6. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
47. Cartiaux O, Paul L, Francq BG, Banse X, Docquier PL. Improved accuracy with 3D planning and patient-specific instruments during simulated pelvic bone tumor surgery. Ann Biomed Eng 2014;42:205-13. PMID:23963884. [PubMed] [Google Scholar]
48. Landi A, Mancarella C, Gregori F, Delfini R. Spinal neuronavigation and 3D-printed tubular guide for pedicle screw placement: a really new tool to improve safety and accuracy of the surgical technique? J Spine 2015;4: e118. doi: 10.4172/21657939.1000e118. [CrossRef] [Google Scholar]
49. Brown GA, Firoozbakhsh K, DeCoster TA, Reyna JR., Moneim M. Rapid prototyping: the future of trauma surgery? J Bone Joint Surg Am 2003;85-A(suppl 4):49-55. PMID:14652393. [PubMed] [Google Scholar]
50. Pietrabissa A, Marconi S, Peri A, et al. From CT scanning to 3-D printing technology for the preoperative planning in laparoscopic splenectomy. Surg Endosc 2016;30:366-71.doi: 10.1007/s00464-015-4185-y Epub 2015.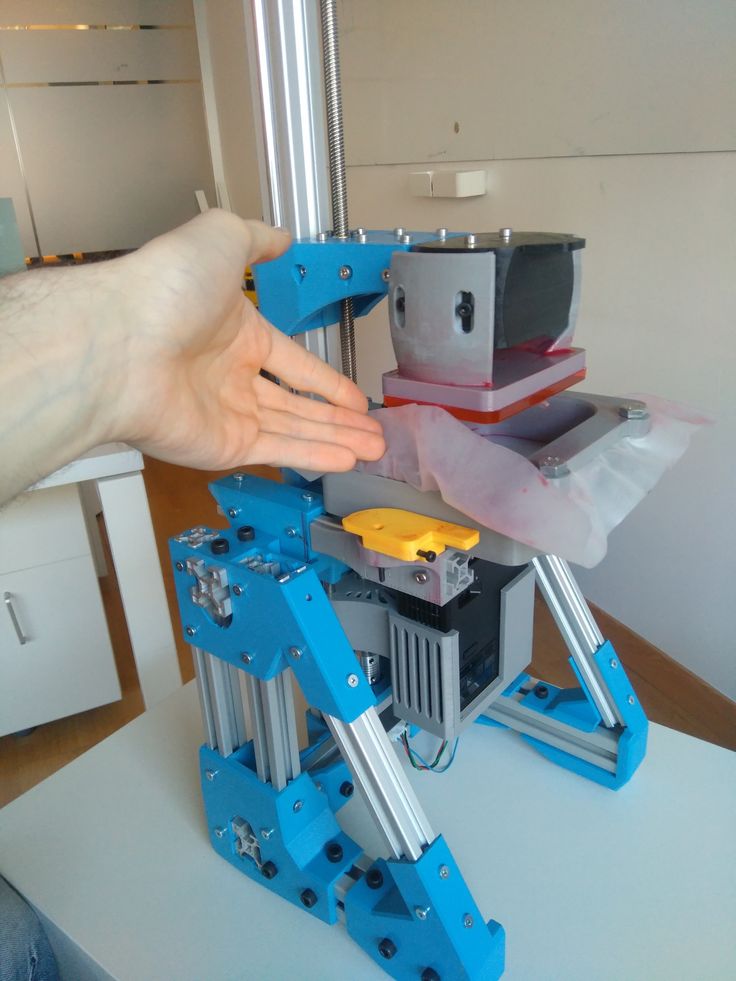 July 3. [PubMed] [CrossRef] [Google Scholar]
July 3. [PubMed] [CrossRef] [Google Scholar]
51. Frisoli A, Solazzi M, Reiner M, Bergamasco M. The contribution of cutaneous and kinesthetic sensory modalities in haptic perception of orientation. Brain Res Bull 2011;85:260-6. [PubMed] [Google Scholar]
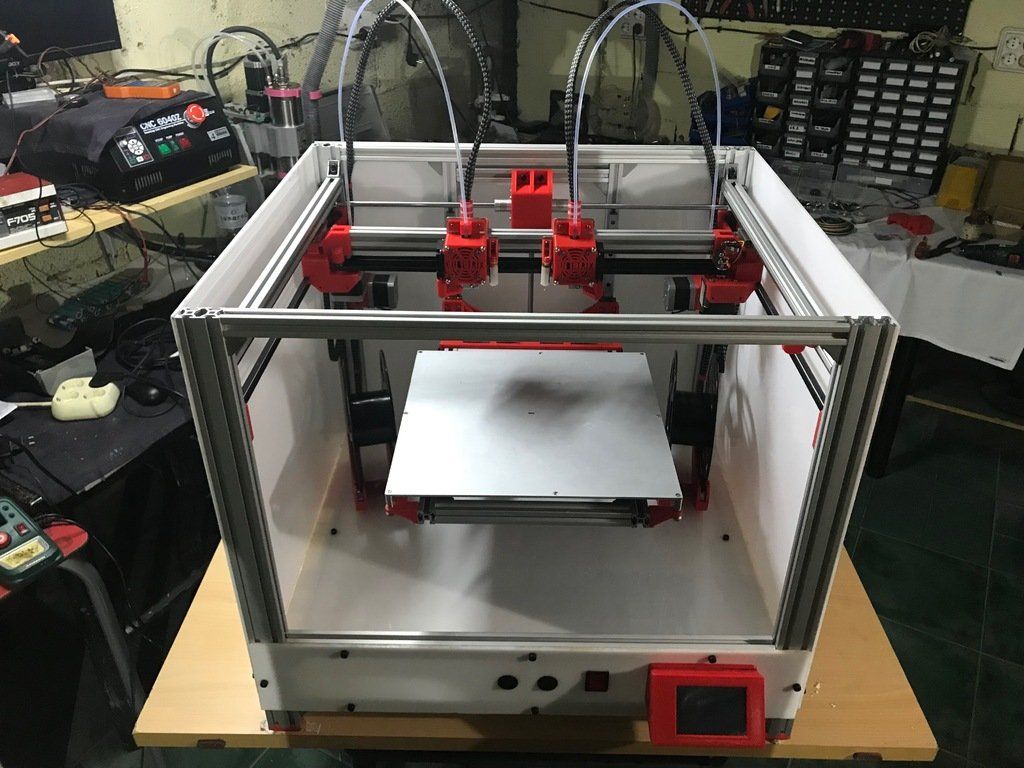
Process of making orthopedic insoles using the Raise3D printer
3D printing is a versatile form of additive manufacturing that is gaining popularity in a variety of fields. Currently, it is increasingly being used in plastic surgery and in the creation of orthopedic medical products and equipment. 3D printing has come to be used to improve medical devices due to the production stability and time efficiency it provides. An example of such an application can be seen in the collaboration between the Italian company CREA3D and the orthopedist Dr. Valenti. They are successfully combining 3D printing with other digital technologies to produce customized insoles and other custom-designed orthotics, thus enhancing the effectiveness of assistive care.
Dr. Mirko Valenti used 3D printing technology to treat clinical cases of tibialis posterior tenosynovitis with conservative corrective therapy. The introduction of technology into the treatment process was both innovative and highly effective. Valenti purchased a Raise3D E2 3D printer equipped with IDEX technology (independent dual extruder) for his office. The Raise3D E2 is ideal for printing a pair of orthopedic insoles at the same time.
Individual orthopedic insoles
Traditional manufacturing of insoles before 3D printing
Each pair of orthopedic insoles is individual for a particular patient, because everyone has their own needs. The strength properties of the various parts of the insoles must be adjusted according to individual characteristics.
This proved to be a problem for the traditional manufacturing process. The traditional process requires using a CNC machine to mill a piece of material into the desired shape.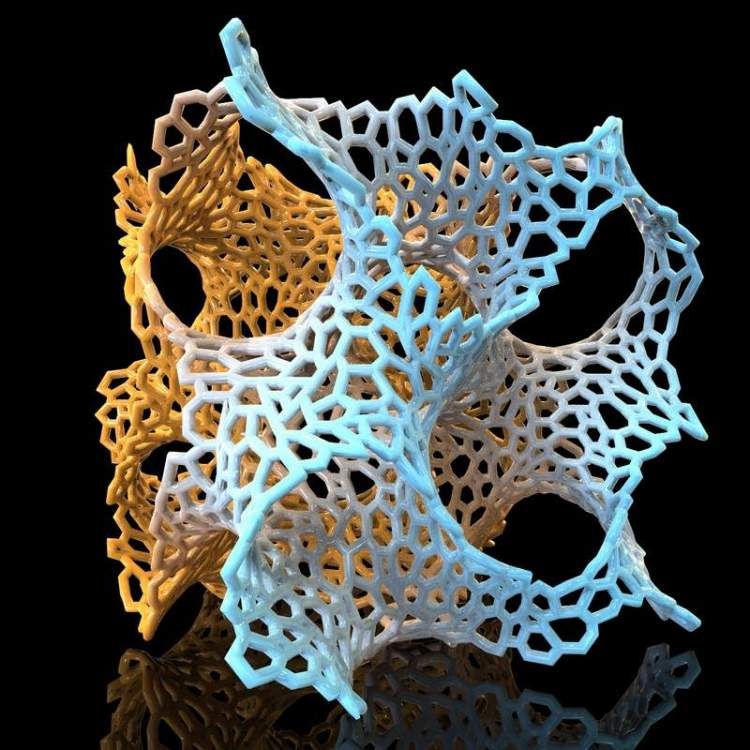 To ensure the accuracy of the anatomical region in the insole, a high-precision CNC machine and high labor costs are required. This is a laborious and complex process. The production process creates a lot of garbage and dust, pollutes the working environment, endangers the health of workers.
To ensure the accuracy of the anatomical region in the insole, a high-precision CNC machine and high labor costs are required. This is a laborious and complex process. The production process creates a lot of garbage and dust, pollutes the working environment, endangers the health of workers.
Manufacture of insoles after the advent of 3D printing
Abandoning traditional CAD-CAM machines, Dr. Mirko Valenti began to print orthopedic insoles with PP plastic thread. Due to the durability and strength of the material, excellent support for the patient's foot is provided. Printing a pair of orthopedic insoles with PP thread is a simple process.
First, the doctor scans the patient's leg. He then uses a CAD program to make a model of an orthopedic insole with compensating supports for the affected areas, thereby ensuring that the arch of the foot is supported and the heel is stable. Valenti then loads the model file into ideaMaker 3D print preparation software to optimize technical properties such as shape change and infill percentage of the model.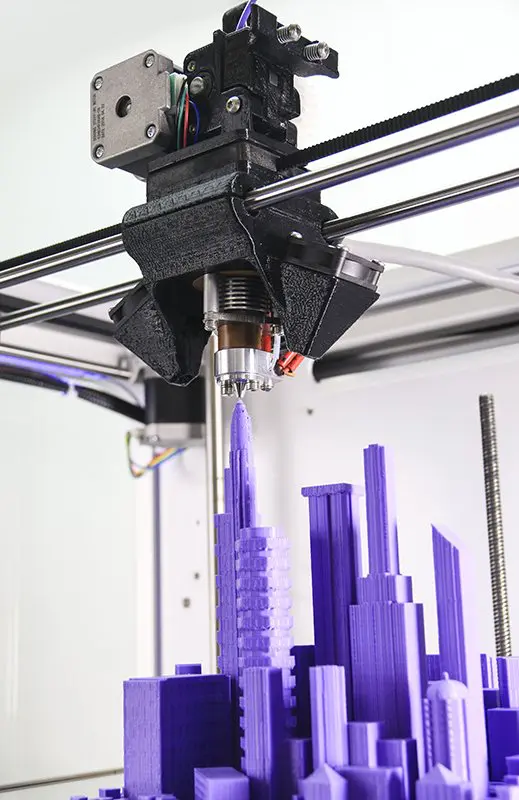 For example, honeycomb infill can make the structure rigid. The filling allows different results in terms of deformability and softness of the orthosis. Then the doctor uploads the model file to the E2 3D printer, which prints out a pair of insoles at the same time. Finally, Dr. Valenti wraps the sole with EVA or other special materials suitable for skin contact.
For example, honeycomb infill can make the structure rigid. The filling allows different results in terms of deformability and softness of the orthosis. Then the doctor uploads the model file to the E2 3D printer, which prints out a pair of insoles at the same time. Finally, Dr. Valenti wraps the sole with EVA or other special materials suitable for skin contact.
The entire manufacturing process, including scanning, design and production, takes less than 24 hours.
Benefits of 3D oven orthopedic insoles;
3D printing simplifies the traditional process and shortens the production cycle, as well as the time it takes for the customer to receive the product. A 3D printed model can be produced in a single process without the use of any other additional machines and tools. Printing a pair of orthopedic insoles on the Raise3D E2 printer takes only 2-3 hours, and the whole process is done automatically without the need for manual control. Making insoles without 3D printing requires a lot of hand tools, a lot of time to get an accurate model according to the anatomical features.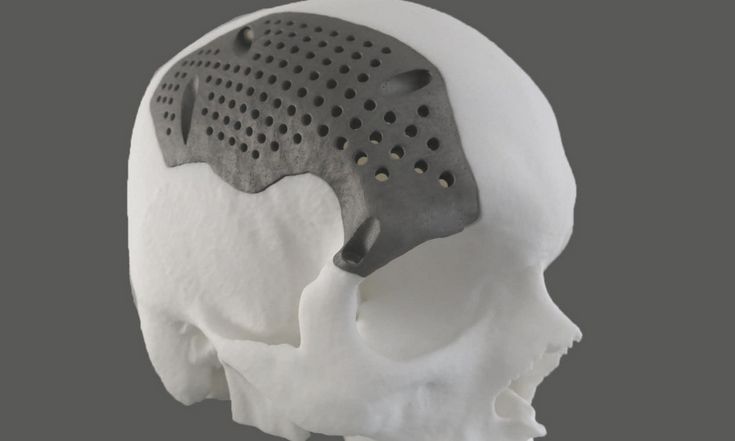 3D printing makes it possible to successfully carry out individual orthopedic treatment.
3D printing makes it possible to successfully carry out individual orthopedic treatment.
3D printing is an efficient manufacturing process
3D printing is a more efficient process for producing insoles. Users can design models and mass-produce them at the same time. With 3D printing, there is no need for multiple design, verification, and modification processes. 3D printing makes it possible to produce small batches on demand. The model is available immediately.
Enclosed 3D printers provide a greener working environment
Enclosed 3D printers like the Raise3D filter out any fumes that are released when the material is heated during 3D printing. This reduces the need for large workshops or separate production rooms. As a result, 3D printing provides a cleaner and healthier environment. You can perform mass production right in the office.
Correct software for 3D printing
Dr. Valenti chose polypropylene as the material for the 3D printing to provide support and flexibility for various insoles. Each kind of polymer needs different settings. The right software can greatly simplify the job of customizing settings.
Each kind of polymer needs different settings. The right software can greatly simplify the job of customizing settings.
For example, ideaMaker is a file-to-print software that has many built-in preset templates for various polymers (including polypropylene).
The main advantage is that users can adjust internal structure parameters such as infill density, infill angle, and others to control strength properties.
Adjust the model properties in ideaMaker to prepare the model for printing.
Raise3D provides a complete process for the production of orthopedic insoles
Dr. Valenti chose the Raise3D E2 desktop 3D printer for the production of orthopedic insoles. As a medium-sized professional desktop printer, the E2 meets all print quality requirements. At the same time, E2 is suitable for home and small studios. IDEX E2 technology allows users to print a pair of orthopedic insoles at once, maximizing production efficiency. In addition, during the manufacturing process, Dr. Valenti uses ideaMaker 3D printing file preparation software to reinforce the internal structure of the insole. ideaMaker has parameter settings and various templates, allows you to customize and change the technical properties of the insole. The E2 desktop 3D printer supports a variety of plastics, including polypropylene. Users can learn about polymer characteristics and download related files.
In addition, during the manufacturing process, Dr. Valenti uses ideaMaker 3D printing file preparation software to reinforce the internal structure of the insole. ideaMaker has parameter settings and various templates, allows you to customize and change the technical properties of the insole. The E2 desktop 3D printer supports a variety of plastics, including polypropylene. Users can learn about polymer characteristics and download related files.
3D printing will benefit more medical fields
3D printing provides better customization, precision, aesthetic appearance and light structure. It also significantly reduces the production process and lead times and manufacturing. Dr. Mirko Valenti used 3D printing in the manufacture of plantar orthoses. He used Raise3D printers and software for a full production cycle and achieved high efficiency thanks to the Raise3D ecosystem.
The material is provided by the Italian distributor of Raise3D - Crea3D.
3D printed orthotics
05/20/2020
3D printing in orthopedics has been used quite recently. And although the share of its application in this industry is still very small and cannot be compared, for example, with dentistry, the development has already begun and there is no point in denying the effectiveness of a 3D printer in the manufacture of orthopedic products.
Orthopedic products are a fairly broad concept, they can be temporary or permanent wear products used to support, stabilize and rehabilitate injured limbs, such as orthoses, splints, corsets, insoles, etc.
For maximum effectiveness, orthopedic devices are most often made to measure. Traditional production methods are quite labor intensive and require fitting, fitting, which consumes a lot of time and materials.
Due to their affordability and ease of use, 3D scanning and 3D printing have greatly simplified the entire process of manufacturing custom orthotics.
Insoles
Orthopedic insoles are used for non-surgical correction of foot and ankle problems, as well as to improve the athletic performance of professional athletes. The grueling taking of impressions and the lengthy production time are a thing of the past decade.
Now, to make an orthopedic insole, you only need an orthopedic 3D scanner, a 3D printer, and 6-10 hours to get the finished product.
Orthoses
Those who have ever broken an arm, leg or finger know what kind of agony a plaster orthosis delivers. A custom 3D printed plastic orthosis easily replaces a cast for mild to moderate injuries. At the same time, it breathes completely, does not irritate the skin and does not interfere with hygiene procedures.
Corsets
An orthopedic corset is a more complex product, and requires the most accurate fit to the patient's figure.