3D printer bladder
Bladder grown from 3D bioprinted tissue continues to function after 14 years
0Shares
After more than a decade, a 3D bioprinted bladder, created by Dr. Anthony Atala at Boston Children’s Hospital, is sustaining the live of a patient. The 3D bioprinted organ was made to replace patient Luke Massella’s defective bladder in 2004. Since then, Massella has not required any further surgery.
Recalling the transplant to BBC News, Massella stated “It was pretty much like getting a bladder transplant, but from my own cells, so you don’t have to deal with rejection. […] I was able to live a normal life after”
Luke Massella, aged 10 in 2001 with his mother and uncle after numerous surgeries. Photo via BBC News.3D printing a new bladder
Massella was born with spina bifida, which left a gap in his spine, and led him to undergo several surgeries at a young age. Unfortunately, a defective bladder caused his kidneys to fail, leaving him the possibility of being on dialysis for the remainder of his life. Thankfully, Dr. Atala came up with an alternative solution.
The bladder was made using a sample of Massella’ bladder tissue, and modified inkjet printer, presumably used to build a sort of scaffold/host for the cells. Incubated in lab condition, the new bladder was grown in 2 months, and then successfully transplanted into the patient.
Massella is 1 of 10 people with a bioprinted bladder grown from his own cells. According to Dr. Atala, flat structures like skin are easiest to print, whereas tubular structures like blood vessels and hollow non-tubular organs like bladders are more complex. Solid organs like hearts, lungs, and kidneys, are the most difficult to bioprint as they have more cells per centimetre, though some researchers have had small successes in this field.
Investing in bioprinted organs
The potential of 3D bioprinted organs has led further research by many organizations around the world. Recently, a team at Indiana University School of Medicine (IUSM) were awarded $9 million to further their 3D bioprinting research for the development of transplantable organs.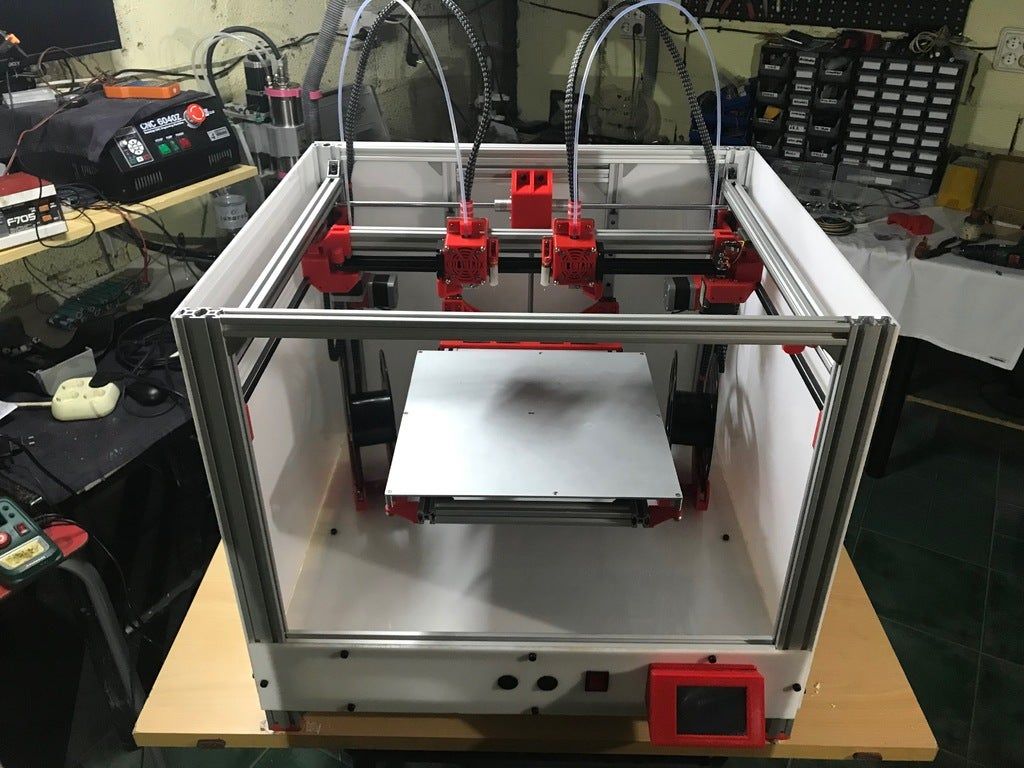 Leading 3D printer manufacturer 3D Systems has entered into a partnership with United Therapeutics Corporation for the purpose of 3D printing lung tissue, and BIOLIFE4D researchers at Brigham and Women’s Hospital (BWH) have successfully 3D bioprinted tubular structures which imitate the human body’s vessels.
Leading 3D printer manufacturer 3D Systems has entered into a partnership with United Therapeutics Corporation for the purpose of 3D printing lung tissue, and BIOLIFE4D researchers at Brigham and Women’s Hospital (BWH) have successfully 3D bioprinted tubular structures which imitate the human body’s vessels.
For more 3D bioprinting partnership updates subscribe to the 3D Printing Industry newsletter, following us on Facebook and liking us on Twitter.
Seeking new professional opportunities? Search and post 3D Printing Jobs now.
Featured image shows Boston Children’s Hospital. Photo via Boston Business Journal.
Tags 3D Bioprinting 3d printed organs Anthony Atala Boston Children’s Hospital surgery
Brian Lord
Brian Lord was a journalist for 3D Printing Industry. Originally hailing from Miami, he moved to the UK where he graduated from the University of Stirling with a Bachelor's degree in History & Media. In the past he has conducted and transcribed interviews for his own personal blog.
Originally hailing from Miami, he moved to the UK where he graduated from the University of Stirling with a Bachelor's degree in History & Media. In the past he has conducted and transcribed interviews for his own personal blog.
CloudTweaks | The History Of 3D Printing
3D printing, also called additive manufacturing, has been one of the breakout technologies of the last 18 months. People are now clamouring to get involved with the technology, with printable objects ranging from hand-guns to medical equipment. Yet, despite its recent popular emergence and contrary to popular belief, 3D printing has been existence for more than 35 years, with the inception of the concept traced back to 1976 and the first example of it coming in the early 1980s.
(Tedtalk – What is next for 3d printing?)
The first published account of a printed solid model was made by Hideo Kodama from the Nagoya Municipal Industrial Research Institute in either 1981 or 1982 (accounts vary).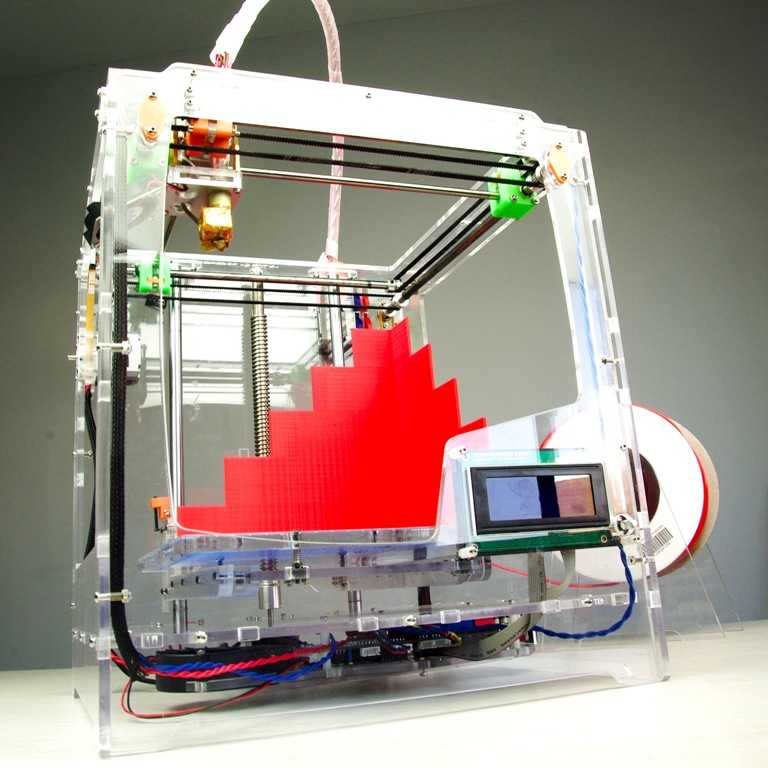 His paper theorised about the potential behind a rapid prototyping system that used photopolymers to build a solid, ‘printed’ object that was built up in layers, each of which would correspond to a cross-sectional slice in a model.
His paper theorised about the potential behind a rapid prototyping system that used photopolymers to build a solid, ‘printed’ object that was built up in layers, each of which would correspond to a cross-sectional slice in a model.
Charles Hull, who at the time worked for 3D Systems Corporation, invented stereolithography – a process which lets designers create 3D models using digital data which can then be used to create a tangible object. Hull went on to publish a number of patents on the concept of 3D printing, many of which are used in today’s processes.
3D Systems Corporation built the first stereolithographic apparatus (SLA) machine. It used a UV laser to solidify photopolymers, thus making 3D objects layer-by-layer. Although the machince faced difficulties, it was the first time it was proved that complex objects could be ‘printed’ overnight.
The stroke of the new millennium saw a world first as the first 3D printed organ was transplanted into a human. Created by scientists at Wake Forest Institute for Regenerative Medicine, a human bladder was printed, covered in the recipient’s own cells, and then implanted. It was a scientific breakthrough; because the device used the patient’s own cells, there was no chance the implant would be rejected.
It was a scientific breakthrough; because the device used the patient’s own cells, there was no chance the implant would be rejected.
3D printing collided with the open source movement for the first time in the middle of the decade. The idea was championed by Dr Adrian Bowyer at the University of Bath in England. His idea was to create a printer than could print itself – thus making units and parts cheaper, more accessible, and easier to distribute.
After the success of the bladder in 1999, then of the first printed kidney in 2002, 2008 was the year that saw the first 3D printed prosthetic limb. It incorporated all parts of a biological limb, was printed ‘as is’, without the need for any latter assembly.
The world’s first 3D printed car was launched by Kor Ecologic at the TEDxWinnipeg conference. Designed to be ‘green’, the prototype could reportedly do 200 mpg and would retail for between $10,000 and $50,000, depending on the model.
The costs of 3D printers are falling phenomenally. While they cost around $20,000 just three years ago, there are now machines being developed that will be sold for under $500, thus making the technology increasingly available to the average consumer and laying the foundations for a potential explosion in the home inventor and home DIY markets. It’s not hard to imagine a future where a trip to the dentist will see him print you a new tooth, if you have a crash in your car you can just print a new chassis, or all furniture will simply be downloaded and printed at home.
While they cost around $20,000 just three years ago, there are now machines being developed that will be sold for under $500, thus making the technology increasingly available to the average consumer and laying the foundations for a potential explosion in the home inventor and home DIY markets. It’s not hard to imagine a future where a trip to the dentist will see him print you a new tooth, if you have a crash in your car you can just print a new chassis, or all furniture will simply be downloaded and printed at home.
Included is an infographic by engineering.com which illustrates the brief history of this growing industry
By Dan Price
Printing organs: how ears, skin and noses are made with a 3D printer
- Natalka Pisnya
- BBC Russian Service, USA
it will help you sort things out.
Image copyright, Masela family archive
Photo caption, Luc Masela with his parents one month after the artificial bladder transplant. year 2001.
year 2001.
Luc Masela, now 27, is an athlete with a degree in economics, works for a major exhibition company, travels a lot and recently met, in his words, "the most beautiful girl in the world." Both she and most of his current friends were extremely surprised when they learned that 17 years ago he survived a dozen and a half operations.
Luke was born with spina bifida - and although he was able to walk, his bladder was severely damaged. By the age of 10, he almost did not leave hospitals: due to improper functioning of the bladder, fluid began to return to the boy's kidneys, doctors diagnosed an irreversible pathology of the organ.
You need JavaScript enabled or a different browser to view this content
Video caption,"3D printed" organs are here
Doctors offered the family two solutions: lifelong dialysis or the creation of a new bladder from a segment of the intestine.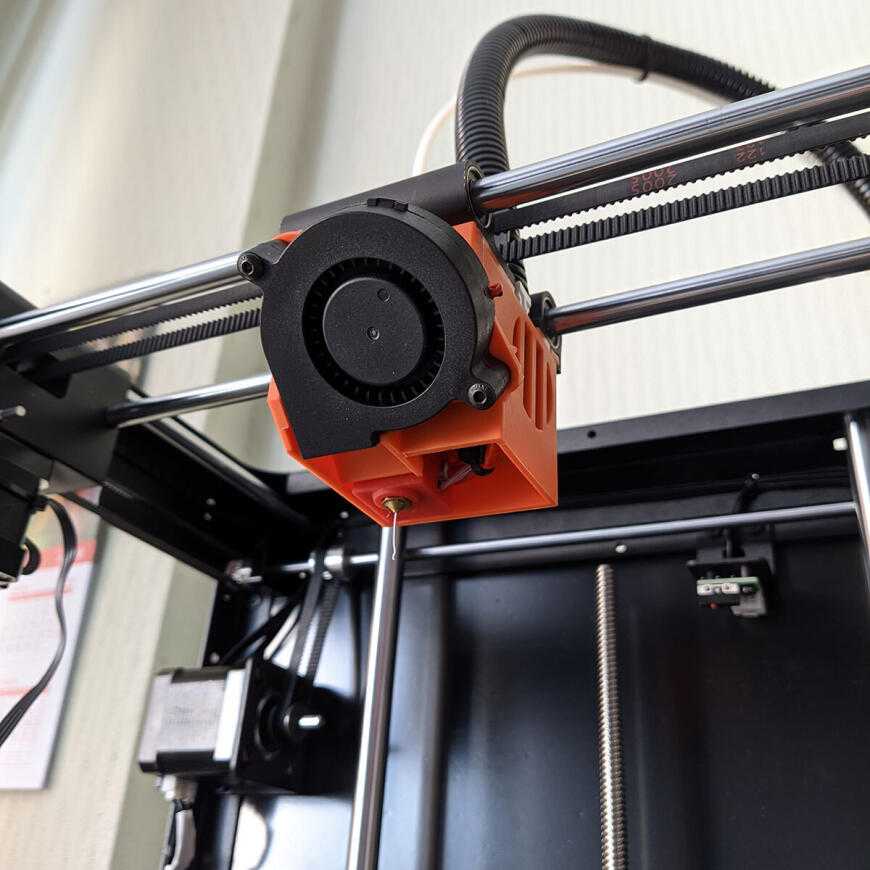 This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
This would guarantee Luke several years of medically supervised life and a high risk of developing cancer.
The urologist in charge of the boy suggested that Masela's family take part in an experimental program to grow a new bladder from his own cells. Then, in 2001, it sounded like science fiction: only nine people took part in the program before Luke. Despite this, his family agreed.
"The essence of the operation was reduced to two stages: first, a piece of bladder tissue was taken from me, and over the next two months, cells were grown in the laboratory in order to grow a new healthy bladder from them," says Luke.
Photo copyright, Masela family archive
Photo caption,Luc Masela, 17 years after the artificial bladder transplant
Next was the transplant operation, which, according to him, lasted 16 hours. “I opened my eyes and saw a cut through my entire stomach, tubes of all possible sizes were sticking out of me, except for them - four IVs and a bottle-feeding machine,” he recalls. “I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
“I stayed in the hospital for another month, I was prescribed bed rest, after that I stayed at home for another month.
The operation was performed by Dr. Anthony Atala, Pediatric Regenerative Surgeon. In two months, out of a hundred patient cells, scientists created one and a half billion. Further, an engineering structure was created on a collagen frame: the bladder was “sculpted” like a two-layer pie, the core of which dissolved over time, and it started working like a normal organ, taking root thanks to Luke’s own cells.
- An animal capable of regrowing its head
- The birth of a chimera: why do scientists need a human-animal hybrid?
- Swedish company 3D prints body parts
Luke and Dr. Atala haven't seen each other for 10 years after being discharged from the hospital. Once a dying child became the champion of the school wrestling team and went to college.
The professor took charge of the Wake Forest Institute of Regenerative Medicine in North Carolina in those 10 years, but Luke was never forgotten: his bladder was one of the most challenging and most successful projects in his early practice.
By 2018, Atala won the Christopher Columbus Award for "work on a discovery that will have a significant impact on society"; The Times and Scientific American magazines at various times named him "Physician of the Year", he was also recognized as "one of the 50 scientists on the planet who in the next 10 years will change the way we live and work."
How to print a new face
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
In the mid-2000s, Atala's team turned their attention to an ordinary household 3D printer and wrote special software for it, later specialized machines were created for the laboratory. Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
Now the laboratory "grows" up to 30 different types of cells and organs, as well as cartilage and bones.
One of the team's latest achievements is ears and noses grown outside the human body.
The main customer and sponsor of Atala's developments is the US Department of Defense, and many of the patients are military victims of military operations.
It works like this: first, a CT scan of the ear or nose is done. One of Atala's assistants, Joshua Corpus, jokes that at this stage, people often ask to "improve" the shape of the nose if they thought theirs was too wide or hooked, and the ears if they were too wide.
After that, a special computer code is written, and the printing of the base of the organs begins.
For this, a bioabsorbable polymer, polycaprolactam, is used. At the same time flexible and durable, in the human body it disintegrates within four years.
After printing, the layers of polycaprolactam resemble lace; after transplantation, their place will be taken by a person's own cartilage tissue in a few years after transplantation.
Polycaprolactam is then saturated with a gel created from the patient's cells, cooled to -18 degrees Celsius - so the cells, according to scientists, are not damaged, they are "alive and happy."
Image caption,Printing a test kidney sample on a bioprinter
In order for the polymer and gel structure to take shape and become something more durable, ultraviolet light is used in the laboratory - it does not damage cells.
The future implant is printed for 4-5 hours, then it is finally formed and inserted under the epidermis.
Skin can also be grown: children affected by the fires were the first to participate in the early trials of Atala - after the "printing" of the skin, scientists observed the patients for several more years. The new skin did not crack, did not burst, and grew with the children.
The most difficult job, according to the scientist, is facial wounds: it’s not enough just to stretch the skin, you need to accurately calculate the geometry, align swelling, bone structure, and understand how a person will look after that.
In addition to the skin and ears, Atala can "print" the bones of the jaws, grow blood vessels and cells of some organs - the liver, kidneys, lungs.
This technology is especially appreciated by oncologists: on the basis of patient cells, it is possible to recreate the body's response to various types of chemotherapy and observe the reaction to a particular type of treatment in the laboratory, and not on a living person.
But the liver, kidneys, lungs and heart are still being tested. Atala says he raised them in miniature, but creating organs from various tissues to real size requires a lot of additional research.
But, according to him, cells were grown in the laboratory and a vagina was created for a girl who was born several years ago with a congenital deformity of the genital organs - several years have passed since the transplant.
Image caption,Bioprinted polycaprolactam ear implant base
Atala smiles and adds that his team is also working on a working penis. This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
This research has been going on for several years, and the most troublesome for scientists is the complex structure of tissues and the specific sensitivity of the organ itself.
Among others, Igor Vasyutin, a Russian post-graduate student of the First Moscow State Medical University (MGMU) named after Sechenov, is working on this under laboratory conditions. He is a cell biologist, Atala's right hand.
Vasyutin has been in the USA for about a year - he came on an exchange. He is ready to talk about the behavior of stem cells for hours, but becomes less verbose when it comes to Russian science.
Vasyutin's alma mater has not reached mass regeneration of human organs and is still training on animals: local scientists "printed" a mouse thyroid gland on a 3D printer.
However, they are also involved in the study of human organs. According to the head of the Institute of Regenerative Medicine at MSMU Denis Butnar, several years ago the Institute recreated a special engineering design of the buccal mucosa. She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
She functioned perfectly for the first six months, but subsequently had to undergo a second operation.
Test specimen of an ear implant exposed to ultraviolet light
In Russia, however, over the past few years, the Italian surgeon-transplantologist Paolo Macchiarini has been practicing - the man who was the first in history to perform an operation on transplanting a synthetic organ - a plastic tube that replaced the patient trachea.
- Paolo Macchiarini: the rise and fall of the famous surgeon
However, seven of his nine patients died, and the breathing tubes implanted in the remaining two subsequently had to be replaced with donor ones.
Several criminal cases were brought against him, including on charges of pressure on patients and fraud, and the world's leading doctors called Macchiarini's operations "ethical Chernobyl."
Will printed organs replace donors?
At the zenith of his career, Macchiarini argued that a new perspective is opening up for humanity: you can "print" any human organ on a printer, create an engineering structure from it, enriched with the patient's stem cells, and get the perfect prosthesis.
Be that as it may, complex human organs - the liver, kidneys, heart, lungs - have not yet been grown by any regenerative surgeon.
Bioprinting of the so-called simple organs, however, is already available in the USA, Sweden, Spain and Israel - at the level of clinical trials and special programs.
The US government is actively investing in such programs - in addition to Wake Forest, cooperating with the Pentagon, the Massachusetts Institute of Technology also receives significant amounts to recreate the functioning of the liver, heart and lungs.
Image caption,Skin application test on a burnt wound
According to Professor Jorge Raquela, a gastroenterologist at the Mayo Clinic Research Center, "Bioprinting is one of the most exciting branches of modern medicine, it has huge potential, and the turning point of the most important discoveries is already close."
Meanwhile, Pete Basillier, head of R&D at analytics firm Gartner, insists technology is advancing much faster than understanding the implications of 3D printing.
Such developments, according to Basilière, even if created with the best of intentions, give rise to a set of questions: what will happen when "improved" organs are created, the basis of which will not only be human cells - will they have "superpowers"? Will a regulatory body be created to monitor their production? Who will check the quality of these organs?
More than 150,000 Americans are on the waiting list for organ transplants every year, according to a report from the US National Library of Medicine. Donor organs will receive only 18% of them; every day in the United States, without waiting for a transplant, 25 people die. Organ transplants and subsequent rehabilitation cost insurance companies and patients $300 billion in 2012 alone.
- A 3D printer helped a cyclist who lost his jaw
- Genetically modified pigs - human organ donors?
- The world's first child who received both hands transplanted plays baseball
Most Americans are potential donors: upon obtaining a driver's license, they voluntarily answer the question of whether they agree to donate their organs in the event of a car accident or other dangerous incident . In case of consent, a small "heart" and the word "donor" appear in the corner of the document.
In case of consent, a small "heart" and the word "donor" appear in the corner of the document.
Professor Atala's driver's license is the same - despite all his achievements and faith in the press, he is ready to share his with others.
Neither the professor himself, nor his subordinates hide the fact that science is not yet able to "print" organs for thousands of those who need transplantation right now. According to him, it will take several decades to replace donor organs with grown ones at the mass market level.
The work of Atala and others in the field of regenerative medicine remains more probing than mainstream, and still tailored to the individual patient.
We will live. When people start transplanting organs printed on 3D bioprinters
Starting from the new academic year, the Moscow Technopolis will for the first time start recruiting students for the Additive Technologies course. High school students will be introduced to professional 3D printing, which is no longer something unusual and is moving into the category of ordinary knowledge. If technology continues to develop and penetrate everyday life at the same pace, then perhaps the bioprinting of human organs will eventually become a common hospital procedure.
If technology continues to develop and penetrate everyday life at the same pace, then perhaps the bioprinting of human organs will eventually become a common hospital procedure.
PHOTO: mos.ru / Official website of the Mayor of Moscow
It all started with an unexpected discovery about the size ratio of two seemingly incommensurable things. That's when one lucky researcher instead of the traditional: "Eureka!" - could enthusiastically exclaim: "Tutelka in tyutelka!" It was not yesterday and not with us. And 20 years ago and, who would doubt it, in America. Bioengineer Thomas Boland - thin, brainy and bespectacled - found that the size of a human cell (about 10 microns) is almost equal to the size of the drop of ink that the printer "squeezes" out of itself when printing. And what will happen, then the curious Thomas thought, if we “fill” into the cartridge of the “typewriter” not a banal paint, but some kind of biological liquid, densely seasoned with cellular organics? Thought and then experimented. Speaking generally, without technical subtleties, he "shamanized" an ordinary office inkjet printer and printed a fragment of human DNA on it. This small step taken by Boland in the twilight of a new direction of near-medical research (by modern standards, of course, “knee-taking experience”) was a real breakthrough in the development of bioprinting as such. A huge step for all mankind. Actually, something big always starts with something small. Whether it's space exploration or the seal of a living human heart.
Speaking generally, without technical subtleties, he "shamanized" an ordinary office inkjet printer and printed a fragment of human DNA on it. This small step taken by Boland in the twilight of a new direction of near-medical research (by modern standards, of course, “knee-taking experience”) was a real breakthrough in the development of bioprinting as such. A huge step for all mankind. Actually, something big always starts with something small. Whether it's space exploration or the seal of a living human heart.
Smelling what it smells like, futurologists plunged into pink dreams of a future in which donor organs will lose their value. Generally. Anyone can be printed on a special bioprinter in a matter of hours and successfully transplanted to someone in need. Even bones, even skin, even kidneys or lungs with a liver.
— At that time, our scientific director Vladimir Alexandrovich Mironov, a recognized pioneer of bioprinting, while being a visionary futurist, said that bioprinting had moved from science fiction to science fiction, — says the commercial director of the Moscow laboratory of biotechnological research of one of the international companies, being a resident of Skolkovo, Andrey Rukavishnikov.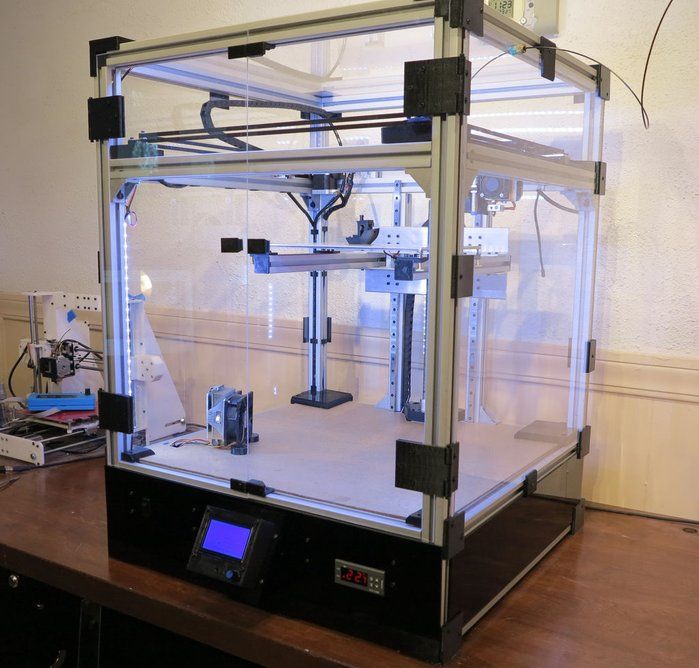 - But today it is already scientific and test work. Real science, and not theoretical, but practical. If once the visionary Mironov, speaking about bioprinting, foresaw it, now it is already a rapidly developing industry. In 2012, when we started, our company was the first in Russia and the sixth laboratory in the world conducting research in the field of bioprinting. And today there are about a hundred such companies around the world.
- But today it is already scientific and test work. Real science, and not theoretical, but practical. If once the visionary Mironov, speaking about bioprinting, foresaw it, now it is already a rapidly developing industry. In 2012, when we started, our company was the first in Russia and the sixth laboratory in the world conducting research in the field of bioprinting. And today there are about a hundred such companies around the world.
Arms race
Now there is a rivalry between the world's scientific laboratories. The stakes for the winner are very high. Scientists and researchers understand that the one who is the first to be able to print a living human organ that can take root and function will go down in the history of medicine and receive the Nobel Prize. What is there! He will change this world forever. Moreover, today we are no longer talking about a piece of skin for transplantation, or, say, an ear, or a bladder - bioprinting has already coped with this task, and experiments conducted in China and America have shown that these organs successfully take root.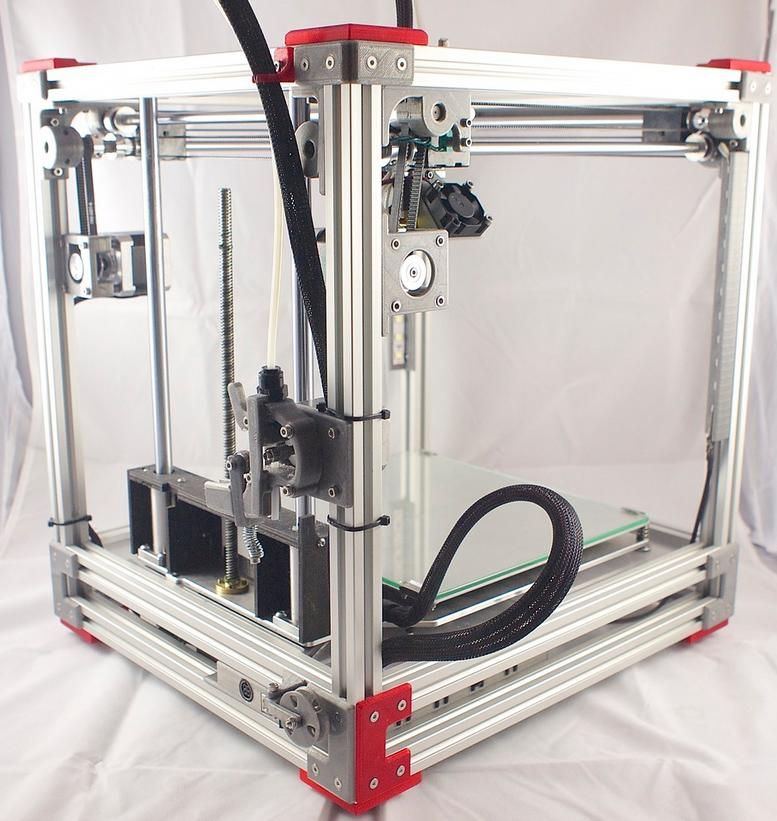 Bioprinters call them simple, because cartilage, bones, and skin are made up of a small set of cells that are relatively easy to reproduce. The same bladder is essentially a shell. If the word “simple” is generally applicable in bioprinting technology. The main big goal is a complex viable organ, penetrated by thousands of capillaries and consisting of dozens of groups of different cells, even isolating some of which is an almost impossible technical task. Like the kidney, lung, or heart that bioprinters call their holy grail. So far, no one in the world has managed to print a living human heart with which a person could live. Equally, by the way, like another complex organ. Last year, Israeli scientists tried to surprise the world with an incredible achievement, but in fact it turned out to be just a noisy hype: a heart printed on a 3D bioprinter was not transplanted into a person, and it remains unclear whether it can take root and work like a living one or like most complex organs. created from cells in recent years will die in 40 hours.
Bioprinters call them simple, because cartilage, bones, and skin are made up of a small set of cells that are relatively easy to reproduce. The same bladder is essentially a shell. If the word “simple” is generally applicable in bioprinting technology. The main big goal is a complex viable organ, penetrated by thousands of capillaries and consisting of dozens of groups of different cells, even isolating some of which is an almost impossible technical task. Like the kidney, lung, or heart that bioprinters call their holy grail. So far, no one in the world has managed to print a living human heart with which a person could live. Equally, by the way, like another complex organ. Last year, Israeli scientists tried to surprise the world with an incredible achievement, but in fact it turned out to be just a noisy hype: a heart printed on a 3D bioprinter was not transplanted into a person, and it remains unclear whether it can take root and work like a living one or like most complex organs. created from cells in recent years will die in 40 hours.
— It will take a long time before experiments on mice can be switched to experiments involving humans, — Andrey Rukavishnikov explains. - First - preclinical and clinical trials on rodents, then on larger animals, and only then on volunteers. And then after reliable results appear, proving that organ structures are safe for human health and will not cause unexpected consequences. In addition, it is necessary to certify such a treatment method as a surgical intervention with an organ construct printed on a bioprinter. And so far, as far as I know, such operations have not yet been certified anywhere. The path is long, thorny and winding, because no one will risk the lives of people, and the technology must be brought to perfection. Now it is in the process of development.
Mission Possible
Analysts estimate that the global 3D bioprinting market is currently valued at more than $960 million and will reach $4.4 billion by 2026. The average annual growth rate is 19.5 percent. And, looking at these figures, you believe the forecasts of experts from the International Society for Biofabrication, who predict that already in 2030 complex organs printed on a printer will be successfully transplanted into humans. And another year or two will pass, and such operations will be carried out as planned, in the conditions of capital clinics.
The average annual growth rate is 19.5 percent. And, looking at these figures, you believe the forecasts of experts from the International Society for Biofabrication, who predict that already in 2030 complex organs printed on a printer will be successfully transplanted into humans. And another year or two will pass, and such operations will be carried out as planned, in the conditions of capital clinics.
Scientific experiments will be replaced by ordinary medical practice.
“The peculiarity of transplanting a printed organ is that there is no immune attack on it,” emphasizes Rukavishnikov. “After all, even a donor organ that is as close as possible in terms of blood composition is rejected by the body. And a person has to take medicines that suppress immunity all his life. Bioprinting solves this problem. The mission of printers is to enable people to live longer and better lives. There will be no need for diets, drugs, or exercise restrictions, as is now the case for people who have received a donor organ.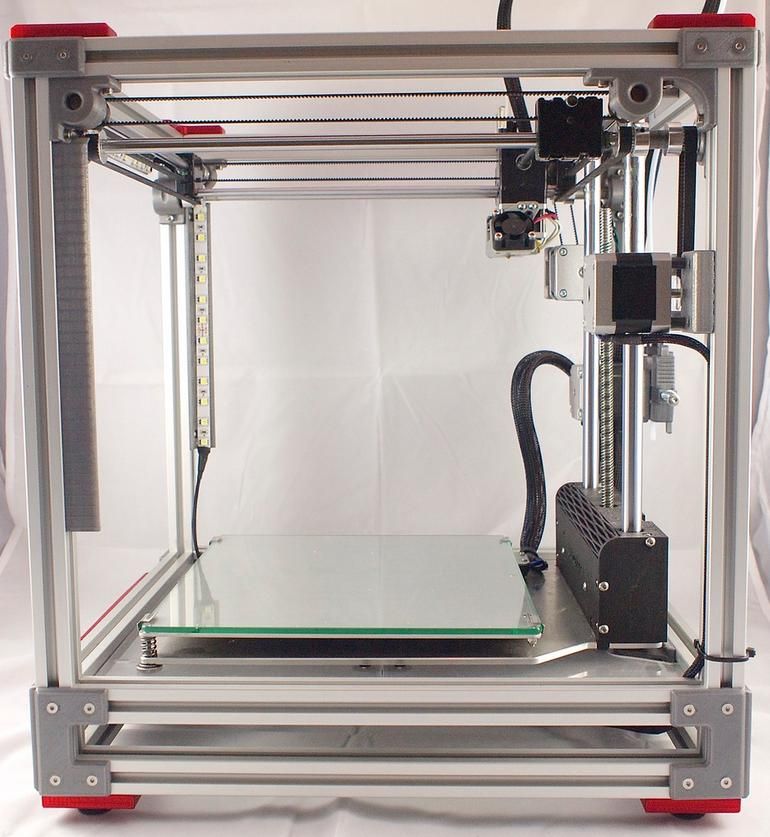 The printed organs will take root as native ones. This is a mission that will change all of medicine. It will take it to another level, where we can print organs on demand from the patient's own cells. Plus, you won’t have to wait in line for a transplant. And that means you don't have to wait for the other person to die. It's not easy from a moral and ethical point of view.
The printed organs will take root as native ones. This is a mission that will change all of medicine. It will take it to another level, where we can print organs on demand from the patient's own cells. Plus, you won’t have to wait in line for a transplant. And that means you don't have to wait for the other person to die. It's not easy from a moral and ethical point of view.
In the meantime, "bioprinters" are working with simpler organs and living human tissue, on which pharmacists test new types of drugs. Including from the coronavirus.
“We print lung tissue and give it to virologists,” says Rukavishnikov. “They infect her and then test antiviral drugs. In this way, we reduce the time, because before human experiments become available, it may take years. Many groups around the world are looking for a cure for coronavirus, dozens of drugs are being tested. And bioprinting can drastically reduce testing time.
As for organs, simple ones in Russia (the same printed skin) are successfully transplanted into laboratory mice, and in the States and China there have already been successful experiments on humans.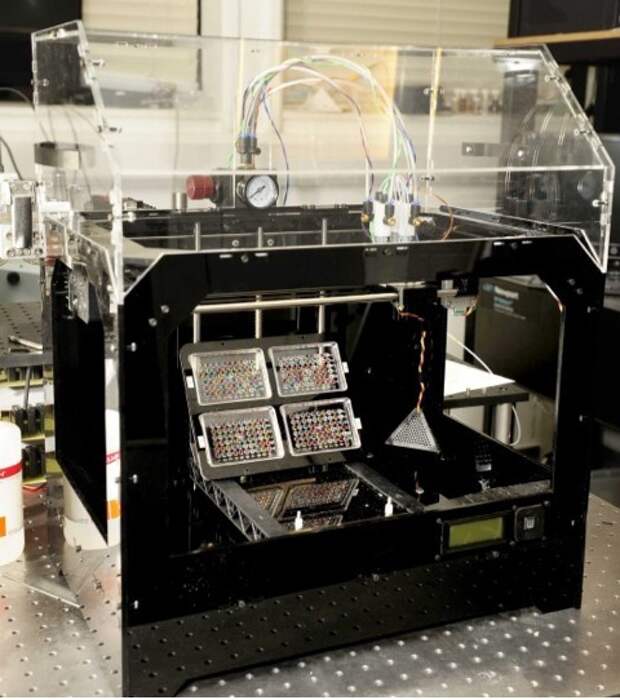 They also learned how to print "working" fragments of complex organs - heart valves, blood vessels, bone tissue for "patches" on the skull. By the way, printing parts of organs for replacement is a more tangible prospect. And this method makes the procedure itself less traumatic. If, when “patching” the skull today, a metal patch is adjusted to the size of a living bone almost with a hammer, then the one modeled on a computer and printed on a printer fits perfectly.
They also learned how to print "working" fragments of complex organs - heart valves, blood vessels, bone tissue for "patches" on the skull. By the way, printing parts of organs for replacement is a more tangible prospect. And this method makes the procedure itself less traumatic. If, when “patching” the skull today, a metal patch is adjusted to the size of a living bone almost with a hammer, then the one modeled on a computer and printed on a printer fits perfectly.
“In addition, bioprinting can help in the fight against cancer,” sums up Rukavishnikov. “It can be used to propagate a piece of a tumor in a bioreactor, print samples of tumor tissue, and further conduct experiments to select the ideal drug and ideal treatment for a particular patient. Now “chemistry” is carried out for good luck: this or that medicine will help, it will not help, and then, this is a very traumatic treatment for the whole body. Bioprinting will make cancer treatment completely painless.
REFERENCE
Bioprinting (bioprinting or “printing of life”) is a technology for creating three-dimensional models on a cell basis using 3D printing, which preserves the viability of cells.
Organs are created using a photosensitive hydrogel, powder filler or a special liquid based on living cells to create organs on a 3D printer.
First, fragments of cellular material are printed according to a computer-calculated form, then it is grown to a whole organ in an incubator, where the cells are fused with each other. By the way, living printed tissue is used not only to test drugs, but also cosmetics. This eliminates the need for animal testing.
A separate branch of bioprinting, not directly related to organ printing, is the production of bone prostheses from polymers, plastics or ceramics.
REPLICA
Ashkhen Hovsepyan, General Director of Additive Engineering, Technopolis Moscow SEZ:
— The state should get involved in the development of bioprinting. Not in the sense that a huge bureaucracy should work, but it seems to me very important when developing technology is supported from all sides.
The field must be well sponsored. We need serious money. If, for example, in America these are the funds of venture investors who are ready to invest, because this is part of the culture, then in our country, by and large, the state has always been responsible for such global projects. As for the commercial component, there are patrons who want to invest for the sake of faith in bright future. But if we talk about business investors who are waiting for a return on investment, then real demand needs to be raised. We need real projects with real forecasts. And our scientists are not yet working in the format of a business plan.
We need serious money. If, for example, in America these are the funds of venture investors who are ready to invest, because this is part of the culture, then in our country, by and large, the state has always been responsible for such global projects. As for the commercial component, there are patrons who want to invest for the sake of faith in bright future. But if we talk about business investors who are waiting for a return on investment, then real demand needs to be raised. We need real projects with real forecasts. And our scientists are not yet working in the format of a business plan.
And with regards to specialists. In addition to people who are directly deeply involved in the printing of organs, a whole direction of ethical education has appeared. When we learn how to print viable human organs, we will essentially orchestrate nature.
But if a person does not have strong spiritual qualities, he can do stupid things. Therefore, now educational centers and mentors have appeared, telling about how important it is to remain human and not go too far.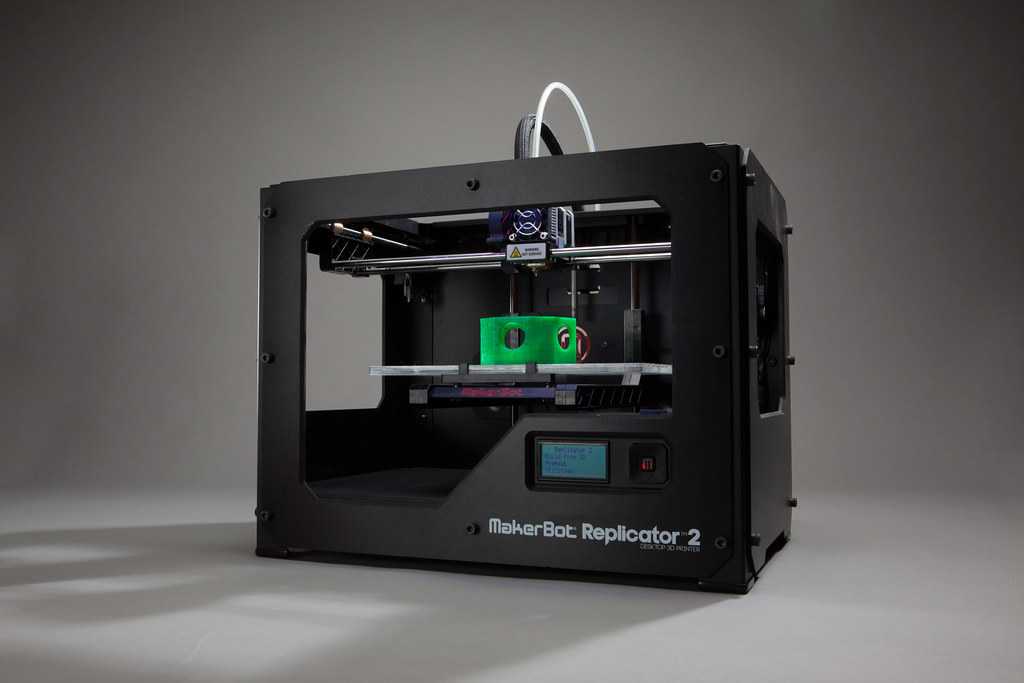
LITTLE VICTORIES
- 2003 Thomas Boland received a patent for 3D printing for the manufacture of a cell structure using inkjet printing.
- 2006. The first major success in the field of 3D bioprinting was the transplantation of a bladder printed on a printer by American doctors.
- 2008. Professor Makoto Nakamura from Toyama University presented a ready-made device for printing biomaterials. For the first time, he managed to print a biological tube that looks like a blood vessel.
- 2010. US company Organovo has printed the first complete blood vessel.
- 2014. The specialists of the same company printed the liver. The fabric lived for five weeks.
— 2015. Russian researchers transplanted a mouse with a thyroid gland printed using a new Russian FABION bioprinter. The constructs took root.
- 2017. In China, 3D printed ears were transplanted to children with a congenital ear defect.
- 2018. Russian “bioprinters” sent a new bioprinter to the ISS, where they printed the thyroid gland of a mouse in zero gravity. For the first time, a new magnetic bioprinting technology was tested using a magnetic field instead of a biodegradable substrate.
Russian “bioprinters” sent a new bioprinter to the ISS, where they printed the thyroid gland of a mouse in zero gravity. For the first time, a new magnetic bioprinting technology was tested using a magnetic field instead of a biodegradable substrate.
- 2019. Scientists at the American Rensselaer Polytechnic Institute printed skin with blood vessels and transplanted it into mice.
- 2020. Toronto researchers have tested a portable 3D printer on pigs that can be used to treat skin burns. The device applies fibrin sheets directly to the wound.
OBSTACLES AND DIFFICULTIES
■ At the current level, bioprinting is still not in great demand in practice. Even companies operating in its well-developed areas receive a small number of orders.
■ The human body contains a huge number of groups and types of cells. And isolating them in order to then multiply and use in bioprinting is a very difficult task. Not all cells have yet succumbed to scientists.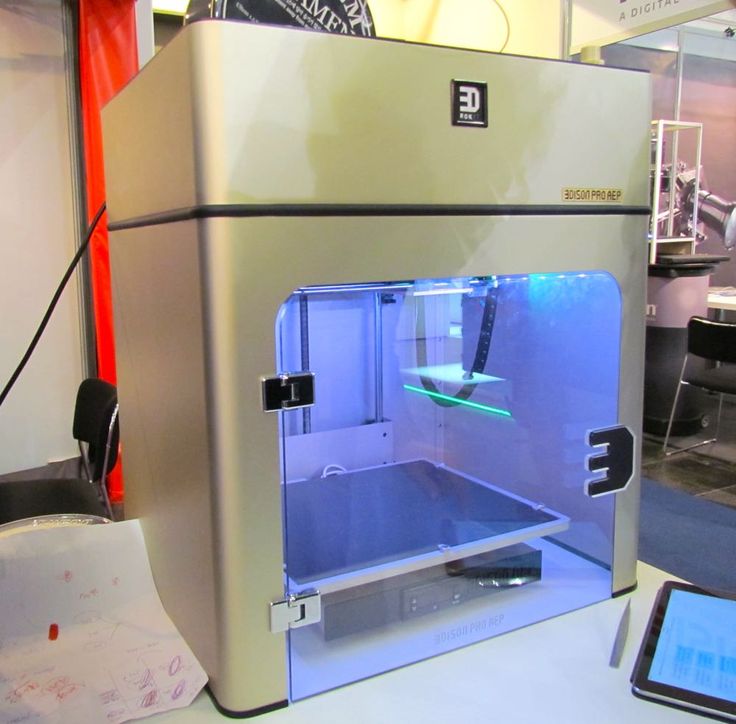
■ Short life of printed organs. Even when it was possible to print a liver or a kidney, the organs did not live very long.
■ In the West, where 3D printing is more common, this service is expensive. How it will be with us is unknown. Will printed organs become available to everyone and will such operations be carried out under compulsory medical insurance, as is now, say, happening with the same kidney transplantation, the costs of which were assumed by the state? Or will bioprinting become the property of the elite? These are questions to which we will not get answers soon.
■ The medical profession is still apprehensive about the prospect of working with printed organs. Although the "bioprinters" are sure that this will pass. In the same way, even five years ago, printing in dentistry was treated with distrust, but today 3D printers are used very actively in this area.
■ Many questions about certification. There are no standards in bioprinting yet. And it is not yet clear what they should be.